Abstract
Parental accommodation refers to ways in which caregivers modify their behavior to decrease child distress in the short-term. Accommodation is prevalent among anxious youth and related to decreased treatment and functional outcomes. Although separation anxiety disorder (SAD) is associated with increased accommodation, SAD is not a predictor of treatment response, suggesting that a diagnosis of SAD alone may not be enough to clarify the relationship between accommodation and separation anxiety symptoms within a clinical context. Participants were youth with a primary anxiety disorder (N = 186; aged 7–17) enrolled in an outpatient anxiety clinic. Latent class analysis was used to extract profiles from parent-reported SAD symptoms using the Anxiety Disorders Interview Schedule for DSM-IV/5. Profiles were compared on pre-treatment accommodation. Low, moderate, and interfering SAD classes emerged. Interfering SAD was associated with high accommodation. Results help to clarify the association between SAD and accommodation and has implications for personalized intervention.
Keywords: Youth, Youth anxiety, Accommodation, Latent class analysis
Parental accommodation is an important variable that may be associated with the onset and maintenance of anxiety disorders in youth. Accommodation describes ways in which family members, primarily parents and guardians in the case of pediatric disorders, modify their behavior in an effort to diminish, alleviate or avoid distress caused by a disorder [1]. Accommodating behaviors observed among parents and family members can involve providing excessive reassurance about a child’s fears, modifying family routines or schedules, or engaging in or facilitating safety behaviors [2, 3]. Initially investigated in adults suffering from OCD, accommodation has since been studied in youth with OCD and anxiety disorders [1; for a review see 4, 5]. Results from these investigations have found that accommodation occurs in nearly all families with a child or adolescent with an anxiety disorder [2, 6–8], with a majority of parents experiencing distress resulting from said accommodation [2]. Importantly, accommodation has been linked to increased anxiety symptom severity, functional impairment and caregiver burden [1, 6, 7, 9, 10]. Accommodation also appears to be associated with treatment response, with findings suggesting that every one-unit increase in self-reported parental accommodation at baseline is associated with a 26% decrease in the odds of remission at the end of treatment [11].
Theories about the relationship between accommodation and the maintenance of anxiety symptoms have behavioral roots. Mowrer’s theory specifies that avoidance, safety-seeking and compulsive behaviors, hallmarks of anxiety which come about as a reaction to fear-inducing situations, are negatively reinforced through operant conditioning [12]. The avoidance behaviors temporarily reduce anxiety, thus increasing the likelihood that they will occur in the future. The continuation of these symptoms in the long term then interferes with the natural extinction of the conditioned fear that would otherwise occur via exposure to the feared situation [13].
Parental accommodations act similarly to avoidance behaviors, allowing the child to physically or mentally avoid a fear-inducing situation—be it worry around uncertainty or a tangible object or situation. As a result, accommodation prevents opportunities for exposure, and subsequent reduction of anxiety. Accommodation is negatively reinforcing and increases a child’s expectation of continued accommodation in the future [14]. Although many parents react to their child’s anxiety in a protective way, this protectiveness becomes maladaptive when these reactions allow the child to avoid anxiety-provoking situations [15]. Because exposure is considered to be an active ingredient in the effective treatment of anxiety-based disorders, accommodation is detrimental because it prevents opportunities for exposure [16, 17]. Accommodation can impede the development of independent coping skills, contribute to lower insight on the part of the child, and unwittingly validate the child’s perceived need to avoid the feared situations by contributing to the child’s avoidance [2, 6]. Despite broad findings relating child anxiety to accommodation, the varied strength of this relationship suggests that additional variables should be explored. For example, several studies have suggested that self-reported maternal empathy, maternal anxiety and child anxiety sensitivity might moderate the relationship between child anxiety and accommodation [18, 19].
One factor that warrants further exploration is separation anxiety symptoms. Research findings indicate that accommodation is most prevalent in youth with a primary diagnosis of separation anxiety disorder (SAD) compared to other anxiety disorders in DSM-5 and that SAD is correlated with higher ratings of many different types of accommodating behaviors such as allowing a child to leave an event early or a parent staying home from work [2, 7]. Although the lifetime prevalence rate of SAD in the general population is 4.1%, anxiety disorders are highly co-morbid in childhood and adolescence [20, 21]. Symptoms of SAD are also seen in many youths diagnosed with other anxiety disorders. Despite the prevalence of SAD and separation anxiety symptoms in anxious youth, there has been little research to date investigating the nature of the relationship between SAD symptom presentations and parental accommodation within a clinical context.
Starting with Kiesler’s famous question in 1966: “What treatment, provided by whom, is most effective for what type of individual?” research has sought to identify the best treatment for subgroups of individuals [22]. The movement towards personalized medicine in mental health has grown stronger, with National Institute of Health (NIH), National Institute of Mental Health (NIMH), American Psychological Association (APA) and Federal Drug Administration (FDA) issuing public calls to identify individual markers linked to differential treatment outcomes [23–26]. Given high levels of heterogeneity and co-morbidity observed cross-diagnostically [27, 28] and within youth anxiety disorders [29], greater specificity is needed. Efforts such as the Unified Protocol, MATCH, process-based therapy and other approaches target specific symptoms rather than broad diagnostic categories [30–32]. Consistent with these approaches, it is important to identify characteristics of individuals who might best benefit from specific treatment modalities.
Despite research indicating less favorable treatment outcomes for youth with high levels of baseline accommodation as well as findings indicating strong relationships between SAD and accommodation, it is not the case that all youth with SAD have poorer treatment outcomes. Rather, youth with SAD show comparable treatment outcomes to peers with other primary anxiety disorders [e.g., 33]. These findings suggest that there may be certain features of SAD, rather than simple inclusion in the diagnostic category, that are more associated with parental accommodation and with subsequent diminished treatment outcomes. There have been mixed findings regarding the usefulness of parent involvement in the treatment of anxiety disorders in youth [15, 34]. One explanation is that these parenting interventions have been too broad, and another is that they are not founded in theory [15]. As such, it is useful to investigate a sample of anxious youth to clarify which symptoms of SAD are related to high levels of parental accommodation so that these youth could potentially be targeted with accommodation-specific interventions.
The present study, using latent class analyses (LCA), examined whether children and adolescents seeking treatment for a range of DSM-5 anxiety disorders (i.e., SAD, generalized anxiety disorder [GAD], social anxiety disorder [Soc] and specific phobia [SP]) and OCD exhibit distinct separation anxiety symptom profiles. The study also examined the degree to which the identified SAD symptom profiles are associated with parental accommodation. We hypothesized that observed separation anxiety symptom profiles would be distinct and differentially associated with parental accommodation.
Methods
Participants
Participants were 186 youth (aged 7–17) seeking treatment at an anxiety specialty clinic. Diagnoses were based on the Anxiety Disorders Interview Schedule for DSM-IV and DSM-5 [ADIS-IV-C/P and ADIS-5-C/P; 35], administered separately to youth and their parents/guardians. Composite diagnoses were determined using both interviews. In cases with multiple diagnoses, the diagnosis with the highest clinical severity rating (CSR) was the principal diagnosis. Participants were referred through multiple sources including clinics, public and nonpublic schools, media descriptions, and local presentations. All legal guardian(s) of participants provided written informed consent. Data collection was approved by the Institutional Review Board of Temple University. All data were obtained prior to the onset of treatment. The mean age of the sample was 11.76 years (SD = 2.8). Of the participants, 45.30% were female (Table 1). Overall frequencies, across the entire sample, of parent-reported SAD symptoms are reported in Table 1. Overall, 26% of the sample met diagnostic criteria for SAD and 89.6% of the sample met diagnostic criteria for SAD, GAD or Soc (Table 1).
Table 1.
