Abstract
Almost one third of adults in the United States have hypertension. Prevalence data among different racial or ethnic groups indicate that a disproportionate number of African Americans have hypertension compared with non‐Hispanic whites and Mexican Americans. Earlier onset of high blood pressure and greater severity of hypertension contribute to a greater burden of hypertensive target organ damage in African Americans and may be a factor in the shorter life expectancy of this population compared with white Americans. There is a clear need for improved management of hypertension in African Americans via therapeutic lifestyle interventions and pharmacotherapy. While there is some evidence that particular antihypertensive agent classes provide blood pressure‐lowering advantages over others, there is no support for withholding agents of any one class. When given as monotherapy, diuretics and calcium channel blockers may be relatively more effective in lowering blood pressure in African Americans than β blockers, angiotensin‐converting enzyme inhibitors, and angiotensin II receptor blockers. However, when combined with a diuretic, African Americans respond as well to these agents as other racial groups. Combination therapy using antihypertensive agents with differing modes of action provides additive antihypertensive efficacy and is well tolerated. Recent guidelines recommend combination therapy as the standard of care for patients with significant blood pressure elevation, especially those with diabetes mellitus and renal disease. These comorbidities are more common in African Americans and indicate the potential need for initial therapy with more than one agent or a combination of agents in one pill.
Almost one third of adults in the United States have hypertension. 1 However, a disproportionate number of African Americans have hypertension, which is generally of greater severity, develops at a younger age, and is associated with more clinical sequelae in this racial group than in age‐matched non‐Hispanic whites and Mexican Americans. 2 , 3 Growing realization of the importance of high blood pressure (BP) as an independent risk factor for a number of serious cardiovascular and renal conditions, along with the availability of a wide variety of BP‐lowering agents, has resulted in a decreasing prevalence of hypertension in both African‐American and non‐Hispanic white populations between the periods of 1976 to 1980 and 1988 to 1994. 1 However, data for the period of 1999 to 2002 show that the prevalence of hypertension increased in these populations, rising to approximately 40% in African Americans (Figure 1). 1 The most recent data for the United States estimated that the prevalence of hypertension, defined as systolic BP (SBP) ≥140 mm Hg or diastolic BP (DBP) ≥90 mm Hg, was 41.8% in African‐American men compared with 30.6% in white men, and 45.4% in African‐American women compared with 31.0% in white women. 1 An analysis of the Third National Health and Nutrition Examination Survey (NHANES III) 4 in children has indicated that differences in BP between black and white women are evident before the age of 10 years.
Figure 1.
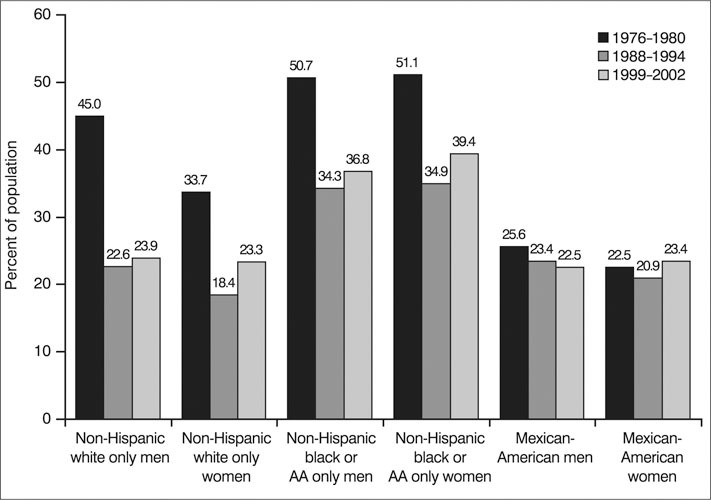
Age‐adjusted prevalence trends for hypertension (systolic blood pressure [BP] ≥140 mm Hg or diastolic BP ≥90 mm Hg) in Americans aged 20–74 years participating in the National Health and Nutrition Examination Surveys (NHANES) for 1976–1980, 1988–1994, and 1999–2002. Data are based on a single BP measurement. AA=African American. Reproduced with permission from Heart Disease and Stroke Statistics—2005 Update. 1 ©2005, American Heart Association.
THE SPECIAL CHALLENGE OF HYPERTENSION IN AFRICAN AMERICANS
It is widely appreciated that hypertension is a key independent risk factor for diseases such as heart failure, coronary heart disease, stroke, and end‐stage renal failure. 5 Among African Americans, an earlier onset of high BP and greater severity of hypertension are likely contributors to the greater mortality rate from heart disease and shorter life expectancy of this population relative to whites. 6 In particular, African Americans have a 1.8‐fold greater incidence of fatal stroke, a 1.5‐fold greater incidence of heart disease mortality, and a 4.2‐fold greater incidence of end‐stage renal disease than the general population. 7
Mortality rates for specific cardiovascular diseases have been compared between residents aged 25 to 64 years in New York City (n=7,322,564) and central Harlem (n=115,483) using 1990 data. 8 The analysis found that central Harlem residents were at least twice as likely to have a fatal cardiovascular disease event as age‐matched New York City residents and that hypertension‐related deaths were the greatest contributor to the excess morality rate. In 2002, the overall US mortality rate attributed to elevated BP was 17.1% 1 When analyzed according to race and gender, African Americans, particularly men, had a disproportionately high BP‐related death rate: 49.6% and 40.5% for African‐American men and women, respectively, compared with 14.4% and 13.7% for white men and women. 1
The disparity in hypertension‐related mortality between African‐American and white populations does not appear to be due to differences in awareness of hypertension, but may be explained by demographic differences including an aging population and increasing body mass indices. 9 Of concern, in terms of the greater prevalence of hypertension in African Americans, a review of a cohort of 6368 African Americans who described themselves as hypertensive found that almost 40% were not receiving BP‐lowering therapy. 10 Among these patients, half had never received antihypertensive therapy. Enhanced awareness of hypertension management guidelines among physicians who care for African Americans is clearly warranted.
