Abstract
J Clin Hypertens (Greenwich). 2012;14:877–886. ©2012 Wiley Periodicals, Inc.
Multiple barriers can influence adherence to antihypertensive medications. The aim of this systematic review was to determine what adherence barriers were included in each instrument and to describe the psychometric properties of the identified surveys. Barriers were characterized using the World Health Organization (WHO) Multidimensional Adherence Model with patient, condition, therapy, socioeconomic, and health care system/team‐related barriers. Five databases (Medline, Embase, Health and Psychological Instruments, CINHAL, and International Pharmaceutical Abstracts [IPA]) were searched from 1980 to September 2011. Our search identified 1712 citations; 74 articles met inclusion criteria and 51 unique surveys were identified. The Morisky Medication Adherence Scale was the most commonly used survey. Only 20 surveys (39%) have established reliability and validity evidence. According to the WHO Adherence Model domains, patient‐related barriers were most commonly addressed, while condition, therapy, and socioeconomic barriers were underrepresented. The complexity of adherence behavior requires robust self‐report measurements and the inclusion of barriers relevant to each unique patient population and intervention.
Hypertension is the leading risk factor for mortality and the third cause of disability world‐wide. 1 By the year 2025, it is estimated that there will be 1.56 billion patients with hypertension. 2 Poor medication adherence is a major cause of failure to achieve blood pressure (BP) control. 3 Patients take only 50% to 70% of the prescribed doses of antihypertensive medications and up to 50% of patients discontinue their antihypertensive treatment within the first year. In addition, up to 75% of patients do not achieve target BP. 4
Adherence is defined as “the extent to which a person’s behavior corresponds with agreed recommendations from a health care provider.” 4 Oftentimes, nonadherence is attributed to patient‐related barriers; however, medication taking is a complex phenomenon and responsibility for nonadherence should not be solely attributed to the patient. 4 Nonadherence can also be caused by therapy, illness, health system/health care team, and socioeconomic‐related barriers. 4 Patient self‐report is an efficient and practical method for assessing medication adherence and is the only method that can be used to explore patients’ perspective about adherence barriers. 5 Research using patient self‐report of adherence have focused on patient‐related barriers (eg, forgetting doses); however, these barriers represent only part of the problem of nonadherence. 6
Ecological or multilevel system models do not only focus on individual behavior but also on direct attention to environmental barriers. 7 Ecological models encompass intrapersonal, interpersonal, organizational, policy, and community barriers such as patient‐pharmacist interactions, access to health care, drug coverage, social support, and complexity of drug regimen. 4 , 8 Examples of ecological models are Healthy People 2020, 9 the Model of Health and Behavior by the Institute of Medicine, 10 and the World Health Organization (WHO) Multidimensional Adherence Model. 4
In 2003, the WHO described adherence to long‐term therapies as a behavior that is influenced by multiple barriers. The WHO organized adherence barriers into 5 dimensions: health care team/health system, therapy, condition, patient, and socioeconomic‐related barriers. These 5 dimensions represent the WHO Multidimensional Adherence Model. 4 For instance, health care team barriers include the quality of the relationship between patient and health care provider and health care system–related barriers include quality of health care services, health insurance, and drug reimbursement. Therapy‐related barriers (eg, side effects and complexity of drug regimen), condition‐related barriers (eg, severity of symptoms, presence of comorbid conditions, and illness‐related demands), and patient‐related barriers (eg, forgetfulness to take medication, low self‐efficacy, and inaccurate beliefs about diseases and medications) impact patients’ adherence. Although socioeconomic status has not been consistently determined as an independent predictor of adherence, barriers such as poverty, illiteracy, low social support, and unemployment have been found to impact adherence. 4 This comprehensive model can be used to systematically study adherence barriers in hypertensive patients. 11 , 12
A comprehensive understanding of adherence barriers is necessary to determine strategies to improve medication adherence. 13 Interventions that address multiple barriers are most effective to enhance medication adherence. 14 Understanding the barriers affecting a patient’s ability to adhere to antihypertensive therapy will allow researchers to design effective interventions. Moreover, a better understanding will help evaluate the impact of these interventions on perceived and actual barriers to medication use, adherence rates, and ultimately patient outcomes. 13
The aim of this systematic review was to describe patient self‐report instruments measuring barriers to antihypertensive medication adherence and to determine what dimensions of the WHO Adherence Model were included in each instrument.
Methods
Data Sources
A computerized search was performed to identify patient self‐reported studies published in English between 1980 and September 2011. The inception date was selected because the first articles examining patient use of medication—defined as “compliance” at that time—began to appear. 15 The search was conducted by using 5 databases: Medline, Embase, Health and Psychological Instruments (HAPI), CINHAL, and International Pharmaceutical Abstracts (IPA). Two medical librarians (TC) and (DS) assisted in developing a list of appropriate database search terms and synonyms for adherence, hypertension, medication, and self‐report to identify studies that measured patient self‐reported adherence to antihypertensive medications. The following search words were used: drug, medication, pharmaceutical, prescription, patient, adherence, compliance, persistence, cooperation, self‐report, belief, attitude, satisfaction, behavior, communication, concordance, Morisky, social support, knowledge, stress, complexity, interaction, acceptance, survey, scale, instrument, questionnaire, assess, screen, inventory, data collection, antihypertensive agents, hypertension, and high BP.
Study Selection
Two authors (SAG and LMG) identified citations by screening titles and abstracts for potential relevance. The full‐text article for each potentially relevant citation was obtained for further evaluation. Studies eligible for inclusion were observational and experimental studies that measured patient‐perceived barriers of adherence to antihypertensive medications, enrolled adults (18 years and older), and were published in English as a peer‐reviewed full‐text article. Studies were excluded if they measured adherence to other health behaviors such as diet, exercise, and smoking cessation; measured adherence through patient diaries or open‐ended questions; measured only adherence rates; or included patients with multiple chronic diseases (hypertension, dyslipidemia, asthma, diabetes). The full‐text articles were examined to determine eligibility for inclusion; any discrepancies regarding inclusion were resolved by discussion.
Data Synthesis
A standardized data abstraction form was used to obtain information on the surveys used in each study. We identified the survey instrument used, number of items, adherence barriers, and evidence of reliability and validity testing.
