Abstract
J Clin Hypertens (Greenwich). 2012;14:139–143. ©2012 Wiley Periodicals, Inc.
Self blood pressure measurement (SBPM) improves the overall management of hypertension provided it is implemented with methodologic care. This concerns especially the accuracy and technical requirements of blood pressure (BP) measuring devices that should be validated according to internationally accepted protocols. The use of memory‐equipped automatic home monitors is strongly recommended because they reduce observer bias, avoid patients’ misreporting, and allow fully automatic analysis by software. For current use, simple software should be worked out that allow for analysis of readings in an objective manner. Miscuffing is also a frequent source of measurement error in obese arms when oscillometric devices are used. Modern automatic devices can overcome this problem because of special software algorithms that can provide accurate measurements over a wide range of arm circumferences when coupled with a single cuff of standard dimensions. Tronco‐conical–shaped cuffs are a key component of this instrumentation because they better fit on large conical arms frequently present in obese individuals. Semi‐rigid cuffs should be increasingly used because they ensure that the proper amount of tension is applied without the intervention of the user. Continuous technology improvement of instrumentation for SBPM can be achieved through close cooperation between manufacturers and validation centers.
Although the conventional Riva‐Rocci‐Korotkoff approach is still the cornerstone in the diagnostic and therapeutic management of arterial hypertension, several concerns have been raised over the years concerning its ability to accurately and reliably reflect the BP load exerted on the cardiovascular system. 1 BP measurement by the doctor has been known for decades to induce a BP reaction in the patient. 2 The problem of the white‐coat effect can be overcome with the use of out‐of‐office BP measurement. This includes techniques for self‐measurement of BP in the home or work place and for ambulatory BP monitoring by automated devices. 1 , 3 Use of these different approaches may actually lead to an improved assessment of the patients’“real” BP levels, provided that the most appropriate method for any given condition is adopted and the selected approach is implemented with the required methodologic care. SBPM has been recommended by many scientific societies because it may improve the overall management of hypertension and evidence of its utility continues to accumulate. 4 , 5 , 6 The aim of this article is to provide the necessary information for optimal SBPM, focusing especially on accuracy and technical requirements of BP measuring devices including cuffs and bladders.
Devices and Techniques
Automated oscillometric BP devices are increasingly being used for office BP measurement. Automated devices can eliminate several observer errors and avoid the problem of observer bias and digit preference. 4 , 5 , 6 Moreover, a long period of training is not necessary as it is with the standard auscultatory technique, and these devices can easily be used in patients’ home. Another advantage of automated measurement is the ability to take a series of rapid sequential readings 7 and automatically average them. The main disadvantage may be the error inherent in the oscillometric method. This is due to the fact that systolic BP and diastolic BP values are computed through a proprietary algorithm that is not disclosed to the operators. For this reason, a reliable use of these devices requires validation by internationally accepted protocols. European States are legally obligated to obtain certification on the safety and essential performance of BP‐measuring devices and the European Union (MDD93/42/EEC) requires clinical evaluation of automatic monitors. 8 At least until now, however, an independent validation after established international protocols is not always a compulsory requirement. In Europe it is up to the individual manufacturer’s Notified Body to establish what clinical data they require for the approval of the BP‐measuring devices. The application of harmonized EN standards, however, is highly recommended for the fulfillment of the MDD93/42/EEC essential requirements (http://www.ghtf.org). These guidelines are regularly updated accordingly with regulatory developments but are not legally binding. Validation of BP‐measuring devices should follow the protocols proposed by internationally acknowledged ad‐hoc societies. One of them is the Association for the Advancement of Medical Instrumentation (AAMI), 9 which in 1987 published standards for the evaluation of automated and aneroid sphygmomanometers, including a protocol for assessing the accuracy of devices. These recommendations were followed in 1990 by the protocol of the British Hypertension Society. 