Abstract
J Clin Hypertens (Greenwich). 2012; 14:396–400. ©2012 Wiley Periodicals, Inc.
Shorter‐interval (6‐hour) ambulatory blood pressure monitoring (ABPM) has been shown to correlate well with 24‐hour ABPM in adults, but this has not been studied in children. The authors selected 131 patients aged 9 to 18 who underwent 24‐ABPM from 2000–2008. Six‐hour intervals beginning at different start times were compared with the daytime and 24‐hour period, with subset analysis for normotensive and hypertensive patients. Concordance correlation coefficients (CCCs) were used to assess for agreement. Among normotensive patients, the mean difference between daytime and 6‐hour intervals ranged from −0.1 mm Hg to 0.0 mm Hg for diastolic blood pressure (DBP) and −1.1 mm Hg to 0.6 mm Hg for systolic blood pressure (SBP) with CCCs of 0.88 to 0.93 for DBP and 0.93 to 0.96 for SBP. For hypertensive patients, mean difference ranged from −0.6 to 1.3 mm Hg for DBP and −0.8 to 1.1 mm Hg for SBP with CCCs of 0.89 to 0.98 for DBP and 0.86 to 0.95 for SBP. Shorter‐interval monitoring correlates significantly with full daytime monitoring in children, allowing for assessment of blood pressure with improved convenience.
Hypertension is one of the leading health care problems in the United States. The incidence of hypertension in children prior to the past decade was 1% to 3%. Recent reports confirm an increase in the average blood pressure (BP) in children with a prevalence of hypertension as high as 4.5% in school‐aged children. 1 Currently, studies evaluating end organ structures demonstrate hypertension as a risk factor for development of left ventricular hypertrophy 2 and carotid artery intimal‐medial thickness. 3
Clinic BP (CBP) is the standard for measuring BP in the office; however, ambulatory BP monitoring (ABPM) is becoming the preferred standard for evaluation of children with suspected hypertension. The indications for use of an ABPM device continue to grow and prompted the American Heart Association (AHA) in 2008 to publish a scientific statement providing guidelines on the use and the interpretation of ABPM in the pediatric population. 4 One indication for ABPM includes identifying children at greater risk for end organ damage. The ABPM results are a stronger predictor of hypertension‐associated target organ damage compared with CBP. 5 , 6 , 7
The 2008 AHA scientific statement outlines utilization of 24‐hour ABPM. Many families may find 24‐hour monitoring too burdensome or too costly. As such, one option is to order a shorter interval of monitoring. To date, nothing in the literature has provided evidence on the efficacy of shorter intervals of monitoring for the diagnosis of hypertension among children. Several studies have evaluated shorter intervals among the adult population. Ernst and colleagues 8 found that 6‐hour monitoring can approximate mean 24‐hour BP results; however, it does not provide information about circadian variations. Graves and colleagues 9 report 6‐hour monitoring as comparable to accurate office measurements without the limitations of poor reproducibility and observer bias. Two older studies 10 , 11 concluded that 3 or 4 readings per hour during a shorter interval correlated with mean daytime pressures by 24‐hour ABPM.
Given the option of 6‐hour ABPM at our institution and the recommendations for the use of 24‐hour monitoring, the evaluation of the concordance between the shorter and longer intervals could provide guidance for clinicians as well as increase power of future research studies on ABPM in children. The aim of this study was to determine whether mean and median systolic BP (SBP) and diastolic BP (DBP) from a 6‐hour daytime interval correlate with statistical significance with the mean and median daytime and 24‐hour SBP and DBP among pediatric patients who have undergone 24‐ABPM.
Methods
The study was approved by the Mayo Clinic’s institutional review board. All patients aged 9 to 18 who underwent 24‐hour ABPM between 2001 and 2008 were identified from a pre‐existing database of all ABPM at the Mayo Clinic. Patients had ABPM testing to assess for hypertension or syncope. Patients who denied access to their medical records for research purposes were excluded. Patients with secondary hypertension were excluded. Patients were not excluded based on medication use.
