Abstract
J Clin Hypertens (Greenwich). 2012;14:787–791. ©2012 Wiley Periodicals, Inc.
During the past decades, blood pressure (BP) measurement technique has evolved rapidly from the traditionally manual measuring to fully automatic monitoring. In terms of management of BP, there have been tremendous changes from the controlling of daytime BP, nondipping pattern to nocturnal BP (NBP). Since the focus has turned to NBP, a number of dilemmas of NBP measurement have gradually emerged in clinical practice and research settings, including methods for monitoring NBP, different period definition of nocturnal time, different diagnostic thresholds of abnormal NBP, whether to control abnormal NBP, and how to manage abnormal NBP. Currently, these issues have hindered progress in the appropriate management of hypertensive patients. Therefore, the purpose of this review is to concisely discuss the dilemmas of NBP.
Widely used conventional blood pressure (BP) monitoring technique was first described by Riva‐Rocci and Korotkoff more than a century ago. 1 Since ambulatory BP monitoring (ABPM) was originally described more than 40 years ago, 2 however, it is generally accepted that ABPM estimates “true” mean BP and has better correlation with end‐organ damage and cardiovascular outcomes compared with traditional office or clinic BP measurement technique. 3 , 4 , 5 , 6 , 7 , 8 ABPM is increasingly being used for the management of hypertensive patients. 9
It has been 24 years since the dipping phenomenon was first coined by O’Brien and colleagues 10 in The Lancet. In healthy individuals, NBP decreases by 10% to 20% and increases promptly on waking. However, certain abnormal diurnal variation patterns have been described in which the nocturnal fall of BP may be more than 20% (extreme dippers), <10% (nondippers), or even reversed (reverse dippers). Since then, nondipping has been considered an abnormal diurnal rhythm, which is associated with greater cardiovascular 6 and cerebrovascular 11 diseases. Nevertheless, in recent years, evidence has shown that nocturnal BP (NBP) levels rather than circadian BP pattern are more accurate in predicting mortality and morbidity related to BP, independent of mean BP and daytime BP levels. 12 , 13 In 2007, isolated nocturnal hypertension as a potentially novel clinical entity derived from a Chinese population study was examined by Li and colleagues. 14 Through post‐hoc analysis of an international ABPM database, the prevalence of isolated nocturnal hypertension was between 6% and 10.5%. 14
Given the above facts, the indispensible importance of NBP has been widely accepted. 15 The management of NBP has also been generally recognized as essential in controlling abnormal BP. 16 However, there also exist some pivotal and intricate issues on NBP that have not been ideally treated. This review is an attempt to discuss the dilemmas of NBP.
Methods for Monitoring NBP
ABPM typically provides the following three types of information: an estimate of mean BP level, the diurnal rhythm of BP, and BP variability. 17 This fully automatic and theoretical nonsleep disturbance technique is also an ideal method to monitor NBP. To date, it is generally recognized that indirect intermittent ABPM has been the only method for assessing NBP, particularly during overnight sleep. 18 , 19 This monitoring method is considered a gold standard for NBP measurement. 17
This seemingly perfect measurement for NBP, however, has its own vital limitations. First, all currently available ambulatory BP monitors produce sonorous stimuli, which have been found to disturb sleep significantly in a substantial proportion of patients. 20 , 21 , 22 Furthermore, the correlation between NBP derived from ABPM and target organ damage tends to be weaker, with the lowest sleep quality mainly resulting from the repeated cuff inflations during overnight BP monitoring. 21 , 23 Verdecchia and colleagues 24 performed a prospective study with a median follow‐up of 7 years. They concluded that baseline NBP was not only higher in hypertensive patients who perceived sleep deprivation of at least 2 hours, but also lost its ability to predict future cardiovascular events and death. Second, ABPM is not commonly employed in routine clinical practice for evaluating NBP, mainly because of its high cost and inconvenience in performing multiple NBP measurements. 17
Other methods for monitoring NBP have also been investigated. 18 , 19 , 25 Fully automatic home BP devices were used to estimate NBP by a single measurement at 2 am. 18 , 19 Its observed reproducibility in NBP was poor during a 5.9‐day interval. 19 The application of this technique for NBP measurement certainly still requires large‐scale studies. Additionally, the manual device has been used to measure NBP at the point of 3 hours after sleep at the patient’s house. 25 It is suggested that BP recorded during sleep with traditional equipment appears to be reliable in predicting target organ damage. However, this study has only 30 hypertensive patients and absence of the estimation of sleep quality, which can significantly disturb NBP. 25 It is important to recognize that an exact and practical method for the measurement of NBP is essential.
