Abstract
J Clin Hypertens (Greenwich). 2012;14:828–835. ©2012 Wiley Periodicals, Inc.
Patient inertia is defined as an individual’s failure to take responsibility for proactive lifestyle change and health conditions including hypertension. Generalized and hypertension‐specific patient inertia factors were compared in 110 patients (48% women; 52% African American) from a Forsyth County, NC, emergency department (ED) and 104 community members (79% women; 70% African American) using the patient inertia–facilitated survey Patient Inertia‐36. Statistically, more ED than community participants added salt to food at the table and consumed fast foods 5 to 7 days a week. ED patients agreed less often with health literacy questions about salt and BP. Hypertension associated Patient inertia questions asked of 45 ED and 40 community participants with a personal history of hypertension revealed a statistically higher sense of hopelessness surrounding blood pressure management in ED participants. Past BP control experiences of family members had statistically greater impact on community participants regarding their own BP control. Using a logistic regression model, advancing age and being surveyed in the ED were correlated with hopelessness towards BP control. ED patients make unhealthier diet choices and possess heightened generalized and hypertension‐specific patient inertia including hopelessness towards controlling their BP that increases with age. These factors may contribute to this population’s poor BP control, particularly self‐efficacy barriers.
Hypertension affects 1 in 4 Americans adults, costing $93.5 billion in direct and indirect costs annually. 1 According to the Healthy People 2010 report, only 50% of hypertensive patients surveyed reported that their blood pressure (BP) is controlled. 3 Among other factors, a lack of BP control can result from physician gaps in application of evidence‐based treatment algorithms (ie, clinical inertia), adherence to prescribed medications, gaps in patient individual lifestyle actions, and observance of physician recommendations. 4 , 5 To further evaluate the patient’s role in hypertension management, we developed a novel health paradigm model to examine an individual’s mindset towards perceived lifestyle and BP control barriers. 6 This approach, termed by us as “patient inertia,” is defined as an individual’s failure to take responsibility for proactive change and health conditions. Defined specifically for the hypertension disease state, patient inertia is the failure to assume healthy lifestyle behaviors and to follow physician recommendations contributing to poorly controlled hypertension.
Previous studies have shown that certain factors both improve and limit BP control. Patient behaviors including medication adherence, 7 improved diet and exercise, and weight loss 8 have been shown to be effective in reducing and controlling BP. Psychological distress was found using the Brief Symptom Inventory (BSI) assessment in approximately half of surveyed emergency department (ED) hypertensive patients in our previous patient inertia study. 6 Increases in BSI depression subcategory test scores are associated with lower odds of BP medication compliance. 9 However, perceived self‐efficacy, defined as an individual’s ability to judge their own coping, is associated with self‐management behaviors 10 and plays a role in the success of recovery from myocardial infarction, adherence to preventive health programs, control of smoking cessation relapse, and control of eating and weight. 11 Socioeconomic factors also play a role in declining health and mortality from cardiovascular disease. 12 Chronic diseases such as hypertension and diabetes are risk factors for cardiovascular disease and have long durations and slow progressions. They can carry important psychological and social consequences that demand significant social adjustment because they interfere with life activities. 13 Furthermore, patients may receive sympathy due to their chronic disease or experience consequences including strains on relationships that can result in depression.
External loci of control such as hopelessness are associated with poorer health. 14 , 15 , 16 Previously, we documented internalized hopelessness towards BP control as a key patient inertia factor contributing to lack of protective behavioral lifestyle practices in 61% of Forsyth County, NC ED patients. 6 Numerous physiological effects can simultaneously accompany chronic disease including stress, self‐pity, unwillingness to thrive, and self‐destructive behaviors. 13 These factors could impact a patient’s motivation towards controlling their chronic disease. This could lead to increased patient inertia and contribute to reduced BP control rates as compared with awareness and treatment rates. 3
The objective of the current study was to compare generalized lifestyle and hypertension‐associated patient inertia in the acute medical environment of the Wake Forest University Baptist Medical Center (WFUBMC) ED and the Forsyth County, NC, community. A second study objective was to determine whether hopelessness prevailed outside of the acute ED medical environment.