Data were obtained for a 24‐hour period using the Spacelab monitor 90217 oscillometric monitor (Spacelabs Healthcare, Issaquah, WA). Patients recorded on the monitor the hours in which they were sleeping. Daytime readings were defined as any recording taken while the patient was awake, individualized for each patient depending on their personal time schedule. The 24‐hour ABPM study was considered adequate if fewer than 2 hours passed between successful readings, at least 70 readings were recorded over 24 hours, at least 50 readings during daytime, and at least 10 readings during the nighttime. Fifteen patients were excluded due to inadequate number of readings.
The starting time of the 24‐hour period varied for each patient, between 7 am and 5 pm. For each patient, the BP readings were divided into a total of ten 6‐hour intervals, beginning at 10 different start times (7:00–16:00) during the daytime hours of the 24‐hour period. The 6‐hour intervals were selected from the daytime period because this is when an ABPM can be logistically placed for patients. Each 6‐hour interval of BP readings was utilized for analysis if more than 20 readings were obtained during a consecutive period of 5 to 6 hours. The monitor is programmed to take recordings on average every 10 minutes. Six‐hour intervals were not included if they overlapped between two separate calendar days. For example, for a patient who started monitoring at noon, only 5 of ten 6‐hour intervals constructed on that same day were utilized in the analysis. We did not include the 6‐hour intervals that started after the person awoke the next morning since the monitoring ended at noon. For each patient and each 6‐hour interval, the mean (and median) SBP and DBP readings over that interval were calculated. For comparison, the same summary measures were obtained for each patient’s entire daytime period that the patient indicated they were awake and entire 24‐hour period. Both mean and median (50% BP load) were used because these two criteria are used to establish the diagnosis of hypertension in children based on 24‐hour ABPM. 4
Analyses were performed separately for normotensive and hypertensive patients in order to validate 6‐hour ABPM for both normotensive and hypertensive patients. Hypertension was defined by AHA 2008 guidelines as a mean BP >95th percentile for sex and height based on the 24‐hour ABPM. 4 For each of the ten 6‐hour intervals, the agreement between the measures from the 2 periods (6‐hour interval vs entire 24‐hour period, 6‐hour interval vs awake period) was assessed graphically using the Bland‐Altman method and quantified using the concordance correlation coefficient (CCC). The CCC is a reproducibility index that evaluates the agreement between two measurements by measuring the variation from the concordance line. 12 For example, when the summary measures for a group of patients from their 6‐hour interval starting at 12 pm are plotted in a scatter plot against the summary measures for the same patients from their 24‐hour interval, the 45° reference line in the scatter plot is considered the concordance line. The CCC ranges from 0 to 1; the closer the data fall along the concordance line, the closer the CCC is to 1.
Descriptive statistics were made between the patients’ classification of hypertensive status based on mean BP values by 24‐hour ABPM and mean BP values by 6‐hour ABPM. The classification is based on age, sex, and height according to the 2008 AHA guidelines. 4
Results
In total, 131 patients were included. Of these, 96 were normotensive and 35 were hypertensive. The average age of the patients was 15.7 years (range, 9.6–18.9 years), and 82 (62.6%) were female.
The mean difference between mean DBP readings for the entire daytime period compared with the 6‐hour intervals ranged from −0.1 mm Hg to 0.0 mm Hg among normotensives and from −0.6 to 1.3 mm Hg among hypertensive patients (Table I). The mean difference in mean SBP readings for the entire daytime period compared with the 6‐hour intervals ranged from −1.1 mm Hg to 0.6 mm Hg among normotensives and −0.8 mm Hg to 1.1 mm Hg among hypertensives (Table II).
Table I.