Sample characteristics
| SAD symptoms | % endorsed |
|---|---|
| Symptom 1 | 33.30 |
| Symptom 2 | 26.00 |
| Symptom 3 | 21.9 |
| Symptom 4 | 9.90 |
| Symptom 5 | 31.30 |
| Symptom 6 | 29.20 |
| Symptom 7 | 16.70 |
| Symptom 8 | 19.80 |
| Symptom 9 | 31.80 |
| Symptom 10 | 30.70 |
| Symptom 11 | 21.40 |
| Symptom 12 | 41.10 |
| Symptom 13 | 26.00 |
| Symptom 14 | 9.90 |
| Symptom 15 | 27.10 |
| Diagnosis | % met Dx criteria |
| SAD | 26.00 |
| School Refusal | 8.30 |
| Soc | 59.9 |
| GAD | 79.700 |
| OCD | 10.90 |
| SAD, Soc or GAD | 89.60 |
| Gender | % male | % female | % missing data |
|---|---|---|---|
| 54.20 | 45.30 | 0.50 | |
| Measure | M | SD | % missing |
| Age | 11.76 | 2.85 | 0.00 |
SAD separation anxiety disorder, Soc social anxiety disorder, GAD generalized anxiety disorder, OCD obsessive compulsive disorder, SAD symptom number correspond with Fig. 2
Measures
Anxiety Disorders Interview Schedule, Child and Parent Versions (ADIS‑IV‑C/P; ADIS‑5‑C/P)
Trained and reliable diagnosticians (Cohen’s κ ≥ .85) assessed youth for anxiety disorders and comorbid disorders (e.g., depressive disorder) using the ADIS-IV-C/P and the ADIS-5-C/P [35, 36]. Diagnosticians produced a composite diagnosis based on both reports, providing CSR’s for each diagnosis, ranging from 0 (not a problem) to 8 (a debilitating problem). A CSR of 4 or above was required for diagnosis (Table 2).
Table 2.
Correlation matrix showing Phi-coefficients (ϕ) for SAD symptoms
| SAD symptoms | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
| 1 | – | ||||||||||||||
| 2 | 0.58** | – | |||||||||||||
| 3 | 0.42** | 0.51** | – | ||||||||||||
| 4 | 0.39** | 0.40** | 0.50** | – | |||||||||||
| 5 | 0.53** | 0.49** | 0.42** | 0.34** | – | ||||||||||
| 6 | 0.39** | 0.24** | 0.26** | 0.17* | 0.42** | – | |||||||||
| 7 | 0.38** | 0.24** | 0.06 | 0.03 | 0.31** | 0.35** | – | ||||||||
| 8 | 0.35** | 0.39** | 0.43** | 0.36** | 0.52** | 0.25** | 0.33** | – | |||||||
| 9 | 0.36** | 0.33** | 0.31** | 0.26** | 0.43** | 0.27** | 0.26** | 0.36** | – | ||||||
| 10 | 0.38** | 0.42** | 0.27** | 0.19* | 0.45** | 0.26** | 0.24** | 0.31** | 0.58** | – | |||||
| 11 | 0.24** | 0.20** | 0.12 | 0.04 | 0.28** | 0.19* | 0.14 | 0.18* | 0.43** | 0.47** | – | ||||
| 12 | 0.22* | 0.17* | 0.29** | 0.11 | 0.31** | 0.41** | 0.21** | 0.19* | 0.26** | 0.28** | 0.41** | – | |||
| 13 | 0.25** | 0.32** | 0.28** | 0.20** | 0.31** | 0.24** | 0.17* | 0.35** | 0.25** | 0.34** | 0.20** | 0.31** | – | ||
| 14 | 0.33** | 0.16* | 0.24** | 0.18* | 0.30** | 0.20** | 0.09 | 0.23* | 0.15* | 0.19** | 0.08 | 0.21** | 0.12 | – | |
| 15 | 0.51** | 0.32** | 0.47** | 0.30** | 0.41** | 0.30** | 0.24** | 0.35** | 0.29** | 0.28** | 0.20** | 0.29** | 0.30** | 0.19* | – |
SAD separation anxiety disorder, SAD symptom numbers correspond with Fig. 2
ρ < 0.05, two-tailed.
ρ < 0.01, two-tailed
Research indicates that the ADIS-IV-C/P has interrater reliability for agreement on principal diagnosis (κ = .92), individual anxiety disorders (κ = .80 – 1.0) and common comorbid disorders [κ = .65 – .77; 37]. Both the ADIS-IV-C and the ADIS-IV-P have been found to have retest reliability for SAD, Soc, SP and GAD [κ = .63 – .80 and κ = .65 – .88, respectively; 38]. The anxiety disorders section of the ADIS-IV-C/P displays convergent validity, especially for SAD and SP [39]. Psychometrics on the ADIS-5-C/P are currently being investigated, but the measure’s structure and items mirror those of the ADIS-IV-C/P.
For this investigation, parent and child composite scores were used to report on diagnoses within the sample. Only parent reports of SAD symptoms were used to maintain a consistency with the parent self-report measure of accommodation. Previous research on a similar sample found that parent-youth reporting agreement is high at symptom-level, thus supporting the inclusion of parent report [40]. Within the SAD portion of the ADIS-IV-P and ADIS-5-P, parents were asked to report on the presence and severity of certain cardinal symptoms on a scale of 0 (absent) to 8 (debilitating). SAD symptoms addressed in the ADIS-IV-P are listed in Fig. 2.
Fig. 2.
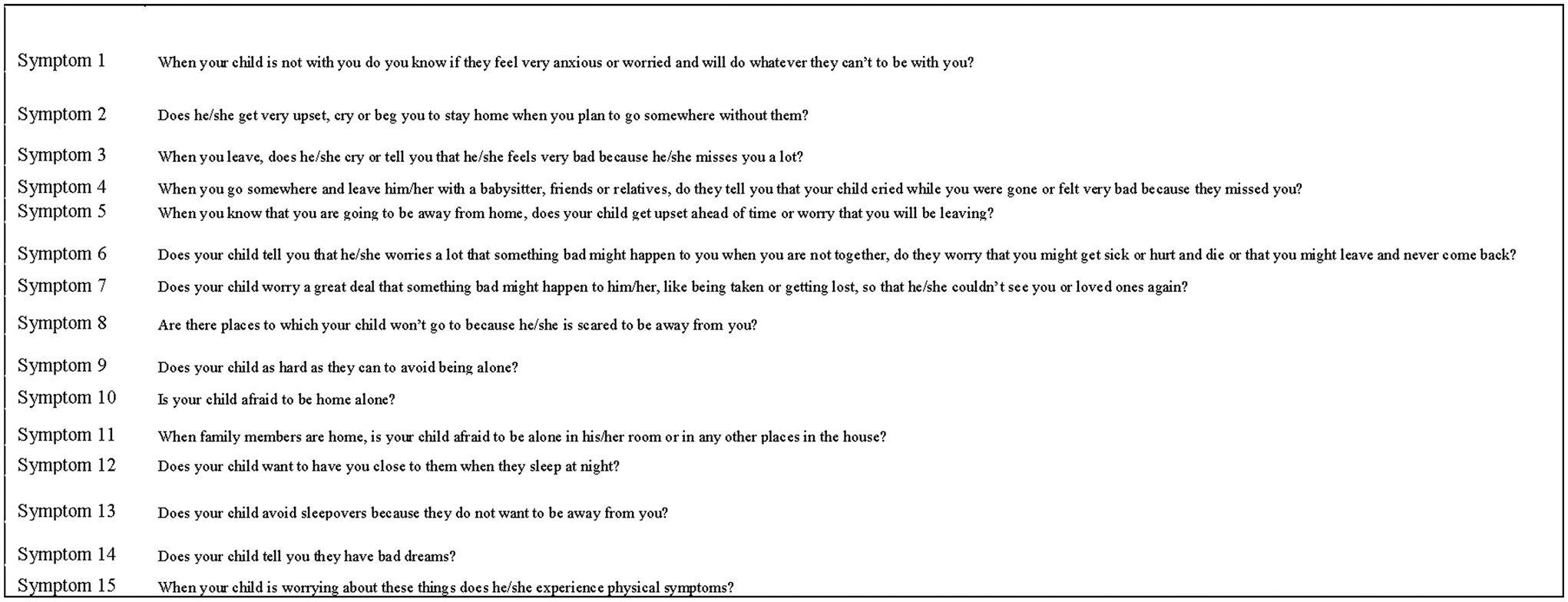
Separation anxiety symptoms (ADIS-5)
Family Accommodation Scale‑Anxiety (FASA)
Parents of participants completed the FASA self-report. The FASA is a modified version of the Family Accommodation Scale (FAS), with changes made to measure accommodation of anxiety symptoms, rather than solely OCD symptoms [1, 2]. The 13-item FASA measures the degree to which family members (i.e., parents) have accommodated a child’s anxiety symptoms [2]. Each item is scored on a 5-point Likert-type scale and the first nine items are combined to create a total score. The latter four items assess distress related to accommodation and negative consequences of not accommodating. Research has shown that the FASA demonstrates excellent internal consistency = (α = .90 – .91) and convergent validity between scores and self-report measures of anxiety (r = 0.45). Additionally, FASA scores were not significantly related to depressive symptoms (r = 0.17) suggesting divergent validity [2].