It is evident, therefore, that normalizing BP in hypertensive African‐American patients continues to remain a challenge and a priority. Primary care providers, including physicians, physician assistants, and nurse practitioners must overcome any misconceptions they may have that lowering BP is inherently more difficult in African Americans than in other individuals and work with their patients to ensure that effective education and therapy are maintained and are in line with current guidelines. This will aid in protecting target organs from hypertension‐related damage and reduce cardiovascular and renal morbidity and mortality.
SPECIFIC RISK FACTORS FOR HYPERTENSION IN AFRICAN AMERICANS
The pathophysiology of hypertension is multifactorial; however, a number of important causal factors have been identified, including obesity, physical inactivity, excess alcohol intake, excess dietary sodium, and inadequate dietary intake of potassium, fruits, and vegetables. 11 , 12 Specific factors that may be associated with the increased risk of greater than optimal BP and hypertension in African Americans compared with whites include a higher prevalence of obesity, particularly in women 12 ; a higher incidence of various clinical markers associated with hypertension, such as a low birth weight; and a strong family history of cardiovascular disease, type 2 diabetes mellitus, and premature heart disease. 13 , 14 Several pathophysiologic factors have been postulated, such as cellular sodium transport defects and lower levels of natriuretic vasodilator prostaglandins and kinins, which may also contribute to the increased risk of hypertension in this population. Nevertheless, there are important socioeconomic and health systems‐related concerns that are associated with disproportionate hypertensive morbidity and mortality, including inadequate access to health care services and accurate health‐related information. 9 , 15
The multiple risk factors prevalent in African Americans and the fact that they are often undertreated for these risk factors make this population particularly susceptible to end‐organ damage and, consequently, excess hypertension‐related morbidity and mortality. However, as in other populations, many of the risk factors identified as being particularly prevalent in African Americans are modifiable with lifestyle changes and appropriate pharmacotherapy. 16
IMPORTANCE OF ACHIEVING TARGET BP LEVELS IN AFRICAN AMERICANS
There is much evidence supporting the importance of lowering BP to target levels in all hypertensive patients. Even a modest decrease in BP has the potential to significantly reduce hypertension‐related morbidity and mortality. For example, it has been estimated that lowering SBP by 5 mm Hg across the population would reduce the incidence of fatal stroke by 14%, fatal coronary heart disease by 9%, and all‐cause mortality by 7%. 17 Data from a meta‐analysis of 61 prospective studies involving almost 1 million individuals suggest that even when BP is normal, the increase in risk of ischemic heart disease and stroke mortality is progressive and linear from SBP levels ≥115 mm Hg and DBP levels ≥75 mm Hg (i.e., before reaching the conventional definition of hypertension of SBP ≥140 mm Hg or DBP ≥90 mm Hg). 18 Indeed, if the population levels of SBP were lowered by 2 mm Hg, this would translate into approximately 7% lower mortality from ischemic heart disease or other vascular causes and 10% lower risk of stroke mortality in middle age.
The larger burden of risk in African Americans indicates that it is particularly important to achieve target BP levels in this population. Contrary to the belief that many physicians have that it is inherently more difficult to lower BP in African Americans than in whites and that the outcome of therapy can therefore be expected to be less than optimal, 13 the benefits of BP‐lowering therapy may actually be particularly large in this population. 19 For example, the Hypertension Detection and Follow‐up Program (HDFP) 20 showed that the reduction in all‐cause mortality using a stepped‐care approach to BP‐lowering was greater in blacks (who comprised 44% of the 10,940 study population) than whites. Clinical trials that have included a large number of African Americans have demonstrated that BP can be controlled in even the most challenging and/or difficult‐to‐treat patients. Examples of such trials include the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), 21 which included patients with hypertension and one or more additional risk factors for coronary heart disease, and the African American Study of Kidney Disease and Hypertension (AASK), 22 , 23 , 24 which included patients with hypertensive renal disease. ALLHAT included 10,702 non‐Hispanic black participants (35% of the trial population), 21 and AASK included 1094 African American patients. 22 Two thirds of the patients in ALLHAT achieved BP control (<140/90 mm Hg) after 5 years of treatment with chlorthalidone, amlodipine, or lisinopril, although BP control rates were lower for black men than non‐black men (63.3% vs. 70.0%) and for black women than non‐black women (58.8% vs. 65.2%). 25 In AASK, patients who received ramipril, amlodipine, or metoprolol for 3 to 6.4 years had BP recordings of <140/90 mm Hg at over 50% of visits during treatment. 22 The International Verapamil/ Trandolapril Study (INVEST) 26 enrolled 22,576 hypertensive patients with coronary artery disease, 13% (n=3029) of whom were black. Although the BP control rate at 2 years was higher among Caucasians than blacks (62% vs. 49%), 27 there was no difference between the two races in the primary outcome of death, nonfatal myocardial infarction, or nonfatal stroke. 26
Recommended Target BP Levels in African Americans
A recent consensus statement from the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks (ISHIB) 13 provides a practical and evidence‐based tool for achieving BP goals in African‐American patients. Recommendations for BP targets in this guideline are based on evidence from large clinical trials such as ALLHAT and AASK, existing guidelines, and expert opinion. The BP goal recommended by ISHIB is <140/90 mm Hg for patients with uncomplicated hypertension, but lower goals are recommended for individuals with hypertension plus additional risk factors (Table). Many patients are likely to require two or more antihypertensive agents to achieve these goals. For all patients, emphasis is placed on the importance of achieving meaningful reductions in both the systolic and diastolic components of BP.