Methods
A facilitated self‐report survey lasting approximately 15 minutes was conducted via a one‐on‐one interview with study staff members. The survey was completed using a convenience sample of 110 patients from the WFUBMC ED (Forsyth County, NC) and 104 Forsyth County community members. Forsyth community surveys were performed within church, business, and civic organization environments, often during health fairs in these locations. Surveys were given to eligible participants during a 2‐year period beginning in March 2009 and ending in March 2011.
Eligible participants included any English‐speaking individuals (18 years and older) regardless of personal hypertension history status. Eligible patients were invited to participate in a modified patient inertia survey called Patient Inertia‐36. The Patient Inertia‐36 is a condensed version of our previously utilized survey 6 that is more appropriate for use in a community setting due to fewer questions, a shorter completion time, ability to be administered regardless of a hypertension history, and lower participator burden. While the previous version of the Patient Inertia survey 6 was only directed at individuals with a personal history of hypertension, section I of the Patient Inertia‐36 included 17 questions appropriate for all individuals regardless of their hypertension history status. Section II of the Patient Inertia‐36 contained 19 questions that were appropriate only if the person had a personal history of hypertension. Within the ED, 45 of 110 patients surveyed (41%) had a personal history of hypertension. Within the community, 40 of 104 participants surveyed (38%) had a personal history of hypertension.
Due to differences in the survey target audience and based on results from our previous publication, 6 we chose to alter the number and content of the patient inertia questions. A total of 71% Patient Inertia‐36 part I questions and 47% of part II questions were new or altered as compared with our previous study. 6 All questions within the Patient Inertia‐36 were derived from the experience of an accredited hypertension specialist (CMF), a hypertension fellow (JJ), an emergency medicine physician who specializes in cardiovascular disease management (DMC), and a health psychologist (DLM). For items to be included, an expert panel consensus agreement was obtained. Based on the critique of items from the expert panel, the properties of each item are believed to measure the intended subject matter.
Patient Inertia‐36 questions were mostly multiple choice and close‐ended using a 5‐point Likert scale (1, strongly agree; 2, somewhat agree, 3, neutral, 4; somewhat disagree; and 5, strongly disagree) that were combined into a 3‐point Likert scale for analysis purposes. Other questions were yes/no/sometimes, scaled, or fill‐in‐the‐blank. Section II of the Patient Inertia‐36 incorporated a slightly modified four‐item Morisky scale assessing BP medication adherence. 17 The Patient Inertia‐36 survey, project protocols, and consent forms were approved by the WFUBMC institutional review board.
All approached community‐based individuals agreed to participate in the survey. However, several individuals approached in the ED declined participation due to nausea, being tired, disinterest in participating in research, pain, family members not wanting them to participate, and sadness in relation to their health.
De‐identified data were entered into the SAS statistical program (SAS Institute Inc, Cary, NC). Descriptive statistics including frequencies, percentages, means, and standard deviations were calculated as appropriate. Chi‐square was used to compare categorical variables, and nonparametric approach using Wilcoxon rank‐sum test was used for ordinal variables to compare differences between the ED and community. The Student t test was utilized for numerical variables. Logistic regression was employed to determine factors associated with hypertension‐related hopelessness. A P value of <.05 was considered statistically significant.
Results
Demographics: Community vs Emergency Department
There were statistically fewer women (79%, community; 48%, ED), African Americans (70%, community; 52%, ED), and insured individuals (84%, community; 67%, ED) surveyed within the ED as compared with the community. ED participants surveyed were also statistically younger (52±14 years, community; 47±16years, ED). Approximately 70% to 75% of patients in both groups self‐reported a family history of high BP, and 48% to 52% of participants in both groups self‐reported seeing a doctor concerning BP management within the previous 12 months.
Generalized Patient Inertia: Community vs Emergency Department
Food consumption behavior was significantly different between the two groups (Figure 1). Fifteen percent of surveyed ED participants self‐reported eating fast food 5 to 7 days per week while only 4% reported this survey response in the community. Participants in the community differentially eat less fast food than those in the ED (Figure 1). Eighty‐three percent of community participants responded that they eat fast food 0 to 2 days per week while 66% of ED counterparts reported this survey response.