One author (SAG) used the WHO Multidimensional Adherence Model to categorize adherence barriers examined in the identified surveys into 5 dimensions. Survey instruments that did not measure any adherence barriers were excluded from this review. Surveys were then compared according to the addressed component of the WHO Adherence Model and according to the reliability and validity evidence.
Results
Search Results
The search identified 1712 citations from the 5 electronic databases. After removing duplicate citations, 1185 titles and abstracts were screened for potential relevance. Investigators disagreed on allocation of 44 articles, and discrepancies were resolved by discussion. In total, 199 citations were retained for full article review, of which 74 citations were included in this systematic review (Figure).
Figure FIGURE.
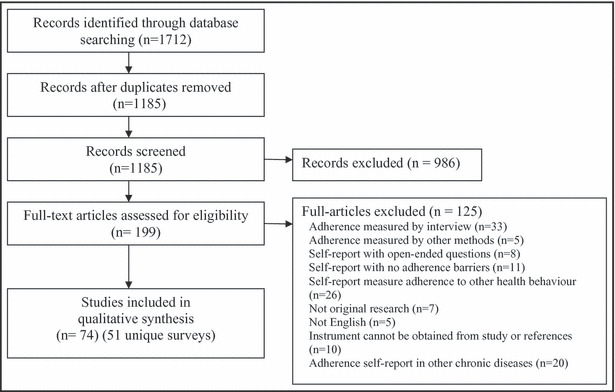
Flow diagram of study selection and studies included in this review.
Surveys
The 74 selected studies included 51 unique survey instruments (Table II). The majority of studies (56 [76%]) used >1 survey to identify adherence barriers, while 18 (24%) studies used 1 survey to identify barriers.
The Morisky Medication Adherence Scale 16 was the most commonly used survey instrument and was utilized in 42 (57%) studies. Other commonly used surveys were the Medication Adherence Self‐Efficacy Scale (MASES) (used in 5 studies), 17 the Medication Adherence Report Scale (MARS) (used in 4 studies), 18 Beliefs about Medicine Questionnaire (BMQ) (used in 3 studies), 19 and the Brief Medication Questionnaire (BMQ) 20 (used in 3 studies).
Of all the survey instruments identified from the included studies, 20 surveys (39%) had established reliability and validity evidence, 14 surveys (27%) had either reliability or validity evidence, and 17 surveys (33%) had neither reliability nor validity evidence (Table II).
Adherence Barriers Identified in the Included Studies
None of the identified surveys measured all dimensions of the WHO Multidimensional Adherence Model, only 5 surveys (10%) 21 , 22 , 23 , 24 , 25 measured 4 WHO dimensions, 4 surveys (7.8%) measured 3 WHO dimensions, 20 , 26 , 27 , 28 6 surveys (11.8%) 27 , 29 , 30 , 31 , 32 , 33 measured 2 dimensions, and the remaining 36 surveys (70%) measured 1 dimension (I, II). The average number of the WHO barrier domains examined in the surveys was 1.61 (median 2.5, and mode was 1).
Table I.
World Health Organization Domains in the Surveysa
| Patient Barriers | Condition Barriers | Therapy Barriers | Socioeconomic Barriers | Health System/Health Care Team Barriers |
|---|---|---|---|---|
| Self‐efficacy 17 , 20 , 21 Forget/remember medications 16 , 18 , 19 , 20 , 22 , 24 , 27 , 30 , 32 , 53 , 54 , 55 Remember to get refill 20 , 56 Careless medication taking 16 Patient’s beliefs about medications/hypertension 20 , 34 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 Self‐efficacy 19 , 21 , 64 Patient’s attitude 52 , 65 Intentionally stop or modify the dosage 16 , 18 , 19 , 30 , 53 , 55 Use of herbal medicine or acupuncture to treat hypertension 23 Awareness about drug insurance 26 Patient knowledge about hypertension and antihypertensive medications 26 , 66 Patient’s expectations about the consequences of poor adherence to medications Patient’s awareness of adherence aids | Patient depression 24 , 27 , 41 Ability to open or close the medication bottle 20 Ability to read the print on the bottle 20 The extent to which the disease influences patient’s risk perception Severity of symptoms Rate of progression of the disease | Side effect occurrence 22 , 23 , 27 , 28 , 29 , 30 , 32 , 33 Medication efficacy 29 , 67 Medication convenience 29 Drug regimen complexity 20 , 24 , 25 , 30 , 32 Frequent medication change 24 Previous treatment failures The availability of medical support to deal with side effects of meds | Financial burden 22 , 24 , 25 , 26 , 67 Social support 23 , 28 , 39 , 66 , 68 Influence of social normatives 31 Cultural and language barriers 23 Health literacy Distance from health care facilities | Difficulty in obtaining a refill 25 , 27 Health care system–related problems 69 Lack of information 66 , 69 , 70 Heath care provider support 69 Practical aspects of hypertension care 71 Medication reimbursement 22 , 69 Quality of physicians’ communication and patient participation 47 Access to health care providers 22 Relationship between patient and health care provider 23 , 54 Difficulty in scheduling appointments 26 Satisfaction with pharmacy services 67 Patient’s perceptions about physician 72 Patient’s perceptions about pharmacist 72 |
aThe barriers in italics represent barriers that were not identified in this systematic review.
Table II.
