Abstract
The objective was to examine trend and care quality outcomes associated with nurse practitioner (NP) involvement in Accountable Care Organizations (ACOs) via a cross-sectional study of 521 Medicare Shared Savings Program ACOs during 2014 to 2016. Data include ACO provider/beneficiary files, Medicare claims, and ACO performance data with a focus on Medicare beneficiaries with diabetes, chronic obstructive pulmonary disease, or heart failure. ACO care quality measures were stratified by NP involvement and adjusted for patient, provider, and ACO factors. NP involvement was highest in larger ACOs, states that allow NPs full scope of practice, and rural areas. Greater involvement was associated with fewer readmissions and higher scores on measures of preventive care but not chronic disease and medication management. Greater NP involvement in ACOs was associated with improvement in some care quality measures. With NPs’ increasing involvement in ACOs, more research is needed to understand the NP role in processes and outcomes of care.
Keywords: nurse practitioners, quality of care, accountable care organizations, Medicare
Team-based care—a collaborative health care model consisting of a diverse group of health professionals—improves health outcomes in primary care settings and reduces hospital readmission rates, emergency department (ED) visits, and cost of care.1 An Accountable Care Organization (ACO) is one such model in which health care professionals coordinate care for patients and share responsibility for total health care costs. Providers are incentivized financially to improve care quality while reducing spending.2 ACOs can have public contracts with Medicare and/or private insurance companies.2 Integrated care is especially needed for Medicare beneficiaries, who tend to be older and to have complex, chronic conditions. Medicare ACOs have expanded across the nation since their establishment in 2011.2 The largest Medicare ACO is the Medicare Shared Savings Program (MSSP) ACO, with 561 organizations as of 2018.3 MSSP ACOs target Medicare Fee-for-Service patients. Legal qualification requires ACOs to have more than 5000 beneficiaries and to sign a contract for at least 3 years.2 To encourage smaller practices and rural providers to participate in ACOs, Medicare created an advance payment model. ACOs in this model receive up-front payments, giving them adequate capital to invest in infrastructure for better care management.2
One challenge to the growth and success of ACOs is the projected shortage of primary care physicians. To address this shortage, nonphysician providers, specifically nurse practitioners (NPs), increasingly serve as primary care providers (PCPs) in various settings.4 NPs are especially suited to provide the care coordination and integration critical to ACOs.5,6 About 80% of NPs, versus 30% of physicians, deliver primary care,4 with a nonsignificant difference in outcomes of primary care for specific chronic conditions (eg, heart failure) with clear-cut clinical practice guidelines.7–9 Some studies show NPs spend more time with patients and provide better continuity of care when compared to PCPs.6 The literature reports that patients of NPs versus PCPs experience fewer hospital admissions, readmissions, and inappropriate ED use.10 However, NPs are more likely to care for less clinically complex patients.11–13
Though prior studies support the association of NPs with improved process and coordination of care in team-based care models,14 it is unclear how the degree of NP participation in ACOs affects not just the process of care but also the quality and outcomes of care between and within ACOs. ACOs provide higher care quality compared to non-ACOs,15 but variations exist in the process and quality of care between and within ACO types.16 To better understand these variations, the research team studied the extent and outcomes of NP involvement in ACOs from 2014 to 2016. The aim was to determine ACO and beneficiary characteristics associated with NP involvement and examine how NP involvement in these ACOs was associated with quality of care. The team focused on beneficiaries with the most common chronic conditions in the Medicare population: diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), or heart failure (HF). These conditions require higher levels of coordinated care and have established guidelines for health care providers to follow. In addition, COPD and HF make up one third of the high-readmission conditions examined in the Hospital Readmissions Reduction Program, a Medicare program implemented to discourage excess readmissions via reducing payments to hospitals.17 A thorough understanding of the impact of NPs on quality of care in ACOs can inform NP scope of practice legislation and guide health care policy decision-making.
Methods
Data Source
Data were from MSSP ACO beneficiary and provider files from 2014 through 2016. Provider files included facilities, clinics, and individual providers participating in ACOs. The master beneficiary summary file, Outpatient Standard Analytical Files, and Medicare Carrier files also were used. The aforementioned data files were located at the Centers for Medicare & Medicaid Services (CMS) Virtual Research Data Center. ACO performance measures and aggregated beneficiary characteristics were obtained from MSSP ACO public-use files (PUFs).18
Study Sample
There were 333, 392, and 432 ACOs enrolled in MSSP in 2014, 2015, and 2016. Two ACOs were excluded because their performance data at ACO PUFs could not be linked to ACO provider files in 2014. Overall, 521 ACOs were enrolled from 2014 through 2016.