Table.
Blood Pressure Targets for African Americans
| Target Blood Pressure* (mm Hg) | ||
|---|---|---|
| Diagnosis | SBP | DBP |
| Uncomplicated hypertension | <140 | <90 |
| Hypertension plus nondiabetic renal disease with proteinuria ≤1 g/d | <140 | <90 |
| Hypertension plus nondiabetic renal disease with proteinuria >1 g/d | <130 | <80 |
| Hypertension plus type 2 diabetes mellitus (with or without nephropathy) | <130 | <80 |
| Hypertension plus history of a cardiovascular event, stroke, or transient ischemic attack; target organ damage (including microalbuminuria); or high‐risk or presence of coronary heart disease | <130 | <80 |
| *Recommends combination therapy as initial therapy for patients whose systolic blood pressure (SBP) is ≥15 mm Hg or whose diastolic blood pressure (DBP) is ≥10 mm Hg above goal. Recommendations in the Consensus Statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med. 2003;163:525–541. 13 | ||
Components of an Effective Plan for BP Control
An effective plan for BP control in the African‐American patient will involve a cardiovascular risk assessment followed by determination of the appropriate BP goal, identification of modifiable risk factors, appropriate lifestyle changes (followed by assistance to make such changes), and selection of the most appropriate pharmacotherapeutic regimen. 13 Cardiovascular risk assessment involves consideration of the patient's medical and family history (including risk factors for high BP), physical examination, and laboratory studies to identify those at high risk for cardiovascular events. Framingham risk charts, developed using data from the Framingham Heart Study, 28 can be used to estimate the risk of coronary heart disease in individual patients. Although the Framingham Heart Study did not include a significant African‐American population, the Framingham coronary heart disease functions have been subsequently validated in African Americans and other ethnic groups. 29
STRATEGIES TO TARGET MODIFIABLE RISK FACTORS AND REDUCE BP IN AFRICAN AMERICANS
The ultimate goal of antihypertensive therapy is to delay, prevent, or reverse BP‐related end‐organ damage. As part of the overall management strategy, it is important that patients are made aware of the seriousness of high BP and uncontrolled hypertension in terms of irreversible damage to the heart, blood vessels, brain, kidneys, and eyes, and the increased risk of cardiovascular, cerebrovascular, and renal morbidity and mortality associated with such damage. 13 Maximum benefits to patients will be seen when pharmacotherapy is combined with other strategies to reduce modifiable risk factors. 30
Therapeutic Lifestyle Interventions
Therapeutic lifestyle changes should be implemented to reduce or eliminate modifiable risk factors for high BP. Diet and physical activity goals are particularly important for African‐American individuals, given the high sodium and low potassium intake and the high prevalence of obesity and inadequate physical activity levels in this population. 1
The importance of diet has been underlined by the findings of the Dietary Approaches to Stop Hypertension (DASH) trial, 31 which involved 459 hypertensive patients, 60% (n=275) of whom were black, with a baseline BP of 131.3/84.7 mm Hg. A diet rich in fruits, vegetables, fiber, and low‐fat dairy foods, along with reduced saturated and total fat, significantly reduced SBP and DBP over 8 weeks, despite maintaining weight status and without attempting to restrict salt intake. The beneficial effects of this diet were especially pronounced in black patients. Even greater effects on BP were seen when sodium restriction was added to the DASH diet and, again, these effects were particularly notable in black patients. 32 While the focus has been on moderating sodium intake, it has been recommended that dietary interventions should also increase potassium intake because of the benefits of potassium in reducing BP. 33 , 34
Achieving weight loss is also an important goal, as this should translate into a decrease in BP. The weight loss arm of the Trials of Hypertension Prevention II, 35 which involved 1191 overweight individuals (17.5% of whom were black) with DBP 83–89 mm Hg and SBP <140 mm Hg, showed that a modest reduction in body weight of 4.5 kg (approximately 10 pounds) at 6 months, and maintained for an additional 36 months, was associated with sustained reductions in BP. In addition, patients should also be encouraged to increase their exercise levels, cease smoking, limit their alcohol intake, and have their cholesterol levels monitored. 13
Although lifestyle interventions are important in managing hypertension in African‐American patients, pharmacotherapy should not be overlooked since it may be crucial in ensuring that patients are treated adequately and sufficiently early to maintain an appropriate BP and prevent the consequences of uncontrolled hypertension.
PHARMACOLOGIC INTERVENTIONS
A large number of BP‐lowering drugs have been approved for the treatment of hypertension. They fall into several therapeutic classes including thiazide (and thiazide‐like) diuretics, calcium channel blockers (CCBs), β blockers, angiotensin‐converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), direct‐acting vasodilators, and central α‐agonists. Although there is some evidence that particular drug classes provide advantages over others, all classes of antihypertensive agents have BP‐lowering efficacy in hypertensive African Americans, and there is no support for withholding any one particular class of agents when treating this population. 19
DRUG SELECTION CONSIDERATIONS
When given as monotherapy, diuretics and CCBs have been reported to exert relatively greater BP‐lowering efficacy in African Americans compared with other classes of antihypertensives, such as β blockers, ACE inhibitors, and ARBs. 36 , 37 , 38 However, there is some controversy surrounding this observation because of the limitations of the studies reporting such data. For example, some studies have reported patients achieving a BP reduction of 10 mm Hg, rather than those achieving target BP, or have not reported patients' SBP responses. 13 Not only are there apparent variations among racial and ethnic groups in the therapeutic response to different agents, but there also appears to be wide variations within those groups that are similar, or even greater than, the between‐group differences.