Multidimensional Anxiety Scale for Children–Parent and Child Report (MASC‑C/P)
Both parents and youth completed the MASC. The MASC is a 39-item measure of child anxiety. Each item is scored on a 4-point Likert-type scale, yielding scores on four subscales; Social Anxiety, Separation/Panic, Harm Avoidance and Physical Symptoms. The MASC demonstrates internal consistency (α = .87) [41]. Research has shown the MASC demonstrates acceptable to good internal consistency within subscales (α = .74 – .85) and convergent validity with other youth measures of anxiety (r = 0.63) [42]. Findings have shown convergent and predictive validity with the ADIS-C/P, with the MASC successfully predicting to ADIS-identified anxiety disorders [43, 44]. Additionally, MASC-C/P subscales were not significantly related to externalizing or depressive symptoms (r = 0.07 to 0.19) thus showing divergent validity [42].
Revised Child Anxiety and Depression Scale (RCADS)
Parents of participants completed the RCADS, an adaptation of the Spence Child Anxiety Scale [SCAS; 45] amended to correspond with the DSM-IV. The RCADS is a 47-item measure of youth anxiety. Each item is scored on a 3-point scale corresponding to “sometimes,” “often,” and “never.” It includes five anxiety subscales which correspond to the DSM-IV categories of GAD, OCD, SP, Sep and Soc. Research has shown the RCADS demonstrates acceptable to good internal consistency within subscales (α = .78 to .88). Findings indicate that the RCADS has convergent validity with others measure of anxiety and depression (e.g., r = 0.22–0.45), and the subscales were not significantly related to externalizing symptoms thus suggesting divergent validity [46]. Reliability and validity have similarly been established in community samples [47, 48]. The RCADS has also been found to measure symptoms of anxiety consistently over youth development [49].
Statistical Analyses
All statistical analyses were performed with MPlus Version 8.0 [50] and SPSS Version 24.0 [51]. Descriptive analyses were run to determine demographic frequencies in the sample. Additional descriptive analyses were used to determine the frequency and severity of separation anxiety symptoms in the sample. Latent class analysis (LCA) was used to identify groups (e.g. classes) based on SAD symptoms. LCA describes the probability of observed variables across groups of individuals when class membership is unknown and presumed contingent on unknown (e.g., latent) qualities [52]. LCA focuses on relations among individuals, rather than among variables, to classify them into discrete “classes” that potentially differ by separation anxiety symptom frequency, severity or quality [53, 54]. LCA does not require pre-determined assumptions about the structure or number of anxiety symptom classes [55]. In the present LCA, 15 separation anxiety symptoms items were entered as predictors of class membership. These 15 items were dictated by the diagnostic criteria for SAD as well as the symptoms that can be endorsed in the SAD portion of both the ADIS-IV-C/P and the ADIS-5-C/P (Fig. 2). All items, which are included in both versions of the interview, address the nature and content of the youth’s separation worries and symptoms and asks parents to endorse the presence or absence of SAD symptoms. All items were treated as dichotomous variables (e.g. yes, present or no, absent).
LCA begins with a one-class (e.g., unconditional) model and increase the number of classes until additional increases yield no improvement to the fit of the model [55, 56]. The first step in determining goodness of fit was to examine the Akaike Information Criterion [AIC; 57], Bayesian Information Criterion [BIC; 58], and sample-size adjusted BIC [ABIC; 59] values. The model that produces the smallest absolute values on these three indices was considered that with the best fit. Additionally, it is preferable to rely more heavily on the BIC and ABIC as this usually results in a more parsimonious model. Second, because a common likelihood ratio is incompatible with LCA models, we used the Bootstrap Likelihood Ratio Test (BLRT) to yield p-values for the various model fits to determine the optimal number of classes [60]. Third, class sizes were examined and any models including classes that were composed of less than 5% of the total sample were rejected. Finally, classes were assessed as to whether they are theoretically sound and/or clinically useful.
Once latent classes were identified, tests of equality of means were used to identify significant covariates. Tests of equality of means are optimal as they hold class membership constant and provide Chi square statistics for omnibus and pairwise comparisons across latent classes instead of selecting one class as the referent class for pairwise comparisons. Significant omnibus test statistics (p < 0.05) indicate a covariate that predicts class membership and thus improves model fit. These tests were conducted with FASA scores to determine if scores on said accommodation measure predicts class membership.
Little is known about statistical power for detecting number of classes in LCA [61] and there is disagreement as to how to determine what the appropriate sample size and number of items to yield sufficient power to determine latent classes. Dziak et al. [61] propose that the Cohen’s W measure can be modified to determine power for LCA. This method determines that 186 participants is a sufficient sample size to maintain power at 0.80 if including 15 items, as long as the resultant model is between two and four classes.
Results
Extraction of Latent Classes
LCAs were conducted that specified 2–6 classes (Table 3). Initially, the best fitting model, as indicated by the AIC, BIC and Adjusted BIC, was a five-class model but it was clinically uninformative. The five-class model contained one class that represented less than 10% of the total sample (N = 13) which suggested overfitting. Additionally, the sample size did not provide sufficient power to support an interpretable 5-class model. For this sample, the best fitting model was the three-class solution that provided clinically interpretable information, the most parsimonious solution and, the most meaningful and best fit to the data. As shown in Fig. 1, this model included the following: two classes of individuals whose parents endorsed a moderate number of SAD symptoms (Class 1 and 2) and a class of individuals whose parents did not endorse symptoms of SAD (Class 3). Upon further investigation, it was determined that the parents of individuals in Classes 1 and 2 endorsed symptoms 6, 7, 9–12 and 14 at comparable rates (full ADIS-P SAD symptom probes are listed in Fig. 2). Where there appears to be a meaningful difference is in symptoms 1–5, 8, 13 and 15. These symptoms were endorsed significantly more often by parents of individuals in Class 2 than of those individuals in Class 1. Parents of individuals in Class 2 endorsed their child feeling very anxious and worried when they are not around, doing whatever they can to be with their parents, becoming upset if they know their parent will be leaving, crying and becoming distressed upon separation, avoiding certain places in order to stay close to parents and being unable to engage in sleepovers at higher rates than parents of youth in Class 1. Parents of youth in Classes 1 and 2 endorsed their child worrying that something bad might happen to them or their parents when they are apart, avoiding being alone either in other areas of the house or home alone, staying close during bedtime, experiencing bad dreams about separation and experiencing physical symptoms upon separation or worrying about separation at similar rates. Parents of individuals in Class 3 endorsed low levels of all SAD symptoms with less than 10% of parents of members of this group endorsing 14 out of the 15 total SAD symptoms. The classes were identified as Moderate SAD (Class 1), Interfering SAD (Class 2) and Low SAD (Class 3) (Table 4).
Table 3.
Model fit parameters
| Number of classes | AIC | BIC | ABIC |
|---|---|---|---|
| 1 | |||
| 2 | 2574.70 | 2681.15 | 2576.70 |
| 3 | 2526.74 | 2688.03 | 2529.66 |
| 4 | 2529.68 | 2745.80 | 2533.59 |
| 5 | 2518.68 | 2789.64 | 2523.58 |
AIC Akaike information criterion, BIC Bayesian information criterion, ABIC sample-size adjusted Bayesian information criterion
Fig. 1.