Study Outcome: ACO Performance Measures for Quality of Care
ACO performance measures evolved throughout the years. Documentation from each year can be found on the CMS MSSP Program Guidance & Specifications web page.19 The research team focused on 17 measures that fit the scope of the research interest and remained consistent throughout the 3 years (Supplementary Appendix Table A1). The 17 measures were further divided into 5 categories based on ACO domains: patient and caregiver experience, all-condition readmission, preventive care, chronic disease management, and medication management (Supplementary Appendix Table A2).
Main Independent Variable of Interest: PCP Involvement in ACO
PCPs were identified in MSSP ACO provider files using the following CMS provider specialty codes: 01 (general practice), 08 (family practice), 11 (internal medicine), and 38 (geriatric medicine). The physicians included medical doctors (MDs) and doctors of osteopathy; all are referred to as MDs in this article. NPs were selected using specialty code 50 and physician assistants (PAs) using specialty code 97, and later identified in primary care using taxonomy codes listed in Supplementary Appendix Table A3. For each provider, the research team calculated the annual proportion of Medicare claims for Evaluation and Management (E&M) services (Supplementary Appendix Table A4) provided to ACO beneficiaries as the proportion of clinical effort (PCE) to the ACO. For each ACO, all MD PCEs, NP PCEs, and PA PCEs were summed separately and the sums were divided by the total number of beneficiaries in the ACO to estimate their involvement.
E&M invoices for beneficiaries with DM, COPD, or HF were used to estimate provider involvement. The team was not able to estimate PCE for some providers because of a lack of E&M invoices for these patients. The proportion of providers missing the PCE estimate was 8.7%, 10.0%, and 9.3% in 2014, 2015, and 2016, respectively. PCEs for such providers were assumed to be zero. To ensure that provider PCE estimates for these 3 conditions could represent those for all conditions, the team analyzed 100% Medicare claims from 11 states in 2016 and calculated provider involvement for all conditions. The analysis included 11 308 313 Medicare beneficiaries and 24 557 providers across 80 ACOs. Among 25 514 ACO-National Provider Identifier records, the mean value of PCE for beneficiaries with DM, COPD, or HF was larger than the PCE for all beneficiaries (0.47 vs 0.45, P < .001, paired t test). The PCE estimation from 2 different approaches was highly correlated (Pearson correlation coefficients, r = 0.93, P < .001).
Covariates: ACO Characteristics
Initial ACO agreement start year, number of minority patients, total person-years in the performance year, end-stage renal disease person-years in the performance year, and disabled person-years in the performance year were obtained from the MSSP ACO PUFs. ACO state affiliation was from MSSP ACO provider files, which was used along with the 27th, 28th, and 29th Advanced Practice Registered Nurses Annual Legislative Updates to determine NP practicing and prescription authority.20–22 Three levels of state regulation for practice/prescriptions (ie, full authority; full authority, conditional; requiring physician supervision) were defined. ACO inclusion of a critical access hospital (CAH), a rural health center (RHC), or a Federally Qualified Health Center (FQHC) was identified using MSSP ACO provider files. Average age, proportion of male patients, and proportion of dual eligible beneficiaries were estimated from MSSP ACO beneficiary files.
For each year, proportion of beneficiaries with DM, COPD, or HF at each ACO was estimated by linking MSSP ACO beneficiary file to DM, COPD, or HF cohorts. These cohorts were selected from 100% national Medicare data between 2014 and 2016 using chronic condition end-of-year or mid-year indicators from the CMS Chronic Condition Data Warehouse.
The same method was used to estimate PCP PCE for MD specialists as a covariate. The research team selected endocrinology, cardiology, pulmonology, nephrology, and ophthalmology because the focus was on beneficiaries with DM, COPD, or HF.
Statistical Analysis
The research team plotted NP, MD, and PA involvement in ACO by year to show the time trends. The team also presented a map showing NP involvement in ACO by state using data from 2016. For each year, ACOs were categorized into 3 groups based on tertiles of NP involvement in ACOs. Tertiles were used for consistency with prior population-based studies that focused on nurse providers, care coordination, and ACOs.23,24 Differences in ACO characteristics and performance measures were examined among the 3 groups. Association between NP involvement and each ACO characteristic was analyzed using a generalized estimating equation (GEE) model adjusted for year. In these models, NP involvement tertile was the dependent variable and modeled with multinomial distribution and cumulative logit link function. Then, for each of the 5 ACO performance measure domains, the team constructed 3 GEE models to examine the association between NP involvement and ACO performance. In these models, the NP involvement tertile was an independent variable and the ACO performance measure was the dependent variable, modeled with normal distribution and identity link function. Because an ACO could participate in MSSP in multiple years, the team used the first-order autoregressive covariance structure to account for such clustering. A stepwise adjustment was applied to each model in order to gain insight into and remove potential confounders driving differences in quality of care measures among providers. The first model was unadjusted. ACO beneficiary characteristics were added in Mode l2, including average age of benefciiaries, proportions of males, dual eligible beneficiaries, minorities, DM patients, HF patients, and COPD patients; and total number of end-stage renal disease or disabled person-years per 1000 person-years in the ACO. Model 3 included beneficiary characteristics from Model 2 as well as ACO characteristics, including size, involvement in advance payment model, number of years in MSSP, and MD, PA, and specialist involvement. The map was prepared using ArcMap version 10.5.1 (ESRI, Redlands, California). All other analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, North Carolina). All hypothesis tests were 2-sided at a significance level of 0.05.
