Abstract
Background and objectives:
Poor self-management contributes to reduced renal allograft survival during adolescence and young adulthood. Providing patients with self-reflection tools to help explore the question “Is my experience normal?” may help mitigate these challenges. We explore Photograph-elicitation, a qualitative method where images are used to prompt individuals to talk about their personal experiences and values, engages pediatric transplant recipients and their families to generate insight into their experiences and the challenges they face after transplant.
Design, setting, participants, and measurements:
Pediatric renal transplant recipients and one family member from Seattle Children’s Hospital submitted 5 photographs showcasing their transplant story, which were used as prompts during semi-structured interviews. Interviews were recorded, transcribed, and analyzed using thematic analysis.
Results:
Twenty-four individuals (13 patients: ages 7–21, and 11 parents) completed the study. Conversations generated by the photographs covered topics in more depth than a routine clinical encounter leading to more opportunities for reflection by patients and their family. The photographs generated conversations on four emergent themes: (a) sensemaking; (b) transitions and agency; (c) social interactions and community engagement; and (d) barriers and obstacles.
Conclusions:
Photograph elicitation generated a rich dataset describing a range of pediatric renal transplant experiences helping physicians gain a rich and nuanced understanding of the daily lives and experiences of their patients outside the clinical setting. Photograph elicitation, as a clinical intervention, may provide new opportunities to address previously unrecognized modifiable risk factors, improving graft survival and health-related quality of life.
Keywords: adherence, kidney transplant, photograph elicitation
1 |. INTRODUCTION
Kidney transplants provide lifesaving treatment to children and adolescents living with ESRD, yet for a recipient to realize the full benefit of a transplant, they and their families must adhere to rigorous and complex treatment protocols.1,2 Non-adherence with post-transplant medical regimens resulting in acute rejection episodes significantly reduces the lifespan of a transplanted kidney as well as of the patient.3–6 Medication non-adherence is the leading cause of late acute rejection after a kidney transplant7–9 and the leading cause of accelerated kidney loss limiting survival of the transplanted organ.5,6 Even minor rates of non-adherence have been associated with higher rejection rates.9–11 Further, adolescents have the highest risk of non-adherence rates with estimates as high as 43%, which are up to twice as high as younger children and 2.5 times higher than adults.4,8,12 As older children transition to young adulthood, it is critical to instill strong habits of adherence.
For clinicians, understanding and addressing problems faced by patients in adhering to treatment plans require familiarity with patient narratives, both in the moment and over time.13 While formal barrier assessment tools exist,34 more work is required to better understand contextual factors related to family dynamics, home life, and impacts of managing chronic health conditions which all influence adherence.
In order to gain more insight into these nuanced factors, we explored how PE15,16 can augment information gathered in traditional clinical interviews and provide novel insights into the experiences of individuals and their families after a kidney transplant. PE is a qualitative method that uses images to prompt individuals to talk about their personal experiences and values, helping researchers gain understanding of participant perspectives. Our study explored the ways that PE can uncover otherwise hidden adherence barriers at multiple levels. This allowed us to address the research question: How can Photograph-elicitation provide clinicians with insights regarding important non-clinical barriers to adherence and self-management of chronic health conditions?
2 |. MATERIALS AND METHODS
PE was used in a set of interviews with pediatric kidney transplant patients and their primary caregivers. English-speaking pediatric renal transplant recipients and one family member were recruited from a single, large volume pediatric transplant center in the United States as well as the IROC, Community Engagement Workgroup (CEW). IROC is a network-based learning health system working to improve the lives of children living with kidney disease, and the Community Engagement Workgroup (CEW) is a group of engaged parents, patients, and other caregiver partners within the collaborative. Potential participants from the transplant center were identified via convenience sampling, by identifying individuals with a scheduled transplant clinic visit who had a kidney transplant at least 3 months prior. Once identified, individuals were provided with a flyer in clinic or sent an invitation letter with details about the study, by either a member of the research team, a clinic-based medical assistant, or the attending provider scheduled to see the patient. In addition, a flyer was also distributed to the IROC Community Engagement Workgroup (CEW). If a potential participant indicated interest in participating, the lead author reached out to them to provide additional details and ultimately obtain consent and/or assent. To minimize the potential for power imbalances or influence, no primary patients of the first author were approached or included in the study.
Interviews were conducted by the first author, a pediatric nephrologist. The objective of the interviews was to better understand the experience of ESRD and transplant from the perspective of patients and their families. The authors’ Institutional Review Board approved this study.
After obtaining consent and assent, all participants were asked to submit five photographs telling their transplant story. Participants used their own devices to take the photographs, and no restrictions were placed on what images individuals could submit. We encouraged participants to bring in five photographs that captured both mundane and exceptional aspects of their experiences. Photographs could be in either digital or print format depending on the preference of the participant. Both the child and adult participants submitted their own set of photographs. During interviews, images were used to prompt participants to talk about their experiences, with particular focus on uncertainty (ie, how they assess progress or decline when disease progression is so individualistic). Based on early feedback, we added two questions at the end of each interview (1) asking participants how the PE process personally impacted them and (2) whether they felt PE would provide new and valuable information to their clinical care team. Interviews were conducted individually with all participants, to minimize parental influence. However, for participants under the age of 12, a parent was present during the child’s interview, and only participated whether asked a question by the child participant. All interviews, with few exceptions, took place in a private room within our clinical research center; three interviews were conducted via teleconference software. To thank each participant for their participation, individuals (ie, both patients and parents) were provided $25 at the completion of the study.
2.1 |. Analysis
Interviews were recorded and transcribed. Participant-generated images were embedded in transcripts through hypertext links, using the MaxQDA software.17 Exploratory thematic analysis of text and images followed established qualitative, inductive procedures.18 The first author conducted an initial round of inductive analysis to identify participant statements that contained information that would have been unlikely to come up during conventional clinical interviews. These were determined by comparing statement content with standard clinical interview protocols.19,20
Both authors then independently performed inductive thematic analysis of these statements, each coding a unique subset of the interviews equal to about 30% of the entire data set. Themes were then compared and reconciled into an inductive coding scheme comprising four content themes. This codebook was independently applied by each of the researchers to the entire corpus, and results were compared. Discrepancies were discussed and resolved.