Accurate Period of Nocturnal Time
Up to now, there has been no confirmed period of nocturnal time for NBP. In clinical practice and research settings, there are several non‐uniform approaches to classify the daytime and nighttime periods. One popular and accurate method is to assess nocturnal sleeping time from the patients’ diary entries to determine the nocturnal period. 26 , 27 However, this method may not objectively reflect real sleeping time. Another simple method is to use an arbitrary fixed time, for example, 1 am to 6 am 26 or 11 pm to 7 am 12 for nighttime. An arbitrary definition of nocturnal periods yields a significant degree of inaccuracy particularly in the evaluation of nocturnal dipping status and BP loads. 28 Helen and colleagues 29 also suggest that arbitrary (as opposed to patient‐reported) definitions of nocturnal periods can introduce inaccuracies both in the degree and classification of BP status of patients. In clinical practice, this misinterpretation may lead to inappropriate antihypertensive therapy. Therefore, the nocturnal period is indispensable in clinical practice and research settings.
In the definition of NBP, we always associate “nocturnal” with “sleep” when in fact they are different. We must clearly distinguish one from the other. NBP is generally regarded as the average of BP reading recorded during the period most likely coinciding with sleep time. 30
Diagnostic Thresholds of Nocturnal Hypertension and Hypotension
The relationship between cardiovascular risk and BP is continuous. However, in clinical practice a diagnostic reference frame is necessary to interpret BP values and to classify patients. In terms of nocturnal hypertension, different guidelines have diverse thresholds for the definition of nocturnal hypertension. The 2007 European Society of Hypertension/European Society of Cardiology (ESH/ESC) guidelines defined ≥120/70 mm Hg as nocturnal hypertension and the 2005 American Heart Association’s recommendation 31 as 125/75 mm Hg. The guideline definition of nocturnal hypertension is based on its distribution in normal reference populations. However, outcome‐driven thresholds for nocturnal hypertension provided by the International Database of Ambulatory Blood Pressure in Relation to Cardiovascular Outcome (IDACO) are more than 120/70 mm Hg, which conform to the 2007 ESH/ESC guidelines. Nevertheless, with regard to a critical value, this subtle difference may have tremendous impact on newly diagnosed hypertension.
To date, there are no guidelines to define the standard of nocturnal hypotension. More attention should also be paid to the excessive NBP dipping that is associated with cardiac and cerebrovascular risks. 32 , 33
Although there is no consistent definition of nocturnal time in the guidelines, there exists a seemingly uniform threshold for nocturnal hypertension.
Management of NBP
There is mounting evidence that NBP has been demonstrated to better reflect cardiovascular risk and death than daytime BP in hypertensive patients 8 , 34 , 35 , 36 , 37 and population studies. 7 , 38 , 39 , 40 , 41 Therefore, management of abnormal NBP may have positive potential impact on cardiac and cerebrovascular outcomes. Obviously, NBP should be controlled in a relative ideal range; however, the goal of low limits of NBP has never been widely and generally determined. How can clinicians determine which level of NBP is good for an individual patient? In terms of NBP, there also exists the classic debate on “the lower, the better” vs “J‐shaped.” 42 , 43 Nevertheless, there is no specific study on NBP with regard to this debate. An explicit target for the management of NBP needs more careful consideration before making a decision to treat NBP. 30
Different kinds of related events may require diverse levels of NBP. The Ohasama study demonstrated that NBP was not associated with hemorrhagic stroke but ischemic cardiac and cerebrovascular events. 32 It has been suggested that abnormal NBP should be discreetly controlled toward different risk factors. The difference between ischemic events and hemorrhagic events related to NBP has shown the difficulty in the management of abnormal NBP in patients with complicated disease. Although both all‐cause mortality 34 and cause‐specific cardiovascular events 8 are significantly predicted by NBP, knowledge about particularly cerebral events is sparse. 11
Certain populations may require particular levels of NBP. Nocturnal dipping, ie, lower NBP compared with daytime BP, is a normal phenomenon in healthy younger persons; however, it may be harmful for elderly patients leading to cerebral hypoperfusion 44 and even cerebral events related BP. In the elderly, failure of cerebral autoregulation has shown that even minor falls in BP may lead to cerebral dysfunction, 45 , 46 which means that management of NBP in the elderly should be prudent, especially in patients with ischemic or hemorrhagic cerebral events.