Comparison of Mean Diastolic Blood Pressure From 6‐Hour Intervals vs Daytime and Full 24‐Hour ABPM by Group and Start Time
| 6‐H Start Time | Group | No. | 6‐H Mean (SD) | 6‐H vs Daytime | 6‐H vs 24‐H | ||
|---|---|---|---|---|---|---|---|
| Difference Mean (SD)a | CCC | Difference Mean (SD)a | CCC | ||||
| 7 am | Norm | 20 | 69.1 (6.3) | −0.8 (2.1) | 0.92 | −3.6 (3.0) | 0.70 |
| HTN | 7 | 76.3 (7.9) | −0.1 (2.4) | 0.95 | −4.0 (2.6) | 0.79 | |
| 8 am | Norm | 34 | 70.9 (5.8) | −0.8 (2.5) | 0.88 | −4.2 (3.0) | 0.61 |
| HTN | 11 | 78.2 (9.4) | 0.1 (2.4) | 0.97 | −4.0 (2.6) | 0.86 | |
| 9 am | Norm | 33 | 70.2 (6.1) | −0.8 (2.6) | 0.89 | −4.1 (3.2) | 0.63 |
| HTN | 10 | 77.7 (9.8) | 0.1 (1.8) | 0.98 | −3.7 (2.5) | 0.88 | |
| 10 am | Norm | 40 | 71.7 (6.7) | −1.0 (2.7) | 0.90 | −4.6 (3.2) | 0.65 |
| HTN | 11 | 79.1 (8.2) | 0.0 (2.7) | 0.93 | −4.3 (3.0) | 0.77 | |
| 11 am | Norm | 43 | 71.0 (6.2) | −0.7 (2.6) | 0.90 | −4.0 (3.1) | 0.66 |
| HTN | 15 | 76.7 (7.6) | 1.3 (3.4) | 0.89 | −3.0 (4.1) | 0.77 | |
| 12 pm | Norm | 61 | 70.7 (5.9) | −0.3 (2.5) | 0.90 | −3.7 (3.1) | 0.69 |
| HTN | 23 | 78.6 (7.7) | 0.1 (3.1) | 0.91 | −4.0 (3.5) | 0.77 | |
| 1 pm | Norm | 65 | 71.0 (5.9) | −0.2 (2.5) | 0.90 | −3.7 (3.0) | 0.69 |
| HTN | 26 | 79.1 (7.2) | −0.6 (2.6) | 0.93 | −4.8 (2.7) | 0.74 | |
| 2 pm | Norm | 72 | 70.6 (6.3) | −0.1 (2.4) | 0.93 | −3.6 (2.9) | 0.72 |
| HTN | 29 | 79.0 (7.5) | −0.4 (2.7) | 0.93 | −4.6 (3.2) | 0.73 | |
| 3 pm | Norm | 75 | 70.3 (6.1) | −0.1 (2.5) | 0.91 | −3.5 (3.1) | 0.70 |
| HTN | 29 | 78.9 (8.1) | −0.1 (3.3) | 0.91 | −4.2 (4.1) | 0.72 | |
| 4 pm | Norm | 75 | 70.1 (6.4) | 0.0 (2.5) | 0.91 | −3.6 (3.3) | 0.69 |
| HTN | 28 | 78.0 (9.3) | −0.3 (3.7) | 0.91 | −4.1 (4.3) | 0.78 | |
Abbreviations: ABPM, ambulatory blood pressure monitoring; CCC, concordance class coefficient; HTN, hypertensive group (n=35); Norm, normotensive group (n=96); SD, standard deviation. aDifference=daytime period minus 6‐hour period; full 24‐hour period minus 6‐hour period.
Table II.