3 |. RESULTS
Twenty-four individuals (13 patients: ages 7 – 21, and 11 parents) completed the study (Table 1). Only one pair of participants was recruited from the IROC CEW, and the remaining were recruited from Seattle Children’s Hospital. Our sample matched the demographics of the local transplant population. Interviews ranged from 18 to 67 minutes (mean: 37 minutes) in duration. The PE approach prompted frank, emotional, and personal descriptions of patient experiences. A host of new information and insights was revealed through the photograph prompts. Four themes emerged from these interviews: (1) routine barriers and obstacles, (2) sensemaking, (3) transitions and agency, and (4) social interaction and community engagement. Below, we describe each theme and provide examples. Quotes from transplant participants are identified by T#, and their parents as P# and are organized by theme-specific tables.
TABLE 1.
Participant characteristics
| Characteristic | Value |
|---|---|
| Age—Median (range) | |
| Transplant Participants | 17.5 (7–21) |
| Parents | 49.5 (37–75) |
| Gender—number (%) | |
| Transplant Participants | |
| Male | 7 (54%) |
| Female | 6 (46%) |
| Parents | |
| Male | 3 (27%) |
| Female | 8 (74%) |
| Time since transplant—Median (range) | 8.5 y (2–14) |
| Patients requiring dialysis prior to transplant | 10 (77%) |
| Patients on first transplant | 13 (100%) |
| Race (participants could select multiple options) | |
| White | 16 |
| Asian/Pacific Islander | 4 |
| Black or African American | 1 |
| Other/Not Reported | 5 |
3.1 |. Routine barriers and obstacles
3.1.1 |. Access to medications
Not surprising given the strict treatment protocols required for kidney transplant recipients, some of the most frequently discussed day-to-day obstacles involved medications, specifically having the right medication when needed, and remembering to take it (Table 2). For many caregivers and patients alike, adherence to medication protocols requires a significant amount of forethought and planning, not just a reminder in the moment (Figure 1A). For students, their schedule for taking medications might conflict with school and extracurricular activities. This forces patients to make choices about what is more important, recognizing that their decisions have social, academic, and medical consequences. Multiple families described hoarding expired medication (Figure 1B) explaining that they worry about the possibility of running out of their medications and being dependent on a supply chain that could be disrupted at any time.
TABLE 2.
Routine barriers and obstacle quotes
| Factors | Examples |
|---|---|
| Access to medications | We are always trying different gimmicks and things to make it fun for him to remember or just… for him to have more control at school, especially. He doesn’t really wear any… he’s wearing this one right now ‘cause he just recently found it and wanted to track his stuff I think (Figure 1A)—P7 |
| I’d prefer to miss class than missing my medicine because medicine is what’s really affecting me. If I don’t take my medicine then there is a different outcome than if I miss class…if I miss class, I can just talk to the teacher but if I miss my medicine, it’s gonna be a different way—T4 | |
| That is a box of expired meds, because I am scared that there is going to be an earthquake and we won’t be able to get refills on our medications, and the earthquakes going to happen right when we have an order coming and trucks are not going to be able to come to the house, so we’re not going to be able to get to the [medications] (Figure 1B)—P11 | |
| I cannot tell you how many things I’ve had to leave early because we accidentally left my meds at home. I have to say around a hundred maybe more. Right mom?”—T11 | |
| Everything is extraordinary | …how all the other normal kid things become magnified. His tooth didn’t break because he got hit really hard. His tooth broke because the enamel on his teeth are different because of his meds, because of his medical history, because of all that. So, it’s how those little things, those are hard. Those are the things that make me sad, because it’s just like it’s just that much harder for him. (Figure 1C)—P14 |
| I mean, on a daily basis, it’s like there’s the meds and the water and the going to the bathroom…For awhile it was really hard because… all of our parental disciplinary energy is being wasted on going to the bathroom vs stop fighting, all of our leverage. They’re all going just to these things that other kids don’t have to do, and it’s hard.—P14 |
FIGURE 1.
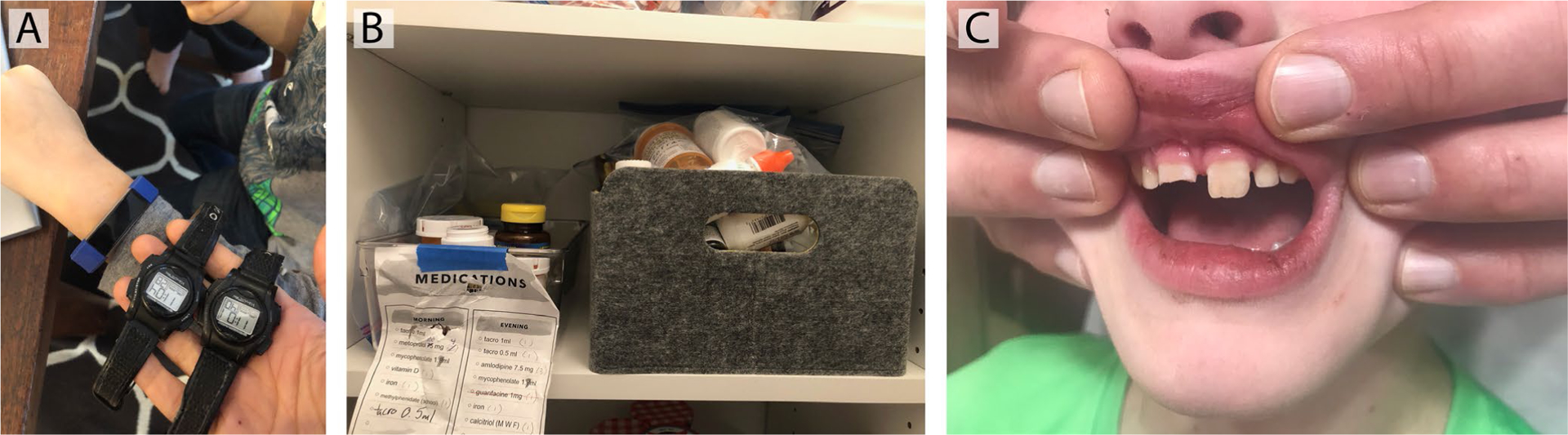
Images of routine barriers and obstacles. A, Medication reminder alarms. Image source: P7; (B) Hoarded medications. Image source: P11; (C) Broken tooth. Image source: P14
3.1.2 |. Everything is extraordinary
While there are many experiences of parenting that are marked by routine barriers, for our caregiver participants the routine challenges of daily life were often tethered to the larger reality of parenting a chronically sick child. One caregiver explained that they picked a photograph showing their child’s chipped tooth, weakened by medications, (Figure 1C) because it made them think about the ways that seemingly normal childhood events like this took on added significance for their child. This same parent explained that even their experience of disciplining their child for day-to-day infractions was impacted by kidney disease. A typical parenting experience is needed to “pick your battles”; however, parents in our study highlighted the ways that for them, this often involved needing to focus on adherence to a medical plan over other behavioral issues. Our participants also identified several other routine barriers such as how to best support young patients when medications altered their appearance in undesirable ways or dealing with the disappointment of not being able to participate in activities like swimming or contact sports.