Nocturnal Hypertension
Certainly nocturnal hypertension should be controlled, especially in high‐risk patients. Lowering high NBP can significantly decrease mortality and morbidity associated with BP. 7 , 8 , 35 , 36 , 37 , 38 , 39 , 41 Antihypertensive drugs are the essential in the management of nocturnal hypertension. The efficacy of divergent classes of antihypertensive drugs on NBP has been widely investigated. 47 Some antihypertensive drugs, such as β‐blockers, interrupt the sympathetic nervous system while others, such as angiotensin‐converting enzyme (ACE) inhibitors and angiotensin receptor blockers, interfere with the renin‐angiotensin system. 15 Morgan and Anderson 48 demonstrated that atenolol lowered daytime BP but had no significant effect on NBP and that perindopril lowered NBP more than daytime BP. Sympathetic nervous system likely makes little contribution to NBP. Conversely, ACE inhibitors confer a greater drop in NBP than in daytime BP. 48 According to guidelines on hypertension, there is no general consistency in the management of NBP, particularly in isolated nocturnal hypertension, let alone with different drugs efficacies on abnormal NBP. In the future, more studies on NBP should focus on the efficacies of antihypertensive drugs.
Nocturnal Hypotension
Due to the benefits derived from lowering high NBP, 7 , 8 , 35 , 36 , 37 , 38 , 39 , 41 there is increasing evidence to lower NBP to a much lower level. However, the harm of extreme low NBP should not be ignored in the management of NBP. Excessive low NBP also increases cardiac and cerebrovascular risks. 32 , 33 Extreme low NBP compared with daytime BP can lead to silent cerebral infarcts and increased cardiovascular events. 33 Other studies have also demonstrated that a very low NBP is associated with adverse cardiac events. 44 , 49 Additionally, nocturnal hypotension has been shown to damage the eye. 50 Studies on whether nocturnal hypotension is associated with visual loss from glaucoma, however, has yielded controversial results. 51 , 52 Therefore, the management of nocturnal hypotension should be considered comprehensively, particular in patients with complicated diseases.
Time of Dosing and Morning BP Surge
Why should antihypertensive drugs be administered in the morning after rising? Timing of cardiac and cerebrovascular events has been shown to be the potential cause and the aforementioned events have a peak incidence during the first few hours after morning waking. 53 In the early morning, BP values surge rapidly. 54 , 55 There exists marked diurnal variation in the onset time of cardiovascular events, with the peak value exhibited in early morning. Coincidently, BP also exhibits a similar diurnal variation, with a surge in the morning. 17 , 56 It has been postulated, although not proved, that there might be some potential essential correlation between the incidence of events and BP surge in the early morning. 57 , 58 , 59 , 60 It stands to reason that we should control the morning BP surge by administrating antihypertensive drugs after morning wakening. 61 , 62 Due to the concern about early morning BP surge, the management of NBP has been substantially ignored. 61 Nevertheless, some studies have provided evidence that it would be preferable to administer ACE inhibitors and ARBs before sleep. 15 , 47 , 48 Up until now, not enough evidence has been accumulated to divert dosing time to evening. 63 Thus, antihypertensive drugs are still typically taken in the morning after wakening. More prospective investigations, clinical trials, and cohort studies focus on outcomes related to modification of the circadian BP rhythm, and NBP values are still needed before recommendations can be made to normalize them.