Results
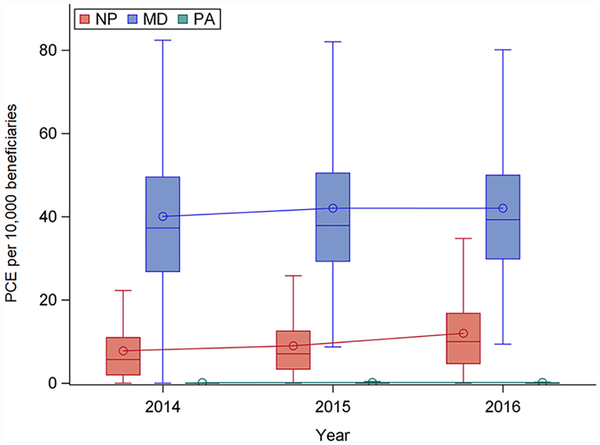
ACOs in MSSPs expanded from 2014 to 2016, especially in rural areas and FQHCs (Table 1). The proportion of ACOs associated with at least 1 CAH or RHC increased from 21.8% in 2014 to 33.1% in 2016. However, ACOs that participated in the advance payment model decreased 6.4% between 2014 and 2016. Following the growth of ACOs, numbers of PCPs involved in ACOs also increased, but at different rates for NPs, MDs, and PAs. As Figure 1 shows, there was a 54% increase in NP PCEs per 10 000 beneficiaries (7.78 ± 7.60 in 2014 to 11.97 ± 9.72 in 2016), a 45% increase in PA PCEs per 10 000 beneficiaries (0.11 ± 0.27 in 2014 to 0.16 ± 0.39 in 2016), and a 5% increase in MD PCEs per 10 000 beneficiaries (40.06 ± 21.57 in 2014 to 42.03 ± 18.76 in 2016).
Table 1.
Characteristics of Medicare Shared Savings Program (MSSP) Accountable Care Organizations (ACOs) by Year.
| ACO characteristic | 2014 (N = 331) | 2015 (N = 392) | 2016 (N = 432) |
|---|---|---|---|
| Number of years in MSSP | |||
| 1 | 119 (36.0) | 89 (22.7) | 100 (23.2) |
| 2 | 101 (30.5) | 112 (28.6) | 85 (19.7) |
| 3 | 111(33.5) | 91 (23.2) | 100 (23.2) |
| 4 | 100 (25.5) | 74 (17.1) | |
| 5 | 73 (16.9) | ||
| ACO size | |||
| ≤ 10 000 beneficiaries | 146 (44.1) | 152 (38.8) | 169 (39.1) |
| 10 001–20 000 beneficiaries | 111 (33.5) | 128 (32.7) | 148 (34.3) |
| >20 000 beneficiaries | 74 (22.4) | 112 (28.6) | 115 (26.6) |
| Regiona | |||
| Midwest | 66 (20.1) | 87 (22.3) | 100 (23.1) |
| Northeast | 68 (20.7) | 86 (22.0) | 86 (19.9) |
| South | 142 (43.2) | 165 (42.2) | 193 (44.7) |
| West | 53 (16.1) | 53 (13.6) | 53 (12.3) |
| State regulation on nurse practitioner practice/prescriptionsa | |||
| Full authorityb | 26 (7.9) | 28 (7.2) | 29 (6.7) |
| Full authority, conditionalc | 22 (6.7) | 45 (11.5) | 59 (13.7) |
| Requiring physician supervisiond | 281 (85.4) | 318 (81.3) | 344 (79.6) |
| Involved in rural health caree | 72 (21.8) | 98 (25.0) | 143 (33.l) |
| Had Federally Qualified Health Center | 58 (17.5) | 76 (19.4) | 94 (21.8) |
| Participate in Advance Payment Model | 35 (10.6) | 33 (8.4) | 18 (4.2) |
Two ACOs from 2014 and 1 ACO from 2015 were located in Puerto Rico.
Full authority denotes that “NPs are regulated by a Board of Nursing (BON) and have full, autonomous practice and prescriptive authority without a requirement or attestation for physician supervision, delegation, consultation, or collaboration.”
Full authority, conditional signifies that “NPs are regulated by a BON and have full autonomous practice and prescriptive authority following a post-licensure/certification period of supervision and/or collaboration.”