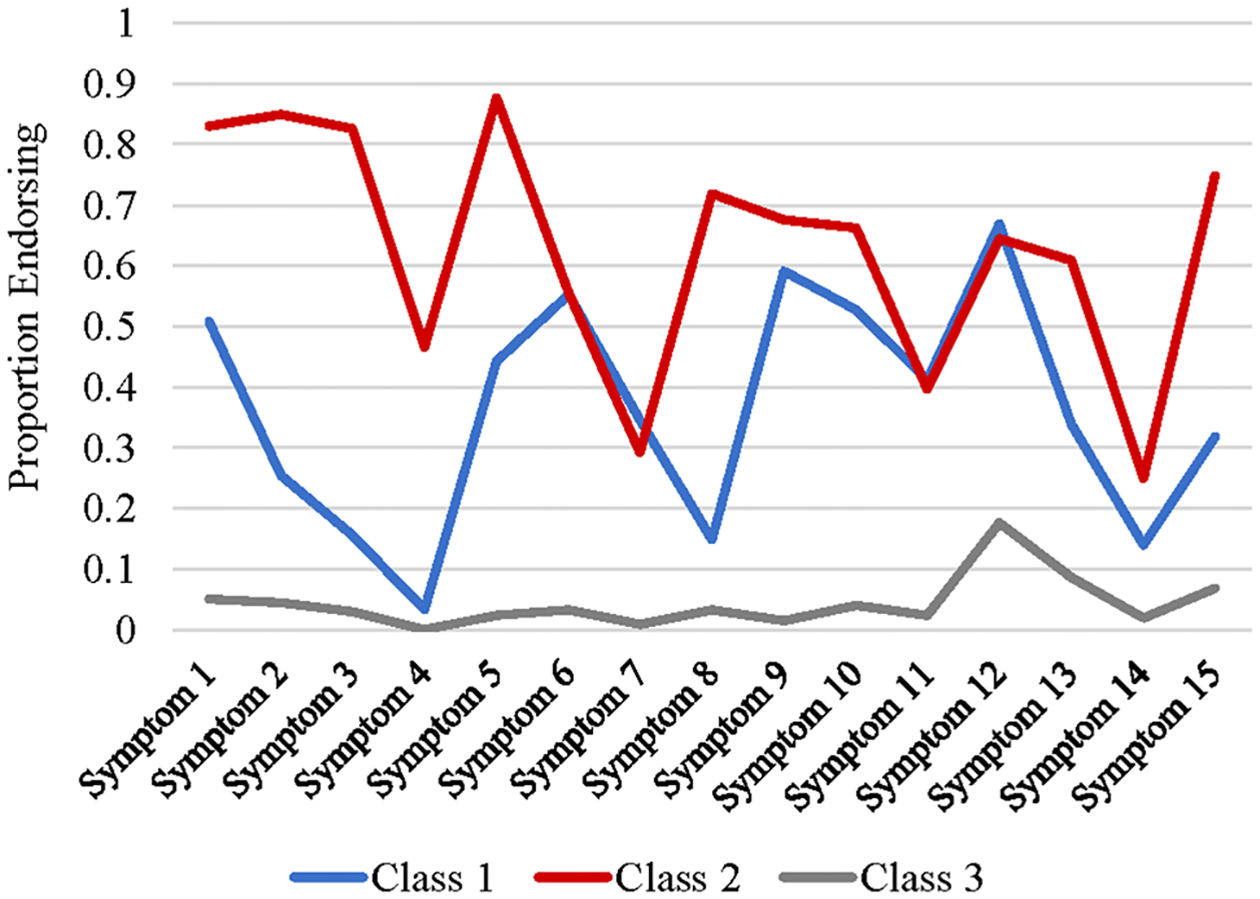
Latent classes by SAD symptoms
Table 4.
Latent classes by SAD symptom endorsement
| SAD symptoms | Class 1 | Class 2 | Class 3 | |||
|---|---|---|---|---|---|---|
| Proportion endorsed | SE | Proportion endorsed | SE | Proportion endorsed | SE | |
| Symptom 1 | 0.51 | 0.10 | 0.83 | 0.07 | 0.05 | 0.13 |
| Symptom 2 | 0.25 | 0.12 | 0.85 | 0.25 | 0.04 | 0.10 |
| Symptom 3 | 0.16 | 0.13 | 0.83 | 0.23 | 0.03 | 0.04 |
| Symptom 4 | 0.03 | 0.03 | 0.47 | 0.25 | 0.00 | 0.00 |
| Symptom 5 | 0.44 | 0.26 | 0.88 | 0.08 | 0.02 | 0.05 |
| Symptom 6 | 0.55 | 0.24 | 0.56 | 0.16 | 0.03 | 0.05 |
| Symptom 7 | 0.35 | 0.26 | 0.29 | 0.26 | 0.01 | 0.01 |
| Symptom 8 | 0.15 | 0.20 | 0.72 | 0.12 | 0.03 | 0.02 |
| Symptom 9 | 0.59 | 0.16 | 0.68 | 0.16 | 0.02 | 0.08 |
| Symptom 10 | 0.53 | 0.21 | 0.66 | 0.10 | 0.04 | 0.04 |
| Symptom 11 | 0.41 | 0.16 | 0.40 | 0.10 | 0.02 | 0.03 |
| Symptom 12 | 0.67 | 0.22 | 0.61 | 0.15 | 0.18 | 0.06 |
| Symptom 13 | 0.34 | 0.17 | 0.61 | 0.10 | 0.09 | 0.05 |
| Symptom 14 | 0.14 | 0.14 | 0.25 | 0.09 | 0.02 | 0.02 |
| Symptom 15 | 0.32 | 0.19 | 0.750 | 0.09 | 0.07 | 0.06 |
SAD separation anxiety disorder; SAD symptom numbers correspond with Figure 2
Comparison of External Validators Among Classes
Potential External Validators
Mean raw scores and proportions for the external validators across classes and omnibus Chi square test statistics are reported in Table 5. Omnibus Chi square analyses did not reveal significant between class difference on measures of parent’s report of parent’s trait anxiety [State-Trait Anxiety Inventory; 62], youth’s report of youth’s broad anxiety [Multidimensional Anxiety Scale for Children-Child Report (MASC-C); 42], absolute difference between youth’s report of youth’s broad anxiety and parents report of youth’s broad anxiety [MASC-C and MASC-P; 42], parent report of parent’s depression [Beck Depression Inventory; 63], youth report of youth’s depression [Child Depression Inventory; 64], parent report of interference of youth’s anxiety [Child Sheehan Disability Scale-Parent Report; 65], youth report of interference of youth’s anxiety [Child Sheehan Disability Scale-Child Report; 65], parent report of youth’s social responsiveness [Social Responsiveness Scale-Parent Report; 66] or on parent report on a global measure of anxiety and depression as well as on the depression and anxiety subscales of said measure [Revised Child Anxiety and Depression Scale (RCADS); 67]. Additionally, classes did not differ significantly on Chi square analyses of proportion of class members meeting diagnostic criteria for Soc, GAD or OCD (Table 6).
Table 5.