As mentioned above, there exist some conflicts in the management of morning BP surge and abnormal NBP. However, to properly manage morning BP surge, NBP should be seriously taken into account. Perhaps we can interpret this relation between NBP and morning BP surge by means of plasma glucose in diabetic patients. It has been assumed that morning hyperglycemia in diabetic patients may be caused by the dawn phenomenon, the Somogyi effect, or poor glycemic control (Figure). 64 Similarly, morning BP surge in hypertensive patients might be caused by the following three aspects. First, the dawn phenomenon in BP means that NBP is normal, but physiologically the pressor effect of the renin‐angiotensin system or sympathetic nervous system is stimulated in the morning. 55 Second, the Somogyi effect in BP is when NBP is lower than normal and pathologically the pressor effect of the two aforementioned systems are excessively activated in the early morning (perhaps the doses of antihypertensive drugs are excessive). Third, poor BP control wherein the NBP is unknown and will inevitably lead to the poor efficacy of morning BP surge control and perhaps adverse events. Therefore, chronological treatment for morning BP surge may be achieved by bedtime dosing of antihypertensives. This may play an important role both in NBP and morning BP surge. 65
Figure FIGURE.
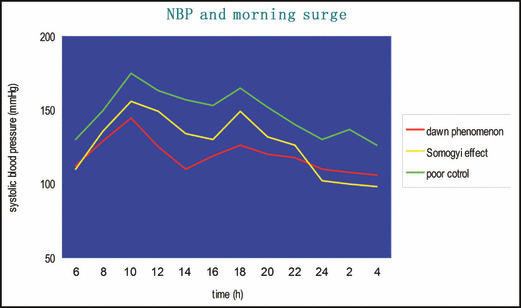
Interpretation of the relationship between nocturnal blood pressure (NBP) and morning blood pressure surge. Dawn phenomenon indicates normal NBP but high morning blood pressure surge; Somogyi effect, NBP lower than normal and the morning blood pressure surge excessively higher than normal in the early morning; poor BP control, abnormal BP not under appropriate control.
Conclusions
There exist a number of dilemmas of NBP in terms of methods for monitoring, the accurate period of nocturnal time, diagnostic thresholds of abnormal NBP, and the management of NBP. To overcome some of these challenges, a simple method to measure NBP, especially during sleeping, should be required. International conformity in the range of nocturnal time for NBP and thresholds of abnormal NBP should be made as soon as possible. To appropriately manage NBP and morning BP surge, we should take into account nocturnal hypertension and the adverse events. Administering antihypertensive drugs for nocturnal hypertension at bedtime may improve the control of NBP. Although some issues prevent progress in the management of NBP, it should be accurately and simply measured and be normalized to reduce the risk of mortality and morbidity related to NBP.
References
- 1. O’Brien E. Ambulatory blood pressure meaurement‐the case for implementation in primary care. Hypertension. 2008;51:1435–1441. [DOI] [PubMed] [Google Scholar]
- 2. Kain HK, Hinman T, Sokolow M. Arterial blood pressure measurments with a portable recorder in hypertensive patients. I. Variablity and correlation with “casual” pressure. Circulation. 1964;30:882–892. [DOI] [PubMed] [Google Scholar]
- 3. Ohkubo T, Hozawa A, Nagai K, et al. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurement in a general population: the Ohasama study. J Hypertens. 2000;18:847–854. [DOI] [PubMed] [Google Scholar]
- 4. Mancia G, Zanchetti A, Gabiti‐Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment‐induced regression of left ventricular hypertrophy. SAMPLE Study Group. Study on Ambulatory Monitoring of Blood Pressure and Lisinopril Evaluation. Circulation. 1997;95:1464–1470. [DOI] [PubMed] [Google Scholar]
- 5. Verdecchia P. Prognostic value of ambulatory blood pressure: current evidence and clinical implications. Hypertension. 2000;35:844–851. [DOI] [PubMed] [Google Scholar]
- 6. Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in EuropeTrial Investigators. JAMA. 1999;282:539–546. [DOI] [PubMed] [Google Scholar]