Requiring physician supervision indicates that “NPs are regulated by a BON or a combination of BON and Board of Medicine oversight exists; requirement or attestation for physician supervision, delegation, consultation, or collaboration for authority to practice and/or prescriptive authority.”
ACOs with at least 1 critical access hospital or rural health center.
Figure 1.
Proportion of clinical efforts (PCEs) per 10,000 beneficiaries in accountable care organizations by year for primary care nurse practitioner (NP), physician (MD), and physician assistant (PA).
The box represents the interquartile range. The line inside the box represents the median and the circle represents the mean.
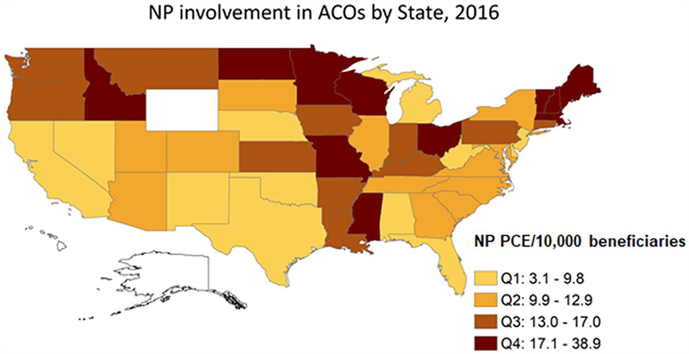
Figure 2 depicts the distribution of NP involvement in ACOs across the United States. Quartiles categorize the degree of NP PCEs per 10 000 beneficiaries. Among 10 states where NPs had full authority in 2016, 8 (80%) had NP involvement greater than the median. In contrast, among 27 states where NPs had restricted authority, 12 (44%) had NP involvement greater than the median.
Figure 2.
Nurse practitioner involvement in accountable care organizations by state.
ACO, accountable care organization; NP, nurse practitioner; PCE, proportion of clinical effort; Q, quarter. The following states had no ACOs enrolled in the Medicare Shared Savings Program in 2016: Alaska, Hawaii, and Wyoming.
Association of ACO characteristics with tertile of NP involvement is shown in Table 2. Compared to ACOs with lower NP involvement, ACOs with higher NP involvement tended to be larger. Within the highest tertile, 40.3% of ACOs had >20 000 beneficiaries compared to 12.8% in the lowest tertile. Greater NP involvement was found in states that provided NPs full authority to practice and prescribe. Among ACOs in the highest tertile, >10% were in states with full practice and prescriptive authority while in the lowest tertile <2% were in such states. Higher NP involvement also was associated with ACOs that provided rural health care (Table 2). More ACOs in the highest tertile had FQHCs. With expansion of NP involvement, MD PCEs also increased (Table 2).
Table 2.
Characteristics of Medicare Shared Savings Program (MSSP) Accountable Care Organizations (ACOs) by Tertilea of Nurse Practitioner (NP) Involvement.
| ACO characteristic | T1, n (%) | T2, n (%) | T3, n (%) | Pb |
|---|---|---|---|---|
| ACO size | ||||
| ≤ 10 000 beneficiaries | 226 (59.0) | 130 (34.0) | 111 (28.5) | <.0001 |
| 10 001–20 000 beneficiaries | 108 (28.2) | 157 (41.1) | 122 (31.3) | |
| >20 000 beneficiaries | 49 (12.8) | 95 (24.9) | 157 (40.3) | |
| Regionc | ||||
| Midwest | 51 (13.4) | 64 (16.8) | 138 (35.4) | <.0001 |
| Northeast | 56 (14.7) | 86 (22.5) | 98 (25.1) | |
| South | 210 (55.3) | 172 (45.0) | 118 (30.3) | |
| West | 63 (16.6) | 60 (15.7) | 36 (9.2) | |
| State regulation on NP practice/prescriptionsc | ||||
| Full authority | 6 (1.6) | 37 (9.7) | 40 (10.3) | .0003 |
| Full authority, conditionald | 28 (7.4) | 48 (12.6) | 50 (12.8) | |
| Requiring physician supervision | 346 (91.1) | 297 (77.7) | 300 (76.9) | |
| Involved in rural health care | 54 (14.1) | 98 (25.7) | 161 (41.3) | <0.0001 |
| Had Federally Qualified Health Center | 45 (11.7) | 65 (17.0) | 118 (30.3) | <0.0001 |
| Participate in Advance Payment Model | 45 (11.7) | 32 (8.4) | 9 (2.3) | 0.0004 |
| Mean ± SD (median) | ||||
| Number of years in MSSP | 2.6 ± 1.2 (3.0) | 2.4 ± 1.2 (2.0) | 2.4 ± 1.2 (2.0) | .2426 |