Latent class characteristics
| Class 1 | Class 2 | Class 3 | Omnibus χ2 test | Pairwise comparisons | |||||
|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | χ2 | ρ | ||
| Age | 10.94 | 0.41 | 10.33 | 0.36 | 12.96 | 0.31 | 35.11 | 0.00 | 1,2 < 3 |
| FASA | 16.43 | 1.22 | 21.03 | 1.40 | 14.02 | 0.91 | 17.82 | 0.00 | 1,3 < 2 |
| ERC | 47.53 | 1.12 | 48.93 | 1.52 | 44.99 | 1.01 | 5.68 | 0.06 | |
| STAIT | 38.37 | 1.08 | 38.99 | 1.62 | 36.90 | 0.95 | 1.77 | 0.41 | |
| MASC abs | 0.93 | 0.11 | 1.05 | 0.12 | 0.95 | 0.09 | 0.63 | 0.73 | |
| MASC diff | 0.33 | 0.17 | 0.50 | 0.21 | − 0.45 | 0.13 | 22.33 | 0.00 | 3 < 1,2 |
| MASC-C | 50.06 | 2.81 | 49.20 | 3.60 | 50.85 | 2.14 | 0.17 | 0.92 | |
| MASC-P | 60.39 | 1.86 | 64.41 | 3.13 | 49.33 | 1.66 | 29.57 | 0.00 | 1,2 > 3 |
| CDI | 6.05 | 0.96 | 5.91 | 0.88 | 6.31 | 0.68 | 0.15 | 0.93 | |
| BDI | 6.44 | 0.86 | 8.96 | 1.40 | 7.02 | 0.79 | 2.12 | 0.35 | |
| SDS-C | 8.33 | 1.303 | 8.91 | 1.30 | 10.11 | 0.89 | 1.42 | 0.49 | |
| SDS-P | 20.74 | 1.7 | 25.33 | 2.32 | 19.99 | 1.28 | 4.09 | 0.13 | |
| SRSP | 129.65 | 2.85 | 133.31 | 3.36 | 136.21 | 2.14 | 3.21 | 0.20 | |
| RCADS-T | 72.47 | 5.01 | 70.41 | 5.49 | 67.42 | 3.11 | 0.78 | 0.68 | |
| RCADS-Dep | 13.09 | 1.20 | 12.13 | 1.24 | 13.75 | 0.81 | 1.24 | 0.54 | |
| RCADS-Anx | 59.34 | 3.90 | 58.27 | 4.37 | 53.66 | 2.41 | 1.96 | 0.38 | |
| RCADS-Sep | 12.99 | 0.78 | 15.05 | 1.01 | 8.53 | 0.52 | 46.35 | 0.00 | 3 < 1,2 |
| Met Dx criteria | Met Dx criteria | Met Dx criteria | χ2 | ρ | ||
|---|---|---|---|---|---|---|
| SAD | 0.14 | 0.78 | 0.04 | 0.00 | 2 > 1,3 | |
| School Refusal | 0.00 | 0.15 | 0.12 | 0.00 | 1 < 2,3 | |
| Soc | 0.62 | 0.60 | 0.60 | 0.88 | ||
| GAD | 0.89 | 0.77 | 0.75 | 0.17 | ||
| OCD | 0.12 | 0.03 | 0.14 | 0.09 |
| Male | Male | Male | χ2 | ρ | ||
|---|---|---|---|---|---|---|
| Gender | 0.69 | 0.39 | 0.48 | 7.12 | 0.03 | 1v3 |
FASA family accommodation scale—anxiety, ERC emotion regulation checklist, STAIT state-trait anxiety inventory—trait version, MASC C/P multidimensional anxiety scale for children—child and parent report, MASC diff the difference in score between parent self-report of the child’s anxiety severity on the MASC and the child’s self-report of their own anxiety severity on the MASC, MASC abs the absolute value of the difference in score between parent self-report of the child’s anxiety severity on the MASC and the child’s self-report of their own anxiety severity on the MASC, CDI the child depression inventory, BDI the beck depression inventory, SDS-C/P the Sheehan disability scale—parent and child report, SRSP the social responsiveness scale—parent report, RCADS-T/Dep/Anx/Sep revised child anxiety and depression scale—total and depression, anxiety and separation anxiety disorder subscales, SAD separation anxiety disorder, Soc social anxiety disorder, GAD generalized anxiety disorder, OCD obsessive compulsive disorder
Table 6.
Pre-treatment measures
| M | SD | % missing | |
|---|---|---|---|
| FASA | 16.06 | 8.24 | 9.40 |
| MASC difference | − 0.02 | 1.20 | 6.30 |
| MASC parent | 55.94 | 15.71 | 5.20 |
| RCADS-sep | 11.22 | 5.29 | 17.70 |
FASA family accommodation scale—anxiety, MASC multidimensional anxiety scale for children, MASC difference is the difference in score between parent self-report of the child’s anxiety severity on the MASC and the child’s self-report of their own anxiety severity on the MASC, RCADS-sep revised child anxiety and depression scale—separation anxiety disorder subscale
Accommodation
Omnibus Chi square analyses revealed significant between-class differences on parent-report of accommodation of their child’s anxiety symptoms [raw scores on the FASA; 2]. Pairwise comparisons indicated that parents of individuals in Interfering SAD Class reported more accommodation than those of individuals in Moderate SAD Class and Low SAD Class (χ2 = 5.45, ρ 0.02 and χ2 = 17.65, ρ < 0.001, respectively).
Demographics
Omnibus Chi square analyses revealed significant between-class differences on age and gender. Pairwise comparisons indicated that Low SAD Class included significantly older individuals than Moderate SAD Class and Interfering SAD Class (M = 12.95, χ2 = 14.519, ρ < 0.001 and χ2 = 31.01, ρ < 0.001, respectively), while there were no significantly differences in average age between Moderate SAD Class and Interfering SAD Class. Additionally, pairwise comparisons analyzing gender indicated that Moderate SAD Class was more predominately male while Low SAD Class had a balanced gender distribution (χ2 = 5.63, ρ = 0.018). Neither Moderate SAD Class nor Low SAD Class differed significantly from Interfering SAD Class on gender distribution.
Anxiety
Omnibus Chi square analyses revealed significant between-class differences on a parent-report measure of broad youth anxiety [MASC-P; 52]. Pairwise comparisons indicated that parents of individuals in Low SAD Class reported significantly less youth anxiety than those in Moderate SAD Class or Interfering SAD Class (M = 49.33, χ2 = 18.23, ρ < 0.001 and χ2 = 18.23, ρ < 0.001, respectively). Additionally, omnibus Chi square analyses revealed significant between-class differences in the magnitude and direction of difference between raw scores on the MASC-C and the MASC-P. Pairwise comparisons indicated that this value in Low SAD Class was significantly different than in Moderate SAD Class or Interfering SAD Class (χ2 = 12.43, ρ < 0.001 and χ2 = 15.43, ρ < 0.001, respectively). Of note, the average difference score for Low SAD Class was a negative value while the average difference scores for Moderate SAD Class and Interfering SAD Class were positive, indicating that on a whole, parents of individuals in Low SAD Class reported less anxiety severity than their children did, while parents of individuals in Moderate SAD Class and Interfering SAD Class reported more anxiety severity than their children did. Omnibus Chi square analyses also revealed significant between-class differences on the SAD subscale of a parent-report measure of youth anxiety and depression (RCADS-Sep). Pairwise comparisons indicated that parents of individuals in Low SAD Class reported significantly less youth SAD symptoms than those in Moderate SAD Class or Interfering SAD Class (M = 8.53, χ2 = 21.22, ρ < 0.001 and χ2 = 33.16, ρ < 0.001, respectively), consistent with class interpretations. Pairwise comparison between Moderate SAD Class and Interfering SAD Class, however, were non-significant, indicating no class differences on the SAD subscale of he RCADS. Omnibus Chi square analyses revealed no significant between-class differences on the GAD, Soc or Depression subscales of the RCADS.
Diagnostic Criteria
As expected, omnibus Chi square analyses revealed significant between-class differences on proportion of class-members who met diagnostic criteria for SAD. Pairwise comparisons indicated that Interfering SAD Class was more likely to meet diagnostic criteria for SAD than Moderate SAD Class or Low SAD Class (χ2 = 35.88, ρ < 0.001 and χ2 = 94.14, ρ < 0.001, respectively). Additionally, omnibus Chi square analyses revealed significant between-class differences on proportion of class-members who displayed clinically significant school-refusal behavior (as measure by the ADIS-C/P). Pairwise comparisons indicated that Moderate SAD Class was less likely to exhibit clinically significant school-refusal behavior than Interfering SAD Class or Low SAD Class (χ2 = 6.09, ρ = 0.014 and χ2 = 10.44, ρ = 0.001, respectively).
Discussion
As hypothesized, youth presenting for treatment of anxiety exhibit different parent-reported SAD symptoms profiles. Analysis yielded three distinct interpretable classes, best characterized as Low SAD (Class 3), Moderate SAD (Class 1) and Interfering SAD (Class 2). These classes were distinguished not only by SAD symptoms profiles, but also by external validators (FASA, age, gender, MASC and diagnostic criteria). The present findings suggest that characterizing treatment-seeking youth using categorical diagnostic group, rather than examining individual variation along the separation anxiety symptom spectrum, may limit useful information that can influence decisions about pertinent treatment targets.