Figure 1.
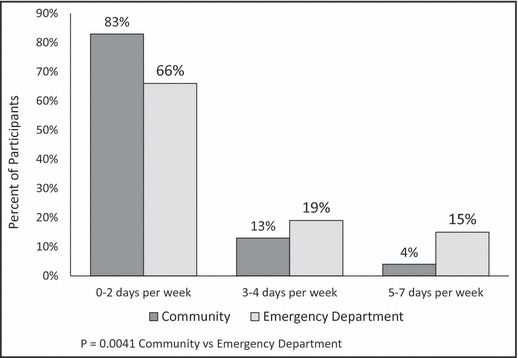
Fast food consumption. A statistical difference in the number of days fast food is eaten between participants in the community and emergency department is shown. There were higher percentages of emergency department participants who ate fast food 5 to 7 days per week as compared with those in the community. There were lower percentages of participants in the emergency department who ate fast food 0 to 2 days per week as compared with those in the community.
Ninety‐one percent of community participants agreed that consuming less salt helps a person control his/her BP while 80% of ED (P<.005) participants agreed with this statement (Figure 2). Participants in the ED added salt to their food at the table more often than do community participants (Figure 3). Forty‐six percent of ED participants reported “yes” or “sometimes” to adding salt to food at the table while 33% of participants reported these responses in the community. There was no difference between the two groups in regards to adding salt while cooking.
Figure 2.
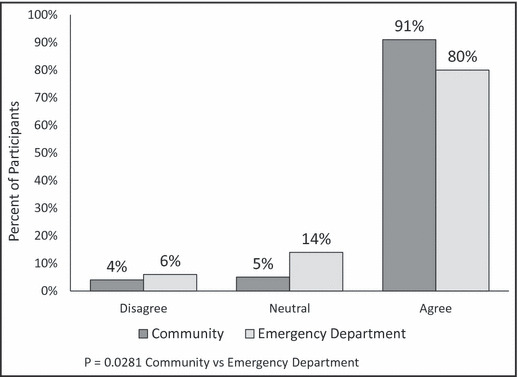
Salt and blood pressure control. Participants in the community and the emergency department had statistically different answers in regards to whether they believed consuming less salt helps one control his/her blood pressure. Fewer emergency department participants agreed with this health literacy statement as compared with those in the community.
Figure 3.
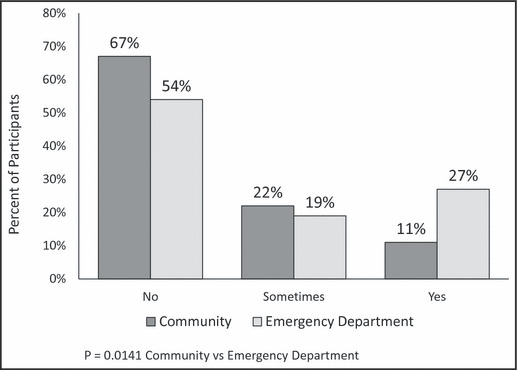
Salting food at the table. Statistically, emergency department participants add salt to their food at the table more often than do community participants.
Participants in both the community and the ED environments reported similar exercise habits, with each group exhibiting almost equal distribution between 0 and 1 times per week (26% community; 38% ED), 2 or 3 times per week (37% community; 29% ED), and ≥4 times per week (38% community; 33% ED). Overwhelmingly, 58% of both groups selected chicken as the meat they purchase most often. Sixty percent to 70% of both groups ate home‐cooked meals 5 to 7 days per week. There were no differences between the groups concerning vegetable and fruit consumption, with 65% to 70% of participants self‐reporting eating vegetables and 48% to 49% reporting eating fruit “frequently” or “always.” Approximately 80% of both groups agreed with the statement that high BP is caused or influenced by the foods one eats.