10 A basic revision of the current AAMI protocol and harmonization with the International Organization for Standardization/International Electrotechnical Commission standards is ongoing. A common limitation of these protocols is their difficult application to routine evaluation of BP‐measuring devices. In an attempt to overcome such a problem, the Working Group on Blood Pressure Monitoring of the European Society of Hypertension (ESH) has published a simplified protocol to facilitate the evaluation process, 11 which was updated in 2010. 12 Up until now, more than 100 upper‐arm devices and 33 wrist monitors for SBPM have passed ≥1 of the validation protocols and can therefore be recommended. An updated list of validated devices can be found on a not‐for‐profit Web site supported by the ESH (http://www.dableducational.org). Further development in this field is represented by the recent proposal of an integrated validation of automated devices, which includes not only the assessment of their accuracy, but also the evaluation of their practical usability and applicability in daily‐life scenarios. 13
Current guidelines for SBPM 4 , 6 recommend that in untreated patients there should be an initial 7‐day measurement period with 2 readings taken in the morning and in the evening at predefined times (6 am–9 am and 6 pm–9 pm). The average of day 2 through 7 values should be taken as reference for the follow‐up period. Once treatment is initiated, SBPM should be used exactly as in the pre‐treatment phase and the readings should preferably be taken at trough, ie, before drug intake in case of once‐daily administration. When changes in treatment occur, the averages of the SBPM values measured over 2 weeks should be used to assess BP control. It follows that many BP readings should be collected that may create some problems for interpretations. For reasons of time and practicality, doctors are reluctant to calculate the average of tens or even hundreds of values and thus they usually make a cursory inspection of patients’ reports. In addition, there is experimental evidence that many patients tend to manipulate the BP reports, excluding those values that do not seem appropriate to them. 14 Current international guidelines do not provide specific recommendations on how to solve these problems. 6 The use of memory‐equipped automatic home BP monitors is strictly recommended only for patients participating in clinical trials. 6 However, to avoid reporting bias, this recommendation should also be extended to manufacturers and all potential users. Memory‐equipped devices would also allow fully automatic analysis by software, as is done with ambulatory recordings. 6 Simple softwares should thus be worked out that allow for the analysis of all BP readings collected by the patient in an objective way. These softwares should be made available to health care professionals, chiefly those working in hypertension clinics (Figure). The recent ESH guidelines do not provide precise criteria for data reporting. 6 Among the features that may be useful, they only mention the separate calculation of morning and evening BP averages and the possibility to select specific time periods for statistical analysis. A basic summary of self‐BP recordings for use in clinical practice is proposed in Table I. Device softwares may include additional optional analyses whose predictive value has been recently highlighted 6 , 15 , 16 (Table II). Obviously, the latter parameters should be used only by competent personnel working in hypertension clinics, because their interpretation requires a specific knowledge of the problems related to BP assessment. Needless to say, these devices would be more expensive and need to be connected with a printer or a personal computer. However, many specialists would be willing to use this equipment in everyday practice and would encourage their patients to buy one such device. 17
Figure FIGURE.
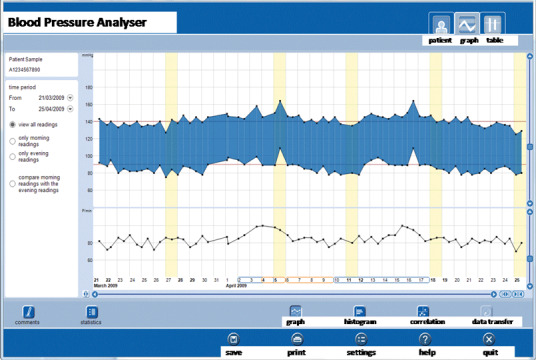
An example of an automatically generated report of self‐measured blood pressure monitoring data that may aid the physician in making therapeutic decisions. The software allows the user to select the list of readings (table) or the graph (top) and to analyze the data according to several options (bottom).
Table I.
Basic Summary of Self‐Measured Blood Pressure (BP) Recordings
| List of each single reading with date, hour, and minute of occurrence |
| A graphical display of single readings with BP and heart rate value referred to the vertical axis and date and time on the horizontal axis |
| Average value of systolic and diastolic BP and heart rate for the whole recording period or of identified subperiods. Possibility of comparing morning and evening readings |
| Listing and linear graph of day‐by‐day and week‐by‐week averages |
aRelevant data that may be helpful in clinical practice for making therapeutic decisions are listed.
Table II.