3.2 |. Sensemaking
3.2.1 |. Fear and uncertainty
In daily life, patients and families must make sense of diagnoses, procedures, and outcomes in the context of everyday routines, family values, and available resources (Table 3). Yet due to kidney transplants being relatively rare, transplant recipients and their families often lack peer guidance about how to navigate challenges related to their transplant. For example, in talking about trying to find the right information, one patient used the visual metaphor of a darkened light to explain uncertainty and isolation (Figure 2A). Often, sensemaking activities appear during the process of working through fear, especially fear of the transplant failing and having to return to dialysis, the ultimate fate for all transplant recipients. When new symptoms or questions arise, patients and especially parents instinctually fear something is wrong with the kidney. The persistent work of disambiguating symptoms, while similar in some ways to the clinical differential diagnostic process, is deeply entwined with the emotions and responsibilities of caregiving, especially for parents. For some young patients, just making sense of a daily routine and following through with it was challenging, knowing the consequences of failing.
TABLE 3.
Sensemaking quotes
| Factors | Examples |
|---|---|
| Fear and uncertainty | “…the light’s out (Figure 2A) because it’s like there isn’t anything, nobody really guides you…there’s nothing, like when I’m in school there won’t be anything that will guide you if you have a kidney transplant. “ (T5) |
| “Or he has, maybe diarrhea, or he has constipation, things like that, then I want to make sure that it’s not the kidney…We always worry about that, we always worry that, God forbid, maybe… You know, rejection.”—P4 | |
| Yeah it was an experience in growth and learning where I really learned okay, how rare is this? Where does it come from? What is it like for other people who have it? It’s pretty rare. Just learning a lot about some of the potential symptoms and some things I may be likely to have because I have this and it was a lot of learning and specifically about a disease I have in my genetics and I really enjoyed that in science with learning about it.—T8 | |
| He hasn’t missed [his medications yet]. Once he went to the movie, he was 10 minutes late and I was so upset, I was worried. Once he was about an hour late and I called the hospital and talked to the doctor twice, I was shaking, that was in the beginning. The doctor said, “Does he have any, you know, diarrhea or has he thrown up?” I said no, he said “So, don’t worry. Ten minutes or 15 minutes is okay”. Then I realized okay, but I was scared.—P4 | |
| New normal | …when I first started I was more stressed on remembering to do it. But I felt like now whenever my daily routine, when I’m done and ready to go to bed I have a routine that I go downstairs, I go into the room, I get everything ready. I think it just has to be, you shouldn’t be scared. I mean you should more or less just be prepared.—T6 |
| I think that they’re just these minor ah-ha moments that happen along the way, where whether it’s just like even a phone call with a friend or a client or something, you’re like, “I can’t do that,” or “I don’t want to do that.”… My tendency is always to be like everything’s normal. Even after he was born, I went back to work after 6 wk, thinking, “I’m going to make life normal.” I think for me, it’s like I get so tired. I’m like okay, readjust, like that’s kind of a silly expectation. And a lot of times for me it takes a sounding board. My sister has been a great sounding board. I have a couple of attorney colleagues that are a great sounding board. They’re like, “No, you can’t expect that.” You know.—P14 | |
| You talk to the other parents and you’re like, we’ve had a couple of bad labs where we had to get biopsies. Or, the worst was she had to have her ureter re-attached because it was letting urine back up into her kidneys. But the other families that I hear about, the constant rejection episodes, and over and over, and losing kidneys, or having a rejection episode and having to be hospitalized and go through all the steroids, and all that stuff. I’m like oh my gosh, we’ve never even been close to that. So, I think our normal is a lot better than other normals for kidney transplant patients.—P11 | |
| I think I am in awe almost every day of just normal stuff that he does. He goes to school, and he can run around and things that when I was pregnant we were like, will he be able to do this? There were so many questions, and so I mean it’s still sort of mind blowing to think that he’s got a transplanted kidney in there. So, I was like, how could I… so this is one random picture of something normal. He puts on his backpack, and he goes to school every day. He’s just a normal kid in that sense. So even though we have all this other stuff, like a big part of my experience, is just like constantly, like I can’t even believe. It just kind of blows my mind…Just normal kid stuff that he’s able to do (Figure 2B).—P7 |
FIGURE 2.