Hypertension‐Specific Patient Inertia: Community vs ED
Statistically, ED participants with a history of hypertension have a higher sense of hopelessness related to their BP than do hypertensive participants in the community (Figure 4). Thirty‐nine percent of participants in the ED agree with the statement “I will have complications with high BP no matter what I do.” In the community, 71% of the participants disagree with this statement as compared with 38% in the ED. Forty‐seven percent to 53% of participants in both groups thought they could control their BP. While not being significantly different between the two groups, 55% of community participants and 41% of ED participants had spent time thinking about better BP control within the past month.
Figure 4.
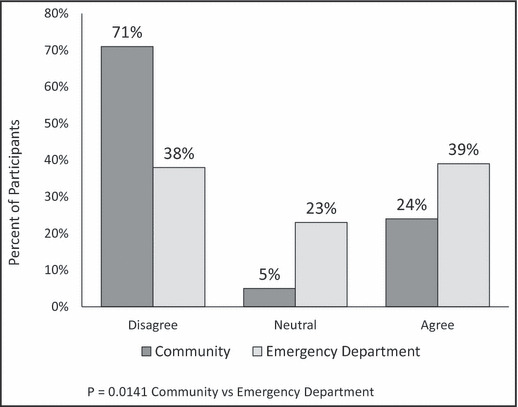
Hopelessness related to blood pressure control. Emergency department patients possess a statistically higher sense of hopelessness related to their blood pressure control than do participants in the community. A higher percentage of emergency department participants agreed with the statement “I will have complications from high blood pressure no matter what I do.” A much greater percentage of community participants disagreed with this statement.
There were more participants in the community who agreed that past experiences of family members affect their thoughts about their own BP management as compared with the ED (36% community; 11% ED) (Figure 5). Seventy‐eight percent of the community and 91% of the ED participants disagreed that past experiences of friends impacted their thoughts about their own BP. The majority of individuals in both groups (63% community; 78% ED) feel they get the emotional support needed from friends and family to assist in controlling their BP. The majority of both groups (80% community; 57% ED) did not feel stressed as a result of their high BP.
Figure 5.
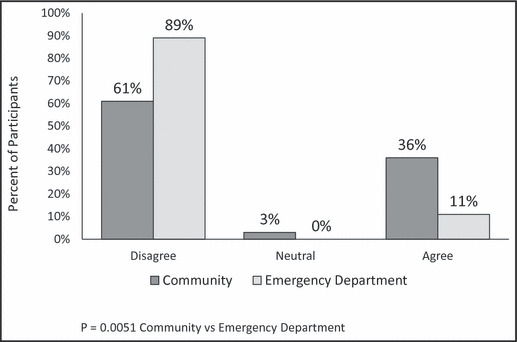
The influence of past experiences of family members on personal blood pressure control. A statistically greater percentage of community members agreed that past experiences of family members affected their thoughts about their own blood pressure management as compared with participants in the emergency department.
BP medication adherence did not differ between the two groups. Forty percent to 45% of participants in both groups self‐reported never forgetting their BP medication. Around 70% (78% community; 67% ED) of participants in both groups did not have difficulty in remembering to take their BP medications. Eighty to 89% of patients continue to take their BP medication when they feel better. One hundred percent of patients in both groups self‐reported continuing to take their BP medication even if they feel worse. Similar percentages of patients in both groups (13% community; 16% ED) stated that finances impact the purchase of BP medications recommended to them. Eighty percent to 82% of participants in both groups were not frustrated with their current BP treatment regimens.
Factors Associated With the Patient Inertia Concept of Hypertension‐Related Hopelessness
A logistic regression analysis was conducted to determine which patient inertia concepts were predictive of hopelessness. The variables included in the model were survey location (community vs ED), race (African American vs non–African American), sex (male vs female), insurance (yes vs no), family history of high BP (yes vs no), and past BP experiences of family members (agree vs neutral/disagree). Location (P= .0118) and age (P=.0237) were the only variables that were independently predictive of hopelessness.