Additional Optional Analyses of Self‐Measured Blood Pressure (BP) Based on Recent Results Highlighting the Predictive Value of Parameters Other Than Average BP
| Calculation of the whole period standard deviation for BP and heart rate |
| Day‐by‐day difference between morning and evening BP and heart rate values or morning‐to‐evening ratio. This parameter may be useful to assess daily changes in BP and heart rate, as done for day‐night changes with ambulatory monitoring. |
| Calculation of the ratio between the morning change in home BP to the evening increase in home BP. Calculation of this parameter, which requires days of monitoring without treatment followed by days of monitoring under treatment may be used for assessment of duration of antihypertensive drug treatment. |
Special Patient Populations
There are possible limitations to the performance of automated devices in diabetics, elderly patients, children, and pregnant women. 11 , 12 Regulations require that devices intended for special populations must be validated in these specific groups (AAMI/ISO81060‐2) to prevent patients from experiencing faulty measurements. Improvement in knowledge of these problems should be promoted among health care personnel and patients using such devices. A controversial issue is the use of automatic devices in patients with arrhythmias. According to current protocols, 9 , 11 , 12 patients with arrhythmias should be excluded from validations. It should be noted that the prevalence of arrhythmias among users of automated BP monitors is increasing due to increasing age of the patients. Scientific societies and standardization bodies should thus address this issue and provide specific validation protocols for patients with arrhythmias, which would stimulate technologic competition.
The Cuff and Bladder
International guidelines recommend that the inflatable rubber bladder inside the cuff should be long enough to match the arm circumference and contained within an inelastic cloth, the full length of which should extend beyond the end of the inflatable bladder. 1 , 4 To secure the cuff around the arm, Velcro surfaces are commonly used, which should be discarded when they lose their grip. Miscuffing may lead to inaccurate BP measurements, and use of a cuff with a bladder of inappropriate dimensions for the arm is a significant source of error. 18 , 19 To avoid the consequences of miscuffing when using automatic devices, more comprehensive requirements for the device validation need to be developed. In the clinical validation report it is important to document the type, shape, and materials of the cuff under test. It should be noted whether the cuff has a D ring typical for self‐application cuffs or no D ring typical in clinical use when the cuff is applied by another person. For the device under test, it is recommended that the average inflation and deflation rates on the patient between systolic and diastolic pressure be recorded or the data from the manufacturer’s specification be obtained in the clinical report. This should be done to avoid later alteration of the measurement speed of a validated device accidentally or due to market demand for always shorter measurement times and better measurement comfort.
BP Measurement in Patients With Large Arms
BP measurement in obese arms may result in inaccurate BP measurements. 18 , 19 , 20 It should be noted that the upper arm in obese patients often has a pronounced tronco‐conical shape that makes it difficult to fit the cuff to the arm, increasing the likelihood of inaccurate BP measurements. 21 , 22 , 23 Thus, for obese subjects the cuff should be tailored according to the arm circumference and shape. 24 This may occur not only in obese individuals but also in men whose arms have highly muscular compositions, due to the effect of large bicep muscles. As mentioned above, the most frequent error in measuring BP in the outpatient clinic is “miscuffing,” with undercuffing of large arms accounting for 84% of the miscuffings. 25 Current guidelines recommend that the length of the bladder should cover 80% to 100% of the upper arm circumference and that the width be about half that of the length, irrespective of the method of measurement. 6 However, the recommendations for cuff size with relation to arm circumference apply to the standard auscultatory method, but not necessarily to BP measured with oscillometric devices. Mercury sphygmomanometers are being removed from clinical practice because of environmental concerns about mercury contamination. Today, modern automatic devices can overcome the problem of miscuffing in patients with large arms as a result of a special software algorithm that can provide accurate BP readings over a wide range of arm circumferences when coupled with a single cuff of standard dimensions. 26 , 27 A tronco‐conical–shaped cuff may be a key component of this instrumentation because it fits better on large, conical arms. 28 In fact, the use of an inappropriately small rectangular cuff can be the source of large errors when BP is measured with the oscillometric method, 28 in which measured cuff pressure oscillations are a reflection of the entire artery volume change under the cuff and does not involve the central section only. 29 Whether validated wrist BP monitors can be an appropriate solution for very obese patients should also be established. 19 , 25 Unfortunately, there is no available evidence to show that BP measured with upper arm oscillometric devices or wrist monitors is reliable in the obese population. Assessment of BP in obese individuals is further complicated by the fact that the discrepancies between office and out‐of‐office BPs are more pronounced in this group than in the nonobese segment of the population. 30 Prospective trials designed to specifically evaluate whether BP measured with automatic devices in obese patients can predict cardiovascular events as accurately as BP measured with the traditional auscultatory technique will shed light on this controversial issue.