- 7. Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–1229. [DOI] [PubMed] [Google Scholar]
- 8. Fagard RH, Celis H, Thijs L, et al. Daytime and nighttime blood pressure as predictors of death and cause‐specific cardiovascular events in hypertension. Hypertension. 2008;51:55–61. [DOI] [PubMed] [Google Scholar]
- 9. O’Brien E, Asmar R, Beilin L, et al. European society of hypertension recommendations for conventional, ambula‐tory and home blood pressure measurement. J Hypertens. 2003;21:821–848. [DOI] [PubMed] [Google Scholar]
- 10. O’Brien E, Sheridan J, O’Malley K. Dippers and non‐dippers. Lancet. 1988;ii:397. [DOI] [PubMed] [Google Scholar]
- 11. Jason JS, Michael SP, Klar Y, et al. Ambulatory blood pressure monitoring among patients with cerebrovascular disease. Blood Press Monit. 2011;16:211–217. [DOI] [PubMed] [Google Scholar]
- 12. Cesare C, Carla S, Cristiana V, et al. Nocturnal blood pressure in untreated essential hypertensives. Blood Press. 2011;20:335–341. [DOI] [PubMed] [Google Scholar]
- 13. Hansen T, Li Y, Boggia J, et al. Predictive role of the nighttime blood pressure. Hypertension. 2011;57:3–10. [DOI] [PubMed] [Google Scholar]
- 14. Li Y, Staessen JA, Lu L, et al. Is isolated nocturnal hypertension a new clinical entity? Hypertension. 2007;50:333–339. [DOI] [PubMed] [Google Scholar]
- 15. Morgan TO. The importance of sleep blood pressure. Expert Rev Cardiovasc Ther. 2010;8:803–809. [DOI] [PubMed] [Google Scholar]
- 16. Rajiv V, Aldo JP. Management of nocturnal hypertension. Expert Rev Cardiovasc Ther. 2009;7:607–618. [DOI] [PubMed] [Google Scholar]
- 17. Thomas GP, Daichi S, Haas D. Ambulatory blood‐pressure monitoring. N Engl J Med. 2006;354:2368–2374. [DOI] [PubMed] [Google Scholar]
- 18. Kenichi C, Masahiro K, Tsutomu A, et al. Device for the self‐measurement of blood pressure that can monitor blood pressure during sleep. Blood Press Monit. 2001;6:203–205. [DOI] [PubMed] [Google Scholar]
- 19. Keiko H, Masahiro K, Takayoshi O, et al. Reproducibility of nocturnal blood pressure assessed by self‐measurement of blood pressure at home. Hypertens Res. 2007;30:707–715. [DOI] [PubMed] [Google Scholar]
- 20. Davies RJ, Jenkins NE, Stradling JR. Effect of measuring ambulatory blood pressure on sleep and on blood pressure during sleep. BMJ. 1994;308:820–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tropeano AI, Roudot‐Thoraval F, Badoual T, et al. Different effects of ambulatory blood pressure monitoring on subjective and objective sleep quality. Blood Press Monit. 2006;11:315–320. [DOI] [PubMed] [Google Scholar]
- 22. Degaute JP, van de Borne P, Kerkhofs M, et al. Does noninvasive ambulatory blood pressure monitoring disturb sleep? J Hypertens. 1992;10:879–885. [PubMed] [Google Scholar]
- 23. Le′ on H, Martin B, Abraham AK, et al. Subjective sleep disturbance increases the nocturnal blood pressure level and attenuates the correlation with target‐organ damage. J Hypertens. 2011;29:242–250. [DOI] [PubMed] [Google Scholar]
- 24. Verdecchia P, Angeli F, Borgioni C, et al. Ambulatory blood pressure and cardiovascular outcome in relation to perceived sleep deprivation. Hypertension. 2007;49:777–783. [DOI] [PubMed] [Google Scholar]
- 25. Pai AU, Chakrapani M, Bhaskaran U, et al. Study of home monitored night blood pressure and its correlation with left ventricular hypertrophy in treatment‐naive hypertensive patients. Singapore Med J. 2012;53:95–98. [PubMed] [Google Scholar]
- 26. O’Brien E, Asmar R, Beilin L, et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens. 2005;23:697–701. [DOI] [PubMed] [Google Scholar]
- 27. Alejandro S, Josep R, Jose′ RB, et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466–472. [DOI] [PubMed] [Google Scholar]