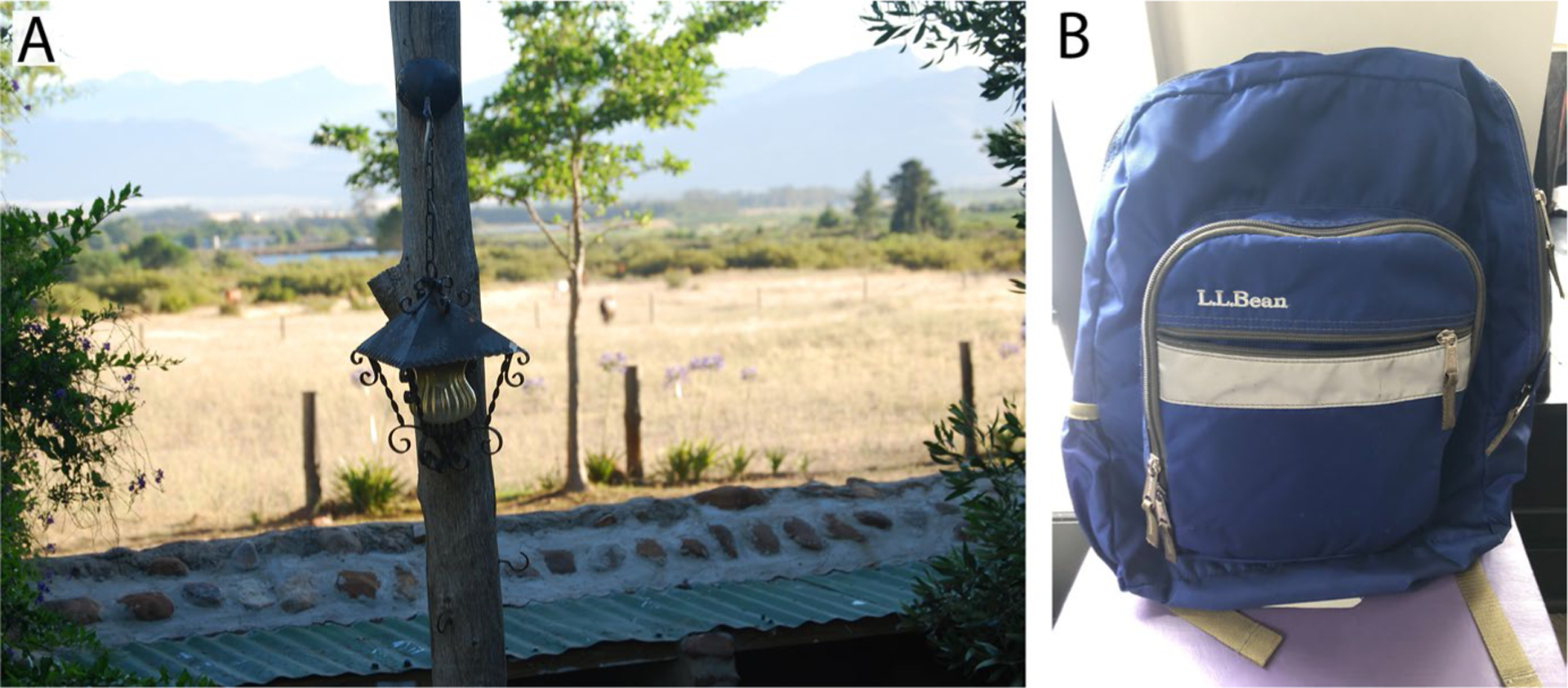
Images of sensemaking: A) The light is out. Image source: T5; B) Normal life. Image source: P7
3.2.2 |. New normal
Over time, as patients and families become more experienced, they become more comfortable with uncertainty. When asked about how he handles the fear of upcoming surgeries, T7, one of our younger participants stated: “I’ve had a lot of surgeries, and I’ve kind of experienced a lot, so yeah.” These lived experiences often help patients and families transition from a state of worry to one of confidence, as they learn how to process and contextualize risk (Figure 2B). This transition is important for clinicians to understand because it can help to explain changes in patient/provider communication. As a patient’s ability to process uncertainty matures, they begin to pay attention to (and report to medical professionals) different types of symptoms, for better or worse. For many of our participants, sensemaking did not just mark the beginning of their transplant journey but also helped them to define normal life after a kidney transplant, including setting realistic expectations for the future. In fact, as our participants became more confident in their abilities, they even recognized their own expertise, which they saw as an opportunity to help others engage in their individual sensemaking process. Our participants wanted to provide advice to their peers on a variety of topics including how to handle an upcoming surgery, taking medications, or even just learning how to talk with their friends about their experiences. A key part of this normalization process is to gather data from others who have also had a kidney transplant, which puts one’s own experiences in the context of the range of experiences after a kidney transplant. When experiences are shared, it is an opportunity to cultivate both empathy and gratitude.
3.3 |. Transitions and agency
3.3.1 |. Shifting responsibilities
Pediatric patients will eventually become responsible for their own care. However, children still have a complicated relationship with their adult caregivers as families continually negotiate evolving roles and responsibilities (Table 4). While some patient participants exhibited a high level of involvement and responsibility regarding their health, some transplant participant’s parents noted that their children had not yet developed high levels of self-efficacy or agency. This recognition often led to substantial concerns about whether a child was well-prepared to self-manage their conditions in the future.
TABLE 4.
