Abstract
Blood pressure normally declines 10%–20% from daytime to sleep. Patients with less than a 10% reduction in daytime blood pressure are referred to as nondippers. A blunted nocturnal decline in blood pressure may be due to diminished sodium excretory capacity, alteration in the autonomic nervous system, or other factors. Secondary hypertension should be considered as a possibility. Target organ damage appears to be more common in nondippers, however, poor reproducibility of nondipping status raises the question as to the appropriate duration of monitoring to establish a diagnosis. Nondippers tend to have a greater reduction in nocturnal blood pressure with nonpharmacologic and pharmacologic treatment.
Ambulatory blood pressure (BP) has changed many concepts about BP. BP is not a static measurement. 1 The diurnal variation in BP is a prominent feature of a normal 24‐hour ambulatory BP tracing. With sleep, BP normally declines 10%–20%. 2 In the Allied Irish Bank Study 3 (n=815), the average nocturnal decline in BP was 18/17 mm Hg. Supine position and sleep explains 65%–75% of the nocturnal decline in BP. 4 Prior to awakening and standing, the sympathetic nervous system is activated and BP rises.
MECHANISMS
Nondippers refer to patients whose BP does not decline during sleep (Figure 1). The mechanism may be due to a redistribution of retained volume during sleep due to reduced sodium renal excretory capacity or an alteration in the autonomic nervous system. 2 , 5 , 6 Impaired nocturnal melatonin secretion has also been reported. 7
Figure 1.
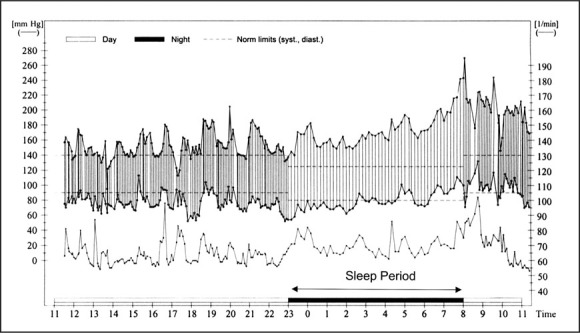
Ambulatory blood pressure testing. Compare the blood pressure during the daytime and nighttime. What is abnormal?
DEFINITIONS
Nondippers who have no decline in systolic or diastolic BP or an increase in BP are called inverted or reverse dippers (Figure 2). 8 , 9 In a rural Japanese population of 1542 residents, ≥40 years of age, the prevalence of nondippers and inverted dippers using the definitions shown in Figure 2 was 16% (Figure 3), however, different definitions of nondipper status will result in different prevalences. 10 Furthermore, arbitrary sleep times, rather than true sleep periods, influence the designation of dipper vs. nondipper. 11 Secondary hypertension may be suggested by a blunted nocturnal decline in BP. Common causes of nondipping are displayed in the Table. Autonomic dysfunction is associated with increased BP at night and daytime hypotension.
Figure 2.
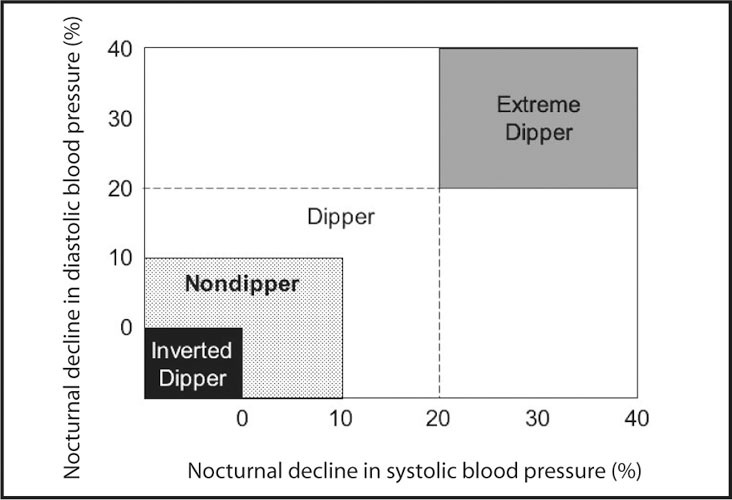
Definitions of dipping patterns. Modified from Am J Hypertens. 1997;10:1201–1207. 8
Figure 3.
