Abstract
J Clin Hypertens (Greenwich). 2012; 14:637–643. © 2012 Wiley Periodicals, Inc.
The authors retrospectively examined data from 3 surveys on hypertension according to the 2010 Chinese Guidelines for the Management of Hypertension. These surveys were conducted in 1991, 1999, and 2007, and included 85,371 individuals 18 years and older who were living in Shandong Province, China. Age‐standardized prevalent hypertension increased from 15.6% in 1991 to 17.3% in 1999 and 32.7% in 2007 (both P<.0001). The ascending prevalence can be partially explained by increasing body weight. Among individuals with hypertension, awareness increased significantly from 27.8% in 1991 to 39.1% in 1999 and 49.2% in 2007. The proportion of pharmacologic treatment also considerably improved, with the estimate of 12.9%, 28.1%, and 43.3% in the 3 surveys, respectively. Hypertension control increased from 3.0% to 4.4% to 7.1% in the past 20 years. The upward trend in blood pressure control was mostly attributable to a rise among men and persons at middle age. This study suggests that the prevalence of hypertension increased in the Shandong population from 1991 to 2007. Although substantially improved, control rates were still unacceptably low. Comprehensive strategies are urgently required to put into practice for the management of hypertension in Shandong Province, China.
Cardiovascular disease (CVD) is the leading cause of death in the world, accounting for 30% of deaths globally. It was estimated that 17.5 million deaths were attributable to CVD worldwide in 2005 and this number will increase to 20 million in 2015. 1 Although the age‐adjusted CVD mortality rate and prevalence of major cardiovascular risk factors have declined in economically developed countries due to aggressive application of preventive interventions, the burden of CVD is substantially increasing in some developing regions where socioeconomy has changed rapidly, including China. 2
Hypertension is not only an important modifiable risk factor for CVD, but also a major public health problem in both developed and developing countries. More than one quarter of adults had hypertension in 2000 worldwide, and this was predicted to be 29.2% by 2025, with almost three quarters in developing countries. 3 The estimated number of adult patients with hypertension in 2000 was 181.6 million in China, and modeled projections indicate an increase to 299.2 million by 2025. 4 The prevalence of hypertension in Chinese adult populations increased from 13.6% in 1991 to 18% in 2002, 5 , 6 but the ratio of controlled to treated individuals were similarly lower, at about 1:4. This situation was even worse in rural China. The prevalence of hypertension in rural residents aged 35 to 74 years was 30.6%, and only 7.3% achieved blood pressure (BP) control. 7
We have participated in the 1991 China National Hypertension Survey 5 and the 1999 China National Hypertension Survey Epidemiology Follow‐Up Study. 8 In 2007, we conducted a cross‐sectional survey in adults on the epidemiology of hypertension in Shandong Province. To delineate the epidemiologic trends and facilitate the development of appropriate strategies for detection and prevention of hypertension, we examined the changes in prevalence, awareness, treatment, and control of hypertension through a retrospective analysis of the data in 1991, 1999, and 2007 in Shandong Province according to the 2010 Chinese Guidelines for the Management of Hypertension. 9
Methods
Study Design
We analyzed the data of Shandong Province retrospectively in this article. They were from the third China National Hypertension Survey 1991, the China National Hypertension Survey Epidemiology Follow‐Up Study 1999, and a cross‐sectional survey 2007. A multi‐stage random cluster sampling strategy was used to collect information by well‐trained physicians and nurses in a standardized interview and physical examination. Specifically, in the first stage, we selected districts or counties in Shandong Province. Secondly, a sampling of neighborhoods or townships was done from districts or counties. The third stage involved the selection of residential committees or villages from neighborhoods or townships. Finally, all households within residential committees or villages were visited. The protocol was approved by the Shandong Academy of Medical Sciences ethics review board. All participants provided written informed consent.
BP Measurements and Definitions
The methodology of BP measurements was available elsewhere. 5 , 8 , 10 , 11 Quality control was ensured with proofreading of health care professionals and statistical staff.