Transitions and agency quotes
| Factors | Examples |
|---|---|
| Shifting responsibilities | Because I’m not sick anymore. I can do things by myself and I don’t need to be watched all the time. That’s one thing I hate about school is that there’s teacher help in some classes and they always feel the need to watch me personally. I just hate that, you know. It just bothers me because I can do things by myself and yet they don’t seem to understand that. (Figure 3)—T3 |
| I do have concerns because learning for him has always been an issue, and of course I worry about how he’s going to take care of himself in the future and everything, but I don’t think that’s any different than how I feel about my other kids.—P3 | |
| Assessing adherence | Because I hate it when he’s taking his last dose, and all of a sudden, “I need these this afternoon.” That is a little frustrating for me. I don’t like that. I like a few days ahead. [Fortunately,] it hasn’t happened for a long time. He’s gotten a lot better.—P3 |
| I’ll beat myself up over it. Or my mom isn’t, she’s the best mom on the planet, but like my mom is like, “You need to do better.” And that doesn’t help because I know I need to do better. But there’s certain things that people say about, that my mom says or there’s certain things that I say to myself that I know isn’t positive. I know isn’t the best thing to say, but sometimes I feel like I need to say them to myself.… You feel like you’re the reason that you have this. I’m not taking care of my kidney, not doing this right, I’m not trying.—T5 |
3.3.2 |. Assessing adherence
For some participants, visiting the doctor and seeing monthly laboratory results validated how well they had been following their treatment plan (Figure 3). When results came back showing negative, unexpected findings, some participants described feeling guilty and a decreased sense of self-efficacy. While many adult caregivers described daily concerns about adherence over the long term, parents like P3 recognized that, despite needing to keep close tabs in the past, her child had become more responsible over the past few months. After long periods of hyper-scrutiny and close monitoring, for some caregivers it was particularly challenging to recognize a youth’s increasing maturity and growing capacity for independence. This transition was often accompanied by periods of some uncertainty when adults gave youth the opportunity to try (and sometimes fail) to adhere to medical routines on their own. Rather than reaching out to clinicians for help in increasing self-efficacy, reasons for lapses in adherence were not fully shared during office visits when feelings of shame and failure were prevalent.
FIGURE 3.
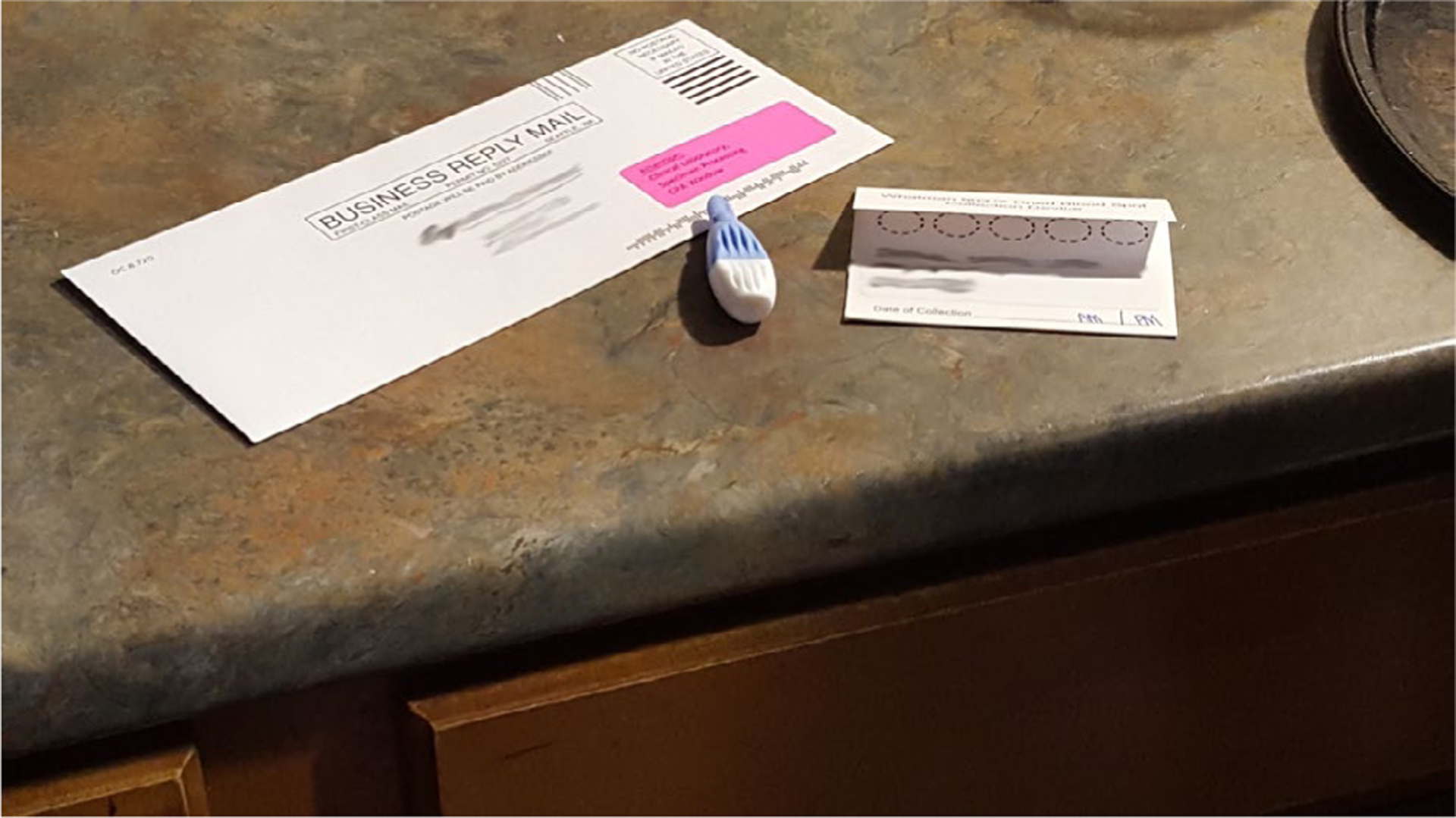
Image of transitions and agency: Home lab testing kit. Image source: T3
3.4 |. Social interaction, community engagement, and support
During certain periods of time, kidney disease, transplant, and recovery overtake daily life for patients, caregivers, and close family and friends (Table 5). Many participants discussed the value of physical and emotional support provided by family members to help overcome these challenges. For example, parents described keeping their child’s medications in a central and highly visible location in the house, facilitating shared accountability and responsibility across the family (Figure 4). However, our participants recognized that the impacts of receiving a transplant extend beyond the patient, also affecting their parents, siblings, and extended family as well as their friends and community. Even our youngest participants expressed guilt knowing their siblings received less attention or missed out on important social events due to urgent or even planned healthcare needs related to the transplant.