Comparison of Mean Systolic Blood Pressure From 6‐Hour Intervals vs Daytime and Full 24‐Hour ABPM by Group and Start Time
| 6‐H Start Time | Group | No. | 6‐H Mean (SD) | 6‐H vs Daytime | 6‐H vs 24‐H | ||
|---|---|---|---|---|---|---|---|
| Difference Mean (SD)a | CCC | Difference Mean (SD)a | CCC | ||||
| 7 am | Norm | 20 | 115.7 (8.0) | 0.6 (2.6) | 0.94 | −1.9 (2.9) | 0.90 |
| HTN | 7 | 139.0 (7.9) | −0.2 (4.3) | 0.86 | −4.7 (4.8) | 0.63 | |
| 8 am | Norm | 34 | 116.9 (7.5) | 0.6 (2.7) | 0.93 | −2.5 (3.2) | 0.85 |
| HTN | 11 | 132.2 (6.5) | 1.1 (3.5) | 0.87 | −2.9 (4.0) | 0.76 | |
| 9 am | Norm | 33 | 116.4 (8.3) | 0.2 (2.7) | 0.94 | −2.7 (3.2) | 0.85 |
| HTN | 10 | 133.0 (6.7) | 0.6 (2.8) | 0.93 | −3.0 (3.5) | 0.81 | |
| 10 am | Norm | 40 | 118.9 (9.0) | 0.3 (2.9) | 0.94 | −3.0 (3.5) | 0.85 |
| HTN | 11 | 130.9 (7.2) | 0.4 (3.0) | 0.91 | −3.8 (3.5) | 0.76 | |
| 11 am | Norm | 43 | 118.9 (8.8) | 0.2 (2.5) | 0.96 | −2.9 (3.2) | 0.87 |
| HTN | 15 | 131.8 (7.4) | 1.7 (3.7) | 0.86 | −2.2 (4.1) | 0.82 | |
| 12 pm | Norm | 61 | 117.8 (8.4) | 0.2 (2.7) | 0.95 | −2.9 (3.3) | 0.86 |
| HTN | 23 | 135.1 (9.7) | 0.0 (3.7) | 0.92 | −4.1 (4.5) | 0.78 | |
| 1 pm | Norm | 65 | 118.4 (8.2) | −0.2 (2.6) | 0.95 | −3.4 (3.2) | 0.84 |
| HTN | 26 | 135.5 (9.9) | −0.4 (3.1) | 0.95 | −4.5 (3.9) | 0.81 | |
| 2 pm | Norm | 72 | 119.1 (9.0) | −0.8 (2.3) | 0.96 | −3.9 (2.8) | 0.85 |
| HTN | 29 | 135.0 (10.4) | −0.7 (3.1) | 0.95 | −4.5 (4.0) | 0.81 | |
| 3 pm | Norm | 75 | 118.9 (8.8) | −0.6 (2.8) | 0.94 | −4.3 (3.0) | 0.82 |
| HTN | 29 | 134.7 (11.4) | −0.5 (4.2) | 0.92 | −4.6 (4.8) | 0.79 | |
| 4 pm | Norm | 75 | 119.1 (8.8) | −1.1 (2.5) | 0.95 | −4.7 (3.0) | 0.80 |
| HTN | 28 | 135.8 (11.3) | −0.8 (3.8) | 0.93 | −5.2 (5.1) | 0.75 | |
Abbreviations: ABPM, ambulatory blood pressure monitoring; CCC, concordance class coefficient; HTN, hypertensive group (n=35); Norm, Normotensive group (n=96); SD, standard deviation. aDifference=daytime period minus 6‐hour period; full 24‐hour period minus 6‐hour period.
Focusing on the median as the criteria of interest, the mean difference between the median DBP readings for the entire daytime period compared with the 6‐hour intervals ranged from −0.9 mm Hg to 0.08 mm Hg among normotensives and −0.4 mm Hg to 1.8 mm Hg among hypertensive patients (data not shown). Similarly, the mean difference in median SBP readings ranged from −1.3 mm Hg to 0.6 mm Hg among normotensives and −1.7 mm Hg to 1.5 mm Hg among hypertensives (data not shown).
The CCC was used to assess the concordance between the criteria estimated from the 6‐hour intervals and from the daytime period. For mean DBP, the CCC values ranged from 0.88 to 0.93 among normotensives and 0.89 to 0.98 for hypertensives (Table I). The CCC for mean SBP varied from 0.93 to 0.96 among normotensive patients and 0.86 to 0.95 among hypertensive patients. A representative Bland‐Altman plot demonstrating concordance between the 6‐hour period starting at 12 pm and the entire daytime period are shown in 1, 2, for normotensive and hypertensive patients, respectively.
Figure 1.