BP on the right arm was measured with a standard mercury sphygmomanometer and appropriately sized cuff after the participant rested in a sitting position for 5 minutes. Participants were instructed to avoid alcohol, coffee or tea, cigarette smoking, and exercise for at least 30 minutes before BP measurement. Systolic BP (SBP) and diastolic BP (DBP) were recorded at the appearance and the disappearance of Korotkoff sound, respectively. For the data from 1991 and 2007 where 3 readings were available, the average of the second and third values was used for analysis. In the survey from 1999, only 1 measurement was obtained. Other methods employed in the 3 surveys were similar.
Hypertension was defined as a mean SBP ≥140 mm Hg and/or mean DBP ≥90 mm Hg or self‐reported current use of antihypertensive medication. Awareness of hypertension was defined as participants having been informed at least once by a health care professional that they had hypertension. Hypertensive patients were categorized as treatment if they were taking a prescribed medicine for management of hypertension. Control of hypertension was defined as antihypertensive treatment associated with mean SBP <140 mm Hg and mean DBP <90 mm Hg. Although current guidelines in China 9 recommend a lower goal of BP <130/80 mm Hg for diabetic patients, recent evidence from clinical trials suggests that an aggressive BP‐lowering therapy is not superior to a standard therapy targeting SBP <140 mm Hg in preventing cardiovascular events. 12 , 13 Therefore, we focus exclusively on the goal of SBP <140 mm Hg and DBP <90 mm Hg. Family history was documented as positive if ≥1 first‐degree relatives have been diagnosed as having hypertension.
Data Collection on Lifestyle Risk Factors and Medical History
Lifestyle risk factors and medical history were recorded according to the self‐report by participants. Cigarette smoking was defined as having smoked at least one cigarette per day for ≥1 year. Alcohol consumption was defined as drinking alcohol at least 12 times during the previous year. Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters. According to the Chinese‐specific criteria, 6 body size was classified into 4 BMI categories: underweight, defined as BMI <18.5 kg/m2; normal weight, 18.5 kg/m2 to <24 kg/m2; overweight, 24 kg/m2 to <28 kg/m2; and obesity, ≥28 kg/m2. Respondents were stratified into 6 age groups: 18 to 29, 30 to 39, 40 to 49, 50 to 59, 60 to 69, and ≥70 years.
Statistical Analysis
SPSS 17.0 for Windows (SPSS Inc, Chicago, IL) was used for data analysis. Participant characteristics were summarized as mean±standard deviation or numbers and percentages as appropriate. Comparisons of the differences in continuous variables were performed using one‐way analysis of variance, while those of categorical variables were treated with chi‐square test. Correlation was determined to assess the association between BP levels and the other parameters of cardiovascular risk factors. A two‐sided P value <.05 was considered statistically significant.
Results
Sociodemographic Characteristics of Study Sample
A total of 85,371 individuals 18 years and older were included in this report, of which 38,146 were from the survey of 1991, 25,532 from 1999, and 21,693 from 2007. Table I presents the sociodemographic characteristics of participants, including age, sex, BP levels, family history of hypertension, body weight, lifestyle, and education. The averages of BP levels and BMI increased with time, which may represent the rapid economic growth in China. The proportion of male smokers was at least 10 times higher than that of female smokers and the estimate for drinkers was 25.
Table I.