Class 3 comprises 48.5% of the sample and appears to fit a low SAD profile. This class is characterized by low proportions of parent-reported SAD symptoms across the diagnostic criteria. Less than 10% of parents of members of this group endorsed 14 out of the 15 total SAD symptoms. This “Low SAD” class may be regarded as individuals who do not display clinically significant symptoms of SAD.
In comparison to the “Low SAD” group, Class 1 (comprising of 31.8% of the total sample) and Class 2 (comprising of 19.6% of the total sample) contain members whose parents endorsed significantly more SAD symptoms. Class 1 and Class 2 displayed comparable levels of SAD symptoms 6, 7, 9–12 and 14 (Fig. 2). Parents of members of Class 2, however, endorsed higher rates of their children feeling very anxious and worried when they are not around, doing whatever they can to be with their parents, becoming upset if they know their parent will be leaving, crying and becoming distressed upon separation, avoiding certain places in order to stay close to parents and being unable to engage in sleepovers. These symptoms, especially doing whatever they can to be with their parents, becoming upset if they know their parent will be leaving, crying and becoming distressed upon separation and avoiding certain places in order to stay close to parents, seem to represent symptoms that cause the greatest impairment in day-to-day functioning. These symptoms may be particularly problematic for parents in instances of transition or separation, such as getting ready to leave for school or work or parents leaving the home to attend social or non-work engagements. Youth who cry noticeably upon separation, take action to prevent parents from leaving or display significant distress to other adults upon separation, likely represent a subset of anxious children who cause particular interference in their home environments. Alternatively, youth who display symptoms of SAD such as experiencing bad dreams about separation, experiencing physical symptoms upon separation or worrying about separation, but not other symptoms which may play out as externalizing behaviors, may represent a subset of individuals with SAD who experience less daily interference. As such, Class 1 appears to represent a group of youth experiencing “Moderate SAD” symptoms, while Class 2 is characterized by increased endorsement of more “Interfering SAD” symptoms.
Results from the between-class comparisons on external validators support our expectation that the observed profiles would be associated with different clinical features of SAD. Most notably, the interfering SAD class exhibited elevated scores on a measure of parent accommodation, supporting our hypothesis that difference symptom profiles may be differentially associated with parental accommodation. This is consistent with findings that parent accommodation is positively correlated with the presence of externalizing behaviors and increased functional impairment [3]. In addition, the interfering SAD class was composed of a higher proportion of members meeting full diagnostic criteria for SAD. This result is in concert with findings relating SAD to heightened levels of accommodation [2, 7]. Despite this difference, the moderate SAD and interfering SAD classes displayed similar parent-reported and youth-reported levels of anxiety severity as well as comparable rates of anxiety disorder and non-anxiety disorder co-morbidities. Additionally, these groups scored comparably on a measure of SAD severity (RCADS-Sep). Across multiple external validators (i.e., measures of depression, gender and age) the moderate and interfering classes appear relatively similar aside from the type of separation symptoms endorsed, parent-reported levels of accommodation and proportion of members meeting diagnostic criteria for SAD. These findings support a relationship between particular SAD symptoms (rather than number of total symptoms or symptom severity) and parental accommodation.
It is plausible that the more interfering-type SAD symptoms such as crying upon separation, begging parents to stay home or doing whatever they can to prevent separation might materialize as externalizing behaviors and make instances of transition and separation particularly stressful. Resultantly, it is possible that these types of behavior elicit more instances of parental accommodation. Parents in these cases may feel as though they have no other choice and that accommodations are necessary to make it through the day. This is congruent with findings that parents of youth with SAD endorse accommodations such as allowing the youth to stay home from school, coming home early from events and staying home from work themselves at higher rates than parents of youth with diagnoses of other anxiety disorders [7].
Although this sample shows unique SAD symptoms profiles, the profile most associated with accommodation (the interfering SAD class) was also the one most associated with a diagnosis of SAD, in line with previous research findings [2, 7]. This is likely because this group endorsed the most SAD symptoms, thus warranting a full SAD diagnosis. It is notable, however, that the two groups (moderate SAD and interfering SAD) did not differ on measures of overall anxiety severity or separation anxiety severity (e.g. the MASC-C and the RCADS-SAD subscale). Given these findings, it is likely that some combination of SAD symptoms and other non-SAD anxiety symptoms may be differentially associated with accommodation, rather than presence or severity of SAD as a whole. These findings suggest that a LCA which includes a broader range of anxiety symptoms (not just SAD symptoms) may be useful in identifying what combination of symptoms is differentially associated with accommodation. This could potentially lead to identifying youth who are best suited to accommodation-specific intervention.
Of note, the low SAD class differed significantly in the observed reporting patterns on measures of general anxiety. Although all three classes did not differ significantly on a measure of child-reported anxiety severity, average scores on a measure of parent-reported anxiety severity were significantly lower for the low SAD class than for the moderate and interfering SAD classes. Additionally, the low SAD class was the only class to have a negative average score of parent–child report discrepancy on a measure of anxiety severity—indicating parents reported less anxiety severity than their children on average. This is notable because the pattern of low reporting of SAD in this class might reflect an underreporting pattern, rather than a lack of SAD pathology, on the part of the parent as classes were built using parent-report items. However, previous research on a similar sample found that parent-youth reporting agreement is significantly higher at symptom-level than diagnosis-level, demonstrating that non-agreement on general reporting measures (i.e. the MASC) does not necessarily indicate variation in symptom-level reporting [40].
Overall, findings from the current study highlight how separation anxiety symptoms exist at clinical and sub-clinical levels across a range of anxiety disorders. Examining classes across multiple diagnoses as well as in a sample displaying clinical and sub-clinical symptoms lends to the generalizability of the findings. Additionally, there is a lack of research about the existence of SAD symptoms in other anxiety disorders despite high rates of comorbidity between disorders. More specifically, the findings detail what types of separation concerns are more likely to be associated with accommodation. Although the literature supports that SAD is broadly associated with accommodation, present findings support that some clusters of SAD symptoms are more strongly associated with accommodation than others. Although it is difficult to determine directionality (e.g. whether children with these types of symptoms elicit more accommodation or if highly accommodating families raise children who then display these types of symptom profiles), research has shown high pretreatment levels of accommodation to be associated with attenuated cognitive-behavioral therapy (CBT) and pharmacological outcomes [10], and that reductions in family accommodation predicted improved CBT outcome [68, 69]. Given these findings, knowing symptoms that are more highly related to accommodation can help select those youth who may benefit more from an accommodation-specific intervention. Given the heterogeneity of symptom presentations in anxiety disorders and the comorbidity of diagnostic categories, the findings represent a move in the direction of person-centered and symptom-specific research [70]. This is in line with the NIMH supported paradigm shift towards a dimensional, rather than categorical, diagnostic classification system via the Research Domain Criteria project (RDoC) [71]. Identifying symptom-specific (instead of disorder-specific) clinical correlates will move the field closer to better personalized interventions.
Potential limitations merit consideration. First the LCA included individuals who were seeking treatment for anxiety, but who had not yet been formally diagnosed with an anxiety disorder. This approach increases generalizability to how SAD symptoms present in a broader population, but cannot be interpreted to apply to an entire population with significant anxiety or SAD. Second, the study relied on parent reports of youth SAD symptoms to build the classes. Though appropriate and meaningful, these reports may not provide the entire picture of symptoms experienced by the youth. Parents may be inclined to report symptoms that are most observable or disruptive. Additionally, parents who engage in n high levels of accommodation may not possess insight into their own behavior thus making them unreliable reporters of accommodation. Parent report on child anxiety may also be influenced by parental psychopathology. Third, parent-reports were disproportionally completed by mothers, thus limiting generalizability to father behavior. It is possible that reported relationships may differ across caregivers within two-parent households. Fourth, LCA is exploratory, suggesting the value of replication. Finally, the present analyses did not take into account the duration or severity of the reported symptoms.
Overall, the identified classes offer clinical utility in identifying those anxiety-disordered youth likely to experience parental accommodation. This adds to the body of knowledge which suggests that focusing on symptom-specific, rather than diagnosis-specific, clinical correlates may be a more fruitful approach to identifying which treatments most benefit which individuals. Altogether, this study’s identification of a three-class structure within SAD (low SAD, moderate SAD and interfering SAD) is a step in the direction of pinpointing which anxious youth may benefit most from accommodation-specific interventions.