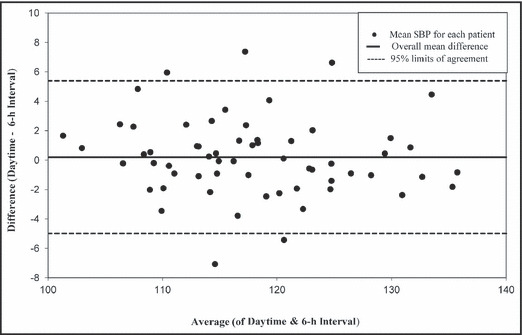
Bland‐Altman plot of mean systolic blood pressure (SBP) among normotensive patients for interval starting at 12 pm.
Figure 2.
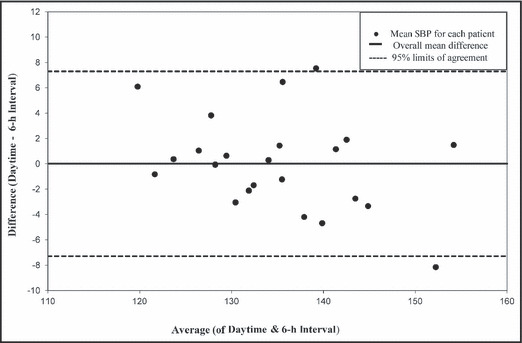
Bland‐Altman plot of mean systolic blood pressure (SBP) among hypertensive patients for interval starting at 12 pm.
The CCC values for median DBP ranges from 0.87 to 0.93 for normotensives and 0.86 to 0.98 for hypertensives. The CCC values for median SBP ranges from 0.94 to 0.96 for normotensives and 0.82 to 0.96 for hypertensives (data not shown).
Comparisons were also made between each 6‐hour interval and the entire 24‐hour period (I, II). The mean differences compared with the full 24‐hour period were greater than those compared with the daytime period. The corresponding CCCs were also lower.
A total of 25 patients were misclassified when solely using 6‐hour ABPM results to identify hypertension when compared with the patients’ 24‐hour ABPM. Ten patients who were diagnosed with hypertension only by loss of nocturnal dipping on the 24‐hour ABPM were normotensive on 6‐hour ABPM. Nine additional patients who were classified as hypertensive on the 24‐hour ABPM based on daytime readings were normotensive on at least one of their 6‐hour intervals. This discrepancy was found only in the mean systolic component, with a mean difference between 95% daytime systolic cutoff value 4 and mean 6‐hour SBP of 4.3 mm Hg (±0.9 standard deviation). Six patients were diagnosed as normotensive on the 24‐hour ABPM but hypertensive on at least one of their 6‐hour ABPM intervals. Of these, 3 patients were misclassified based on diastolic readings, with a mean difference of 2.1 mm Hg (±0.6), and 3 subjects based on systolic readings, with a mean difference of 5.2 mm Hg (±0.8).
Discussion
In a climate of increasing medical costs, clinicians must consider the necessity of every test and choose a test that provides the needed information for the least expense. Additionally, compliance for a 24‐hour period may be difficult for certain pediatric patients. Shorter‐interval ABPM has been recognized in the adult literature as comparable to full 24‐hour monitoring. At the authors’ institution, both types of monitoring are available on the electronic ordering system. When given this choice, clinicians at this institution have ordered 6‐hour studies nearly 50% of the time for pediatric patients. The overall cost for the shorter interval of monitoring is approximately one third that of a 24‐hour interval of monitoring.
The results of this study demonstrate that a strong correlation exists in the pediatric population similar to that previously found among adults. In fact, Ernst and colleagues 8 found adjusted correlation coefficients of 0.83 for systolic pressures from 6‐hour intervals in adults, lower than the results for some intervals in this study. Strong CCCs for 6‐hour periods when compared with all daytime readings suggest that 6‐hour ABPM may be a valid alternative to longer‐term monitoring for diagnosing daytime hypertension in the pediatric population as well.
Six‐hour readings, however, generally take place during the day and fail to capture abnormal nocturnal dipping patterns. In this study, as well as studies among adults, the correlation is weaker when the 6‐hour period is compared with the entire 24‐hour period. Our results demonstrate that the 6‐hour ABPM missed the diagnosis of hypertension based on nocturnal dipping in 10 patients. Prior studies have suggested that inappropriate nocturnal dipping has a higher prevalence among patients with some types of secondary hypertension. 4 All of our patients met the definition of essential hypertension based on chart review. If nocturnal hypertension is suspected or needed to guide therapy, then a 24‐hour ABPM would be more appropriate.