Most African Americans will require treatment with more than one class of antihypertensive agent to achieve BP control. Both the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) and the ISHIB Consensus Statement recommend initiating treatment with combination therapy, usually with a thiazide diuretic plus another agent (e.g., ACE inhibitor, ARB, or β blocker), if the BP is >20/10 mm Hg (JNC 7) or ≥15/10 mm Hg (ISHIB) above the target BP. 5 , 13 The ISHIB guidelines recommend using an ACE inhibitor or an ARB as a component of combination therapy for patients with renal insufficiency or diabetic nephropathy. 13 A clinical algorithm for achieving target BP in African Americans, as recommended by ISHIB, is described in Figure 2.
Figure 2.
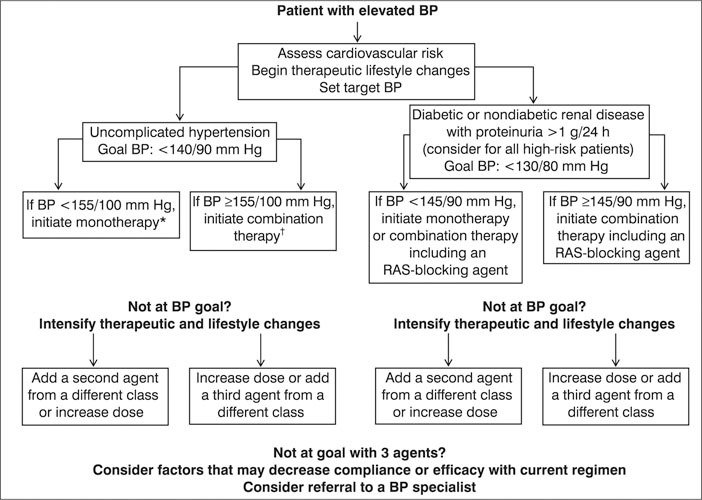
Clinical algorithm for achieving target blood pressure (BP) in African‐American patients, as recommended by the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. RAS=renin‐angiotensin system; *initiate monotherapy at usually recommended doses with a diuretic, β blocker, calcium channel blocker (CCB), angiotensin‐converting enzyme (ACE) inhibitor, or angiotensin receptor blocker (ARB); †initiate low‐dose combination therapy with an ACE inhibitor/diuretic, ARB/diuretic, β blocker/diuretic, or ACE inhibitor/CCB combination. Reproduced with permission from Arch Intern Med. 2003;163:525–541. 13
Diuretics
Thiazide (and thiazide‐like) diuretics are the mainstay of antihypertensive treatment and are unsurpassed at preventing cardiovascular complications of hypertension. 5 , 19 In ALLHAT, the BP‐lowering efficacy of a diuretic (chlorthalidone) was superior to that of an ACE inhibitor (lisinopril) and there was a lower relative risk of stroke in black patients receiving diuretic therapy compared with those receiving an ACE inhibitor. 21 Although thiazide diuretics are well tolerated by African Americans, high doses should be avoided because of the potential for hypokalemia, particularly in patients who do not restrict their sodium intake. 13
Calcium Channel Blockers
In ALLHAT, the diuretic chlorthalidone was superior to the dihydropyridine CCB amlodipine for the prevention of heart failure, although the two agents had similar overall benefits in cardiovascular disease prevention. 21 A number of other studies, including ALLHAT, have shown that, in addition to their BP‐lowering efficacy, CCBs reduce stroke and cardiovascular events to a similar extent as diuretics 21 , 39 and β blockers. 26 , 39 However, the AASK study found that amlodipine was less renoprotective than the ACE inhibitor ramipril in African‐American patients with hypertensive renal insufficiency, especially with significant proteinuria. 22
ACE Inhibitors
Agents of this class are well tolerated and have been found to be beneficial for the prevention of cardiovascular events and target organ protection in patients with diabetes mellitus, congestive heart failure, and diabetic nephropathy, and in post‐myocardial infarction patients. 22 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 Given the considerable data supporting the benefits of ACE inhibitors in reducing cardiac events in patients with congestive heart failure and the high prevalence of heart failure among African Americans, ACE inhibitors are especially recommended in this patient group. 13
The AASK trial provided strong evidence that ACE inhibitors have a greater renoprotective effect in African‐American patients with hypertensive nephrosclerosis and proteinuria than β blockers or CCBs, independently of their effects on BP. 22 However, there is some controversy as to whether ACE inhibitors should be used as initial therapy in diabetic patients without nephropathy. 13 Also, a limitation of ACE inhibitor therapy in African Americans is the higher risk of developing ACE inhibitor‐associated cough or angioedema compared with white patients. 48
Angiotensin II Receptor Blockers
ARBs are associated with a lower incidence of cough than ACE inhibitors and only rare instances of angioedema. 49 ISHIB hypertension guidelines recommend that patients with intolerable cough on an ACE inhibitor be switched to an ARB. 13 Clinical trials have demonstrated the BP‐lowering efficacy of ARBs in African Americans, particularly when combined with hydrochlorothiazide. 50 , 51 Strong BP‐independent renoprotective effects have been documented with monotherapy with the ARBs irbesartan and losartan in randomized, double‐blind, placebo‐controlled trials in patients with diabetic nephropathy, which included almost 500 black patients. 52 , 53 , 54
The Losartan Intervention For Endpoint reduction in hypertension study (LIFE) 55 , 56 in patients with hypertension and left ventricular hypertrophy showed that losartan‐based treatment prevented more cardiovascular morbidity and mortality than atenolol‐based treatment, despite equivalent reductions in BP. Similar benefits were not observed among the 533 black participants, but this sub‐analysis may have been limited by the relatively small number of events in this patient group. 57
ARBs appear to benefit patients with heart failure. In the Valsartan Heart Failure Trial (Val‐HeFT), 58 adding valsartan to existing therapy in patients with chronic heart failure improved outcome and lowered BP by an average of 5 mm Hg more vs. placebo. However, in the small black subpopulation (n=344), the wide confidence interval for the relative risk of the primary combined end point encompassed 1.0. Moreover, in the overall population, the triple combination of valsartan plus an ACE inhibitor and β blocker had an adverse effect on mortality. Further trials will clarify whether this represents a true interaction.