TABLE 5.
Social interaction and community engagement
| Factors | Examples |
|---|---|
| Social supports | Without my family, I think I’d be very alone on it. I sometimes will get a little tired of them always reminding me about stuff, but I know that they only do it because they want me to know that it’s important and they want to remind me how important it all is. It does feel great having all the support.—T3 |
| When a child is diagnosed with kidney failure, I mean it doesn’t just affect that child. It affects the parents, the siblings, everybody. It doesn’t just… It’s not just his life unless he was an only child, but it would still be his parents. Involved in that. We have a whole group and we have four, and a grandchild…So, yeah it’s just a family thing.—P3 | |
| Next to the eating area is our computer desk. There’s a lot that happens there. Homework, family meals. I would say we’re together the most in that area of the house. And there’s accountability with that, too, ‘cause everyone knows where her pillbox is and it’s in an area where we are a frequent team, so other people can look at it and see. It’s not tucked away somewhere. It’s where you can see the pills are still in there or not. (Figure 4)—P8 | |
| Well, when I was in the hospital I didn’t get to see my sister that much…She got the least amount of time with mom and dad. I feel kind of bad that she didn’t really get to see me when I was a baby. [She felt] pretty left out and excluded.—T14 | |
| Just, you know, [people] kind of being too tender around me and not knowing what to say or how to act. And I could tell, I mean, I could tell when someone was acting different to me…I had siblings and close, close family friends. Like they’re my second parents and you know, and they were very supportive of me. So it’s not like I didn’t feel supported, but I felt almost too supported, if that makes sense, Which isn’t anyone’s fault. It’s just how I reacted at the time. And I was growing up with that too. And I was kind of figuring out my place in the world and where I stand and who I am.—T13.2 |
FIGURE 4.

Image of community and social engagement. Medications in the kitchen. Image source: P8
Many of the participants talked about the ways that social engagement led to feelings of support from their community as well as times when they felt ostracized or fragile because of their illness. For example, a pair of siblings (T13.1 and T13.2) within our participant group, both of whom had a kidney transplant, offered distinctly different descriptions of the role that family and peer groups played in providing social support. One sibling felt seen and validated. The other described feeling alienated and lonely. Another patient described feeling frustrated about being treated differently and held at a distance by others while simultaneously feeling a bit smothered by close family and friends. These descriptions reflect social and emotional tensions experienced by many children as they mature into young adults, not just kidney transplant recipients.
3.5 |. Reflecting on the PE experience
Universally, all participants found value and enjoyed engaging in the PE process. PE allowed our participants to reflect on their experiences after transplant providing novel insights about their post-transplant journey. In addition to supporting personal reflection, our participants found that the PE experience helped them communicate and express feelings that had previously been challenging: “I think it really helped me kind of process how I’ve been different, and how I’m learning everything, to be able to put it into pictures without words.”—T13.1
In addition to the personal benefits provided by PE, our participants also felt that it could provide additional information that would be useful for their clinicians. Specifically, PE could give more insight into the lived experiences which may influence the clinical components traditionally discussed during a clinical encounter: “I don’t think we ever really talk about a lot of the outside stuff very often. So it’d be an interesting exercise to talk about.”—P11. In addition, we learned that T7 likes to use his old medical devices, such as face masks or feeding tubes, as water toys. T14 has a reading nook in his room that he shares with his brother. P3 stops at the same coffee stand each day to chat with the barista in addition to getting her coffee. These revelations could be used as patient motivators or even solutions to overcome different challenges that patients and families might encounter.
4 |. DISCUSSION
The results of our study show how photograph elicitation provides insight into the complex interactions, decisions, and challenges patients living with kidney disease experience. Photographs have long played an important role in clinical medicine, traditionally serving three primary functions: education, publication, and documentation in the health record.21 Our work demonstrates that patient-generated photographs have the ability to communicate more than just physical symptoms.22,23 They can also provide the clinical care team with an opportunity to see and get a feeling for the wholistic lived experience of families after a kidney transplant, and just as important, how these experiences influence adherence and self-management.
Our results provide multiple examples of how the details of small everyday struggles provide clinicians with the opportunity to tease out subtle obstacles which prevent treatment plan adherence, which typically do not surface during routine clinical encounters. Providing patients with opportunities to share their experiences through photographs led to insights regarding breakdowns in self-management practices not previously identified. Ultimately, this can enable the clinical care team to provide support and/or additional interventions to address these previously unrecognized challenges and barriers which affect allograft longevity and overall quality of life.
PE surfaced a spectrum of factors known to influence self-management practices of chronic pediatric conditions components, including individual and family behaviors, healthcare system practices, and community influences.24 For example, our participants described significant individual stressors, not to mention potential psychiatric illness they experienced after transplant, both known to interfere with adherence.25,26 In addition, PE led to discussions about the ways in which individual social networks influenced the self-management behaviors of our participants. These social influences play a significant role among adolescents managing a chronic illness in both positive27–29 and negative30,31 ways. Finally, with evidence linking physician depersonalization to negative health outcomes32 and patient perceived quality,33 PE has the potential to strengthen the patient-clinician relationship to positively influence the role clinical practice environments play in self-management.
Improving adherence to prescribed medical regimens is a key goal for self-management intervention. Gains in this area are likely to play a significant role in increasing graft survival for adolescent kidney transplant recipients. Existing formal barrier assessment tools have shown success identifying individuals at risk for or exhibiting non-adherence.34 These tools assess known and frequent causes of non-adherence such as forgetting, lack of medicine availability, interfering with activity, poor taste, or difficulty swallowing.
Our experience with PE not only produced insights regarding medication adherence, but also identified more nuanced and individualized challenges unlikely to be discovered through routine barrier assessments, but nevertheless could result in clinically meaningful non-adherence. For example, P14s photograph of her son’s broken tooth led to a conversation about fear and guilt she experienced as a result of the treatments he receives. These concerns may make her question the role of his medications. Recognizing these fears would allow the physician to engage in a more in-depth conversation about the role of each medication, their side effects, and then consider, with the family, how best to move forward. Ultimately, PE helps physicians answer recurring questions, such as why can’t patients just take their medicine, get their labs, show up on time, or follow through with the agreed upon plan? PE shows that these tasks are not necessarily as simple as they may seem, and there are in fact many barriers that get in the way of seemingly straightforward tasks.