Characteristics of Participants in Surveys of 1991, 1999, and 2007
| 1991 (n=38,146) | 1999 (n=25,532) | 2007 (n=21,693) | P for Trend | |
|---|---|---|---|---|
| Age, y | 46.7±15.8 | 43.8±13.8 | 52.9±12.0 | <.0001 |
| Sex | <.0001 | |||
| Men | 18,495 (48.5) | 12,354 (48.4) | 8385 (38.7) | |
| Women | 19,651 (51.5) | 13,178 (51.6) | 13,308 (61.3) | |
| Systolic blood pressure | 119.7±19.2 | 124.9±14.9 | 140.1±23.3 | <.0001 |
| Diastolic blood pressure | 73.8±11.1 | 79.0±8.9 | 84.5±12.4 | <.0001 |
| Family history of hypertension | 6783 (17.8) | 5840 (22.9) | 2356 (10.9) | <.0001 |
| Body mass index | 22.5±3.3 | 23.4±2.6 | 24.7±3.7 | <.0001 |
| Underweight | 2892 (7.6) | 517 (2.0) | 702 (3.2) | <.0001 |
| Normal weight | 24,560 (64.4) | 15,383 (60.2) | 9016 (41.6) | |
| Overweight | 8405 (22.0) | 8387 (32.8) | 8187 (37.7) | |
| Obesity | 2289 (6.0) | 1245 (4.9) | 3788 (17.5) | |
| Cigarette smoking | 12,177 (31.9) | 6799 (26.6) | 3744 (17.3) | <.0001 |
| Men | 11,034 (59.7) | 6300 (51.0) | 3555 (42.4) | |
| Women | 1143 (5.8) | 499 (3.8) | 189 (1.4) | |
| Alcohol consumption | 7762 (20.3) | 5367 (21.0) | 3674 (16.9) | <.0001 |
| Men | 7535 (40.7) | 5155 (41.7) | 3564 (42.5) | |
| Women | 227 (1.2) | 212 (1.6) | 110 (0.8) | |
| Education | <.0001 | |||
| Illiterate | 9116 (23.9) | 2521 (9.9) | 4567 (21.1) | |
| Primary school | 7410 (19.4) | 9499 (37.2) | 8375 (38.6) | |
| Middle school | 11,947 (31.3) | 12,540 (49.1) | 6967 (32.1) | |
| High school | 7632 (20.0) | 946 (3.7) | 1380 (6.4) | |
| College/university or above | 2041 (5.4) | 26 (0.1) | 404 (1.9) |
The values are expressed as mean±standard deviation or number (percentage).
Prevalence of Hypertension
In 1991, 15.6% of the population had hypertension, with higher prevalence among men than among women (16.8% vs 14.4%; P<.0001). The prevalence was 19.5% in 1999 (19.7% for men vs 19.3% for women; P=.481) and 55.3% in 2007 (58.6% for men vs 53.2% for women; P<.0001). If the prevalence in 1991 was regarded as a reference, the age‐standardized prevalence of hypertension was 17.3% (18.3% for men vs 16.1% for women; P<.0001) in 1999 and 32.7% (36.3% for men vs 29.9% for women; P<.0001) in 2007. In comparison with the data from 1991, the relative increases of age‐standardized prevalence in the later two surveys were 11.1% and 110.2% (both P<.0001), respectively. The elevated prevalence of hypertension may be related to the increasing prevalence of overweight/obesity. For both sexes, the prevalence of hypertension increased with age, except that in the subgroups older than 70 years in 1999 (Table II).