Considerations for Future Development of Cuff and Bladders
Given the problems outlined above, there is a need for devices that make use of cuffs and bladders with appropriate characteristics. Manufacturers should pay special attention to the size and shape of the bladders and to the material used for cuffs. Semi‐rigid cuffs should be increasingly used for self‐BP measurement because they ensure that the proper amount of tension is applied for placement of the cuff. Elderly persons in particular often have problems in wrapping the cuff correctly around the arm. With cuffs made of soft material, it is more difficult for the user to apply the optimal amount of tension, and this may result in improper wrapping. Placing a flexible compliant laminate in the cuff, with an amount of tension pre‐set by the manufacturer, may provide accurate BP measurements without the intervention of the user. Devices for clinical use may have soft cuffs because the BP measurement is performed under the supervision of health care personnel. Soft cuffs also have better durability, are less bulky, and are lower in cost. However, the use of conically shaped bladders in small cuffs may be preferable if they have to be applied on large arms. 24
To verify the appropriateness of these assumptions, a series of studies should be implemented. The appropriate slant angle for conical cuffs should be calculated from the arm characteristics in large samples, with arm circumferences ranging from 22 cm to 50 cm. Cylindrical and conical bladders of different size and shape should be constructed and compared in the various arm size classes, studying the influence of sex, age, adiposity, and BP level. Cuffs of soft and rigid material containing the same type of bladders should be compared either under the supervision of the clinician or by the patient at home. This would allow physicians to ascertain whether semi‐rigid cuffs are more reliable than soft cuffs in real‐life situations.
In the interest of continuous technologic improvement, there should be a positive and close interaction between the validation centers and the manufacturers of the devices. Protocols should not restrict such exchange. For instance, after a negative stage 1 result of a validation, the manufacturer should have the possibility to adjust the device and resubmit it within a given time span, with the overall target of an improved performance of the instrumentation and a better product at the end. Only if such possibility is waived, or the modified device fails the study criteria, a negative publication should be the consequence to document that the device has failed and is not recommended for health care purposes.
Acknowledgments
Disclosures: P. Palatini made device validation studies for A&D, Heine, Microlife, Panasonic, and UEBE companies. G. Frick is a Senior Vice President of Microlife AG in charge of product development and clinical application and member of the International Standard Committees for Blood Pressure Measurement (ISO and AAMI). The authors report no specific funding in relation to this paper.
References
- 1. O’Brien E, Asmar R, Beilin L, et al; on behalf of the European Society of Hypertension Working Group on Blood Pressure Monitoring . European society of hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. [DOI] [PubMed] [Google Scholar]
- 2. Pickering TG, James GD, Boddie C, et al. How common is white coat hypertension? JAMA. 1988;259:255–258. [PubMed] [Google Scholar]
- 3. Palatini P. Reliability of ambulatory blood pressure monitoring. Blood Press Monit. 2001;6:291–295. [DOI] [PubMed] [Google Scholar]
- 4. Pickering TG, Hall JE, Appel LJ, et al; Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research . Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142–161. [DOI] [PubMed] [Google Scholar]
- 5. Palatini P. Ambulatory and home blood pressure measurement: complementary rather than competitive methods. Hypertension. 2012;59:2–4. [DOI] [PubMed] [Google Scholar]
- 6. Parati G, Stergiou GS, Asmar R, et al; ESH Working Group on Blood Pressure Monitoring . European society of hypertension guidelines for blood pressure monitoring at home: a summary report of the second international consensus conference on home blood pressure monitoring. J Hypertens. 2008;26:1505–1526. [DOI] [PubMed] [Google Scholar]
- 7. Yarows AS, Patel K, Brook R. Rapid oscillometric blood pressure measurement compared to conventional ocillometric measurement. Blood Press Monit. 2001;6:145–147. [DOI] [PubMed] [Google Scholar]
- 8. European Committee for Standardization . European Standard EN 1060‐3 1997 (British Standard BSEN 1060‐3: 1997). Specification for Noninvasive Sphygmomanometers. Part 3. Supplementary Requirements for Electro‐Mechanical Blood Pressure Measuring Systems. Brussels, Belgium: European Committee for Standardization; 1997. [Google Scholar]