| Primary care MD PCEs per 10 000 beneficiaries | 33.1 ± 15.2 (31.3) | 38.6 ± 16.5 (36.4) | 52.5 ± 22.2 (48.3) | <.0001 |
| Primary care PA PCEs per 10 000 beneficiaries | 0.0 ± 0.1 (0.0) | 0.1 ± 0.3 (0.0) | 0.3 ± 0.4 (0.0) | .0025 |
| Specialiste PCEs per 10 000 beneficiaries | 2.8 ± 3.6 (1.5) | 4.6 ± 4.7 (4.1) | 8.1 ± 6.2 (7.1) | <.0001 |
| Average age of beneficiaries | 72.1 ± 1.9 (72.4) | 71.7 ± 1.8 (71.9) | 70.5 ± 2.5 (71.0) | <.0001 |
| % Male | 42.3 ± 2.2 (42.3) | 42.6 ± 2.1 (42.6) | 43.0 ± 1.9 (43.0) | .0005 |
| % Dual eligible | 17.5 ± 16.1 (12.1) | 13.6 ± 10.4 (10.7) | 16.5 ± 10.5 (13.9) | .5443 |
| % Minority | 22.6 ± 17.9 (18.4) | 15.3 ± 11.6 (12.6) | 13.6 ± 14.3 (8.5) | <0.0001 |
| % DM | 40.1 ± 9.4 (38.9) | 33.9 ± 7.3 (33.0) | 31.7 ± 5.5 (31.3) | <.0001 |
| % HF | 25.0 ± 6.4 (24.3) | 21.4 ± 5.8 (20.6) | 20.2 ± 4.7 (19.5) | <.0001 |
| % COPD | 24.5 ± 6.5 (23.9) | 22.2 ± 5.9 (21.5) | 21.8 ± 4.9 (21.0) | <.0001 |
| Total number of ESRD/disabled person-years per 1000 person-years | 137.1 ± 59.9 (126.9) | 141.0 ± 65.0 (126.3) | 186.1 ± 84.8 (166.6) | <.0001 |
Abbreviations: COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; ESRD, end-stage renal disease; HF, heart failure; MD, physician; PA, physician assistant; PCE, proportion of clinical effort.
T1, lower tertile; T2, middle tertile; T3, upper tertile. Tertiles were determined by the distribution of NP involvement each year. For 2014, T1: 0.0–3.1, T2: 3.2–9.7, T3: 9.8–49.4. For 2015, T1: 0.0–4.3, T2: 4.4–10.3, T3: 10.4–51.6. For 2016, T1: 0.0–6.0, T2: 6.1–14.4, T3: 14.5–68.2 PCEs per 10 000 beneficiaries in ACO.
The association between NP involvement tertile and each ACO characteristic was analyzed using the generalized estimating equation models adjusted for year with multinomial distribution and cumulative logit link function.
Two ACOs from 2014 and 1 ACO from 2015 were located in Puerto Rico.
Full authority after a period of supervision, collaboration, or mentorship.
Specialists included endocrinologists, cardiologists, pulmonologists, nephrologists, and ophthalmologists.
Beneficiary profiles also varied with tertiles of NP involvement. The highest tertile compared to the lowest one was associated with younger patients, a higher percentage of male individuals, and a lower percentage of minority patients (Table 2). Percentage of patients with chronic conditions, such as DM, HF, or COPD, was lower in the highest tertile compared to the lowest. ACOs with greater NP involvement saw fewer patients with chronic conditions.
Table 3 and Supplementary Appendix Table A5 depict 11 measures analyzed across 5 quality of care domains. All condition readmission rates decreased as NP involvement increased (15.0 ± 0.8 in T1 vs 14.9 ± 0.7 in T2 vs 14.7 ± 0.7 in T3). This association was significant in the unadjusted model (Model 1, P = .0074) and the model adjusted for patient and ACO characteristics (Model 3, P = .0175) but not in the model adjusted for patient characteristics (Model 2, P = .0659). Better preventive care also was associated with greater NP involvement (Table 3). More NP involvement was associated with better chronic disease management. This was significant in Models 1 and 2 (P = .0017, P = .0302). However, when ACO characteristics were added in the model adjustment, the association of NP involvement and chronic disease management was no longer significant. Higher scores on medication management were significantly correlated with more NP involvement in Model 1 but not in Model 2 or Model 3 (Table 3).
Table 3.