Characteristics of Surveys and Use of the World Health Organization Dimensions in the Surveys
| Instrument/References | Items | Reliability | Validity | Barriers | ||||
|---|---|---|---|---|---|---|---|---|
| Patient | Condition | Therapy | Socioeconomic | Health System/Team | ||||
| Patient Hypertension Beliefs Questionnaire 73 , 74 | 30 | Subscale Chronbach’s α=0.39–0.59 | X | |||||
| Health Belief Questionnaire 75 , 76 | 15 | Subscale Chronbach’s α=0.53–0.58 Test‐retest reliability=0.59–0.71 | Content validity | X | ||||
| Perceived susceptibility to the sequelae of hypertension 26 | 3 | Cronbach’s α=0.71 | X | |||||
| Perceived severity of hypertension 26 | 1 | X | ||||||
| Benefits of antihypertensive therapy 26 | 6 | Cronbach’s α=0.79 | X | |||||
| Barriers to treatment maintenance 26 | 6 | X | X | X | ||||
| Knowledge about hypertension 26 | 9 | X | ||||||
| Beliefs and Social Normative Influences Questionnaire 31 | 12 | X | X | |||||
| Morisky Medication Adherence Scale 16 , 28 , 36 , 37 , 44 , 47 , 48 , 49 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 | 4 | Cronbach’s α=0.61 | Concurrent and predictive validity | X | ||||
| Patient Satisfaction With Pharmacy Services 21 , 67 | 44 | Subscale Chronbach’s α=0.36–0.80 | Convergent‐discriminant validity | X | X | X | X | |
| Epidemiologic Studies Depression Scale Short‐Form 27 , 41 | 10 | Test‐retest reliability=0.57 | Criterion validity | X | ||||
| The Hypertension Patient’s Perception of Physician Behavior Scale 73 , 92 | 26 | Cronbach’s α=0.93 | Predictive validity | X | ||||
| The Beliefs About Medicine Questionnaire 19 , 39 , 93 , 94 , 95 | 34 | Subscale Chronbach’s α=0.51–0.86 | Criterion and discriminant validity | X | ||||
| Reported Adherence to Medication 19 , 39 | 4 | Chronbach’s α=0.83 | Criterion and discriminant validity | X | ||||
| Brief Medication Questionnaire 20 , 68 , 96 | 9 | Criterion validity | X | X | X | |||
| Antihypertensive Medication Adherence 44 , 68 | 4 | Concurrent validity | X | |||||
| Social Support Inventory 68 | 9 | X | ||||||
| Perceived problems with hypertension treatment 32 | 7 | X | X | |||||
| Hill‐Bone’s Medication Compliance Scalea 23 , 56 | 9 | Cronbach’s α=0.74 Test–retest reliability=0.84 | Predictive validity | X | ||||
| Perceived health care system–related problems/patient‐related problems 69 | 19 | X | ||||||
| Medication Adherence Report Scale 18 , 63 , 70 , 97 | 5 | Cronbach’s α=0.83 | Criterion and convergent validity | X | ||||
| Medication Taking Questionnaire 25 , 52 | 16 | Subscale Chronbach’s α=0.60–0.77 | Content and construct validity | X | X | X | X | |
| Compliance Survey 72 | 6 | X | ||||||
| Patient Satisfaction Survey 72 | 14 | X | ||||||
| Patient Health Beliefs 66 | 9 | X | ||||||
| Patient knowledge regarding hypertension and its treatment 66 | 14 | X | ||||||
| Social Support with Blood Pressure Medications 66 | 2 | X | ||||||
| Patient satisfaction 66 | 5 | X | ||||||
| Reasons for taking antihypertensives 33 | 20 | Test‐retest reliability=0.5 | X | X | ||||
| Medication Adherence Self‐Efficacy Scale 17 , 37 , 48 , 70 , 98 | 26 | Cronbach’s α=0.95 | Criterion validity | X | ||||
| Treatment Satisfaction Questionnaire for Medication 29 , 99 | 14 | Subscale Chronbach’s α=0.85–0.87 | Construct validity | X | X | |||
| Barriers to antihypertensive medication 22 | 8 | X | X | X | X | |||
| Self‐confidence with hypertension treatment 77 | 4 | Chronbach’s α=0.78 | X | |||||
| Perceptions of Western medications/social support 28 | 5 | Subscale Chronbach’s α=0.57–0.91 | Face validity | X | X | X | ||
| Medication Taking Questionnaire Purposeful Action 34 | 20 | Chronbach’s α=0.88 | Content and construct validity | X | ||||
| Medication Compliance Questionnaire 30 | 10 | Subscale Chronbach’s α=0.67 and 0.84 Test‐retest reliability=0.78 and 0.93 | Validity of this survey has been established in a pilot study | X | X | |||
| Self‐efficacy Scale 36 , 39 | 11 | Chronbach’s α=0.9 | X | |||||
| Patient’s intention, attitude, subjective norms, and perceived behavioral control 36 | 11 | Subscale Chronbach’s α=0.77 and 0.61 | X | |||||
| Morisky Medication Adherence Scale 29 , 42 , 54 , 70 , 100 , 101 , 102 , 103 , 104 , 105 | 8 | Cronbach’s α=0.83 | Concurrent and predictive validity | X | ||||
| Visit‐Specific Satisfaction Questionnaire 71 | 5 | Chronbach’s α=0.87 | Concurrent and predictive validity | X | ||||
| Modified Social Support Survey 39 | 18 | Chronbach’s α=0.88 | Convergent and discriminant validity | X | ||||
| Medication Adherence Inventory 55 | 13 | Subscale Chronbach’s α=0.74–0.90 | Concurrent validity | X | ||||
| Patient perception about provider communication 47 | 13 | Chronbach’s α=0.92 | X | |||||
| Medication Adherence Factors Questionnaire 23 | 10 | Content validity | X | X | X | X | ||
| Self‐Reported Medication Taking Behavior 27 | 10 | Cronbach’s α=0.92 | X | X | X | |||
| Barriers to medication adherence 27 | 4 | X | X | |||||
| Patient‐provider relationship 27 | 8 | X | ||||||
| Medication Adherence Scale 106 | 15 | Cronbach’s α=0.82 | X | |||||
| Reasons for noncompliance with antihypertensive medication 24 | 16 | X | X | X | X | |||
| Satisfaction with Information about Medicines Scale 70 | 17 | Chronbach’s α=0.89 | Criterion validity | X | ||||
| Drug Attitude Inventory 107 | 10 | Cronbach’s α=0.65 | X | |||||
aModified version of Hill‐Bone Compliance Scale that only measures adherence to medication.