In addition to providing more information to clinicians, PE encouraged individuals to reflect on their own experiences, helping them recognize patterns as well as their personal growth since transplant. PE therefore supported individual sensemaking, which is key to successful self-management.35 Sensemaking is the process by which individuals try to understand new situations and place them or define them within the context of previously known examples or experiences.36 PE can support sensemaking by providing individuals the opportunity to look at a new situation and allow for analysis, exploration, and explanation to support decision-making, a key outcome for sensemaking and self-management.37 In addition, PE can help individuals overcome gaps in understanding or even misunderstandings, through “teachable moments”38 when sharing photographs with others who have more experience or expertise, something very common for children and adolescents who encounter new situations.
Not only did PE uncover self-management barriers, it also provided information about patients’ interests and passions, topics that might not normally get discussed in a routine conversation. These insights allow physicians to share in these experiences and see their patients as holistic individuals, where kidney disease is just one part of who they are. Ultimately, the conversations and narratives that accompany the photographs enrich the patient/clinician relationship by fostering empathy which, in turn, supports the collaboration that needs to occur to ensure patients experience life to their fullest potential.
Adding PE to routine transplant clinical encounters can provide many benefits for a range of stakeholders and can be accomplished in a variety of different ways. For example, a clinician could simply ask patients and or families to share a photograph that addresses a specific prompt such as “Choose a photograph that would help you tell your transplant story to someone” or “Choose a photograph that will help me better understand a struggle or challenge you encounter frequently.” More systematically, transplant programs could set up the infrastructure to both distribute prompts (eg, calling families prior to the visit) as well as collect the photographs. This latter approach will likely provide the time required to support a more deliberative and reflective process. Fortunately, the technical requirements of engaging in PE are very flexible, ranging from print outs to digital images. In most instances, a general introduction to the topic and procedures are enough for both patients and clinicians to begin using PE to enhance communication. In contexts involving trauma or serious mental illness, we recommend more extensive training.
4.1 |. Limitations and future work
As with many qualitative studies with vulnerable populations, this work is limited by a relatively small sample size. However, our goal was to establish evidence for the potential of PE in this context. Future work will focus on the ways in which clinical practices related to learning and appreciating patient narratives can help define specific requirements for integrating patient photographs into structured HIT systems. This integration will be key to better understanding the potential for PE to influence clinical outcomes such as adherence, rejection events, or even allograft function. In addition, we would like to assess its impact on self-efficacy and quality of life measures. Therefore, we are currently in the planning phase to develop a pilot PE program at our institution to assess the impact of PE more systematically on these outcomes.
4.2 |. Conclusion
PE has the ability to help clinical providers gain a rich and nuanced understanding of the daily lives and experiences of their patients outside the clinical setting. Our analysis revealed otherwise opaque connections between treatment outcomes, sensemaking practices, social dynamics, and impacts of health-related transitions. We see PE as a potential intervention to first uncover and then address modifiable risk factors which interfere with successful self-management behaviors and ultimately improve graft survival and health-related quality of life for pediatric kidney transplant recipients.
ACKNOWLEDGMENTS
We would like to thank Dr. Jodi Smith for her thoughtful feedback and guidance on this work as well as all of our participants who provided their time. In addition, we would like to thank the Improving Renal Outcome Collaborative for supporting this work by providing the research team access to additional potential participants. Funding was provided by the National Institute of Health NIDDK grant # K23 DK117017.
Abbreviations:
- CEW
Community engagement workgroup
- ESRD
end-stage renal disease
- IROC
Improving Renal Outcomes Collaborative
- PE
Photograph elicitation
REFERENCES
- 1.Curtin RB, Mapes D, Schatell D, Burrows-Hudson S. Self-management in patients with end stage renal disease: exploring domains and dimensions. Nephrol Nurs J J Am Nephrol Nurses Assoc. 2005;32(4):389. [PubMed] [Google Scholar]
- 2.Thomas-Hawkins C, Zazworsky D. Self-management of chronic kidney disease: patients shoulder the responsibility for day-to-day management of chronic illness. How can nurses support their autonomy? Am J Nurs. 2005;105(10):40. [DOI] [PubMed] [Google Scholar]
- 3.Blowey DL, Hébert D, Arbus GS, Pool R, Korus M, Koren G. Compliance with cyclosporine in adolescent renal transplant recipients. Pediatr Nephrol. 1997;11(5):547–551. [DOI] [PubMed] [Google Scholar]
- 4.Pinsky BW, Takemoto SK, Lentine KL, Burroughs TE, Schnitzler MA, Salvalaggio PR. Transplant outcomes and economic costs associated with patient noncompliance to immunosuppression. Am J Transplant. 2009;9(11):2597–2606. [DOI] [PubMed] [Google Scholar]
- 5.Sellarés J, De Freitas DG, Mengel M, et al. Understanding the causes of kidney transplant failure: the dominant role of antibody-mediated rejection and nonadherence. Am J Transplant. 2012;12(2):388–399. [DOI] [PubMed] [Google Scholar]