Discussion
For our population, generalized and hypertension‐specific patient inertia differences exist between Forsyth County participants surveyed in a community setting as opposed to those attending a local ED. Our study shows that ED participants possess higher levels of generalized and hypertension‐specific patient inertia as evidenced by higher frequencies of unhealthy lifestyle choices and increased BP‐related hopelessness, respectively.
Increased hopelessness in the ED as compared with the community is consistent with our previous findings where 61% of surveyed ED participants with a history of hypertension exhibited hopelessness. 6 This sense of hopelessness was associated with 50% of participants having some psychological stress caused by somatization, anxiety, and depression. 6 Poor BP control has been previously associated with high levels of hopelessness toward hypertension treatment. 14 Normotensive men reporting high levels of hopelessness at baseline were three times more likely to become hypertensive within 4 years of prospective follow‐up as compared with men who were not hopeless at baseline. 15 Similar results were found in women. 18 Adverse cardiovascular outcomes have been strongly correlated with a sense of hopelessness. 19 Studies by Stern and colleagues 20 and Everson and coworkers 15 suggest that helplessness and/or hopelessness may be more likely than an overall depressive syndrome to be associated with the development of hypertension.
Psychosocial factors and stressors are associated with the development of cardiovascular disease contributing to the development of angina in adult men, 21 increased myocardial infarction risk and nonfatal myocardial infarction in middle‐aged men, 22 and coronary heart disease (CHD) in prehypertensive and hypertensive adults. 23 Longitudinal studies suggest an increased risk of hypertension development in patients who experience anxiety. 24 The mediators and mechanisms underlying the linkage between depression and cardiovascular mortality are yet to be fully established but could include socioeconomic position, ill health, disability, unhealthy behaviors, increased platelet aggregation, and exaggerated cardiovascular reactions to psychological stress exposure. 25 , 26 , 27 , 28 These previous studies, demonstrating the relationship between hopelessness, hypertension, and cardiovascular disease, document the need to understand more fully the disproportionate amount of hopelessness in the Forsyth County ED as compared with the community. It is possible that hopelessness in the ED could be both the cause and the consequence of the ED as the survey location. It could also be the result of poor BP control as suggested in our previous publication, where, on average, participants presenting to the ED had a BP greater than stage 1 hypertension as defined by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC) recommendations. 6 Future studies to better define factors contributing to hopelessness in the ED are warranted.
Multiple factors drive increasing numbers of patients to visit local EDs including age, decreased availability of primary care physicians, and liability concerns leading primary care physicians to refer more patients to the ED. 29 These factors combined with the ED’s reputation of serving as a healthcare safety net suggest the possibility that the type of person being surveyed in the ED may possess distinctive characteristics that differ from those in the larger community. Several studies have shown that psychological distress can affect one’s health perception and health‐seeking behaviors including visiting an ED. 30 , 31 Frequent ED users have typically been defined as poor, heavy users of other parts of the health care system, and dissatisfied with their own care. 32 However, in the current study, no difference was found between the groups in patient satisfaction with current hypertension treatment regimens. This finding was slightly unexpected since ED patients have a slightly lower socioeconomic status as demonstrated by lower prevalence of health insurance. Self‐reported medication adherence may be higher than actual compliance especially due to financial burdens self‐reported by 13% to 16% of participants regardless of survey location. Financial burdens may have a higher impact on medication adherence in the ED due to the population they typically serve. Disparities in medical care may impact the ED population since the ED is perceived as a health care safety net, functioning as the sole provider for uninsured, the poorly insured, and those who find it difficult to navigate the health care system. 33 No studies were found in the literature assessing changes in generalized psychological distress as a result of typical ED presentation outside of needing emergency psychiatric services. 34
Participants surveyed in the ED also self‐reported unhealthier lifestyle choices, including higher salt consumption, and had lower hypertension health literacy. Most of the US population consume >2300 mg/d of sodium mainly due to inexpensive commercial access. 35 , 36 Foods being purchased from fast food restaurants typically contain higher sodium than food prepared at home. 37 Stress has been associated with increased sodium intake in animal models being mediated through heightened sympatho‐adrenal medullary system and/or hypothalamo‐pituitary‐adrenal axis mechanisms. 38 Human studies on acute stress have found no differences in salt intake, 39 , 40 while studies evaluating chronic stress do not yet exist in the literature.