Association Between Nurse Practitioner (NP) Involvement and Quality of Care of Accountable Care Organizations (ACOs)a.
| NP PCEs per 10 000 beneficiaries in ACO, tertile | ||||||
|---|---|---|---|---|---|---|
| ACO quality of care measure | T1 | T2 | T3 | P, Model 1 | P, Model 2 | P, Model 3 |
| Mean ± SD (Median) | ||||||
| Patient and caregiver experience | 80.1 ± 1.9 (80.3) | 80.3 ± 1.7 (80.4) | 80.6 ± 1.8 (80.7) | .1800 | .1712 | .3083 |
| Risk standardized, all condition readmission | 15.0 ± 0.8 (15.0) | 14.9 ± 0.7 (14.8) | 14.7 ± 0.7 (14.7) | .0074 | .0659 | .0175 |
| Preventive care | 60.8 ± 14.5 (61.9) | 62.5 ± 13.0 (63.7) | 66.8 ± 10.8 (67.3) | <.0001 | .0045 | .0122 |
| Chronic disease managementb | 73.3 ± 10.9 (75.5) | 75.4 ± 8.4 (76.3) | 76.2 ± 6.3 (77.0) | .0017 | .0302 | .1546 |
| Medication management | 80.7 ± 12.2 (82.9) | 83.3 ± 8.1 (84.6) | 84.7 ± 7.2 (85.4) | <.0001 | .0795 | .3008 |
The bold value indicates P<0.05
Abbreviations: COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; ESRD, end-stage renal disease; HF, heart failure; MD, physician; PA, physician assistant; PCE, proportion of clinical effort; SD, standard deviation.
T1, lower tertile; T2, middle tertile; T3, upper tertile.
Model 1: Unadjusted.
Model 2: Adjusted for ACO beneficiary characteristics (average age of beneficiaries, % male, % dual eligible, % minority, % DM, % HF, % COPD, and total number of ESRD/disabled person-years per 1000 person-years in ACO).
Model 3: Adjusted for ACO beneficiary characteristics and ACO characteristics (size, participate in advance payment model, number of years in MSSP, MD, PA, and specialist involvement).
Average of (100-ACO#27) and ACO#28 was calculated for chronic disease management with higher value for better diabetes and hypertension control.
Discussion
From 2014 to 2016, NP involvement in ACOs grew faster than that of MDs. NP involvement was highest in larger ACOs, in states that allow NPs full authority to practice and prescribe, and in rural areas. Higher NP involvement was associated with lower readmission rates and improved preventive care but noninferior chronic disease and medication management. The finding of greater growth rate of NP PCEs per 10 000 ACO beneficiaries compared to that for MD PCEs is consistent with the national trend. Growth rate in the United States for NPs was 3 to 9 times higher than that of MDs. The rapid growth of NPs in ACOs could reflect a large pool of NP graduates available to hire as PCPs for less cost compared to MDs.25 These results demonstrate that increased NP involvement is concentrated in ACOs located in rural areas and states that allow NPs full authority to practice and prescribe, which is consistent with a prior study.26 Correlation of higher NP involvement with rural participation could be explained by the limited supply of physicians in underserved areas,27 with the shortage being filled by NPs.
In this study, NP involvement was associated with a lower percentage of minority patients, younger patients, and those with fewer chronic conditions. Similarly, several studies found that NPs, compared to MDs, provided care for less clinically complex patients.11,12 NPs could be playing a critical role by seeing healthier patients for annual well visits in order to keep patients attributed to the practice over time. This allocation of less complex patients to NPs has been endorsed by many physician groups.13 However, the perspective of NPs differs. In a survey conducted in the Department of Veterans Affairs, more than 80% of NPs endorsed caring for acutely ill/unstable patients independently and 70% claimed to independently manage medications.28 Although 74.9% of NPs in collaborative clinics believe they practice to the “full extent of their education and training,” only 28.3% of physicians agree that NPs provide services for complex cases.29 Despite controversial perceptions held by different providers, NPs having a less complex patient panel could explain the association with reduced readmission rates found in the present study. The lower readmission rates associated with NP involvement also might reflect shorter wait times to see an NP versus an MD. Though the majority of ill adults prefer a same- or next-day primary care appointment, it takes an average of 19.5 days to see a family practice physician.30 Some health systems (eg, Kaiser Permanente) have addressed long wait times by using NPs as chronic disease case managers, leading to a 30% reduction in time from appointment scheduling to visit date.31 A study found that the presence of NPs not only reduces wait times for primary care appointments but also improves timely access to primary health care services. Because limited access to care increases risk of readmission,32 it is logical that greater NP involvement is associated with lower readmission rates.