Patient‐Related Barriers
Thirty‐nine surveys (76%) measured patient‐related barriers associated with no‐adherence (Table II). Twenty‐four surveys (47%) solely identified these barriers and 15 (29%) combined these barriers and barriers from other dimensions. The most commonly studied patient‐related barriers were remembering to take medication, patients’ beliefs about hypertension or antihypertensive medications, and patient self‐efficacy. Johnson and Rogers developed the purposeful action Medication Taking Questionnaire (MTQ), which measures 3 domains of patients’ beliefs: perceived need, perceived effectiveness, and perceived safety of antihypertensive medications. 34 Likewise, the BMQ measures patients’ perceptions about the specific necessity and concerns about medication use. In addition, it measures patients’ perceptions about general harm and general overuse of medications. 19
Another patient‐related barrier is self‐efficacy (ie, a person’s perception about his or her ability to perform a specific behavior). 35 Self‐efficacy influences the initiation and maintenance of health behaviors. 36 In addition, patients with higher self‐efficacy scores were found to have better adherence than those with low self‐efficacy. 18 MASES measures patient self‐efficacy with respect to adherence to antihypertensive medications and this survey has evidence for its psychometric properties. 18 , 37
Health System/Health Care Team–Related Barriers
Fourteen surveys (27%) investigated reasons of nonadherence due to health care team/health system–related barriers. The components of health care team dimension identified from the different surveys in this review can be grouped into the following 3 domains: the patient‐provider relationship, satisfaction with communication, and satisfaction with information. Moreover, the identified components of health system dimension were patients’ perceptions about health care system, satisfaction with pharmacy services, and availability of drug reimbursement.
Therapy‐Related Barriers
Twelve surveys (29%) studied poor adherence caused by therapy‐related barriers. The most commonly identified barriers from this dimension were occurrence of side effects, complexity of drug regimens, and interference of medication taking with daily routines. Although the assessment of side effects in the identified surveys was common, the availability of health care provider support to deal with the side effects was not measured in any study.
Socioeconomic‐Related Barriers
Eleven surveys (22%) investigated socioeconomic‐related barriers. The identified barriers from this dimension were lack of social support, financial burden of medications, and health literacy. Three components of social support have been measured in the identified surveys: practical, informational, and affectionate. Practical support occurs when patients receive practical assistance with taking medication, 38 informational support means assisting patients with necessary information about medication, 39 and affectionate support means being empathic with patients, particularly from family and friends. 38 Maguire and colleagues39 used the Modified Social Support Survey (MSSS) to measure tangible, informational, affectionate, and positive aspects of social interaction. They found that the high level of these components of social support were associated with adherence. On the other hand, Norman31 investigated the impact of practical social support on adherence to antihypertensive drugs and found a significant association with this component of social support and adherence to antihypertensive drugs. Likewise, DiMatteo38 found that patients who received practical social support were 3.6 times more likely to adhere to medications than those who did not. In another study, the practical and information support were more important for starting a medication, whereas emotional support was necessary for the maintenance of adherence. 40
Condition‐Related Barriers
Surveys were least likely to assess condition‐related barriers, with only 4 surveys (8%) used to investigate the influence of condition‐related barriers. Three surveys assessed the presence of psychological disability, particularly depression. 24 , 27 , 41 Only one survey assessed patients’ physical demands on adherence (eg, ability to open a medication bottle and read the print on medication). 20
Discussion
We identified 51 unique survey instruments that have been used to assess patient‐reported barriers to adherence for antihypertensive medications. The 4‐item Morisky Medication Adherence Scale was the most commonly used instrument. This instrument is a generic survey that measures nonadherence to medications due to the following 4 reasons: forgetfulness, carelessness, feeling better, or feeling worse. These 4 reasons are not necessarily correlated with each other. 6 Consequently, the 4‐item Morisky Medication Adherence Scale has a low internal consistency (Cronbach’s α=0.61). Krousel‐Wood and colleagues 42 modified the 4‐item Morisky Medication Adherence Scale to capture more adherence barriers. The new 8‐item Morisky instrument measures a specific medication‐taking behavior instead of a determinant of nonadherence; moreover, this scale has better internal consistency (Cronbach’s α=0.83). Volis and colleagues 6 encouraged researchers to consider a two‐step approach to measuring adherence where brief instruments such as the Morisky model are used to detect the presence of adherence and comprehensive models are used to measure barriers to hypertension.
The majority of survey instruments did not have established psychometric properties.
Self‐report is the only way to gain insight into patient perceptions of barriers; thus, accurate self‐report measurement is imperative. Researchers and clinicians should select tools with good evidence of reliability and validity.
In hypertension, it has been well recognized that adherence requires a multifactorial intervention. 5 , 43 , 44 Current survey instruments are overwhelmingly focused on patient‐related barriers and do not reflect the shift to a multifactorial paradigm. For example, surveys frequently measured forgetfulness but did not measure patients’ awareness or use of adherence aids (eg, reminder packaging and drug calendars), which have been shown to improve adherence to medications. 45 Patients’ use of adherence aids may be related to the communication strategies of the health care professional, the ability of the patient to afford these items, and/or availability in the health care system. All these barriers extend beyond the patient.
This focus on patient‐related barriers reflects the common notion that these barriers are the principal determinants of nonadherence. For a given group of patients, we cannot say with certainty which barriers are prevalent or relevant. In a recent study of African American men who do not have regular health providers, patient factors (ie, age, self‐efficacy, and depression) were predictive of adherence with antihypertensive medication; however, health care professional communication was not. 46 In a separate study, collaborative provider communication was associated with better adherence to antihypertensive medication in African American patients. 47 Relationships between barriers is complex. For example, the association between depressive symptoms and low adherence to antihypertensive medications was mediated by self‐efficacy. 48
While, it is not realistic to have one instrument measure all barriers to medication adherence in hypertension, clinicians and researchers may consider measuring barriers that are relevant to their unique patient population and interventions. 49 Indeed, the majority of studies in this sample elected to employ >1 survey. Social behavioral theory may be useful in helping clinicians and researchers determine which barriers may be most relevant to a given population. 8
There are several barriers that require either survey development and/or integration from other disease areas. Patient participation in the treatment plan is a component of health care team–related dimension that enables patients to reveal their beliefs and concerns about medications; however, this component was measured in only one study. 47 The same can be said with patient physical demands that were not commonly measured, although they represent substantial barriers to adherence. Patients’ health literacy was underrepresented, even though this barrier is correlated with nonadherence and poor health outcomes in patients with cardiovascular diseases. 50 Similarly, financial burden is an underrepresented socioeconomic barrier to adherence in cardiovascular diseases. 51
Each individual barrier may require multiple questions to achieve a valid and reliable measurement. Several barriers such as patients’ beliefs about medications and patients’ satisfaction with health care provider were measured with a single item. For instance, the level of patient satisfaction may require measurement of underlying components of this construct (eg, patients’ perceptions about provider behavior, patients’ perceptions about provider technical skills, and patients’ satisfaction about information provided). Likewise, measurement of patients’ beliefs about medications requires assessment of patients’ perceptions about the necessity and potential harms of medications.