Summary
Anxiety disorders are common among youth. Accommodation is prevalent amongst families where there is a child with an anxiety disorder. Accommodation is associated with maintenance of anxiety symptoms as well as with attenuated treatment outcomes. Accommodation is most commonly seen in youth with a clinical diagnosis of separation anxiety disorder (SAD). Despite this, youth with SAD experience comparable treatment outcomes to those of youth with other anxiety disorders. The present study utilized latent class analysis to empirically define SAD symptom profiles and elucidate whether specific SAD symptom profiles were differentially associated with accommodation. Analyses resulted in three distinct classes of SAD symptoms. Results suggested that a SAD symptom profile identified as consisting of more interfering SAD symptoms was associated with higher levels of parent-reported accommodation. Further research is needed to determine if anxious youth who fit this interfering SAD symptom profile may experience greater improvement when treated using accommodation-focused treatment modalities.
References
- 1.Calvocoressi L, Lewis B, Harris M, Trufan SJ, Goodman WK, McDougle CJ, Price LH (1995) Family accommodation in obsessive-compulsive disorder. Am J Psychiatry 152:441–443. 10.1176/ajp.152.3.441 [DOI] [PubMed] [Google Scholar]
- 2.Lebowitz ER, Woolston J, Bar-Haim Y, Calvocoressi L, Dauser C, Warnick E et al. (2013) Family accommodation in pediatric anxiety disorders. Depress Anxiety 30:47–54. 10.1002/da.21998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Storch EA, Salloum A, Johnco C, Dane BF, Crawford EA, King MA et al. (2015) Phenomenology and clinical correlates of family accommodation in pediatric anxiety disorders. J Anxiety Disord 35:75–81. 10.1016/j.janxdis.2015.09.001 [DOI] [PubMed] [Google Scholar]
- 4.Kagan ER, Frank HE, Kendall PC (2017) Accommodation in youth with OCD and anxiety. Clin Psychol Sci Pract 24:78–98. 10.1111/cpsp.12186 [DOI] [Google Scholar]
- 5.Lebowitz ER, Panza KE, Bloch MH (2016) Family accommodation in obsessive-compulsive and anxiety disorders: a five-year update. Expert Rev Neurother 16:45–53. 10.1586/14737175.2016.1126181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benito KG, Caporino NE, Frank HE, Ramanujam K, Garcia A, Freeman J et al. (2015) Development of the pediatric accommodation scale: reliability and validity of clinician-and parent-report measures. J Anxiety Disord 29:14–24. 10.1016/j.janxdis.2014.10.004 [DOI] [PubMed] [Google Scholar]
- 7.Thompson-Hollands J, Kerns CE, Pincus DB, Comer JS (2014) Parental accommodation of child anxiety and related symptoms: range, impact, and correlates. J Anxiety Disord 28:765–773. 10.1016/j.janxdis.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lebowitz ER, Scharfstein LA, Jones J (2014) Comparing family accommodation in pediatric obsessive-compulsive disorder, anxiety disorders, and nonanxious children. Depress Anxiety 31:1018–1025. 10.1002/da.22251 [DOI] [PubMed] [Google Scholar]
- 9.Crawford AM, Manassis K (2001) Familial predictors of treatment outcome in childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry 40:1182–1189 [DOI] [PubMed] [Google Scholar]
- 10.Garcia AM, Sapyta JJ, Moore PS, Freeman JB, Franklin ME, March JS, Foa EB (2010) Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I). J Am Acad Child Adolesc Psychiatry 49:1024–1033. 10.1016/j.jaac.2010.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salloum A, Andel R, Lewin AB, Johnco C, McBride NM, Storch EA (2018) Family accommodation as a predictor of cognitive-behavioral treatment outcome for childhood anxiety. Fam Soc 99:45–55 [Google Scholar]
- 12.Mowrer OH (1960) Learning theory and behavior. Wiley, New York. 10.1037/10802-000 [DOI] [Google Scholar]
- 13.Foa EB, Kozak MJ (1986) Emotional processing of fear: exposure to corrective information. Psychol Bull 99:20. 10.1037/0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- 14.Abramowitz JS, Jacoby RJ (2014) Obsessive-compulsive disorder in the DSM-5. Clin Psychol Sci Pract 21:221–235. 10.1111/cpsp.12076 [DOI] [Google Scholar]
- 15.Lebowitz ER, Omer H, Hermes H, Scahill L (2014) Parent training for childhood anxiety disorders: the SPACE program. Cogn Behav Pract 21:456–469. 10.1016/j.cbpra.2013.10.004 [DOI] [Google Scholar]
- 16.Kendall PC, Robin JA, Hedtke KA, Suveg C, Flannery-Schroeder E, Gosch E (2005) Considering CBT with anxious youth? Think exposures. Cogn Behav Pract 12:136–148. 10.1016/s1077-7229(05)80048-3 [DOI] [Google Scholar]
- 17.Peterman JS, Read KL, Wei C, Kendall PC (2015) The art of exposure: putting science into practice. Cogn Behav Pract 22:379–392. 10.1016/j.cbpra.2014.02.003 [DOI] [Google Scholar]
- 18.Swan AJ, Kendall PC (2016) Fear and missing out: youth anxiety and functional outcomes. Clin Psychol Sci Pract 23(4):417–435 [Google Scholar]
- 19.Schleider JL, Lebowitz ER, Silverman WK (2018) Anxiety sensitivity moderates the relation between family accommodation and anxiety symptom severity in clinically anxious children. Child Psychiatry Hum Dev 49(2):187–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shear K, Jin R, Ruscio AM, Walters EE, Kessler RC (2006) Prevalence and correlates of estimated DSM-IV child and adult separation anxiety disorder in the National Comorbidity Survey Replication. Am J Psychiatry 163:1074–1083. 10.1176/ajp.2006.163.6.1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J et al. (2010) Clinical characteristics of anxiety disordered youth. J Anxiety Disord 24:360–365. 10.1016/j.janxdis.2010.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kiesler DJ (1966) Some myths of psychotherapy research and the search for a paradigm. Psychol Bull 65:110 [Google Scholar]
- 23.Ashley EA (2015) The precision medicine initiative: a new national effort. JAMA 313:2119–2120 [DOI] [PubMed] [Google Scholar]
- 24.DeRubeis RJ, Cohen ZD, Forand NR, Fournier JC, Gelfand LA, Lorenzo-Luaces L (2014) The Personalized Advantage Index: translating research on prediction into individualized treatment recommendations. A demonstration. PLoS ONE 9:e83875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K et al. (2010) Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 167:748–751 [DOI] [PubMed] [Google Scholar]
- 26.Hamburg MA, Collins FS (2010) The path to personalized medicine. N Engl J Med 363:301–304 [DOI] [PubMed] [Google Scholar]
- 27.Fisher AJ, Bosley HG, Fernandez KC, Reeves JW, Soyster PD, Diamond AE, Barkin J (2019) Open trial of a personalized modular treatment for mood and anxiety. Behav Res Ther 116:69–79 [DOI] [PubMed] [Google Scholar]
- 28.Galatzer-Levy IR, Bryant RA (2013) 636,120 ways to have post-traumatic stress disorder. Perspect Psychol Sci 8:651–662 [DOI] [PubMed] [Google Scholar]
- 29.Nelemans SA, Hale WW, Branje SJ, Raaijmakers QA, Frijns T, van Lier PA, Meeus WH (2014) Heterogeneity in development of adolescent anxiety disorder symptoms in an 8-year longitudinal community study. Dev Psychopathol 26:181–202 [DOI] [PubMed] [Google Scholar]
- 30.Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR et al. (2012) Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav Ther 43:666–678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chorpita BF, Weisz JR (2009) MATCH-ADTC: modular approach to therapy for children with anxiety, depression, trauma, or conduct problems. PracticeWise, Satellite Beach [Google Scholar]
