Abstract
J Clin Hypertens (Greenwich). 2011;13:818–820. ©2011 Wiley Periodicals, Inc.
Recently, the authors experienced four patients who had refractory hypertension and neurovascular compression of the rostral ventrolateral medulla (RVLM). One of them, a 49‐year‐old woman, had undergone continuous intravenous drip injections of calcium channel blockers and β‐blockers for more than 3 years because of severe and refractory hypertension. The patients had undergone microvascular decompression (MVD) of the RVLM, and the changes in blood pressure (BP) and sympathetic nerve activities were recorded. In these patients, BP decreased to the normal range without any antihypertensive drugs 2 to 3 months after MVD. The tibial sympathetic nerve activities under resting and stress conditions significantly decreased, and plasma levels of norepinephrine, urinary levels of adrenaline, and plasma renin activity were also significantly decreased after MVD of RVLM. In some patients with refractory hypertension, arterial compression of the RVLM enhances sympathetic nerve activity and renin‐angiotensin system to thereby increase BP. In these patients, the operative decompression of the RVLM could lower BP via restoration of sympathetic nerve activities and the renin‐angiotensin system.
Sympathetic hyperactivity of central origin is implicated in the pathogenesis of hypertension. However, the precise mechanisms that cause central sympathetic hyperactivity remain unclear. The rostral ventrolateral medulla (RVLM) contains neurons that are the major tonic source of supraspinal sympathoexcitatory outflow to the heart, kidneys, and vessels. 1 In humans, RVLM exists near the dorsal root entry zone of cranial nerves IX and X. A possible association between essential hypertension and neurovascular compression (NVC) of the RVLM has been reported by autopsy, 2 magnetic resonance imaging/magnetic resonance angiography (MRI/MRA), 3 and intraoperative observation. 4 Some of these reports referred to enhanced sympathetic activities in hypertensive patients with NVC compared with hypertensive patients without NVC or normotensive patients. In rats, we reported that pulsatile compression of the RVLM leads to activation of RVLM neurons to elicit sympathetic hyperactivity and blood pressure (BP) elevation. 5 A causative relationship between NVC of the RVLM and hypertension was further ascertained by the fact that surgical microvascular decompression (MVD) substantially decreased BP in patients with refractory hypertension. 4 However, except in our case report, there has been no report that neurovascular decompression of the RVLM restores sympathetic activity to thereby decrease BP. 6 Therefore, in the present report, the effects of surgical MVD of the RVLM on BP, sympathetic nerve activities, and renin‐angiotensin system were explored in patients with refractory hypertension.
Methods
Patients
Four patients were referred to our hospital because of refractory hypertension. Of these, 3 were women and 1 was a man, ranging in age between 35 and 51 years. Three of these patients showed concomitant cranial nerve microvascular compression syndrome, hemifacial spasm (two patients on the left side and 1 patient on the right side), while 1 patient showed no symptoms of cranial rhizopathies. Three patients took >3 antihypertensive drugs, but their BPs remained above normal. A 49‐year‐old woman (case A), who had no cranial nerve syndrome, showed extremely high BP, at about 260/130 mm Hg despite combination therapy with furosemide 40 mg, doxazosin 2 mg, imidapril 5 mg, metoprolol 120 mg, and amlodipine 5 mg. Since her BP did not respond to any combination of oral antihypertensives, she was given a continuous intravenous drip injection of calcium channel blocker (nicardipine 18 mg/d) and β‐blocker (propranolol 20 mg/d) through a central venous catheter for more than 3 years.
Microneurographic Analysis
Muscle sympathetic nerve activity was recorded from the tibial nerve and BP was monitored continuously from the middle finger by a servo‐controlled pressure measurement device before and 1 month after MVD surgery, as described previously. 6 Average burst frequencies (burst per minute) were calculated from 5‐minute recordings with the patient at rest or during tilting and arithmetic stress. Plasma and urinary levels of catecholamines and plasma renin activities and plasma aldosterone concentration were measured. Data expressed as average ± standard error of the mean were analyzed using paired Student t tests, and differences at a 5% level (P<.05) were considered significant.
Results
Preoperative MRI/MRA showed the RVLM compression in these 4 patients. In addition, 3 patients with hemifacial spasms had compressions of the ipsilateral seventh cranial nerve. The compressing arteries were vertebral arteries in 2 patients and posterior inferior cerebellar arteries in 2 patients. In case A, both right and left vertebral arteries were located in the left side of the medulla, and compression of the left RVLM and rotation of the whole medulla due to marked displacement of the left vertebral artery were noted (Figure 1A). These 4 patients were operated on for MVD of the RVLM and of the seventh cranial nerve in 3 patients with hemifacial spasm. Postoperative MRI/MRA revealed adequate decompression of the RVLM in case A (Figure 1B).
Figure 1.
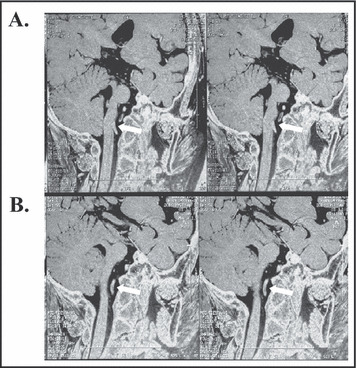
Magnetic resonance imaging–constructive interference in steady state image of the medulla oblongata in case A. The left vertebral artery obviously compressed the left rostral ventrolateral medulla (RVLM) before microvascular decompression (MVD) (A: pre‐MVD, white arrows). The vertebral artery is clearly separated from the RVLM after MVD (B: post‐MVD, white arrows).