Beta Blockers
Agents of this class are especially effective in patients with stable and unstable angina 59 , 60 and they have been shown to be beneficial in reducing mortality in African‐American patients following myocardial infarction. 61 Therefore, hypertension guidelines recommend that β blockers be used in patients with hypertension and myocardial ischemia or acute coronary syndromes. 13
Central α Agonists
Although drugs such as clonidine, methyldopa, and reserpine are rarely used as monotherapy or initial therapy, clinical experience has shown that they are equally effective in blacks and whites when used in combination with a diuretic. 13 Furthermore, these agents may be more affordable for the disproportionate number of low‐income patients among African‐American individuals.
BENEFITS OF COMBINATION THERAPY IN AFRICAN AMERICANS
As noted above, there is evidence to suggest that, when given as monotherapy, β blockers, ACE inhibitors, and ARBs are not as effective as diuretics in lowering BP in African Americans compared with whites. 21 , 37 , 38 , 62 This finding may be attributed to factors such as a greater prevalence of obesity (especially in women) as well as an excess prevalence of salt‐sensitive hypertension and low plasma renin activity in the African‐American population. 2 , 15 However, a key point that needs to be considered is that when given in combination with a diuretic, African Americans respond as well to β blockers, ACE inhibitors, and ARBs as other racial groups. 62
Combination therapy using antihypertensive agents with differing mechanisms of action confers an additive BP‐lowering benefit compared with monotherapy. 63 , 64 , 65 , 66 Relative to high‐dose monotherapy, the combination of two agents with complementary/differing mechanisms of action produces additional decreases in SBP and DBP in the range of 8 to 11 mm Hg and 4 to 6 mm Hg, respectively. 13 A number of large, randomized controlled trials have indicated that combination therapy with at least two BP‐lowering agents is required to achieve target BP goals in many patients with uncomplicated hypertension, 21 , 39 , 67 , 68 and a similar trend is evident when considering the African‐American population separately. In the AASK trial, hypertensive African Americans with mild‐to‐moderate renal disease required at least two agents to achieve a reduction in mean arterial pressure of approximately 10 mm Hg. 22
Aside from the efficacy benefits, another advantage of combination therapy is that because low doses of the component drugs can be used, fewer adverse events are observed. Indeed, certain drug combinations may offset the tolerability issues observed with monotherapy. For example, diuretic‐induced potassium depletion is attenuated by concomitant administration of an ARB 69 , 70 or an ACE inhibitor. 71
Based on clinical trial data, the following combinations are considered effective in lowering BP to target levels and potentially in protecting against end‐organ damage in African‐American patients with hypertension: ACE inhibitor/diuretic, 72 ARB/diuretic, 51 , 69 , 70 , 73 β blocker/diuretic, 74 and ACE inhibitor/CCB combinations. 64 , 75 , 76 , 77
Fixed‐dose formulations of each of these combinations are approved for use in patients with hypertension and should provide greater convenience to patients. Combination therapy also offers a direct economic benefit to the patient through reduced payment shares toward the cost of the prescription. 78
IMPLICATIONS FOR EFFECTIVE MANAGEMENT OF HYPERTENSIVE AFRICAN‐AMERICAN PATIENTS
The prevention and control of hypertension in African Americans is crucial, because this population has a higher prevalence of hypertension than other groups, and the risk of coronary heart disease, stroke, renal disease, and BP‐related mortality all rise with increased BP. There is a great deal of evidence to support the use of thiazide diuretics, β blockers, ACE inhibitors, and ARBs in treating African‐American hypertensive patients. Combination therapy with agents that have differing but complementary modes of action (such as a diuretic plus an ACE inhibitor or ARB) provides additive antihypertensive efficacy and is well tolerated. Recent hypertension guidelines recommend combination therapy as the standard of care for most African Americans with hypertension.
Concerted efforts by primary care physicians to address modifiable risk factors for hypertension and prescribe the most appropriate pharmacotherapy to meet target BP goals in African Americans will ensure that racial disparities in hypertension‐related morbidity and mortality decrease.