- 28. Eissa MA, Poffenbarger T, Portman RJ. Comparison of the actigraph versus patients’ diary information in defining circadian time periods for analyzing ambulatory blood pressure monitoring data. Blood Press Monit. 2001;6:21–25. [DOI] [PubMed] [Google Scholar]
- 29. Helen EJ, Manis DS. The definition of daytime and nighttime influences the interpretation of ABPM in children. Pediatr Nephrol. 2011;26:775–781. [DOI] [PubMed] [Google Scholar]
- 30. Waeber BA, Mourad JJ, O’Brien E. Nighttime blood pressure: a target for therapy? Curr Hypertens Rep. 2010;12:474–479. [DOI] [PubMed] [Google Scholar]
- 31. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals. part 1: blood pressure measurement in humans. A statement for professionals from the subcommittee of professional and public education of the American heart association council on high blood pressure research. Hypertension. 2005;45:142–161. [DOI] [PubMed] [Google Scholar]
- 32. Metoki H, Ohkubo T, Kikuya M, et al. Prognostic significance of night‐time, early morning, and daytime blood pressures on the risk of cerebrovascular and cardiovascular mortality: the Ohasama Study. J Hypertens. 2006;24:1841–1848. [DOI] [PubMed] [Google Scholar]
- 33. shikawa J, Shimizu M, Hoshide S, et al. Cardiovascular risks of dipping status and chronic kidney disease in elderly Japanese hypertensive patients. J Clin Hypertens (Greenwich). 2008;10:787–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ben‐Dov IZ, Kark JD, Ben‐Ishay D, et al. Predictors of all‐cause mortality in clinical ambulatory monitoring. Unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–1241. [DOI] [PubMed] [Google Scholar]
- 35. Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood‐pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–2415. [DOI] [PubMed] [Google Scholar]
- 36. Dolan E, Stanton AV, Thom S, et al. Ambulatory blood pressure monitoring predicts cardiovascular events in treated hypertensive patients – an Anglo‐Scandinavian cardiac outcomes trial substudy. J Hypertens. 2009;27:876–885. [DOI] [PubMed] [Google Scholar]
- 37. Ungar A, Pepe G, Lambertucci L, et al. Low diastolic ambulatory blood pressure is associated with greater all‐cause mortality in older patients with hypertension. J Am Geriatr Soc. 2009;57:291–296. [DOI] [PubMed] [Google Scholar]
- 38. Hansen TW, Jeppesen J, Rasmussen S, et al. Ambulatory blood pressure and risk of cardiovascular disease: a population based study. Am J Hypertens. 2006;19:243–259. [DOI] [PubMed] [Google Scholar]
- 39. Bjo¨rklund K, Lind L, Zethelius B, et al. Prognostic significance of 24‐h ambulatory blood pressure characteristics for cardiovascular morbidity in a population of elderly men. J Hypertens. 2004;22:1691–1697. [DOI] [PubMed] [Google Scholar]
- 40. Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–1249. [DOI] [PubMed] [Google Scholar]
- 41. Li Y, Wang JG, Gao HF, et al. Are published characteristics of the ambulatory blood pressure generalizable to rural Chinese? The JingNing population study. Blood Press Monit. 2005;10:125–134. [DOI] [PubMed] [Google Scholar]
- 42. Florent B, François G, Stuart P, et al. J‐shaped relationship between blood pressure and mortality in hypertensive patients: new insights from a meta‐analysis of individual‐patient data. Ann Intern Med. 2002;136:438–448. [DOI] [PubMed] [Google Scholar]
- 43. Zoltán V, Michiel LB, Albert H, et al. J‐shaped relation between blood pressure and stroke in treated hypertensives. Hypertension. 1999;34:1181–1185. [DOI] [PubMed] [Google Scholar]
- 44. Linda F, Arkadiusz SL, Sölve E. Reduced cerebral perfusion in elderly men with silent myocardial ischaemia and nocturnal blood pressure dipping. Atherosclerosis. 2011;214:231–236. [DOI] [PubMed] [Google Scholar]