Excess dietary sodium intake leads to a resetting of the renal‐function curve and increased BP. 41 In previous studies, groups consuming a low‐sodium diet reduced systolic BP (SBP) by 6.7 mm Hg and diastolic BP (DBP) by 3.5 mm Hg as compared with the high sodium group counterparts. 42 Among hypertensive patients, BP decreases have been even more substantial. 43 Across a population, reductions in SBP by 5 mm Hg and DBP by 2 mm Hg are estimated to reduce CHD and stroke mortality rates by 6% to 9% and 14% to 15%, respectively. 44 , 45 Reducing salt intake may be one of the most cost‐effective interventions to reduce cardiovascular disease. 46 , 47 Additional studies evaluating differences in salt intake and health literacy as it relates to salt and BP control are warranted in the ED population. If a similar trend was seen in a larger sample size, it could warrant the introduction of a simple campaign to educate patients on the influences of salt on hypertension risk and prevalence that could positively influence hypertension control rates in this population.
When interpreting the study results, one should consider study limitations and strengths including the possibility that: (1) the participants using the ED or community are somehow distinctly different than the other group; (2) participants presenting to the ED or the community locations carry as a result of the environment a different attitude at the time of being surveyed that might influence their responses; (3) use of self‐report questionnaires could skew results because patients may provide responses that they perceive the study staff will view as positive. These results may not be able to be generalized to other populations. Our sample size is relatively small but is large enough to detect relationships and tendencies of behavior among the groups. As a result of the convenience sample being used, there were small demographic differences between the groups. Many of the community surveys were conducted at community health fair locations, which seemed to attract higher numbers of African Americans, women, and senior citizens than other demographic groups influencing the community sample available for this study. Since community health promotion efforts balance health education along with disease screening, it is possible that persons attending such events represent a motivated self‐selected population. Reports on motivation, attitudes, and beliefs have previously indicated that health fair participation provides a sense of control, a statement of safety of one’s health, a review of overall health status, and positive encouragement toward better health. 48
Conclusions
Our study indicates generalized and hypertension‐specific patient inertia differences between individuals in the ED and the community. ED participants exhibit lower health literacy surrounding salt and BP, tend to adopt worse dietary habits including more fast food and higher salt intake, and tend to be more hopeless about their BP management. These study findings warrant further assessment of this new health paradigm patient inertia model. The current data suggest that lifestyle actions and feelings toward chronic disease may have a greater impact on the overall health and BP control of persons presenting to the ED as compared with someone in the generalized community.
Acknowledgments
Acknowledgment: There are no conflicts of interest related to this manuscript. All authors contributed to the intellectual development of this paper. JJ, DMC, DLM, and CMF developed the patient inertia survey. JJ, DMC, and DRS developed the study hypothesis. ARM and JJ performed facilitated surveys and statistical analysis. JJ is supported by the Consortium for Southeastern Hypertension Control (COSEHC), and ARM is supported through a MARC U‐Star T34 training grant provided to Winston‐Salem State University.