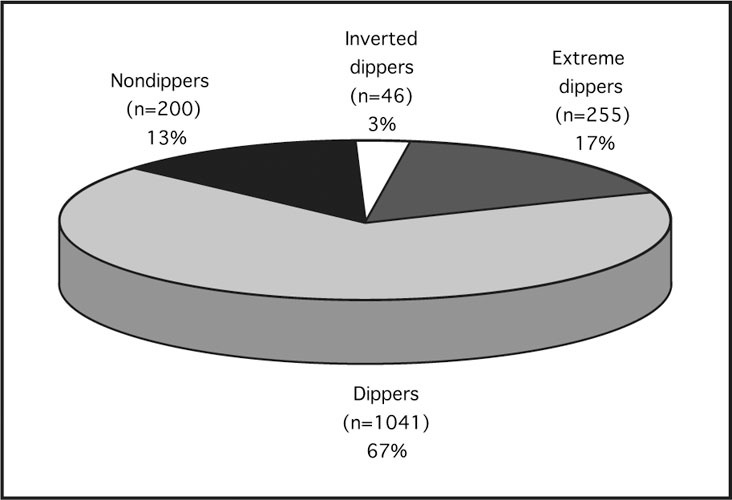
Patterns of blood pressure. Derived from Am J Hypertens. 1997;10:1201–1207. 8
Table.
Causes of Nondipping
| Autonomic dysfunction |
| Cardiac transplantation |
| Cushing's syndrome |
| Diabetes |
| High‐dose corticosteroids |
| Licorice intoxication |
| Obstructive sleep apnea |
| Pheochromocytoma |
| Preeclampsia/toxemia |
| Primary aldosteronism |
| Renal disease |
TARGET ORGAN DAMAGE
The consequence of BP not declining during sleep is a greater 24‐hour BP for a similar level of daytime BP. Cardiovascular morbidity is increased, 12 which is associated with more silent lacunar infarctions, myocardial ischemia, left ventricular hypertrophy, and microalbuminuria. 13 , 14 Using magnetic resonance imaging in a population of 575 older Japanese subjects, the rate of multiple silent cerebral infarcts was 41% in nondippers (n=185) and 49% in reverse dippers (n=63), compared to 29% in dippers (n=230). Also, stroke incidence was more common in reverse dippers than dippers (22% vs. 6.1%). 9 Among the reverse dippers, intracranial hemorrhage was a more common type of stroke than the other groups (29% vs. 7.7% of strokes, p=0.04).
REPRODUCIBILITY
Reproducibility of the nocturnal decline in BP is poor. 15 , 16 , 17 , 18 Based on two 24‐hour ambulatory BP measurements 1 week apart, a week‐to‐week concordance for the categorization of nondipper status was only 14.5% of 69 patients for systolic BP (Week 1=37% and Week 2=32%) and 12% for diastolic BP (Week 1=25% and Week 2=19%). 19 Body and arm position can both significantly influence the nocturnal ambulatory BP. 20 Also, increased movement during sleep, as assessed by wrist actigraphy, is associated with nondipper status. 21 Sleep disturbance during ambulatory BP monitoring potentially contributes to a diminished nocturnal BP. 22 , 23 With an inflation interval of 10 minutes, the duration of stage 4 (deep) sleep shortens and is associated with an increase in nocturnal waking time without an effect on the frequency of awakenings. 22 If a nondipping pattern is confirmed in two 24‐hour periods, more cardiovascular abnormalities are present. 24
TREATMENT
Like sodium restriction, diuretics can restore a nocturnal BP decline in nondippers. 25 BP decreased to a greater extent in nondippers compared to dippers using a chronotherapeutic verapamil as an antihypertensive given at night 26 ; however, the incidence of cardiovascular events was not reduced during the early morning hours in these patients. Similar results were observed using arotinolol, an α‐β adrenergic blocker. 27
CONCLUSION
A blunted nocturnal decline in BP in some patients appears to increase vascular risk when data on groups are considered, however, for individual patients, interpretation is confounded by poor reproducibility.