In case A, her home and in‐hospital BP often increased above 160/100 mm Hg despite continuous intravenous administration of calcium channel blockers and β‐blockers (Figure 2). Soon after operation, her BP began to decline; therefore, the central venous catheter was withdrawn on the operation day (Figure 2). Within 3 months after surgery, the BPs of all 4 patients decreased to a normal range without any medications (preoperative:169±11/108±9 mm Hg, postoperative:129±10/82±10 mm Hg, P<.01).
Figure 2.
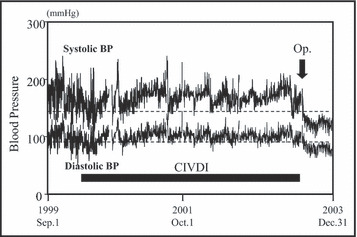
Home and in‐hospital systolic and diastolic blood pressures (BPs) in case A. On the day of operation (Op.), her blood pressure decreased and central venous catheter was withdrawn. CIVDI indicates continuous intravenous drip injection through central venous catheter.
Burst frequencies of sympathetic nerve activities recorded directly from the tibial nerve significantly decreased after MVD surgery: under resting (preoperative: 29±4, postoperative: 21±3 burst/min, P<.01), tilt (preoperative: 57±4, postoperative: 42±2 burst/min, P<.01), and arithmetic stress (preoperative: 29±5, postoperative: 19±4 burst/min, P<.05) conditions (Figure 3). In addition, plasma norepinephrine level (ng/mL), urinary epinephrine level (μg/d), and plasma renin activity (ngAI/mL.h) significantly (P<.01, P<.01, P<.05, respectively) decreased after MVD (preoperative: 0.31±0.14, 7.5±3.9, 1.9±1.2, postoperative: 0.19±0.10, 2.9±1.0, 1.5±1.1, respectively).
Figure 3.
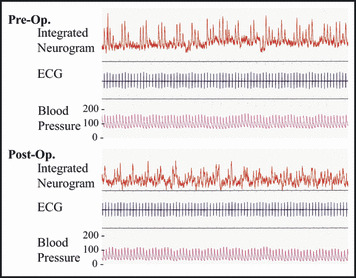
Preoperative (Pre‐Op.) and post‐operative (Post‐Op.) sympathetic neurogram directly recorded from the tibial nerve, electrocardiogram (ECG), and blood pressure at rest. Burst amplitude and frequencies were markedly decreased with decreases in blood pressure after microvascular decompression.
Discussion
In the present studies, we found that MVD of the RVLM lowered BP with decreases in sympathetic nerve activities recorded directly from the tibial sympathetic nerve, plasma norepinephrine, urinary epinephrine, and plasma renin activity in patients with refractory hypertension, regardless of the complication of cranial rhizopathies. Therefore, pulsatile compression of the RVLM seems to enhance sympathetic nerve activities to thereby elevate BP.
Arterial pulsatile compression may either directly stimulate the RVLM neurons or injure arterial and/or cardiopulmonary baroreflex afferent fibers to activate sympathetic nerve activities. Supporting the former hypothesis, we found that direct pulsatile compression of the RVLM with an electrocardiography‐triggered pneumatic pump elevated BP and sympathetic nerve activity in rats. 5 Alternatively, the latter hypothesis was supported by the fact that modulation of baroreflex sensitivity was reduced under mental and physical stress in patients with neurovascular contact of the left RVLM in young normotensive men. 7
Conclusions
Although many patients are well treated by pharma‐cologic means, a subset of patients do not achieve normotensive levels on multiple antihypertensive medications. In these patients with refractory hypertension, NVC of the RVLM is occasionally recognized and MVD often contributes to the significant relief of their hypertension. However, MVD to relieve such vascular contact with the RVLM has not been equally effective in lowering BP in these patients. 8 Accordingly more precise diagnosis of NVC of the RVLM and strict patient selection will be crucial since the relatively acute risks and potential benefits of MVD should be weighed against the chronic morbidity and mortality of refractory hypertension.
References
- 1. Dampney RAL, Moon EA. Role of ventrolateral medulla in vasomotor response to cerebral ischemia. Am J Physiol. 1980;239:H349–H358. [DOI] [PubMed] [Google Scholar]
- 2. Naraghi R, Gaab MR, Walter GF, Kleineberg B. Arterial hypertension and neurovascular compression at the ventrolateral medulla. A comparative microanatomical and pathological study. Neurosurg. 1992;77:103–112. [DOI] [PubMed] [Google Scholar]
- 3. Morimoto S, Sasaki S, Miki S, et al. Neurovascular compression of the rostral ventrolateral medulla related to essential hypertension. Hypertension. 1997;30(part 1):77–82. [DOI] [PubMed] [Google Scholar]
- 4. Jannetta PJ, Segal R, Wolfson S. Neurogenic hypertension: etiology and surgical treatment, I: observations in 53 patients. Ann Surg. 1985;201:391–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morimoto S, Sasaki S, Miki S, et al. Pressor response to compression of the ventrolateral medulla mediated by glutamate receptors. Hypertension. 1999;33:1207–1213. [DOI] [PubMed] [Google Scholar]
- 6. Morimoto S, Sasaki S, Takeda K, et al. Decreases in blood pressure and sympathetic nerve activity by microvascular decompression of the rostral ventrolateral medulla in essential hypertension. Stroke. 1999;30:1707–1710. [DOI] [PubMed] [Google Scholar]
- 7. Wolf KJ, Distler A, Sharma AM. Neurovascular contact and blood pressure response in young, healthy, normotensive men. Am J Hypertens. 2002;15:119–124. [DOI] [PubMed] [Google Scholar]
- 8. Levy EI, Scarrow AM, Jannetta PJ. Microvascular decompression in the treatment of hypertension: review and update. Surg Neurol. 2001;55:2–11. [DOI] [PubMed] [Google Scholar]