- 32.Hofmann SG, Hayes SC (2019) The future of intervention science: process-based therapy. Clin Psychol Sci 7:37–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Compton SN, Peris TS, Almirall D, Birmaher B, Sherrill J, Kendall PC et al. (2014) Predictors and moderators of treatment response in childhood anxiety disorders: results from the CAMS trial. J Consult Clin Psychol 82:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barmish AJ, Kendall PC (2005) Should parents be co-clients in cognitive-behavioral therapy for anxious youth? J Clin Child Adolesc Psychol 34:569–581 [DOI] [PubMed] [Google Scholar]
- 35.Silverman WK, Albano AM (1996) Anxiety Disorders Interview Schedule for DSM-IV: child interview schedule, vol 2. Graywind Publications, New York. 10.1037/t28577-000 [DOI] [Google Scholar]
- 36.O’Neil KA, Puleo CM, Benjamin CL, Podell JL, Kendall PC (2012) Suicidal ideation in anxiety-disordered youth. Suicide Life Threat Behav 42:305–317. 10.1111/j.1943-278x.2012.00091.x [DOI] [PubMed] [Google Scholar]
- 37.Lyneham HJ, Abbott MJ, Rapee RM (2007) Interrater reliability of the anxiety disorders interview schedule for DSM-IV: child and parent version. J Am Acad Child Adolesc Psychiatry 46:731–736. 10.1097/chi.0b013e3180465a09 [DOI] [PubMed] [Google Scholar]
- 38.Silverman WK, Saavedra LM, Pina AA (2001) Test-retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: child and parent versions. J Am Acad Child Adolesc Psychiatry 40:937–944. 10.1097/00004583-200108000-00016 [DOI] [PubMed] [Google Scholar]
- 39.Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V (2002) Concurrent validity of the anxiety disorders section of the anxiety disorders interview schedule for DSM-IV: child and parent versions. J Clin Child Adolesc Psychol 31:335–342. 10.1207/s15374424jccp3103_05 [DOI] [PubMed] [Google Scholar]
- 40.Comer JS, Kendall PC (2004) A symptom-level examination of parent–child agreement in the diagnosis of anxious youths. J Am Acad Child Adolesc Psychiatry 43:878–886 [DOI] [PubMed] [Google Scholar]
- 41.Rynn MA, Barber JP, Khalid-Khan S, Siqueland L, Dembiski M, McCarthy KS, Gallop R (2006) The psychometric properties of the MASC in a pediatric psychiatric sample. J Anxiety Disord 20:139–157 [DOI] [PubMed] [Google Scholar]
- 42.March JS, Parker JD, Sullivan K, Stallings P, Conners CK (1997) The multidimensional anxiety scale for children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 36:554–565 [DOI] [PubMed] [Google Scholar]
- 43.Wei C, Hoff A, Villabø MA, Peterman J, Kendall PC, Piacentini J et al. (2014) Assessing anxiety in youth with the multidimensional anxiety scale for children. J Clin Child Adolesc Psychol 43(4):566–578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Villabø M, Gere M, Torgersen S, March JS, Kendall PC (2012) Diagnostic efficiency of the child and parent versions of the multidimensional anxiety scale for children. J Clin Child Adolesc Psychol 41:75–85 [DOI] [PubMed] [Google Scholar]
- 45.Spence SH (1998) A measure of anxiety symptoms among children. Behav Res Ther 36(5):545–566 [DOI] [PubMed] [Google Scholar]
- 46.Chorpita BF, Moffitt CE, Gray J (2005) Psychometric properties of the revised child anxiety and depression scale in a clinical sample. Behav Res Ther 43:309–322 [DOI] [PubMed] [Google Scholar]
- 47.Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE (2000) Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther 38(8):835–855 [DOI] [PubMed] [Google Scholar]
- 48.Ferdinand RF, van Lang ND, Ormel J, Verhulst FC (2006) No distinctions between different types of anxiety symptoms in pre-adolescents from the general population. J Anxiety Disord 20(2):207–221 [DOI] [PubMed] [Google Scholar]
- 49.Mathyssek CM, Olino TM, Hartman CA, Ormel J, Verhulst FC, Van Oort FV (2013) Does the revised child anxiety and depression scale (RCADS) measure anxiety symptoms consistently across adolescence? The TRAILS study. Int J Methods Psychiatr Res 22(1):27–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muthén LK, Muthén BO (1998–2017) Mplus user’s guide (8th ed). Muthén & Muthén, Los Angeles [Google Scholar]
- 51.Corp IBM (2012) IBM SPSS statistics for windows, version 21.0. IBM Corp, Armonk [Google Scholar]
- 52.McCutcheon AL (1987) Latent class analysis. Sage Publications Inc, Newbury Park [Google Scholar]
- 53.Bates ME (2000) Integrating person-centered and variable-centered approaches in the study of developmental courses and transitions in alcohol use: introduction to the special section. Alcohol Clin Exp Res 24:878–881. [PubMed] [Google Scholar]
- 54.Muthén B, Muthén LK (2000) Integrating person centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res 24:882–891. 10.1111/j.1530-0277.2000.tb02070.x [DOI] [PubMed] [Google Scholar]
- 55.Nylund KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model: Multidiscip J 14:535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- 56.Nylund K, Bellmore A, Nishina A, Graham S (2007) Subtypes, severity, and structural stability of peer victimization: what does latent class analysis say? Child Dev 78:1706–1722. 10.1111/j.1467-8624.2007.01097.x [DOI] [PubMed] [Google Scholar]
- 57.Akaike H (1987) Factor analysis and AIC. Psychometrika 52:317–332. 10.1007/bf02294359 [DOI] [Google Scholar]
- 58.Schwartz G (1978) Estimating the dimension of a model. Ann Stat 6:461–464. 10.1214/aos/1176344136 [DOI] [Google Scholar]
- 59.Sclove SL (1987) Application of model-selection criteria to some problems in multivariate analysis. Psychometrika 52:333–343. 10.1007/bf02294360 [DOI] [Google Scholar]
- 60.McLachlan G, Peel D (2000) Mixtures of factor analyzers. Finite Mix Models. 10.1002/0471721182.ch8 [DOI] [Google Scholar]
- 61.Dziak JJ, Lanza ST, Tan X (2014) Effect size, statistical power, and sample size requirements for the bootstrap likelihood ratio test in latent class analysis. Struct Equ Model: Multidiscip J 21:534–552. 10.1080/10705511.2014.919819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Spielberger CD, Gorsuch RL (1983) State-trait anxiety inventory for adults: sampler set: manual, test, scoring key. Mind Garden, Redwood City [Google Scholar]
- 63.Beck AT, Steer RA, Brown GK (1996) Beck depression inventory-II. San Antonio 78(2):490–498 [Google Scholar]
- 64.Kovacs M (1992) Children’s depression inventory. Multi-Health Systems, North Tonawanda [Google Scholar]
- 65.Whiteside SP (2009) Adapting the Sheehan disability scale to assess child and parent impairment related to childhood anxiety disorders. J Clin Child Adolesc Psychol 38(5):721–730 [DOI] [PubMed] [Google Scholar]
- 66.Constantino J (2005) Social responsiveness scale, parent report. Western Psychological Services, Los Angeles [Google Scholar]
- 67.Chorpita BF, Ebesutani C, Spence SH (2015) Revised children’s anxiety and depression scale. https://www.childfirst.ucla.edu/wpcontent/uploads/sites/163/2018/03/RCADSUsersGuide20150701.pdf
- 68.Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA (2009) Decreased family accommodation associated with improved therapy outcome in pediatric obsessive–compulsive disorder. J Consult Clin Psychol 77:355. 10.1037/a0012652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rudy BM, Lewin AB, Geffken GR, Murphy TK, Storch EA (2014) Predictors of treatment response to intensive cognitive-behavioral therapy for pediatric obsessive-compulsive disorder. Psychiatry Res 220:433–440. 10.1016/j.psychres.2014.08.002 [DOI] [PubMed] [Google Scholar]
- 70.Nandi A, Beard JR, Galea S (2009) Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: a systematic review. BMC Psychiatry 9:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Insel TR (2014) The NIMH research domain criteria (RDoC) project: precision medicine for psychiatry. Am J Psychiatry 171(4):395–397 [DOI] [PubMed] [Google Scholar]