Table II.
Prevalence of Hypertension in the Adult Population of Shandong Province, China, From the 1991, 1999, and 2007 Surveys
| Population Group | 1991 | 1999 | 2007 | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Total | 5936 | 15.6 | 4976 | 19.5 | 11,993 | 55.3 |
| Men | 3114 | 16.8 | 2430 | 19.7 | 4913 | 58.6 |
| Women | 2822 | 14.4 | 2546 | 19.3 | 7080 | 53.2 |
| Total, age, y | ||||||
| 18–29 | 509 | 4.4 | 179 | 4.2 | 102 | 14.1 |
| 30–39 | 763 | 7.9 | 597 | 8.9 | 702 | 28.5 |
| 40–49 | 1030 | 15.7 | 1296 | 19.4 | 1911 | 44.3 |
| 50–59 | 1392 | 27.8 | 1292 | 32.5 | 4385 | 58.2 |
| 60–69 | 1370 | 38.5 | 1090 | 42.2 | 3380 | 70.8 |
| 70+ | 872 | 45.9 | 522 | 39.3 | 1513 | 80.3 |
| Men, age, y | ||||||
| 18–29 | 397 | 7.0 | 122 | 5.1 | 47 | 17.5 |
| 30–39 | 522 | 11.0 | 355 | 10.9 | 331 | 36.0 |
| 40–49 | 528 | 16.6 | 625 | 19.8 | 792 | 50.9 |
| 50–59 | 674 | 28.0 | 631 | 33.2 | 1762 | 60.5 |
| 60–69 | 662 | 39.3 | 507 | 44.0 | 1373 | 69.8 |
| 70+ | 331 | 40.6 | 190 | 38.9 | 608 | 79.9 |
| Women, age, y | ||||||
| 18–29 | 112 | 1.9 | 57 | 3.1 | 55 | 12.1 |
| 30–39 | 241 | 4.9 | 242 | 7.1 | 371 | 24.0 |
| 40–49 | 502 | 14.8 | 671 | 19.0 | 1119 | 40.6 |
| 50–59 | 718 | 27.6 | 661 | 31.9 | 2623 | 56.7 |
| 60–69 | 708 | 37.9 | 583 | 40.7 | 2007 | 71.4 |
| 70+ | 541 | 49.9 | 332 | 39.6 | 905 | 80.5 |
Awareness, Treatment, and Control of Hypertension
In 1991, less than one third of the individuals with hypertension were aware of their condition. This rate increased to two fifths in 1999 (P<.0001) and nearly half in 2007 (P<.0001). The awareness was significantly higher for women than for men (Figure 1A). For each survey and both sexes, the awareness was lowest in the subgroup of 18 to 29 year olds. It peaked at the 50s age range in 1991 and at the 60s age range in 1999 and 2007 (Figure 2A).
Figure 1.
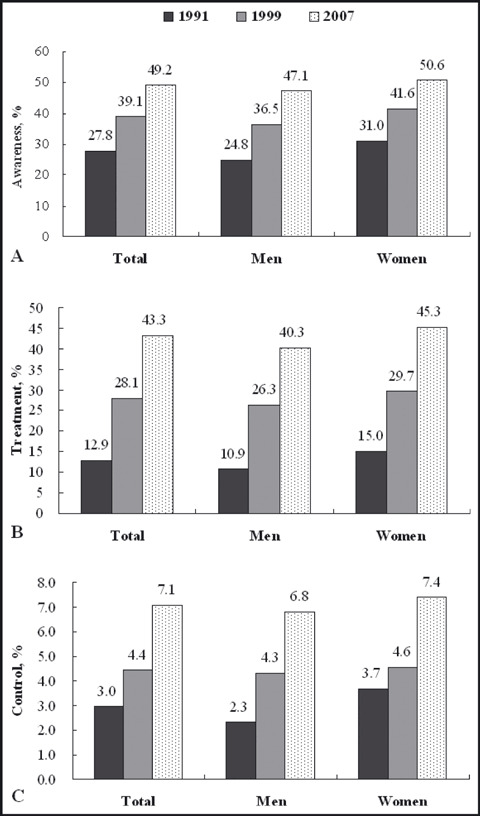
Total and sex‐specific awareness, treatment, and control of hypertension in the adult population of Shandong Province, China. The awareness as well as treatment and control of hypertension was significantly different between surveys among the total or sex‐specific populations (P<.01).
Figure 2.
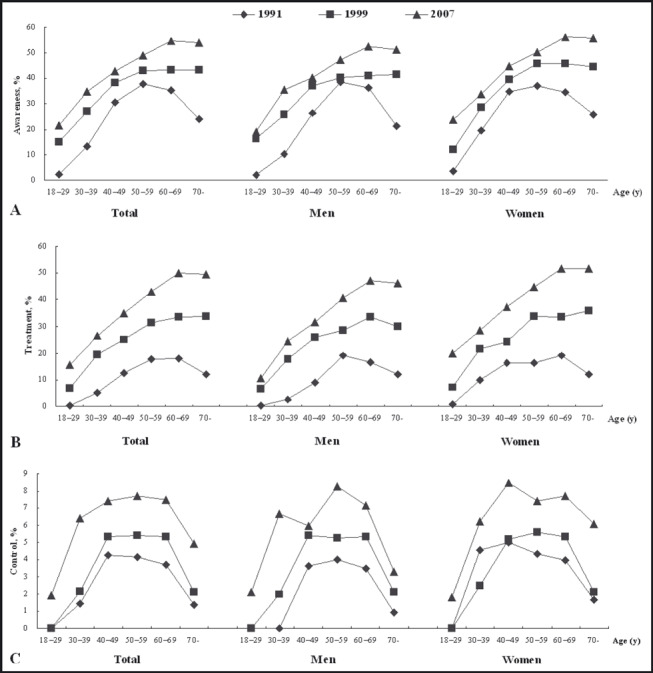
Age‐specific awareness (A), treatment (B), and control (C) of hypertension in the adult population of Shandong Province, China.