References
- 1. Fields LE, Burt VL, Cutler JA, et al. The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension. 2004;44:398–404. [DOI] [PubMed] [Google Scholar]
- 2. Vital signs: prevalence, treatment, and control of hypertension—United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;4:103–108. [PubMed] [Google Scholar]
- 3. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;20:2043–2050. [DOI] [PubMed] [Google Scholar]
- 4. Holland N, Segraves D, Nnadi VO, et al. Identifying barriers to hypertension care: implications for quality improvement initiatives. Dis Manag. 2008;11:71–77. [DOI] [PubMed] [Google Scholar]
- 5. Doroodchi H, Abdolrasulnia M, Foster JA, et al. Knowledge and attitudes of primary care physicians in the management of patients at risk for cardiovascular events. BMC Fam Pract. 2008;9:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Joyner‐Grantham J, Mount DL, McCorkle OD, et al. Self‐reported influences of hopelessness, health literacy, lifestyle action, and patient inertia on blood pressure control in a hypertensive emergency department population. Am J Med Sci. 2009;338:368–372. [DOI] [PubMed] [Google Scholar]
- 7. Hajjar I, Kotchen JM, Kotchen TA. Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health. 2006;27:465–490. [DOI] [PubMed] [Google Scholar]
- 8. Dickinson HO, Mason JM, Nicolson DJ, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–233. [DOI] [PubMed] [Google Scholar]
- 9. Kario K, Schwartz JE, Davidson KW, Pickering TG. Gender differences in associations of diurnal blood pressure variation, awake physical activity, and sleep quality with negative affect: the work site blood pressure study. Hypertension. 2001;38:997–1002. [DOI] [PubMed] [Google Scholar]
- 10. Yoo H, Kim CJ, Jang Y, You MA. Self‐efficacy associated with self‐management behaviours and health status of South Koreans with chronic diseases. Int J Nurs Pract. 2011;17:599–606. [DOI] [PubMed] [Google Scholar]
- 11. O’Leary A. Self‐efficacy and health. Behav Res Ther. 1985;23:437–451. [DOI] [PubMed] [Google Scholar]
- 12. Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. [DOI] [PubMed] [Google Scholar]
- 13. Stanton AL, Revenson TA, Tennen H. Health psychology: psychological adjustment to chronic disease. Annu Rev Psychol. 2007;58:565–592. [DOI] [PubMed] [Google Scholar]
- 14. Jokisalo E, Enlund H, Halonen P, et al. Factors related to poor control of blood pressure with antihypertensive drug therapy. Blood Press. 2003;12:49–55. [PubMed] [Google Scholar]
- 15. Everson SA, Kaplan GA, Goldberg DE, Salonen JT. Hypertension incidence is predicted by high levels of hopelessness in Finnish men. Hypertension. 2000;35:561–567. [DOI] [PubMed] [Google Scholar]
- 16. Meyer D, Leventhal H, Gutmann M. Common‐sense models of illness: the example of hypertension. Health Psychol. 1985;4:115–135. [DOI] [PubMed] [Google Scholar]
- 17. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self‐reported measure of medication adherence. Med Care. 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- 18. Raikkonen K, Matthews KA, Kuller LH. Trajectory of psychological risk and incident hypertension in middle‐aged women. Hypertension. 2001;38:798–802. [PubMed] [Google Scholar]
- 19. Das S, O’Keefe JH. Behavioral cardiology: recognizing and addressing the profound impact of psychosocial stress on cardiovascular health. Curr Hypertens Rep. 2008;10:374–381. [DOI] [PubMed] [Google Scholar]
- 20. Stern SL, Dhanda R, Hazuda HP. Helplessness predicts the development of hypertension in older Mexican and European Americans. J Psychosom Res. 2009;67:333–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Medalie JH, Goldbourt U. Angina pectoris among 10,000 men. II. Psychosocial and other risk factors as evidenced by a multivariate analysis of a five year incidence study. Am J Med. 1976;60:910–921. [DOI] [PubMed] [Google Scholar]
- 22. Kop WJ. Chronic and acute psychological risk factors for clinical manifestations of coronary artery disease. Psychosom Med. 1999;61:476–487. [DOI] [PubMed] [Google Scholar]
- 23. Player MS, King DE, Mainous AG III, Geesey ME. Psychosocial factors and progression from prehypertension to hypertension or coronary heart disease. Ann Fam Med. 2007;5:403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Player MS, Peterson LE. Anxiety disorders, hypertension, and cardiovascular risk: a review. Int J Psychiatry Med. 2011;41:365–377. [DOI] [PubMed] [Google Scholar]