There are various challenges to measurement of adherence barriers. First, specific barriers may not be stable over time and vary with individual medications. Second, the multifactorial nature of nonadherence barriers may lead to lengthy surveys and a significant burden to respondents. Third, different patient characteristics such as age, race, level of health literacy, and patients’ beliefs may represent challenges to measurement. Furthermore, other characteristics associated with social norms, clinical settings, and the integrity of health care systems also represent a challenge to measurement. Fourth, measurement is influenced by the relationships between barriers from different dimensions (eg, self‐efficacy and depression). Finally, longitudinal assessment may be required to distinguish between chronic and episodic nonadherence and related‐barriers that may contribute to these types of nonadherence.
Since adherence is a common and dynamic process that affects patient health, it should be a priority for health care policy. Health care providers should consider measurement of adherence and barriers as common health practices and use patient‐specific information to guide the selection of the most relevant interventions to enhance adherence.
Limitations
There are several limitations of this systematic review. First, the search was limited to literature published in English, which may eliminate studies published in other languages. Second, we restricted this search to hypertension, but we believe that the focus on one disease will enhance the understanding of barriers that may affect adherence to medications of the targeted disease. Third, further validity and reliability testing may have been conducted in research that we did not identify in this review. Fourth, the development of measures of adherence barriers may be influenced by the time period in which the study was peformed, as a typical patients’ age and the number of antihypertensive medications may differ over the 3 decades of study. Fifth, we included studies published from 1980, despite the fact that the WHO Adherence Model was developed in 2003 for two reasons. We observed that many surveys were developed before 2000 and the WHO framework did not introduce new barriers but distributed the focus among multiple barriers. Finally, we did not perform a meta‐analysis because of the heterogeneity of the identified surveys, which measured adherence barriers.
Implications for Research and Practice
Researchers and clinicians may consider using a combination of survey instruments with evidence for reliability and validity to measure adherence barriers specific to their context. The MTQ 25 , 52 covers 4 domains (ie, patients, therapy, socioeconomic, and health systems) in 16 questions and could be paired with the Epidemiologic Studies Depression Scale Short‐Form 41 to measure the condition domain in 10 questions.
While it is important to consider the complete WHO Adherence Model, research in adherence should not use a one‐size‐fits‐all approach. 49 A clinician or researcher may be interested in a specific construct and/or patient response burden may limit measurement of all 5 domains. For example, in an elderly population, the BMQ 20 can be used to identify the potential effect of patient’s physical demands on adherence.
Conclusions
Patient‐related barriers were the most commonly identified in this review, while condition, therapy, and socioeconomic barriers were underrepresented. The majority of surveys did not have evidence for reliability and validity. The complexity of adherence behavior requires robust self‐report measurements and the inclusion of barriers relevant to each unique patient population and intervention. Future research should consider both the psychometric properties of self‐report measures and the use of multidimensional adherence models to guide the measurement of barriers to adherence to antihypertensive medications to help both clinicians and researchers understand how to optimize medication therapy and reduce the burden of uncontrolled hypertension.
Acknowledgments: We would like to acknowledge the medical librarians Mrs Trish Chatterley and Mr Dale Storie for their well‐appreciated assistance with the literature search for this systematic review. Suliman AlGhurair would like to acknowledge the Medical Services Directorate of Saudi Arabian Armed Forces for supporting his graduate study.
Conflict of interest: None.
Supporting information
Table SI. Characteristics of surveys and use of the WHO dimensions in the surveys.
Supporting info item
References
- 1. Ezzati M, Lopez AD, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. [DOI] [PubMed] [Google Scholar]
- 2. Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 3. Waeber B, Burnier M, Brunner HR. How to improve adherence with prescribed treatment in hypertensive patients? J Cardiovasc Pharmacol. 2000;35(Suppl 3):S23–S26. [DOI] [PubMed] [Google Scholar]
- 4. Sabate E. World Health Organization. Adherence to Long Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. [PubMed] [Google Scholar]
- 5. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;4:487–497. [DOI] [PubMed] [Google Scholar]
- 6. Voils CI, Hoyle RH, Thrope CT, et al. Improving the measurement of self‐reported medication nonadherence. J Clin Epidemiol. 2011;64:250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kidd KE, Altman DG. Adherence in social context. Control Clin Trials. 2000;21(Suppl 5):S184–S187. [DOI] [PubMed] [Google Scholar]
- 8. Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice, 4th edn. San Francisco, CA: Jossey‐Bass; 2008. [Google Scholar]
- 9. United States Department of Health and Human Services . Healthy People 2020. http://www.healthypeople.gov/2020/Consortium/HP2020Framework.pdf. Accessed November 8, 2011.
- 10. The National Academies Press. Institute of Medicine: Health and Behaviour Model, the interplay of biological, behavioural, and societal influences. http://www.nap.edu/openbook.php?isbn=0309070309. Accessed November 8, 2011.