The proportion of hypertensive patients receiving treatment improved notably with age. In 1991, only about one eighth of hypertensive individuals were treated with medications. However, it approximately doubled in 1999 (P<.0001) and tripled in 2007 (P<.0001). The treatment was remarkably lower for men than for women in each survey (Figure 1B). This proportion was equivalent to almost half of those aware of their hypertension in 1991, around 70% in 1999, and nearly 90% in 2007. The greatest increment was in the subgroup of those 70 years and older for both sexes (Figure 2B).
In 1991, only 3.0% patients with hypertension had their BP controlled. The control rate increased by 49.7% (P<.0001) in 1999 (86.8% for men, P<.0001; 23.6% for women, P=.009) and by 139.4% (P<.0001) in 2007 (14.0% for men and 100.7% for women, both P<.0001). The difference of control was significant between sexes in 1991 (P=.002), but it disappeared in 1999 (P=.687) and 2007 (P=.203). Although relative increment was substantial in men, the absolute control rate was still lower than that in women (Figure 1C). Unexpectedly, among the patients who were treated with antihypertensive medications, the control rate was about 23.1% in 1991, but 15.8% in 1999 and 16.5% in 2007. As for the age‐specific subgroups, the control rate in each survey demonstrated a pattern of inverted U curve. Pharmacologic intervention was more effective in the hypertensive patients at middle age (Figure 2C).
Relationship Between BP and BMI
From 1991 to 2007, both the prevalence of hypertension and the proportion of overweight/obesity increased over time. In each survey and for both sexes, BMI was positively correlated with BP levels. When the data of all participants were pooled for analysis, Pearson coefficient was 0.298 between BMI and SBP (0.280 for men and 0.317 for women; all P<.0001) and 0.337 between BMI and DBP (0.342 for men and 0.350 for women; all P<.0001). If the patients taking current antihypertensive agents were excluded and only the data of untreated hypertensive and normotensive individuals were analyzed, Pearson coefficient was 0.256 between BMI and SBP (0.248 for men and 0.273 for women; all P<.0001) and 0.307 between BMI and DBP (0.317 for men and 0.319 for women; all P<.0001). The association was stronger for DBP than SBP, and a closer linear relationship was found in women than in men.
Discussion
This study indicates that the prevalence of age‐standardized hypertension for both men and women continues to rise alarmingly in the adult population of Shandong Province in the recent 2 decades. These findings are consistent with the data of China National Surveys from 1991 to 2002. 5 , 6 The InterASIA Collaborative Group reported that 27.2% of the Chinese adult population aged 35 to 74 years had hypertension in 2000 to 2001. Results from a cross‐sectional study conducted in 2007 by Li and colleagues 14 revealed that the prevalence of hypertension was 43.8% in rural residents 25 years and older. A similar trend was also found in India. Data from a small‐sample investigation demonstrated that in the North Indian urban population, the age‐ and sex‐adjusted prevalence of hypertension increased by 30% from 2000 to 2005. 15 However, during the corresponding period, this situation was improved greatly in some developed countries. For example, the prevalent hypertension in the United States increased from 23.9% in 1988–1994 to 28.5% in 1999–2000, but came to a halt at 29.0% in 2007–2008, 16 suggesting achievement in the substantial efforts of preventing hypertension.