Disclosure:
Editorial assistance for the development of this manuscript was provided by Elaine Griffin, PhD, Envision Pharma, with the financial support of the Bristol‐Myers SquibblSanofi‐Synthelabo Partnership. Dr. Ferdinand has received grants from AstraZeneca Pharmaceuticals, Pfizer Inc., and Merck $$ Co. Dr. Saunders provides speaking and consulting services for Abbott Laboratories, Bristol‐Myers Squibb Co., Novartis, Pfizer Inc., Sanofi‐Aventis, and Wyeth/Monarch.
References
- 1. American Heart Association . Heart Disease and Stroke Statistics?. 2005 Update.Dallas, TX: American Heart Association; 2005. [Google Scholar]
- 2. Cooper R, Rotimi C. Hypertension in blacks. Am J Hypertens. 1997;10: 804–812. [DOI] [PubMed] [Google Scholar]
- 3. Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new Joint National Committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164: 2126–2134. [DOI] [PubMed] [Google Scholar]
- 4. Winkleby MA, Robinson TN, Sundquist J, et al. Ethnic variation in cardiovascular disease risk factors among children and young adults: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA. 1999;281: 1006–1013. [DOI] [PubMed] [Google Scholar]
- 5. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42: 1206–1252. [DOI] [PubMed] [Google Scholar]
- 6. Levine RS, Foster JE, Fullilove RE, et al. Black‐white inequalities in mortality and life expectancy, 1933–1999: implications for healthy people 2010. Public Health Rep. 2001;116: 474–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157: 2413–2446. [DOI] [PubMed] [Google Scholar]
- 8. Onwuanyi AE, Clarke A, Vanderbush E. Cardiovascular disease mortality. J Natl Med Assoc. 2003;95: 1146–1151. [PMC free article] [PubMed] [Google Scholar]
- 9. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States,. 1988–2000. JAMA. 2003;290: 199–206. [DOI] [PubMed] [Google Scholar]
- 10. Henderson SO, Bretsky P, DeQuattro V, et al. Treatment of hypertension in African Americans and Latinos: the effect of JNC VI on urban prescribing practices. J Clin Hypertens (Greenwich). 2003;5: 107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stamler J, Stamler R, Neaton JD, et al. Low risk‐factor profile and long‐term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle‐aged men and women. JAMA. 1999;282: 2012–2018. [DOI] [PubMed] [Google Scholar]
- 12. Whelton PK, He J, Appel LJ, et al. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. JAMA. 2002;288: 1882–1888. [DOI] [PubMed] [Google Scholar]
- 13. Douglas JG, Bakris GL, Epstein M, et al. Management of high blood pressure in African Americans: consensus statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med. 2003;163: 525–541. [DOI] [PubMed] [Google Scholar]
- 14. Law CM, Shiell AW. Is blood pressure inversely related to birth weight? The strength of evidence from a systematic review of the literature. J Hypertens. 1996;14: 935–941. [PubMed] [Google Scholar]
- 15. Richardson AD, Piepho RW. Effect of race on hypertension and antihypertensive therapy. Int J Clin Pharmacol Ther. 2000;38: 75–79. [DOI] [PubMed] [Google Scholar]
- 16. Ferdinand KC. Coronary heart disease and lipid‐modifying treatment in African American patients. Am Heart J. 2004;147: 774–782. [DOI] [PubMed] [Google Scholar]
- 17. Stamler R. Implications of the INTERSALT study. Hypertension. 1991;17(suppl 1):I16–I20. [DOI] [PubMed] [Google Scholar]
- 18. Lewington S, Clarke R, Qizilbash N, et al., For the Prospective Studies Collaboration. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360: 1903–1913. [DOI] [PubMed] [Google Scholar]
- 19. Guidelines Subcommittee. 1999 World Health Organization‐International Society of Hypertension Guidelines for the Management of Hypertension. J Hypertens. 1999;17: 151–183. [PubMed] [Google Scholar]
- 20. Hypertension Detection and Follow‐up Program Cooperative Group. Five‐year findings of the hypertension detection and follow‐up program. II. Mortality by race‐sex and age. JAMA. 1979;242: 2572–2577. [DOI] [PubMed] [Google Scholar]
- 21. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group . Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs. diuretic. The Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288: 2981–2997. [DOI] [PubMed] [Google Scholar]
- 22. Wright JT Jr, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288: 2421–2431. [DOI] [PubMed] [Google Scholar]
- 23. Sica DA. The African American Study of Kidney Disease and Hypertension (AASK) trial: what more have we learned? J Clin Hypertens (Greenwich). 2003;5: 159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rahman M. Initial findings of the AASK: African Americans with hypertensive kidney disease benefit from an ACE inhibitor. Cleve Clin J Med. 2003;70: 304–312. [DOI] [PubMed] [Google Scholar]
- 25. Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4: 393–404. [DOI] [PubMed] [Google Scholar]
- 26. Pepine CJ, Handberg EM, Cooper‐DeHoff RM, et al. A calcium antagonist vs a non‐calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil‐Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290: 2805–2816. [DOI] [PubMed] [Google Scholar]
- 27. Cooper‐DeHoff R, Gaxiola E, Cangiano JL, et al. Blood pressure reduction and CV outcomes in hypertensive Hispanics, Blacks, and Caucasians with coronary artery disease: the International Verapamil/trandolapril Study. Circulation. 2003;108(suppl IV):450. Abstract 2070. [Google Scholar]