The results of improved preventive care under NPs are consistent with previous research.11,33 The literature suggests that nonphysician providers are more likely than physicians to be adherent to practice guidelines.33 The measures for preventive care, such as immunizations and cancer screenings, are derived from guidelines provided by institutions, including the American College of Cardiology, American Heart Association, and American Diabetes Association.34–36 Future studies are needed on the association between guideline adherence and outcomes in the context of multimorbidity and limited life expectancy,37 given published evidence showing the potential harms of applying disease-specific practice guidelines to older adults with multimorbidity.38,39
Limitations
Limitations of this study include the cross-sectional design, which cannot establish causality. The 2014 to 2016 study period may not accurately represent MSSP ACOs today as some of the study variables have changed. There also were differing levels of continued participation of ACOs during the 3 years. ACOs may have started before or ended after the study period. Only 3 common chronic conditions were used to estimate PCE per 10 000 beneficiaries. The proportion of patients with these chronic conditions varied across ACOs (interquartile range in 2016: 43.6% to 52.5%). However, the research team did adjust for the proportions of patients with these conditions in the analyses, and the correlation coefficient between PCE estimated from the 3 diseases and the entire population was very high. Furthermore, the team recognizes that the NP PCE, which was calculated from claims, may be underestimated related to some institutions requiring NPs to bill their services under a supervising physician.40 This could lead to some quality of care measures being incorrectly attributed to physicians rather than NPs. Last, this study focused on ACO-level analysis. More research looking at patient-level analysis could possibly address these limitations.
Conclusion
In summary, greater NP involvement in ACOs was associated with improvement in some care quality measures. These results contribute to the literature on NP involvement in health outcomes and point to future avenues of research into how the increasing involvement of NPs in ACOs affects processes and outcomes of primary care in different settings.
Supplementary Material
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Grants R01-HS020642 from the Agency for Healthcare Research and Quality, and P30-AG024832 and UL1TR001439 from the National Institutes of Health. The sponsors had no role in the design, methods, subject recruitment, data collections, analysis, and preparation of the paper.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Goldberg DG, Beeson T, Kuzel AJ, Love LE, Carver MC. Team-based care: a critical element of primary care practice transformation. Popul Health Manag. 2013;16:150–156. [DOI] [PubMed] [Google Scholar]
- 2.Barnes AJ, Unruh L, Chukmaitov A, van Ginneken E. Accountable care organizations in the USA: types, developments and challenges. Health Policy. 2014;118(1):1–7. [DOI] [PubMed] [Google Scholar]
- 3.Association of American Medical Colleges. CMS issues proposed rule making significant changes to the Medicare shared savings program. Accessed January 8, 2020. https://www.aamc.org/advocacy-policy/washington-highlights/cms-issues-proposed-rule-making-significant-changes-medicare-shared-savings-program [Google Scholar]
- 4.Streeter RA, Zangaro GA, Chattopadhyay A. Perspectives: using results from HRSA’s health workforce simulation model to examine the geography of primary care. Health Serv Res. 2017;52(suppl 1):481–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruggiero K, Pratt P, Antonelli R. Improving outcomes through care coordination: measuring care coordination of nurse practitioners. J Am Assoc Nurse Pract. 2019;31:476–481. [DOI] [PubMed] [Google Scholar]
- 6.Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Aff (Millwood). 2010;29:893–899. [DOI] [PubMed] [Google Scholar]
- 7.Kuo YF, Adhikari D, Eke CG, Goodwin JS, Raji MA. Processes and outcomes of congestive heart failure care by different types of primary care models. J Card Fail. 2018;24(1):9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mundinger MO, Kane RL, Lenz ER, et al. Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA. 2000;283:59–68. [DOI] [PubMed] [Google Scholar]
- 9.Kurtzman ET, Barnow BS. A comparison of nurse practitioners, physician assistants, and primary care physicians’ patterns of practice and quality of care in health centers. Med Care. 2017;55:615–622. [DOI] [PubMed] [Google Scholar]
- 10.Buerhaus P, Perloff J, Clarke S, O’Reilly-Jacob M, Zolotusky G, DesRoches CM. Quality of primary care provided to Medicare beneficiaries by nurse practitioners and physicians. Med Care. 2018;56:484–490. [DOI] [PubMed] [Google Scholar]
- 11.Kuo YF, Goodwin JS, Chen NW, Lwin KK, Baillargeon J, Raji MA. Diabetes mellitus care provided by nurse practitioners vs primary care physicians. J Am Geriatr Soc. 2015;63:1980–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan PA, Abbott DH, McNeil RB, Fisher DA. Characteristics of primary care office visits to nurse practitioners, physician assistants and physicians in United States Veterans Health Administration facilities, 2005 to 2010: a retrospective cross-sectional analysis. Hum Resour Health. 2012;10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCleery E, Christensen V, Peterson K, Humphrey L, Helfand M. VA Evidence synthesis program reports evidence brief: the quality of care provided by advanced practice nurses. In: VA Evidence Synthesis Program Evidence Briefs. US Department of Veterans Affairs; 2011. [PubMed] [Google Scholar]