We find that the rising prevalence of hypertension in Shandong Province is paralleled by the prevalent trend of overweight/obesity. In each survey and for both sexes, a moderate and positive linear relationship was confirmed between BMI and BP levels, regardless of whether the data of the individuals whose BP levels were modified with antihypertensive medications were included for analysis. According to the data from 2002 China National Nutrition and Health Survey, the prevalence of overweight and obesity in adults 18 and older was 22.8% and 7.1%, respectively. 17 Although the mean BMI in Chinese citizens was much lower than that in Western populations, it increased significantly in the late 20th century. Intake of high‐calorie food and sedentary lifestyle are major contributors to weight gain. The presence of obesity and overweight predicts the development of hypertension. 18 , 19 Even worse, the mean BMI in Chinese children and adolescents aged 7 to 17 years increased by 0.9 kg/m2 from 1991 to 2006, and the prevalence of overweight and obesity increased from 5.2% to 13.2%. 20 Such temporal trends impose a huge challenge for the prevention of adult hypertension in the next 10 years. Weight loss by means of a healthful diet and physical activity is associated with a notable reduction in BP. 21 , 22
Different from the disappointing tendency of prevalence in the Shandong population, the trends in awareness, treatment, and control of hypertension improved from 1991 to 2007. In recent 20 years, the diagnosis and treatment of hypertension in Mainland China was under the supervision of guidelines on hypertension issued by the World Health Organization and International Society of Hypertension 23 , 24 with some adaptation or by the Chinese Hypertension League. 10 , 11 These guidelines promoted the management of hypertension by offering available and appropriate recommendations to health care providers. Meanwhile, the access to health care in China was remarkably improved in the past decade. Insurance coverage increased from 7% in 1999 to 96% in 2011, 25 , 26 which greatly contributed to the improvements in awareness and treatment of hypertension. Nevertheless, a huge gap exists in dealing with hypertension between China and Western countries. In the United States, the Healthy People 2010 goal of controlling BP in 50% of all individuals with hypertension was achieved 2 years in advance. 16 Public health policies should be reinforced to raise the awareness and intervention of hypertension in China.
The improvement of awareness in youth was remarkable over time. The proportion of younger individuals who were aware of their hypertension and treated with medications was still less than other age groups, however, which resulted in a lower control rate. In general, young people seldom feel ill enough to see a doctor. It is difficult to perceive the elevated BP without any symptoms or physical examinations. On the other hand, more hypertensive patients 60 years or older realized their condition and received pharmacologic therapy, but the control rate is paradoxically lower in this group than that in the middle‐aged group. Aging and concomitant diseases are clinical characteristics associated with resistant hypertension. 27 Achievement of BP control is one of the most important targets for public health policy and clinical practice. Complementary programs are in urgent demand to raise the awareness and treatment in the young population and enlarge the proportion of patients treated and controlled in the elderly.
In comparison with the findings in women, the prevalence of hypertension was higher in men, while the BP control as well as awareness and treatment was lower. In addition to the protective role of endogenous estrogen against hypertension, 28 cigarette smoking and alcohol consumption explain this disparity between sexes to some extent. As indicated in Table I, the proportion of smokers was exceedingly higher in men than in women, and so was that of drinkers. Recent cross‐sectional studies suggested that cigarette smoking and excessive alcohol consumption are both associated with elevated BP and risk of hypertension in the Chinese adult population. 29 , 30 Even so, when compared with the trends from 1991 to 2007 in women, the acceleration of awareness, treatment, and control rate was slightly greater in men.
Limitations
This retrospective analysis was conducted to delineate the epidemiological trends of adult hypertension in 3 large representative samples of the Shandong population. Stringent procedures were used to ensure high quality in data collection and processing. However, several limitations should be taken into consideration. Firstly, some subpopulations were not sampled in each survey, such as pregnant women, hospitalized patients, prisoners, and military personnel, which may undermine the estimates related to hypertension. Secondly, a small minority of individuals were diagnosed with stage 1 hypertension. Underestimation bias may exist if their BP falls into the high‐normal category or was controlled with nonpharmacologic therapy at the time of survey. On the other hand, inclusion of white‐coat hypertension results in potential overestimates. Patients with these conditions are of particular concern in view of the fact that they are at an increased risk of sustained hypertensive state and poor prognosis. 31 Moreover, the guidelines recommend that the diagnosis and classification of hypertension should be made on the basis of 3 measurements from different days, 9 and patients with various stages of hypertension should be followed‐up for confirmation. 32 A single‐visit BP measurement may overestimate the prevalence and underestimate the control rate of hypertension. Finally, the first reading of BP is often higher than the actual level. It is advisable to attenuate the physician effect on BP values by using the average of the second and third readings for analysis. 16 However, only one BP reading was available in the survey from 1999.