- 25. Wulsin LR, Vaillant GE, Wells VE. A systematic review of the mortality of depression. Psychosom Med. 1999;61:6–17. [DOI] [PubMed] [Google Scholar]
- 26. Mikuni M, Kagaya A, Takahashi K, Meltzer HY. Serotonin but not norepinephrine‐induced calcium mobilization of platelets is enhanced in affective disorders. Psychopharmacology. 1992;106:311–314. [DOI] [PubMed] [Google Scholar]
- 27. Kibler JL, Ma M. Depressive symptoms and cardiovascular reactivity to laboratory behavioral stress. Int J Behav Med. 2004;11:81–87. [DOI] [PubMed] [Google Scholar]
- 28. Phillips AC. Blunted cardiovascular reactivity relates to depression, obesity, and self‐reported health. Biol Psychol. 2011;86:106–113. [DOI] [PubMed] [Google Scholar]
- 29. Newton MF, Keirns CC, Cunningham R, et al. Uninsured adults presenting to US emergency departments: assumptions vs data. JAMA. 2008;16:1914–1924. [DOI] [PubMed] [Google Scholar]
- 30. Sun BC, Burstin HR, Brennan TA. Predictors and outcomes of frequent emergency department users. Acad Emerg Med. 2003;10:320–328. [DOI] [PubMed] [Google Scholar]
- 31. McCusker J, Cardin S, Bellavance F, Belzile E. Return to the emergency department among elders: patterns and predictors. Acad Emerg Med. 2000;7:249–259. [DOI] [PubMed] [Google Scholar]
- 32. Hunt KA, Weber EJ, Showstack JA, et al. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48:1–8. [DOI] [PubMed] [Google Scholar]
- 33. Blanchard JC, Haywood YC, Scott C. Racial and ethnic disparities in health: an emergency medicine perspective. Acad Emerg Med. 2003;10:1289–1293. [DOI] [PubMed] [Google Scholar]
- 34. Nurius PS. Emergency psychiatric services: a study of changing utilization patterns and issues. Int J Psychiatry Med. 1983;13:239–254. [DOI] [PubMed] [Google Scholar]
- 35. The Intersalt Cooperative Group . Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988;297:319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mohan S, Campbell NR. Salt and high blood pressure. Clin Sci (Lond). 2009;117:1–11. [DOI] [PubMed] [Google Scholar]
- 37. Centers for Disease Control and Prevention . Vital signs: food categories contributing the most to sodium consumption – United States, 2007–2008. MMWR Morb Mortal Wkly Rep. 2012;61:92–98. [PubMed] [Google Scholar]
- 38. Torres SJ, Turner AI, Nowson CA. Does stress induce salt intake? Br J Nutr. 2010;103:1562–1568. [DOI] [PubMed] [Google Scholar]
- 39. Oliver G, Wardle J, Gibson EL. Stress and food choice: a laboratory study. Psychosom Med. 2000;62:853–865. [DOI] [PubMed] [Google Scholar]
- 40. Miller SB, Friese M, Dolgoy L, et al. Hostility, sodium consumption, and cardiovascular response to interpersonal stress. Psychosom Med. 1998;60:71–77. [DOI] [PubMed] [Google Scholar]
- 41. Meneton P, Jeunemaitre X, de Wardener HE, MacGregor GA. Links between dietary salt intake, renal salt handling, blood pressure, and cardiovascular diseases. Physiol Rev. 2005;85:679–715. [DOI] [PubMed] [Google Scholar]
- 42. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH‐Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 43. Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens. 2003;17:471–480. [DOI] [PubMed] [Google Scholar]
- 44. The Guidelines Subcommittee of the World Health Organization‐International Society of Hypertension (WHO‐ISH) Mild Hypertension Liaison Committee . 1999 World Health Organization‐International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17:151–183. [PubMed] [Google Scholar]
- 45. Cook NR, Cohen J, Hebert PR, et al. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–709. [PubMed] [Google Scholar]
- 46. Joffres MR, Campbell NR, Manns B, Tu K. Estimate of the benefits of a population‐based reduction in dietary sodium additives on hypertension and its related health care costs in Canada. Can J Cardiol. 2007;23:437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Asaria P, Chisholm D, Mathers C, et al. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–2053. [DOI] [PubMed] [Google Scholar]
- 48. Heath JM, Lucic KS, Hollifield D, Kues JR. The health beliefs of health fair participants. J Community Health. 1991;16:197–203. [DOI] [PubMed] [Google Scholar]