- 14.Poghosyan L, Norful AA, Martsolf GR. Primary care nurse practitioner practice characteristics: barriers and opportunities for interprofessional teamwork. J Ambul Care Manage. 2017;40:77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borza T, Oerline MK, Skolarus TA, et al. Association between hospital participation in Medicare shared savings program accountable care organizations and readmission following major surgery. Ann Surg. 2019;269:873–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comfort LN, Shortell SM, Rodriguez HP, Colla CH. Medicare accountable care organizations of diverse structures achieve comparable quality and cost performance. Health Serv Res. 2018;53:2303–2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). Accessed June 23, 2019. https://www.cms.gov/medicare/medicarefee-for-service-payment/acuteinpatientpps/readmissionsreduction-program.html [Google Scholar]
- 18.Centers for Medicare & Medicaid Services. Shared Savings Program Accountable Care Organizations (ACO) public-use files. Published 2014–2016. Accessed June 20, 2018. https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/SSPACO/index.html [Google Scholar]
- 19.Centers for Medicare & Medicaid Services. Program guidance and specifications. Accessed June 20, 2018. https://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/sharedsavingsprogram/program-guidance-andspecifications.html#quality-measures
- 20.Phillips S. 27th annual APRN legislative update: advancements continue for APRN practice. Nurse Pract. 2015;40(1):16–42. [DOI] [PubMed] [Google Scholar]
- 21.Phillips S. 28th annual APRN legislative update: advancements continue for APRN practice. Nurse Pract. 2016;41(1):21–48. [DOI] [PubMed] [Google Scholar]
- 22.Phillips S. 29th annual APRN legislative update. Nurse Pract. 2017;42(1):18–46. [DOI] [PubMed] [Google Scholar]
- 23.Murrells T, Ball J, Maben J, Ashworth M, Griffiths P. Nursing consultations and control of diabetes in general practice: a retrospective observational study. Br J Gen Pract. 2015;65:e642–e648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ouayogode MH, Mainor AJ, Meara E, Bynum JPW, Colla CH. Association between care management and outcomes among patients with complex needs in Medicare accountable care organizations. JAMA Netw Open. 2019;2(7):e196939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roblin DW, Howard DH, Becker ER, Kathleen Adams E, Roberts MH. Use of midlevel practitioners to achieve labor cost savings in the primary care practice of an MCO. Health Serv Res. 2004;39:607–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuo YF, Loresto FL Jr, Rounds LR, Goodwin JS. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Aff (Millwood). 2013;32:1236–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gadbois EA, Miller EA, Tyler D, Intrator O. Trends in state regulation of nurse practitioners and physician assistants, 2001 to 2010. Med Care Res Rev. 2015;72:200–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fletcher CE, Copeland LA, Lowery JC, Reeves PJ. Nurse practitioners as primary care providers within the VA. Mil Med. 2011;176:791–797. [DOI] [PubMed] [Google Scholar]
- 29.Donelan K, DesRoches CM, Dittus RS, Buerhaus P. Perspectives of physicians and nurse practitioners on primary care practice. N Engl J Med. 2013;368:1898–1906. [DOI] [PubMed] [Google Scholar]
- 30.Swan M, Ferguson S, Chang A, Larson E, Smaldone A. Quality of primary care by advanced practice nurses: a systematic review. Int J Qual Health Care. 2015;27:396–404. [DOI] [PubMed] [Google Scholar]
- 31.Potts B, Adams R, Spadin M. Sustaining primary care practice: a model to calculate disease burden and adjust panel size. Perm J. 2011;15:53–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warchol SJ, Monestime JP, Mayer RW, Chien WW. Strategies to reduce hospital readmission rates in a non-Medicaid-expansion state. Perspect Health Inf Manag. 2019;16(Summer):1a. [PMC free article] [PubMed] [Google Scholar]
- 33.Ohman-Strickland PA, Orzano AJ, Hudson SV, et al. Quality of diabetes care in family medicine practices: influence of nurse-practitioners and physician’s assistants. Ann Fam Med. 2008;6:14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gc K, Cadet MJ, Hirani S, Thomas T. Type 2 diabetes management: a practice guide for NPs. Nurse Pract. 2018;43(10):40–47. [DOI] [PubMed] [Google Scholar]
- 35.Nishimura R, Otto C, Bonow R, et al. 2014. AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014129:2440–2492. [DOI] [PubMed] [Google Scholar]
- 36.Yancy C, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure. J Am Coll Cardiol. 2013;62(16):e147–e239. [DOI] [PubMed] [Google Scholar]
- 37.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294:716–724. [DOI] [PubMed] [Google Scholar]
- 38.Tinetti ME, Bogardus ST Jr, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351:2870–2874. [DOI] [PubMed] [Google Scholar]
- 39.Boyd CM, McNabney MK, Brandt N, et al. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society expert panel on the care of older adults with multimorbidity. J Am Geriatr Soc. 2012;60(10):E1–E25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buerhaus P, Skinner J, McMichael B, et al. The integrity of MACRA may be undermined by “incident to billing” coding. Published January 8, 2018. Accessed May 10, 2020. 10.1377/hblog20180103.135358/full/ [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.