Conclusions
The overall trend of hypertension control was upward from 1991 to 2007, but the rates were far from acceptable. Meanwhile, the age‐standardized prevalence of hypertension doubled, driven primarily by a rise in BMI. Shandong Province is located in the east of North China. The dietary intake of sodium is significantly higher in northern residents than those living in the southern areas of China. Salt consumption accounts partially for the geographic variations in hypertension prevalence. 33 , 34 In addition, cigarettes and alcohol might contribute to the difference of hypertension between sexes. Population‐based health education, dietary and lifestyle modification, and pharmacologic therapy are all effective measures to reduce the prevalence and increase the control rate of hypertension. Comprehensive strategies are urgently required to focus on maintaining optimal body weight, lowering sodium intake, abstaining from smoking and drinking in men, raising awareness and treatment of hypertension in youth, and implementing aggressive antihypertensive interventions in the elderly.
Disclosures: This study was supported by the National Natural Science Foundation of China (grant No. 30900608) and the Shandong Provincial Natural Science Foundation of China (grant No. ZR2010HQ048). The authors have no conflicts of interest to disclose.
References
- 1. Hong Y. Burden of cardiovascular disease in Asia: big challenges and ample opportunities for action and making a difference. Clin Chem. 2009;55:1450–1452. [DOI] [PubMed] [Google Scholar]
- 2. Sanderson JE, Mayosi B, Yusuf S, et al. Global burden of cardiovascular disease. Heart. 2007;93:1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 4. Perkovic V, Huxley R, Wu Y, et al. The burden of blood pressure‐related disease: a neglected priority for global health. Hypertension. 2007;50:991–997. [DOI] [PubMed] [Google Scholar]
- 5. Tao S, Wu X, Duan X, et al. Hypertension prevalence and status of awareness, treatment and control in China. Chin Med J (Engl). 1995;108:483–489. [PubMed] [Google Scholar]
- 6. Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–2686. [DOI] [PubMed] [Google Scholar]
- 7. Yang J, Lu F, Zhang C, et al. Prevalence of prehypertension and hypertension in a Chinese rural area from 1991 to 2007. Hypertens Res. 2010;33:331–337. [DOI] [PubMed] [Google Scholar]
- 8. Gu D, Kelly TN, Wu X, et al. Blood pressure and risk of cardiovascular disease in Chinese men and women. Am J Hypertens. 2008;21:265–272. [DOI] [PubMed] [Google Scholar]
- 9. Liu LS; Writing Group of 2010 Chinese Guidelines for the Management of Hypertension . 2010 Chinese guidelines for the management of hypertension [in Chinese]. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579–615. [PubMed] [Google Scholar]
- 10. Liu LS, Gong LS; Writing Group of Chinese Guidelines for the Management of Hypertension . 1999 Chinese guidelines for the management of hypertension [in Chinese]. Chin J Hypertens. 2000;8:94–104. [Google Scholar]
- 11. Committee for Revision of Chinese Guidelines for Prevention and Treatment of Patients with Hypertension . Chinese guidelines for prevention and treatment of patients with hypertension [in Chinese]. Chin J Hypertens. 2005;134(Suppl):S2–S41. [Google Scholar]
- 12. ACCORD Study Group , Cushman WC, Evans GW, et al. Effects of intensive blood‐pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cooper‐DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li H, Meng Q, Sun X, et al. Prevalence, awareness, treatment, and control of hypertension in rural China: results from Shandong Province. J Hypertens. 2010;28:432–438. [DOI] [PubMed] [Google Scholar]