Strengths and Limitations
Our study demonstrated that 6‐hour ABPM was able to identify 94% of normotensive patients identified on 24‐hour ABPM results. This could be a cost‐effective tool for assessing patients for whom the clinician has a high suspicion for white‐coat hypertension. However, the 6‐hour ABPM misclassified 54% of our hypertensive patients as having a normal BP. Ten of the 19 patients did not have nocturnal dipping pattern. The remaining 9 patients were misclassified based on at least one of their multiple 6‐hour intervals meeting criteria for being normotensive. This small sample size limits our ability to identify additional caveats behind misclassification. However, for future studies, the use of a different BP load or different start times may be more effective in categorizing patients with hypertension based on the 6‐hour ABPM. Future studies could also allow for exploration of various time intervals to correctly categorize.
This study is limited by its retrospective design and the use of the same data set for comparing 6‐hour intervals with daytime and 24‐hour intervals. Future studies with prospective enrollment could assess 24‐hour measurements compared with various time intervals obtained on separate days. We did exclude patients with secondary forms of hypertension, which may limit the generalizability of our findings.
Conclusions
Prior studies have correlated end organ damage with 24‐hour ABPM results. Future studies correlating shorter ABPM intervals with end organ damage will help define their role in monitoring BP in children.
Disclosures: The authors report no specific funding in relation to this research and no conflicts of interest to disclose.
References
- 1. Sorof JM, Lai D, Turner J, et al. Overweight, ethnicity, and the prevalence of hypertension in school‐aged children. Pediatrics. 2004;113(3 pt 1):475–482. [DOI] [PubMed] [Google Scholar]
- 2. Hanevold C, Waller J, Daniels S, et al. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association. Pediatrics. 2004;113:328–333. [DOI] [PubMed] [Google Scholar]
- 3. Lande MB, Carson NL, Roy J, Meagher CC. Effects of childhood primary hypertension on carotid intima‐media thickness: a matched controlled study. Hypertension. 2006;48:40–44. [DOI] [PubMed] [Google Scholar]
- 4. Urbina E, Alpert B, Flynn J, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433–451. [DOI] [PubMed] [Google Scholar]
- 5. Sorof JM, Portman RJ. White coat hypertension in children with elevated casual blood pressure. J Pediatr. 2000;137:493–497. [DOI] [PubMed] [Google Scholar]
- 6. Belsha CW, Wells TG, McNiece KL, et al. Influence of diurnal blood pressure variations on target organ damage abnormalities in adolescents with mild essential hypertension. Am J Hypertens. 1998;11(4 pt 1):410–417. [DOI] [PubMed] [Google Scholar]
- 7. Sorof JM, Cardwell G, Franco K, Portman RJ. Ambulatory blood pressure and left ventricular mass index in hypertensive children. Hypertension. 2002;39:903–908. [DOI] [PubMed] [Google Scholar]
- 8. Ernst ME, Weber CA, Dawson JD, et al. How well does a shortened time interval characterize results of a full ambulatory blood pressure monitoring session? J Clin Hypertens. 2008;10:431–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Graves JW, Nash CA, Grill DE, et al. Limited (6‐h) ambulatory blood pressure monitoring is a valid replacement for the office blood pressure by trained nurse clinician in the diagnosis of hypertension. Blood Press Monit. 2005;10:169–174. [DOI] [PubMed] [Google Scholar]
- 10. Sheps SG, Bailey KR, Zachariah PK. Short term (six‐hour) ambulatory blood pressure monitoring. J Hum Hypertens. 1994;8:873–878. [PubMed] [Google Scholar]
- 11. Chanudet X, Chau NP, Larroque P. Short‐term representatives of daytime and nighttime ambulatory blood pressures. J Hypertens. 1992;10:595–600. [DOI] [PubMed] [Google Scholar]
- 12. Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–268. [PubMed] [Google Scholar]