- 28. Grundy SM, Balady GJ, Criqui MH, et al. Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the AHA Task Force on Risk Reduction. American Heart Association. Circulation. 1998;97: 1876–1887. [DOI] [PubMed] [Google Scholar]
- 29. D'Agostino RB Sr, Grundy S, Sullivan LM, et al. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286: 180–187. [DOI] [PubMed] [Google Scholar]
- 30. Ashaye MO, Giles WH. Hypertension in Blacks: a literature review. Ethn Dis. 2003;13: 456–462. [PubMed] [Google Scholar]
- 31. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336: 1117–1124. [DOI] [PubMed] [Google Scholar]
- 32. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344: 3–10. [DOI] [PubMed] [Google Scholar]
- 33. Kotchen TA, McCarron DA. Dietary electrolytes and blood pressure: a statement for healthcare professionals from the American Heart Association Nutrition Committee. Circulation. 1998;98: 613–617. [DOI] [PubMed] [Google Scholar]
- 34. Whelton PK, He J, Cutler JA, et al. Effects of oral potassium on blood pressure. Meta‐analysis of randomized controlled clinical trials. JAMA. 1997;277: 1624–1632. [DOI] [PubMed] [Google Scholar]
- 35. Stevens VJ, Obarzanek E, Cook NR, et al. Long‐term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134: 1–11. [DOI] [PubMed] [Google Scholar]
- 36. Saunders E, Weir MR, Kong BW, et al. A comparison of the efficacy and safety of a beta‐blocker, a calcium channel blocker, and a converting enzyme inhibitor in hypertensive blacks. Arch Intern Med. 1990;150: 1707–1713. [PubMed] [Google Scholar]
- 37. Cushman WC, Reda DJ, Perry HM, et al. Regional and racial differences in response to antihypertensive medication use in a randomized controlled trial of men with hypertension in the United States. Arch Intern Med. 2000;160: 825–831. [DOI] [PubMed] [Google Scholar]
- 38. Materson BJ, Reda DJ, Cushman WC, et al. Single‐drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. N Engl J Med. 1993;328: 914–921. [DOI] [PubMed] [Google Scholar]
- 39. Hansson L, Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension‐2 study. Lancet. 1999;354: 1751–1756. [DOI] [PubMed] [Google Scholar]
- 40. Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin‐converting‐enzyme inhibitor, ramipril, on cardiovascular events in high‐risk patients. N Engl J Med. 2000;342: 145–153. [DOI] [PubMed] [Google Scholar]
- 41. Parving HH, Hommel E, Jensen BR, et al. Long‐term beneficial effect of ACE inhibition on diabetic nephropathy in normotensive type 1 diabetic patients. Kidney Int. 2001;60: 228–234. [DOI] [PubMed] [Google Scholar]
- 42. Køber L, Torp‐Pedersen C, Carlsen JE, et al. A clinical trial of the angiotensin‐converting‐enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 1995;333: 1670–1676. [DOI] [PubMed] [Google Scholar]
- 43. Tatti P, Pahor M, Byington RP, et al. Outcome results of the Fosinopril Versus Amlodipine Cardiovascular Events Randomized Trial (FACET) in patients with hypertension and NIDDM. Diabetes Care. 1998;21: 597–603. [DOI] [PubMed] [Google Scholar]
- 44. Estacio RO, Jeffers BW, Hiatt WR, et al. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non‐insulin‐dependent diabetes and hypertension. N Engl J Med. 1998;338: 645–652. [DOI] [PubMed] [Google Scholar]
- 45. Cleland JG, Erhardt L, Murray G, et al., On behalf of the AIRE Study Investigators. Effect of ramipril on morbidity and mode of death among survivors of acute myocardial infarction with clinical evidence of heart failure. A report from the AIRE Study Investigators. Eur Heart J. 1997;18: 41–51. [PubMed] [Google Scholar]
- 46. Lewis EJ, Hunsicker LG, Bain RP, et al., For the Collaborative Study Group. The effect of angiotensin‐converting‐enzyme inhibition on diabetic nephropathy. N Engl J Med. 1993;329: 1456–1462. [DOI] [PubMed] [Google Scholar]
- 47. The SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med. 1992;327: 685–691. [DOI] [PubMed] [Google Scholar]
- 48. Elliott WJ. Higher incidence of discontinuation of angiotensin converting enzyme inhibitors due to cough in black subjects. Clin Pharmacol Ther. 1996;60: 582–588. [DOI] [PubMed] [Google Scholar]
- 49. Pylypchuk GB. ACE inhibitor‐versus angiotensin II blocker‐induced cough and angioedema. Ann Pharmacother. 1998;32: 1060–1066. [DOI] [PubMed] [Google Scholar]
- 50. Weir MR, Smith DH, Neutel JM, et al. Valsartan alone or with a diuretic or ACE inhibitor as treatment for African American hypertensives: relation to salt intake. Am J Hypertens. 2001;14: 665–671. [DOI] [PubMed] [Google Scholar]
- 51. McGill JB, Reilly PA. Combination treatment with telmisartan and hydrochlorothiazide in black patients with mild to moderate hypertension. Clin Cardiol. 2001;24: 66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin‐receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345: 851–860. [DOI] [PubMed] [Google Scholar]
- 53. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345: 861–869. [DOI] [PubMed] [Google Scholar]
- 54. Parving HH, Lehnert H, Brochner‐Mortensen J, et al. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345: 870–878. [DOI] [PubMed] [Google Scholar]
- 55. Dahlöf B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359: 995–1003. [DOI] [PubMed] [Google Scholar]