- 9. Association for the Advancement of Medical Instrumentation . American National Standard for Electronic or Automated Sphygmomanometers: ANSI/AAMI SP10‐1993. Arlington, VA: AAMI; 1993. [Google Scholar]
- 10. O’Brien E, Petrie J, Littler WA, et al. The British Hypertension Society protocol for the evaluation of blood pressure measuring devices. J Hypertens. 1993;11(suppl 2):S43–S63. [DOI] [PubMed] [Google Scholar]
- 11. O’Brien E, Pickering T, Asmar R, et al; Working Group on Blood Pressure Monitoring of the European Society of Hypertension . European Society of Hypertension international protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2002;7:3–17. [DOI] [PubMed] [Google Scholar]
- 12. O’Brien E, Atkins N, Stergiou G, et al; on behalf of the Working Group on Blood Pressure Monitoring of the European Society of Hypertension . European Society of Hypertension international protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit. 2010;15:23–38. [DOI] [PubMed] [Google Scholar]
- 13. Omboni S, Costantini C, Pini C, et al. PA.NET international quality certification protocol for blood pressure monitors. Blood Press Monit. 2008;13:285–289. [DOI] [PubMed] [Google Scholar]
- 14. Mengden T, Hernandez Medina RM, Beltran B, et al. Reliability of reporting self‐measured blood pressure values by hypertensives patients. Am J Hypertens. 1998;11:1413–1417. [DOI] [PubMed] [Google Scholar]
- 15. Kikuya M, Ohkubo T, Metoki H, et al. Day‐by‐day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension. 2008;52:1045–1050. [DOI] [PubMed] [Google Scholar]
- 16. Matsui Y, Eguchi K, Shibasaki S, et al. Association between the morning‐evening difference in home blood pressure and cardiac damage in untreated hypertensive patients. J Hypertens. 2009;27:712–720. [DOI] [PubMed] [Google Scholar]
- 17. Stergiou GS, Giovas PP, Gkinos CP, et al. A tool for reliable self‐home blood pressure monitoring designed according to the European Society of Hypertension recommendations: the Microlife WatchBP Home monitor. Blood Press Monit. 2007;12:127–131. [DOI] [PubMed] [Google Scholar]
- 18. O’Brien E. A century of confusion: which bladder for accurate blood pressure measurement? [review]. J Hum Hypertens. 1996;10:565–572. [PubMed] [Google Scholar]
- 19. Palatini P, Parati G. Blood pressure measurement in very obese patients: a challenging problem. J Hypertens. 2011;29:425–429. [DOI] [PubMed] [Google Scholar]
- 20. Alpert BS. Cuff width and accuracy of measurement of blood pressure. Blood Press Monit. 2000;5:151–152. [DOI] [PubMed] [Google Scholar]
- 21. Huige MC. Reliability of blood pressure measurement on fat upper arms. Ther Umsch. 1982;39:87–91. [PubMed] [Google Scholar]
- 22. Maxwell GF, Pruijt JF, Arntzenius AC. Comparison of the conical cuff and the standard rectangular cuffs. Int J Epidemiol. 1985;14:468–472. [DOI] [PubMed] [Google Scholar]
- 23. Watson S, Aguas M, Bienapfl T, et al. Postanesthesia patients with large upper arm circumference: is use of an “extra‐long” adult cuff or forearm cuff placement accurate? J Perianesth Nurs. 2011;26:135–142. [DOI] [PubMed] [Google Scholar]
- 24. Palatini P, Benetti E, Fania C, et al. Rectangular cuffs may overestimate blood pressure in subjects with large conical arms. J Hypertens. In press [DOI] [PubMed] [Google Scholar]
- 25. O’Brien E. What to do when faced with an unmeasurable ambulatory blood pressure? J Hypertens. 2011;29:451–453. [DOI] [PubMed] [Google Scholar]
- 26. Bonso E, Dorigatti F, Palatini P. Accuracy of the BP A100 blood pressure measuring device coupled with a single cuff with standard‐size bladder over a wide range of arm circumferences. Blood Press Monit. 2009;14:216–219. [DOI] [PubMed] [Google Scholar]
- 27. Stergiou GS, Tzamouranis D, Nasothimiou EG, et al. Can an electronic device with a single cuff be accurate in a wide range of arm size? Validation of the Visomat Comfort 20/40 device for home blood pressure monitoring J Hum Hypertens. 2008;22:796–800. [DOI] [PubMed] [Google Scholar]
- 28. Bonso E, Saladini F, Zanier A, et al. Accuracy of a single rigid conical cuff with standard‐size bladder coupled to an automatic oscillometric device over a wide range of arm circumferences. Hypertens Res. 2010;33:1186–1191. [DOI] [PubMed] [Google Scholar]
- 29. Lan H, Al‐Jumaily AM, Lowe A, et al. Effect of tissue mechanical properties on cuff‐based blood pressure measurements. Med Eng Phys. 2011;33:1287–1292. [DOI] [PubMed] [Google Scholar]
- 30. Redon J. Hypertension in obesity. Nutr Metab Cardiovasc Dis. 2001;11:344–353. [PubMed] [Google Scholar]