- 11. Jansa M, Hernandez C, Vidal M, et al. Multidimensional analysis of treatment adherence in patients with multiple chronic conditions. A cross‐sectional study in a tertiary hospital. Patient Educ Couns. 2010;81:161–168. [DOI] [PubMed] [Google Scholar]
- 12. Gallagher R, Warwick M, Chenoweth L, et al. Medication knowledge, adherence and predictors among people with heart failure and chronic obstructive pulmonary disease. J Nurs Healthc Chronic Illn. 2011;3:30–40. [Google Scholar]
- 13. Brown TB, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86:304–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van Eijken M, Tsang S, Wensing M, et al. Interventions to improve medication compliance in older patients living in the community: a systematic review of the literature. Drugs Aging. 2003;20:229–240. [DOI] [PubMed] [Google Scholar]
- 15. Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–342. [DOI] [PubMed] [Google Scholar]
- 16. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self‐reported measure of medication adherence. Med Care. 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- 17. Ogedegbe G, Mancuso CA, Allegrante JP, et al. Development and evaluation of a medication adherence self‐efficacy scale in hypertensive African‐American patients. J Clin Epidemiol. 2003;56:520–529. [DOI] [PubMed] [Google Scholar]
- 18. Horne R, Weinman J. Self‐regulation and self‐management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non‐adherence to preventer medication. Psychol Health. 2002;17:17–32. [Google Scholar]
- 19. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14:1–24. [Google Scholar]
- 20. Svarstad BL, Chewning BA, Sleath BL, et al. The brief medication questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ Couns. 1999;37:113–124. [DOI] [PubMed] [Google Scholar]
- 21. MacKeigan LD, Larson LN. Development and validation of an instrument to measure patient satisfaction with pharmacy services. Med Care. 1989;27:522–536. [DOI] [PubMed] [Google Scholar]
- 22. Vawter L, Tong X, Gemilyan M, et al. Barriers to antihypertensive medication adherence among adults – United States, 2005. J Clin Hypertens. 2008;10:922–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hsu YH, Mao CL, Wey M. Antihypertensive medication adherence among elderly Chinese Americans. J Transcult Nurs. 2010;21:297–305. [DOI] [PubMed] [Google Scholar]
- 24. Culig J, Leppee M, Boskovic J, et al. Determining the difference in medication compliance between the general patient population and patients receiving antihypertensive therapy: a case study. Arch Pharm Res. 2011;34:1143–1152. [DOI] [PubMed] [Google Scholar]
- 25. Lehane E, McCarthy G. An examination of the intentional and unintentional aspects of medication non‐adherence in patients diagnosed with hypertension. J Clin Nurs. 2007;16:698–706. [DOI] [PubMed] [Google Scholar]
- 26. Cummings KM, Kirscht JP, Binder LR, et al. Determinants of drug treatment maintenance among hypertensive persons in inner city Detroit. Public Health Rep. 1982;97:99–106. [PMC free article] [PubMed] [Google Scholar]
- 27. Martin MY, Kohler C, Kim YI, et al. Taking less than prescribed: medication nonadherence and provider‐patient relationships in lower‐income, rural minority adults with hypertension. J Clin Hypertens. 2010;12:706–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li WW, Stewart AL, Stotts NA, et al. Cultural factors and medication compliance in Chinese immigrants who are taking antihypertensive medications: instrument development. J Nurs Meas. 2005;13:231–252. [DOI] [PubMed] [Google Scholar]
- 29. Bharmal M, Payne K, Atkinson MJ, et al. Validation of an abbreviated treatment satisfaction questionnaire for medication (TSQM‐9) among patients on antihypertensive medications. Health Qual Life Outcomes. 2009;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hassan NB, Hasanah CI, Foong K, et al. Identification of psychosocial factors of noncompliance in hypertensive patients. J Hum Hypertens. 2006;20:23–29. [DOI] [PubMed] [Google Scholar]
- 31. Norman SA, Marconi KM, Schezel GW, et al. Beliefs, social normative influences, and compliance with antihypertensive medication. Am J Prev Med. 1985;1:10–17. [PubMed] [Google Scholar]
- 32. Enlund H, Jokisalo E, Wallenius S, et al. Patient‐perceived problems, compliance, and the outcome of hypertension treatment. Pharm World Sci. 2001;23:60–64. [DOI] [PubMed] [Google Scholar]
- 33. Benson J, Britten N. Patients’ views about taking antihypertensive drugs: questionnaire study. BMJ. 2003;326:1314–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Johnson MJ, Rogers S. Development of the purposeful action medication‐taking questionnaire. West J Nurs Res. 2006;28:335–351. [DOI] [PubMed] [Google Scholar]
- 35. Bandura A. Self‐efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 36. Bane C, Hughes CM, McElnay JC. Determinants of medication adherence in hypertensive patients: an application of self‐efficacy and the theory of planned behaviour. Int J Pharm Pract. 2006;14:197–204. [Google Scholar]
- 37. Fernandez S, Chaplin W, Schoenthaler AM, et al. Revision and validation of the medication adherence self‐efficacy scale (MASES) in hypertensive African Americans. J Behav Med. 2008;31:453–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for non‐compliance with medical treatment: meta‐analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. [DOI] [PubMed] [Google Scholar]
- 39. Maguire LK, Hughes CM, McElnay JC. Exploring the impact of depressive symptoms and medication beliefs on medication adherence in hypertension – a primary care study. Patient Educ Couns. 2008;73:371–376. [DOI] [PubMed] [Google Scholar]
- 40. Culos‐Reed SN, Rejeski WJ, McAuley E, et al. Predictors of adherence to behavior change interventions in the elderly. Control Clin Trials. 2000;21(Suppl 5):S200–S205. [DOI] [PubMed] [Google Scholar]
- 41. Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: evaluation of a short form of the CES‐D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 42. Krousel‐Wood M, Islam T, Webber LS, et al. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]
- 43. Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;(2):CD000011. [DOI] [PubMed] [Google Scholar]
- 44. Krousel‐Wood M, Hyre A, Muntner P, Morisky D. Methods to improve medication adherence in patients with hypertension: current status and future directions. Curr Opin Cardiol. 2005;20:296–300. [DOI] [PubMed] [Google Scholar]