References
- 1. Prisant LM. Ambulatory blood pressure monitoring in the diagnosis of hypertension. Cardiol Clin. 1995;13:479–490. [PubMed] [Google Scholar]
- 2. Izzo JL, Pickering TG. Diurnal and Other Cyclic Variations of Blood Pressure. In: Izzo JL, Black HR, eds. Hypertension Primer. Dallas , TX : Lippincott Williams & Wilkins;2003:334–336. [Google Scholar]
- 3. O'Brien E, Murphy J, Tyndall A, et al. Twenty‐four‐hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991;9:355–360. [DOI] [PubMed] [Google Scholar]
- 4. Degaute JP, van de Borne P, Linkowski P, et al. Quantitative analysis of the 24‐hour blood pressure and heart rate patterns in young men. Hypertension. 1991;18:199–210. [DOI] [PubMed] [Google Scholar]
- 5. Uzu T, Fujii T, Nishimura M, et al. Determinants of circadian blood pressure rhythm in essential hypertension. Am J Hypertens. 1999;12:35–39. [DOI] [PubMed] [Google Scholar]
- 6. Carvalho MJ, van Den Meiracker AH, Boomsma F, et al. Diurnal blood pressure variation in progressive autonomic failure. Hypertension. 2000;35:892–897. [DOI] [PubMed] [Google Scholar]
- 7. Jonas M, Garfinkel D, Zisapel N, et al. Impaired nocturnal melatonin secretion in non‐dipper hypertensive patients. Blood Press. 2003;12:19–24. [PubMed] [Google Scholar]
- 8. Ohkubo T, Imai Y, Tsuji I, et al. Relation between nocturnal decline in blood pressure and mortality. The Ohasama Study. Am J Hypertens. 1997;10:1201–1207. [DOI] [PubMed] [Google Scholar]
- 9. Kario K, Pickering TG, Matsuo T, et al. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–857. [DOI] [PubMed] [Google Scholar]
- 10. Butkevich A, Phillips RA, Sheinart KF, et al. The effects of various definitions of dipping and daytime and night‐time on the characterization of 24 h profiles of blood pressure. Blood Press Monit. 2000;5:19–22. [DOI] [PubMed] [Google Scholar]
- 11. Rosansky SJ, Menachery SJ, Whittman D, et al. The relationship between sleep deprivation and the nocturnal decline of blood pressure. Am J Hypertens. 1996;9:1136–1138. [DOI] [PubMed] [Google Scholar]
- 12. Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801. [DOI] [PubMed] [Google Scholar]
- 13. Berrut G, Bouhanick B, Fabbri P, et al. Loss of the nocturnal decline in blood pressure in subjects with essential hypertension and microalbuminuria. Blood Press Monit. 1996;1:469–473. [PubMed] [Google Scholar]
- 14. O'Brien E, Atkins N, Staessen J. Are overnight dip and target‐organ damage related? A clinical perspective. Blood Press Monit. 1996;1(suppl 1):S41–S46. [Google Scholar]
- 15. van der Steen MS, Lenders JW, Graafsma SJ, et al. Reproducibility of ambulatory blood pressure monitoring in daily practice. J Hum Hypertens. 1999;13:303–308. [DOI] [PubMed] [Google Scholar]
- 16. Prisant LM. Ambulatory blood pressure monitoring: test reproducibility and its implications. Blood Press Monit. 1998;3:221–225. [PubMed] [Google Scholar]
- 17. Omboni S, Parati G, Palatini P, et al. Reproducibility and clinical value of nocturnal hypotension: prospective evidence from the SAMPLE study. Study on Ambulatory Monitoring of Pressure and Lisinopril Evaluation. J Hypertens. 1998;16:733–738. [DOI] [PubMed] [Google Scholar]
- 18. Mochizuki Y, Okutani M, Donfeng Y, et al. Limited reproducibility of circadian variation in blood pressure dippers and nondippers. Am J Hypertens. 1998;11:403–409. [DOI] [PubMed] [Google Scholar]
- 19. Prisant LM, Thompson WO, Bottini PB et al. Racial aspects of ambulatory blood pressure. J Hum Hypertens. 1991;5:369–373. . [PubMed] [Google Scholar]
- 20. van der Steen MS, Pleijers AM, Lenders JW, et al. Influence of different supine body positions on blood pressure: consequences for night blood pressure/dipper‐status. J Hypertens. 2000;18:1731–1736. [DOI] [PubMed] [Google Scholar]
- 21. Mansoor GA, White WB, McCabe EJ, et al. The relationship of electronically monitored physical activity to blood pressure, heart rate, and the circadian blood pressure profile. Am J Hypertens. 2000;13:262–267. [DOI] [PubMed] [Google Scholar]
- 22. Degaute JP, van de Borne P, Kerkhofs M, et al. Does non‐invasive ambulatory blood pressure monitoring disturb sleep? J Hypertens. 1992;10:879–885. [PubMed] [Google Scholar]
- 23. Schwan A, Eriksson G. Effect on sleep—but not on blood pressure—of nocturnal non‐invasive blood pressure monitoring. J Hypertens. 1992;10:189–194. [DOI] [PubMed] [Google Scholar]
- 24. Cuspidi C, Meani S, Salerno M, et al. Cardiovascular target organ damage in essential hypertensives with or without reproducible nocturnal fall in blood pressure. J Hypertens. 2004;22:273–280. [DOI] [PubMed] [Google Scholar]
- 25. Uzu T, Kimura G. Diuretics shift circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1999;100:1635–1638. [DOI] [PubMed] [Google Scholar]
- 26. White WB, Mehrotra DV, Black HR, et al. Effects of controlled‐onset extended‐release verapamil on nocturnal blood pressure (dippers vs. nondippers). COER‐Verapamil Study Group. Am J Cardiol. 1997;80:469–474. [DOI] [PubMed] [Google Scholar]
- 27. Wu H, Zhang Y, Huang J, et al. Clinical trial of arotinolol in the treatment of hypertension: dippers vs. non‐dippers. Hypertens Res. 2001;24:605–610. [DOI] [PubMed] [Google Scholar]