- 56. Lindholm LH, Ibsen H, Dahlöf B, et al. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359: 1004–1010. [DOI] [PubMed] [Google Scholar]
- 57. Julius S, Alderman MH, Beevers G, et al. Cardiovascular risk reduction in hypertensive black patients with left ventricular hypertrophy: the LIFE study. J Am Coll Cardiol. 2004;43: 1047–1055. [DOI] [PubMed] [Google Scholar]
- 58. Cohn J., Tognoni G, for the Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin‐receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345: 1667–1675. [DOI] [PubMed] [Google Scholar]
- 59. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non‐ST‐segment elevation myocardial infarction: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on the management of patients with unstable angina). Circulation. 2000;102: 1193–1209. [DOI] [PubMed] [Google Scholar]
- 60. Gibbons RJ, Abrams J, Chatterjee K, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina—summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina). Circulation. 2003;107: 149–158. [DOI] [PubMed] [Google Scholar]
- 61. Gottlieb SS, McCarter RJ, Vogel RA. Effect of beta‐blockade on mortality among high‐risk and low‐risk patients after myocardial infarction. N Engl J Med. 1998;339: 489–497. [DOI] [PubMed] [Google Scholar]
- 62. Prisant LM, Mensah GA. Use of beta‐adrenergic receptor blockers in blacks. J Clin Pharmacol. 1996;36: 867–873. [DOI] [PubMed] [Google Scholar]
- 63. Mogensen CE, Neldam S, Tikkanen I, et al. Randomised controlled trial of dual blockade of renin‐angiotensin system in patients with hypertension, microalbuminuria, and non‐insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. BMJ. 2000;321: 1440–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lüscher TF, Waeber B. Efficacy and safety of various combination therapies based on a calcium antagonist in essential hypertension: results of a placebo‐controlled randomized trial. J Cardiovasc Pharmacol. 1993;21: 305–309. [DOI] [PubMed] [Google Scholar]
- 65. Fogari R, Corea L, Cardoni O, et al. Combined therapy with benazepril and amlodipine in the treatment of hypertension inadequately controlled by an ACE inhibitor alone. J Cardiovasc Pharmacol. 1997;30: 497–503. [DOI] [PubMed] [Google Scholar]
- 66. Materson BJ, Reda DJ, Williams., For the Department of Veterans Affairs Cooperative Study Group on antihypertensive agents. Lessons from combination therapy in Veterans Affairs Studies. Am J Hypertens. 1996;9: 187S–191S. [DOI] [PubMed] [Google Scholar]
- 67. Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood‐pressure lowering and low‐dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351: 1755–1762. [DOI] [PubMed] [Google Scholar]
- 68. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265: 3255–3264. [PubMed] [Google Scholar]
- 69. Kochar M, Guthrie R, Triscari J, et al. Matrix study of irbesartan with hydrochlorothiazide in mild‐to‐moderate hypertension. Am J Hypertens. 1999;12: 797–805. [DOI] [PubMed] [Google Scholar]
- 70. McGill JB, Reilly PA. Telmisartan plus hydrochlorothiazide versus telmisartan or hydrochlorothiazide monotherapy in patients with mild to moderate hypertension: a multicenter, randomized, double‐blind, placebo‐controlled, parallelgroup trial. Clin Ther. 2001;23: 833–850. [DOI] [PubMed] [Google Scholar]
- 71. Weinberger MH. Angiotensin converting enzyme inhibitors enhance the antihypertensive efficacy of diuretics and blunt or prevent adverse metabolic effects. J Cardiovasc Pharmacol. 1989;13(suppl 3):S1–S4. [DOI] [PubMed] [Google Scholar]
- 72. Pool JL, Cushman WC, Saini RK, et al. Use of the factorial design and quadratic response surface models to evaluate the fosinopril and hydrochlorothiazide combination therapy in hypertension. Am J Hypertens. 1997;10: 117–123. [DOI] [PubMed] [Google Scholar]
- 73. Soffer BA, Wright JT Jr, Pratt JH, et al. Effects of losartan on a background of hydrochlorothiazide in patients with hypertension. Hypertension. 1995;26: 112–117. [DOI] [PubMed] [Google Scholar]
- 74. Frishman WH, Bryzinski BS, Coulson LR, et al. A multifactorial trial design to assess combination therapy in hypertension. Treatment with bisoprolol and hydrochlorothiazide. Arch Intern Med. 1994;154: 1461–1468. [PubMed] [Google Scholar]
- 75. Roca‐Cusachs A, Torres F, Horas M, et al. Nitrendipine and enalapril combination therapy in mild to moderate hypertension: assessment of dose‐response relationship by a clinical trial of factorial design. J Cardiovasc Pharmacol. 2001;38: 840–849. [DOI] [PubMed] [Google Scholar]
- 76. Frishman WH, Ram CV, McMahon FG, et al. Comparison of amlodipine and benazepril monotherapy to amlodipine plus benazepril in patients with systemic hypertension: a randomized, double‐blind, placebo‐controlled, parallelgroup study. J Clin Pharmacol. 1995;35: 1060–1066. [DOI] [PubMed] [Google Scholar]
- 77. Messerli FH, Oparil S, Feng Z. Comparison of efficacy and side effects of combination therapy of angiotensin‐converting enzyme inhibitor (benazepril) with calcium antagonist. (either nifedipine or amlodipine) versus high‐dose calcium antagonist monotherapy for systemic hypertension. Am J Cardiol. 2000;86: 1182–1187. [DOI] [PubMed] [Google Scholar]
- 78. Hilleman D. Cost effectiveness of combination therapy. Am J Manag Care. 1999;5: S449–S453. [PubMed] [Google Scholar]