- 45. Heneghan CJ, Glasziou P, Perera R. Reminder packaging for improving adherence to self‐administered long‐term medications. Cochrane Database Syst Rev. 2011;(1):CD005025. [DOI] [PubMed] [Google Scholar]
- 46. Lewis LM, Schoenthaler AM, Ogedegbe G. Patient factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. J Clin Hypertens. February 13, 2012. 2012;14:250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Schoenthaler A, Chaplin WF, Allegrante JP, et al. Provider communication effects medication adherence in hypertensive African Americans. Patient Educ Couns. 2009;75:185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schoenthaler A, Ogedegbe G, Allegrante JP. Self‐efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive African Americans. Health Educ Behav. 2009;36:127–137. [DOI] [PubMed] [Google Scholar]
- 49. Blalock SJ. The theoretical basis for practice‐relevant medication use research: patient‐centered/behavioral theories. Res Social Adm Pharm. 2011;7:317–329. [DOI] [PubMed] [Google Scholar]
- 50. Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. [DOI] [PubMed] [Google Scholar]
- 51. Wu JR, Moser DK, Chung ML, et al. Predictors of medication adherence using a multidimensional adherence model in patients with heart failure. J Card Fail. 2008;14:603–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Johnson MJ. The medication‐taking questionnaire for measuring patterned behavior adherence. Commun Nurs Res. 2002;35:65–70. [PubMed] [Google Scholar]
- 53. Kressin NR, Wang F, Long J, et al. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med. 2007;22:768–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Morisky DE, Ang A, Krousel‐Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–354. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 55. Chen SL, Tsai JC, Lee WL. The impact of illness perception on adherence to therapeutic regimens of patients with hypertension in Taiwan. J Clin Nurs. 2009;18:2234–2244. [DOI] [PubMed] [Google Scholar]
- 56. Kim MT, Hill MN, Bone LR, et al. Development and testing of the Hill‐Bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs. 2000;15:90–96. [DOI] [PubMed] [Google Scholar]
- 57. Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti‐hypertensive treatment in Pakistan. PLoS One. 2007;2:e280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lau R, Stewart K, McNamara KP, et al. Evaluation of a community pharmacy‐based intervention for improving patient adherence to antihypertensives: a randomised controlled trial. BMC Health Serv Res. 2010;10:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nelson MR, Reid CM, Ryan P, et al. Self‐reported adherence with medication and cardiovascular disease outcomes in the second Australian national blood pressure study (ANBP2). Med J Aust. 2006;185:487–489. [DOI] [PubMed] [Google Scholar]
- 60. Ogedegbe G, Schoenthaler A, Richardson T, et al. An RCT of the effect of motivational interviewing on medication adherence in hypertensive African Americans: rationale and design. Contemp Clin Trials. 2007;28:169–181. [DOI] [PubMed] [Google Scholar]
- 61. Thorpe CT, Bryson CL, Maciejewski ML, et al. Medication acquisition and self‐reported adherence in veterans with hypertension. Med Care. 2009;47:474–481. [DOI] [PubMed] [Google Scholar]
- 62. Amado Guirado E, Pujol Ribera E, Pacheco Huergo V, et al. Knowledge and adherence to antihypertensive therapy in primary care: results of a randomized trial. Gac Sanit. 2011;25:62–67. [DOI] [PubMed] [Google Scholar]
- 63. Van De Steeg N, Sielk M, Pentzek M, et al. Drug‐adherence questionnaires not valid for patients taking blood‐pressure‐lowering drugs in a primary health care setting. J Eval Clin Pract. 2009;15:468–472. [DOI] [PubMed] [Google Scholar]
- 64. Turki AK, Sulaiman SAS. Adherence to antihypertensive therapy in general hospital of Penang: does daily dose frequency matter? Jord J Pharm Sci. 2009;2:167–176. [Google Scholar]
- 65. Morgado M, Rolo S, MacEdo A, et al. Predictors of uncontrolled hypertension and antihypertensive medication nonadherence. J Cardiovasc Dis Res. 2010;1:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wang PS, Bohn RL, Knight E, et al. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Blenkinsopp A, Phelan M, Bourne J, et al. Extended adherence support by community pharmacists for patients with hypertension: randomised controlled trial. Int J Pharm Pract. 2000;8:165–175. [Google Scholar]
- 68. Choo PW, Rand CS, Inui TS, et al. A cohort study of possible risk factors for over‐reporting of antihypertensive adherence. BMC Cardiovasc Disord. 2001;1:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Jokisalo E, Kumpusalo E, Enlund H, et al. Factors related to non‐compliance with antihypertensive drug therapy. J Hum Hypertens. 2002;16:577–583. [DOI] [PubMed] [Google Scholar]
- 70. Kjeldsen LJ, Bjerrum L, Herborg H, et al. Development of new concepts of non‐adherence measurements among users of antihypertensives medicines. Int J Clin Pharm. 2011;33:565–572. [DOI] [PubMed] [Google Scholar]
- 71. Bell RA, Kravitz RL. Physician counseling for hypertension: what do doctors really do? Patient Educ Couns. 2008;72:115–121. [DOI] [PubMed] [Google Scholar]
- 72. Vivian EM. Improving blood pressure control in a pharmacist‐managed hypertension clinic. Pharmacotherapy. 2002;22:1533–1540. [DOI] [PubMed] [Google Scholar]
- 73. Morrell RW, Park DC, Kidder DP, et al. Adherence to antihypertensive medications across the life span. Gerontologist. 1997;37:609–619. [DOI] [PubMed] [Google Scholar]
- 74. Jette AM, Cummings KM, Brock BM, et al. The structure and reliability of health beliefs indices. Health Serv Res. 1981;16:81–98. [PMC free article] [PubMed] [Google Scholar]
- 75. Anderoli KG. Self‐concept and health beliefs in compliant and noncompliant hypertensive patients. Nurs Res. 1981;30:323–327. [PubMed] [Google Scholar]
- 76. Cronin SN. Health beliefs in compliant and noncompliant hypertensive clients. J Community Health Nurs. 1986;3:87–97. [DOI] [PubMed] [Google Scholar]
- 77. Bosworth HB, Olsen MK, Gentry P, et al. Nurse administered telephone intervention for blood pressure control: a patient‐tailored multifactorial intervention. Patient Educ Couns. 2005;57:5–14. [DOI] [PubMed] [Google Scholar]