- 15. Bansal M, Shrivastava S, Mehrotra R, et al. Time‐trends in prevalence and awareness of cardiovascular risk factors in an asymptomatic North Indian urban population. J Assoc Physicians India. 2009;57:568–573. [PubMed] [Google Scholar]
- 16. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 17. Wu YF, Ma GS, Hu YH, et al. The current prevalence status of body overweight and obesity in China: data from the China National Nutrition and Health Survey [in Chinese]. Zhonghua Yu Fang Yi Xue Za Zhi. 2005;39:316–320. [PubMed] [Google Scholar]
- 18. Zhou B, Wu Y, Yang J, et al. Overweight is an independent risk factor for cardiovascular disease in Chinese populations. Obes Rev. 2002;3:147–156. [DOI] [PubMed] [Google Scholar]
- 19. Liu L, Ikeda K, Chen M, et al. Obesity, emerging risk in China: trend of increasing prevalence of obesity and its association with hypertension and hypercholesterolaemia among the Chinese. Clin Exp Pharmacol Physiol. 2004;31(suppl 2):S8–S10. [DOI] [PubMed] [Google Scholar]
- 20. Cui Z, Huxley R, Wu Y, et al. Temporal trends in overweight and obesity of children and adolescents from nine Provinces in China from 1991–2006. Int J Pediatr Obes. 2010;5:365–374. [DOI] [PubMed] [Google Scholar]
- 21. Stevens VJ, Obarzanek E, Cook NR, et al. Long‐term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134:1–11. [DOI] [PubMed] [Google Scholar]
- 22. Neter JE, Stam BE, Kok FJ, et al. Influence of weight reduction on blood pressure: a meta‐analysis of randomized controlled trials. Hypertension. 2003;42:878–884. [DOI] [PubMed] [Google Scholar]
- 23. Guidelines Sub‐Committee . 1993 guidelines for the management of mild hypertension: memorandum from a World Health Organization/International Society of Hypertension meeting. J Hypertens. 1993;11:905–918. [DOI] [PubMed] [Google Scholar]
- 24. Guidelines Subcommittee . 1999 World Health Organization‐International Society of Hypertension Guidelines for the Management of Hypertension. J Hypertens. 1999;17:151–183. [PubMed] [Google Scholar]
- 25. Barber SL, Yao L. Development and status of health insurance systems in China. Int J Health Plann Manage. 2011;26:339–356. [DOI] [PubMed] [Google Scholar]
- 26. Meng Q, Xu L, Zhang Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross‐sectional study. Lancet. 2012;379:805–814. [DOI] [PubMed] [Google Scholar]
- 27. Persell SD. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension. 2011;57:1076–1080. [DOI] [PubMed] [Google Scholar]
- 28. Ashraf MS, Vongpatanasin W. Estrogen and hypertension. Curr Hypertens Rep. 2006;8:368–376. [DOI] [PubMed] [Google Scholar]
- 29. Ruixing Y, Hui L, Jinzhen W, et al. Association of diet and lifestyle with blood pressure in the Guangxi Hei Yi Zhuang and Han populations. Public Health Nutr. 2009;12:553–561. [DOI] [PubMed] [Google Scholar]
- 30. Zhang WS, Jiang CQ, Cheng KK, et al. Alcohol sensitivity, alcohol use and hypertension in an older Chinese population: the Guangzhou Biobank Cohort Study. Hypertens Res. 2009;32:741–747. [DOI] [PubMed] [Google Scholar]
- 31. Mancia G, Bombelli M, Facchetti R, et al. Long‐term risk of sustained hypertension in white‐coat or masked hypertension. Hypertension. 2009;54:226–232. [DOI] [PubMed] [Google Scholar]
- 32. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 33. Liu Z. Dietary sodium and the incidence of hypertension in the Chinese population: a review of nationwide surveys. Am J Hypertens. 2009;22:929–933. [DOI] [PubMed] [Google Scholar]
- 34. Zhao L, Stamler J, Yan LL, et al. Blood pressure differences between northern and southern Chinese: role of dietary factors: the International Study on Macronutrients and Blood Pressure. Hypertension. 2004;43:1332–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]