- 45. Wollner L, McCarthy ST, Soper ND, et al. Failure of cerebral autoregulation as a cause of brain dysfunction in the elderly. Br Med J. 1979;1:1117–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Nagai M, Hoshide S, Ishikawa J, et al. Ambulatory blood pressure as an independent determinant of brain atrophy and cognitive function in elderly hypertension. J Hypertens. 2008;26:1636–1641. [DOI] [PubMed] [Google Scholar]
- 47. Alastair W, Urs F, Ziyah M, et al. Effects of antihypertensive‐drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta‐analysis. Lancet. 2010;375:906–915. [DOI] [PubMed] [Google Scholar]
- 48. Morgan TO, Anderson A. Different drug classes have variable effects on blood pressure depending on the time of day. Am J Hypertens. 2003;16:46–50. [DOI] [PubMed] [Google Scholar]
- 49. Kario K, Shimada K. Risers and extreme‐dippers of nocturnal blood pressure in hypertension: antihypertensive strategy for nocturnal blood pressure. Clin Exp Hypertens. 2004;26:177–189. [DOI] [PubMed] [Google Scholar]
- 50. Hayreh SS. Blood flow in the optic nerve head and factors that may influence it. Prog Retin Eye Res. 2001;20:595–624. [DOI] [PubMed] [Google Scholar]
- 51. Graham L, Drance M, Wijsman K, et al. Ambulatory blood pressure monitoring in glaucoma. The nocturnal dip. Ophthalmology. 1995;102:61–69. [DOI] [PubMed] [Google Scholar]
- 52. Collignon N, Dewe W, Guillaume S, et al. Ambulatory blood pressure monitoring in glaucoma patients, the nocturnal systolic dip and its relationship with disease progression. Int Ophthalmol. 1998;22:19–25. [DOI] [PubMed] [Google Scholar]
- 53. Quyyumi AA. Circadian rhythms in cardiovascular disease. Am Heart J. 1990;120:726–733. [DOI] [PubMed] [Google Scholar]
- 54. Kazuyuki S, Kazuomi K, Yuji U, et al. Early morning surge in blood pressure. Blood Press Monit. 2001;6:349–353. [DOI] [PubMed] [Google Scholar]
- 55. Kario K, Hoshide S, Shimizu M, et al. Morning surge in blood pressure and cardiovascular risk. Evidence and perspectives. Hypertension. 2010;56:765–773. [DOI] [PubMed] [Google Scholar]
- 56. Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989;79:733–743. [DOI] [PubMed] [Google Scholar]
- 57. Muller JE, Stone PH, Turi ZG, et al. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985;313:1315–1322. [DOI] [PubMed] [Google Scholar]
- 58. Gosse P, Lasserre R, Minifié C, et al. Blood pressure surge on rising. J Hypertens. 2004;22:1113–1118. [DOI] [PubMed] [Google Scholar]
- 59. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: prospective study. Circulation. 2003;107:1401–1406. [DOI] [PubMed] [Google Scholar]
- 60. Verdecchia P, Schillaci G, Borgioni C, et al. Adverse prognostic value of a blunted circadian rhythm of heart rate in essential hypertension. J Hypertens. 1998;9:1335–1343. [DOI] [PubMed] [Google Scholar]
- 61. Hermida R, Ayala D. Chronotherapy with ramipril in essential hypertension: improved ambulatory blood pressure control with bedtime dosing. Hypertension. 2009;54:40–46. [DOI] [PubMed] [Google Scholar]
- 62. Svensson P, Faire U, Sleight P, et al. Comparative effects of ramipril on ambulatory and office blood pressures: a HOPE substudy. Hypertension. 2001;38:E28–E32. [DOI] [PubMed] [Google Scholar]
- 63. Fox KM. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease; randomized, double‐blind, placebo‐controlled, multicentre trial (the EUROPA study). Lancet. 2003;362:782–788. [DOI] [PubMed] [Google Scholar]
- 64. Malwina R, Robert K, Bogusław O. The dawn phenomenon and the Somogyi effect – two phenomena of morning hyperglycaemia. Endokrynol Pol. 2011;62:276–283. [PubMed] [Google Scholar]
- 65. Kario K, Hoshide S, Shimizu M, et al. Effect of dosing time of angiotensin II receptor blockade titrated by self‐measured blood pressure recordings on cardiorenal protection in hypertensives: the Japan Morning Surge‐Target Organ Protection (J‐TOP) study. J Hypertens. 2010;28:1574–1583. [DOI] [PubMed] [Google Scholar]