- 78. Cote I, Farris K, Feeny D. Is adherence to drug treatment correlated with health‐related quality of life? Qual Life Res. 2003;12:621–633. [DOI] [PubMed] [Google Scholar]
- 79. de Souza WA, Sabha M, de Faveri Favero F, et al. Intensive monitoring of adherence to treatment helps to identify “true” resistant hypertension. J Clin Hypertens. 2009;11:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Fernandez S, Scales KL, Pineiro JM, et al. A senior center‐based pilot trial of the effect of lifestyle intervention on blood pressure in minority elderly people with hypertension. J Am Geriatr Soc. 2008;56:1860–1866. [DOI] [PubMed] [Google Scholar]
- 81. Gregoire JP, Guibert R, Archambault A, et al. Medication compliance in a family practice: testing a self‐report questionnaire in a primary care setting. Can Fam Physician. 1992;38:2333–2337. [PMC free article] [PubMed] [Google Scholar]
- 82. Lowry KP, Dudley TK, Oddone EZ, et al. Intentional and unintentional nonadherence to antihypertensive medication. Ann Pharmacother. 2005;39:1198–1203. [DOI] [PubMed] [Google Scholar]
- 83. Morris AB, Li J, Kroenke K, et al. Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy. 2006;26:483–492. [DOI] [PubMed] [Google Scholar]
- 84. Ogedegbe G, Schoenthaler A, Fernandez S. Appointment‐keeping behavior is not related to medication adherence in hypertensive African Americans. J Gen Intern Med. 2007;22:1176–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Ann Pharmacother. 2002;36:40–45. [DOI] [PubMed] [Google Scholar]
- 86. Suleiman A, Sulaiman S, Albarq A. Hospital admission and poor adherence to antihypertensive therapy: is there any relationship? Int J Pharm Pharm Sci. 2010;2:38–46. [Google Scholar]
- 87. Chabot I, Moisan J, Gregoire JP, et al. Pharmacist intervention program for control of hypertension. Ann Pharmacother. 2003;37:1186–1193. [DOI] [PubMed] [Google Scholar]
- 88. McNagny SE, Ahluwalia JS, Clark WS, et al. Cigarette smoking and severe uncontrolled hypertension in inner‐city African Americans. Am J Med. 1997;103:121–127. [DOI] [PubMed] [Google Scholar]
- 89. Muntner P, Halanych JH, Reynolds K, et al. Low medication adherence and the incidence of stroke symptoms among individuals with hypertension: the REGARDS study. J Clin Hypertens. 2011;13:479–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Wang J, Wu J, Yang J, et al. Effects of pharmaceutical care interventions on blood pressure and medication adherence of patients with primary hypertension in China. Clin Res Regul Aff. 2011;28:1–6. [Google Scholar]
- 91. Hui‐min X, Xiao‐ying J. Relationship between treatment compliance and quality of life in patients with primary hypertension. Chin J Clinic Rehabil. 2005;9:146–147. [Google Scholar]
- 92. Wolf MH, Putnam SM, James SA, et al. The medical interview satisfaction scale: development of a scale to measure patient perceptions of physician behavior. J Behav Med. 1978;1:391–401. [DOI] [PubMed] [Google Scholar]
- 93. Horne R, Clatworthy J, Polmear A, et al. Do hypertensive patients’ beliefs about their illness and treatment influence medication adherence and quality of life? J Hum Hypertens. 2001;15(Suppl 1):S65–S68. [DOI] [PubMed] [Google Scholar]
- 94. Magadza C, Radloff SE, Srinivas SC. The effect of an educational intervention on patients’ knowledge about hypertension, beliefs about medicines, and adherence. Res Social Adm Pharm. 2009;5:363–375. [DOI] [PubMed] [Google Scholar]
- 95. Manze M, Rose AJ, Orner MB, et al. Understanding racial disparities in treatment intensification for hypertension management. J Gen Intern Med. 2010;25:819–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Dennis T, Meera NK, Binny K, et al. Medication adherence and associated barriers in hypertension management in India. CVD Prev Control. 2011;6:9–13. [Google Scholar]
- 97. Horne R, Clatworthy J, Hankins M, et al. High adherence and concordance within a clinical trial of antihypertensives. Chronic Illn. 2010;6:243–251. [DOI] [PubMed] [Google Scholar]
- 98. Gozum S, Hacihasanoglu R. Reliability and validity of the Turkish adaptation of medication adherence self‐efficacy scale in hypertensive patients. Eur J Cardiovasc Nurs. 2009;8:129–136. [DOI] [PubMed] [Google Scholar]
- 99. Atkinson MJ, Sinha A, Hass SL, et al. Validation of a general measure of treatment satisfaction, the treatment satisfaction questionnaire for medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes. 2004;2:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Islam T, Muntner P, Webber LS, et al. Cohort study of medication adherence in older adults (CoSMO): extended effects of Hurricane Katrina on medication adherence among older adults. Am J Med Sci. 2008;336:105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Morisky DE, Kominski GF, Afifi AA, et al. The effects of a disease management program on self‐reported health behaviors and health outcomes: evidence from the “Florida: a healthy state (FAHS)” medicaid program. Health Educ Behav. 2009;36:505–517. [DOI] [PubMed] [Google Scholar]
- 102. Berni A, Ciani E, Cecioni I, et al. Adherence to antihypertensive therapy affects ambulatory arterial stiffness index. Eur J Intern Med. 2011;22:93–98. [DOI] [PubMed] [Google Scholar]
- 103. Holt EW, Muntner P, Joyce CJ, et al. Health‐related quality of life and antihypertensive medication adherence among older adults. Age Ageing. 2010;39:481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Krousel‐Wood MA, Muntner P, Joyce CJ, et al. Adverse effects of complementary and alternative medicine on antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J Am Geriatr Soc. 2010;58:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Muntner P, Joyce C, Holt E, et al. Defining the minimal detectable change in scores on the eight‐item Morisky medication adherence scale. Ann Pharmacother. 2011;45:569–575. [DOI] [PubMed] [Google Scholar]
- 106. Li W, Wallhagen MI, Froelicher ES. Factors predicting blood pressure control in older Chinese immigrants to the United States of America. J Adv Nurs. 2010;66:2202–2212. [DOI] [PubMed] [Google Scholar]
- 107. Saleem F, Hassali MA, Shafie AA, et al. Association between knowledge and drug adherence in patients with hypertension in Quetta, Pakistan. Trop J Pharm Res. 2011;10:125–132. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table SI. Characteristics of surveys and use of the WHO dimensions in the surveys.
Supporting info item