- 6.Spivey CA, Chisholm-Burns MA, Damadzadeh B, Billheimer D. Determining the effect of immunosuppressant adherence on graft failure risk among renal transplant recipients. Clin Transplant. 2014;28(1):96–104. [DOI] [PubMed] [Google Scholar]
- 7.De Bleser L, Matteson M, Dobbels F, Russell C, De Geest S. Interventions to improve medication-adherence after transplantation: a systematic review. Transpl Int. 2009;22(8):780–797. [DOI] [PubMed] [Google Scholar]
- 8.Dobbels F, Ruppar T, De Geest S, Decorte A, Van Damme-Lombaerts R, Fine RN. Adherence to the immunosuppressive regimen in pediatric kidney transplant recipients: A systematic review. Pediatr Transplant. 2010;14(5):603–613. [DOI] [PubMed] [Google Scholar]
- 9.Jarzembowski T, John E, Panaro F, et al. Impact of non-compliance on outcome after pediatric kidney transplantation: An analysis in racial subgroups. Pediatr Transplant. 2004;8(4):367–371. [DOI] [PubMed] [Google Scholar]
- 10.Nevins TE, Thomas W. Quantitative patterns of azathioprine adherence after renal transplantation. Transplantation. 2009;87(5):711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simons LE, Gilleland J, Blount RL, Amaral S, Berg A, Mee LL. Multidimensional Adherence Classification System: Initial development with adolescent transplant recipients. Pediatr Transplant. 2009;13(5):590–598. [DOI] [PubMed] [Google Scholar]
- 12.Dew MA, Dabbs AD, Myaskovsky L, et al. Meta-analysis of medical regimen adherence outcomes in pediatric solid organ transplantation. Transplantation. 2009;88(5):736–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zolnierek KBH, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petre M, Blackwell AF. Mental imagery in program design and visual programming. Int J Hum-Comput Stud. 1999;51:7–30. [Google Scholar]
- 15.Mitchell C Doing Visual Research. Thousand Oaks: Sage. 2011. [Google Scholar]
- 16.Rose G Visual Methodologies: An Introduction to the Interpretation of Visual Materials. Thousand Oaks: Sage Publications; 2007. [Google Scholar]
- 17.MAXQDA | All-In-One Qualitative & Mixed Methods Data Analysis Tool. MAXQDA - The Art of Data Analysis. https://www.maxqda.com/. Accessed April 13, 2020. [Google Scholar]
- 18.Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. Thousand Oaks: SAGE Publications; 2011. [Google Scholar]
- 19.Lazare A, Putnam SM, Lipkin M. Three functions of the medical interview. In: Lipkin Mack, Putnam Samuel M, Lazare Aaron, Gregory Carroll J, Frankel Richard M, eds. The Medical Interview. New York, NY: Springer New York; 1995:3–19.. [Google Scholar]
- 20.Lipkin M, Putnam SM, Lazare A, Carroll JG, Frankel RM. The Medical Interview: Clinical Care, Education, and Research. Berlin: Springer; 1995. [Google Scholar]
- 21.Wiedemann LA. Using clinical photos in EHRs. J AHIMA. 2010;81(4):44–45. [PubMed] [Google Scholar]
- 22.Evans HL, Lober WB. A Pilot Use of Patient-Generated Wound Data to Improve Post-discharge Surgical Site Infection Monitoring. JAMA Surg. 2017;152(6):595–596. [DOI] [PubMed] [Google Scholar]
- 23.Sanger PC, Simianu VV, Gaskill CE, et al. Diagnosing surgical site infection using wound photography: a scenario-based study. J Am Coll Surg. 2017;224(1):8–15. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Modi AC, Pai AL, Hommel KA, et al. Pediatric self-management: a framework for research, practice, and policy. Pediatrics. 2012;129(2):e473–e485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaw RJ, Palmer L, Blasey C, Sarwal M. A typology of non-adherence in pediatric renal transplant recipients. Pediatr Transplant. 2003;7(6):489–493. [DOI] [PubMed] [Google Scholar]
- 26.Helgeson VS, Escobar O, Siminerio L, Becker D. Relation of stressful life events to metabolic control among adolescents with diabetes: 5-year longitudinal study. Health Psychol. 2010;29(2):153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.La Greca AM, Auslander WF, Greco P, Spetter D, Fisher EB, Santiago JV. I Get by with a little help from my family and friends: adolescents’ support for diabetes care. J Pediatr Psychol. 1995;20(4):449–476. [DOI] [PubMed] [Google Scholar]
- 28.Funck-Brentano I, Dalban C, Veber F, et al. Evaluation of a peer support group therapy for HIV-infected adolescents. AIDS. 2005;19(14):1501–1508. [DOI] [PubMed] [Google Scholar]
- 29.Janicke DM, Gray WN, Kahhan NA, et al. Brief report: the association between peer victimization, prosocial support, and treatment adherence in children and adolescents with inflammatory bowel disease. J Pediatr Psychol. 2009;34(7):769–773. [DOI] [PubMed] [Google Scholar]
- 30.Hains AA, Berlin KS, Hobart Davies W, Smothers MK, Sato AF, Alemzadeh R. Attributions of adolescents with type 1 diabetes related to performing diabetes care around friends and peers: the moderating role of friend support. J Pediatr Psychol. 2007;32(5):561–570. [DOI] [PubMed] [Google Scholar]
- 31.Drew LM, Berg C, Wiebe DJ. The mediating role of extreme peer orientation in the relationships between adolescent–parent relationship and diabetes management. J Fam Psychol. 2010;24(3):299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Halbesleben JRB, Rathert C. Linking physician burnout and patient outcomes: Exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33(1):29–39. [DOI] [PubMed] [Google Scholar]
- 33.Rossberg JI, Melle I, Opjordsmoen S, Friis S. The relationship between staff members’ working conditions and patients’ perceptions of the treatment environment. Int J Soc Psychiatry. 2008;54(5):437–446. [DOI] [PubMed] [Google Scholar]
- 34.Varnell CD Jr, Rich KL, Nichols M, et al. Assessing barriers to adherence in routine clinical care for pediatric kidney transplant patients. Pediatr Transplant. 2017;21(7):e13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lorig KR, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. [DOI] [PubMed] [Google Scholar]
- 36.Weick KE. Sensemaking in Organizations. Thousand Oaks: SAGE; 1995. [Google Scholar]
- 37.Mamykina L, Smaldone AM, Bakken SR. Adopting the sensemaking perspective for chronic disease self-management. J Biomed Inform. 2015;56:406–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–170. [DOI] [PubMed] [Google Scholar]


