Telepsychiatry, a subset of telemedicine, has been defined as the provision of psychiatric services to patients remotely using information and communication technologies (Chakrabarti, 2015). This cross-sectional survey was conducted to assess the knowledge, attitudes, and practices of healthcare professionals working in the Mental Health Services, Hamad Medical Corporation, Doha Qatar towards telepsychiatry.
Methodology: An online questionnaire based cross-sectional survey was conducted among all mental health professionals including psychiatrists, nurses, occupational therapists, clinical pharmacists, social workers, and psychologists. A thirty-item questionnaire was developed to assess the knowledge, attitude, and practices of telepsychiatry in relation to COVID-19 following extensive literature search on the topic. An email with a link to the online survey was sent to all the eligible participants through a department group email. Responses were collected during a six-week period. All approvals from respective departments were obtained before proceeding with the study.
Results: A total of 224 respondents completed the survey giving a response rate of around 50 %. A majority of the participants belonged to age brackets 25–34 and 35–44 years, and there was a slight male preponderance 53 % vs. 47 %. Most responses were from nurses (50 %) followed by occupational therapists (11 %) and consultants (9 %). As to knowledge about telepsychiatry and related terms, 173 (77 %) of the respondents were familiar with the term telepsychiatry and 164 (73 %) were able to explain the concept. However, only 40 respondents (18 %) reported being familiar with the term virtual care.
The majority of respondents (n = 188; 84 %) knew that telepsychiatry was currently being used around the globe during COVID-19 pandemic. Fifty-one respondents (22 %) believed telepsychiatry decreased patient satisfaction, whilst 93 respondents (41 %) felt telepsychiatry had little impact on cost, access and stigma.
As to the practice of telepsychiatry specifically in the context of COVID-19 pandemic, an overwhelming majority of respondents (n = 190; 95 %) believed it decreased infection risk, 190 respondents (85 %) felt it was the best mode of service delivery, and 178 respondents (80 %) considered it equally or more effective than conventional practice.
A large number of respondents (n = 197; 88 %) concurred that telepsychiatry could be utilized in the community settings, COVID-19 treatment facilities (n = 156; 70 %) and quarantine sites (n = 172; 77 %). However, only 57 respondents (25 %) believed it could be used in the emergency department. Over half of the respondents (122; 54 %) believed telepsychiatry could be used for both new and follow up patients. Respondents believed that telepsychiatry could be reliably used for obtaining patient history (n = 189; 84 %), providing psychoeducation (n = 205; 92 %), risk assessment (n = 126, 56.3 %) mental status examination (n = 102, 45.5 %), and formulating a management plan (n = 164; 73 %).
Challenges in telepsychiatry were reported as follows: building rapport (n = 154; 69 %), assessing non-verbal cues and body language (n = 187; 84 %), and maintaining privacy (n = 102; 56 %). One hundred eighty-three respondents (82 %) felt that teleconsultations could be used even after the pandemic is over. Most respondents (n = 192; 86 %) believed they would benefit from further training in telepsychiatry. As to using telepsychiatry alongside conventional practice, all trainee doctors were in favour as compared to two third of the senior doctors.
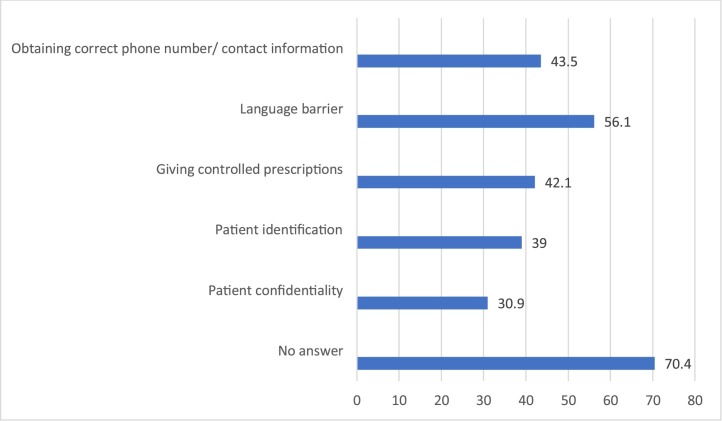
Two thirds of the respondents (n = 150; 67 %) reported conducting telephone consultations, and they described this experience as good or excellent from both their own and their patients’ perspective. Overall, 57.14 % thought that switching to telephone consultation decreased the no show rate of patients at the outpatient clinics. Fig. 1 enlists the common problems encountered by responders using telepsychiatry. Interestingly, videoconferencing for consultations was used by only a minority of the respondents (n = 27; 16 %).
Fig. 1.
A list of reported difficulties encountered during the conduction of teleconsultations.
When compared to other mental health professionals (53.25 %); more doctors (80 %) thought that telepsychiatry can be used alongside face-to-face interviews. With regards to COVID-19, 96 % of doctors considered telepsychiatry the best treatment option, compared to 81 % of the others group, while more than 90 % of both groups thought that telepsychiatry can play a role in reducing the risk of infection for both, the health care givers as well as for patients. As for post pandemic, more than 80 % of both groups considered telepsychiatry a viable option for future appointments at outpatient settings.
This study was conducted during the early days of the COVID-19 pandemic. Even at that time, a majority of the participants of our study reported using teleconsultations and considered it a favorable option from both the patient's and their own perspectives. The questionnaire we used was not validated, and that may be regarded as a limitation. Another limitation perhaps is the fact that the study was conducted early on during pandemic and over the ensuing few months most professionals used telepsychiatry thereby causing a change in their knowledge and attitudes.
In conclusion, this study demonstrated positive perception toward telepsychiatry in mental health professionals. The current pandemic has fast-tracked telepsychiatry as a mode of service delivery. Telepsychiatry holds hope and promise for the future as a cost-effective method of treatment alongside conventional practice.
Funding
The study had no funding.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgment
The authors acknowledge the Medical Research Center at Hamad Medical Corporation for their support.
References
- Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation of videoconferencing-based approaches. World J. Psychiatry. 2015;5(3):286–304. doi: 10.5498/wjp.v5.i3.286. [DOI] [PMC free article] [PubMed] [Google Scholar]