Abstract
African Americans have twice the risk of suffering a stroke compared to whites, but the reasons for this disparity have yet to be elucidated. Recent data suggest that the morning blood pressure (BP) surge is an independent predictor of strokes. Whether African Americans and whites differ with respect to morning BP surge is unknown. African‐American (n=183) and white (n=139) participants, age 18‐65, were studied with 24‐hour ambulatory BP monitoring. Morning surge was defined as morning BP minus the trough BP during sleep. The morning surge was significantly lower in African Americans than in whites (23 mm Hg vs. 27 mm Hg; both SEM=1.0; p=0.009). This relationship was no longer evident after adjusting for gender, age, and body mass index (23 mm Hg vs. 26 mm Hg; SE=1.0 and 1.1; p=nonsignificant). Morning BP surge is unlikely to account for differences in stroke incidence between African Americans and whites.
In the United States, African Americans are at significantly greater risk for suffering a stroke compared to whites. 1 , 2 , 3 African Americans suffer increased stroke mortality relative with whites 4 and have higher stroke incidence rates, particularly in the young and middle‐aged. 5 The increased risk for stroke among African Americans persists within communities of similar socioeconomic status that are ethnically diverse. For example, Sacco and colleagues 1 reported that within a single, ethnically diverse community composed of members with comparable socioeconomic status, African Americans had a 2.4‐fold greater stroke incidence compared with whites over a 3‐year follow‐up period. The excess burden of stroke incidence among African Americans constitutes a serious public health problem in the United States, 6 making it important to identify potential etiological factors that contribute to this racial disparity.
It is well established that the onset of many cardiovascular and cerebrovascular events exhibits a marked diurnal pattern, with adverse events occurring most frequently in the morning hours. 7 This pattern parallels the diurnal variation of blood pressure (BP), which is typically lower during sleep and then increases substantially upon awakening. This increase is known as the morning BP surge. 8 Until recently, there was only indirect evidence that the morning BP surge was associated with increased cardiovascular morbidity. For example, the magnitude of morning BP surge was found to correlate with left ventricular hypertrophy assessed by echocardiography. 9 More recently, Kario et al. 10 have now demonstrated that the morning BP surge is an independent risk factor for both silent cerebral infarcts (assessed by magnetic resonance imaging) and clinical stroke events over 41 months of follow‐up in elderly hypertensive Japanese patients. The risk associated with the morning surge persisted after controlling for the average 24‐hour BP level.
In view of the potential importance of the morning BP surge for cerebrovascular disease, we determined whether morning BP surge differed between African Americans and whites. A higher morning BP surge among African Americans would suggest a possible mechanism explaining the racial stroke disparity. We analyzed data from a recent crosssectional study of race, socioeconomic status, and diurnal BP patterns.
METHODS
Participants
The sample consists of 322 participants in a crosssectional study of race, socioeconomic status, and diurnal BP patterns. Subjects were recruited at four New York City institutions: Weill Medical College of Cornell University, Mount Sinai School of Medicine, Harlem Hospital, and North General Hospital, using a common protocol. The protocol and consent form were approved by the institutional review committees for research involving human subjects at each institution.
Participants were 18–65 years of age, white or African American, had no previous cardiovascular disease, and had no major medical problems other then hypertension. Subjects could be either normotensive or hypertensive. Normal BP, assessed at the clinic, was defined as ≤135/85 mm Hg based on the average of three readings. In addition, normotensive subjects were excluded if they had a history of hypertension within the past 5 years. Hypertension was defined as an average clinic BP ≥140/90 mm Hg over two visits, with at least one assessment taken while off medication. Hypertensive participants had to be willing and able to be withdrawn from medication for 2 weeks prior to the study. If their BP exceeded 160/105 mm Hg, they were excluded from the study.
BP Measurements
Ambulatory BP monitoring was performed using either a Meditech Cardiotens (Meditech Ltd., Budapest, Hungary) or a SpaceLabs 90207 (OSI Systems, Inc., Hawthorne, CA) monitor. Recording for the majority of subjects (81%) began between 10 a.m. and 1 p.m. The monitor was fitted during a research visit to one of the four study sites and calibrated by comparison of five successive systolic and diastolic readings against simultaneously determined auscultatory readings taken with a mercury column by a trained observer. Agreement of the averages to within 5 mm Hg was considered acceptable. The monitor was programmed to take readings at 20‐minute intervals throughout the 24‐hour monitoring period, and the participant was instructed to proceed through a normal day. Each participant was asked to remain as motionless as possible each time the monitor took a reading during waking hours and then to record his or her location, position, activity, and mood in a preprinted paper‐and‐pencil diary. Average awake and sleep BPs for each participant were analyzed only if at least five readings were recorded for that condition, except that one subject had an average sleep BP based on four readings.
Ambulatory BP Definitions
Sleep BP was defined as the average of BPs from the time when the participant went to bed until the time he or she got out of bed, and awake BP was defined as the average of BPs recorded during the rest of the day. Morning BP was defined as the average of the BP readings (minimum of three required) obtained during the first 2 hours after awakening and maximum morning BP was the highest systolic reading during this same interval. The BP trough during sleep was defined as the minimum value of the three‐reading moving average of BP during sleep. Finally, the morning BP surge was defined as the morning systolic BP (SBP) minus the SBP trough during sleep. 10
The nocturnal BP fall (dipping) was defined as the difference between the average awake and average sleep BP. Participants were classified into one of four dipping status categories according to the percentage of nocturnal SBP reduction [100×(1‐sleep SBP/awake SBP)] as follows: 1) extreme dippers (nocturnal SBP reduction ≥20%); 2) dippers (nocturnal SBP reduction ≥10% but <20%); 3) nondippers (nocturnal SBP reduction ≥0% but <10%); and 4) risers (nocturnal SBP reduction <0%). 11
We note that while the test‐retest reproducibility of dipping is quite poor at the individual level, the finding of racial group differences in average dipping or the distribution of dipping status is quite robust. 12 , 13 , 14
Statistical Analysis
The Pearson chi‐square test of independence was used to test for a racial difference in the distributions of categorical variables. The Student t test was used to compare means of continuous measures. The pooled variances test was used when the p value for the test of equal variances was greater than 0.10; otherwise the unequal variances test was used with the Satterthwaite estimate of degrees of freedom. Analysis of covariance was used to estimate adjusted means and test for racial differences in morning BP surge after statistically controlling for sex, age, and body mass index (BMI).
RESULTS
The characteristics of the study sample are presented in the Table. There were more African‐American participants than white (n=183 and 139, respectively). The African‐American cohort differed significantly from the white cohort in several ways: the African‐American cohort contained significantly more women (p=0.008), was younger (p=0.0008), and had higher average BMI (p=0.0008). The differences between whites and African Americans in the awake SBP and morning SBP were not significant; however African Americans had higher average sleep SBP (p=0.0004) and a higher average sleep SBP trough (p=0.0001). Figure portrays the distribution of dipping status in the two cohorts. Compared to whites, African Americans were more likely to be classified as nondippers (44% for African Americans vs. 32% for whites) and less likely to be classified as normal dippers (47% vs. 55%) or extreme dippers (3% vs. 9%; chi square=9.56; df=3, p=0.02). The racial difference is somewhat stronger when we combined non‐dippers and risers (51% in African Americans vs. 37% in whites) and compared them to normal dippers and extreme dippers (49% vs. 63%; chi square=6.13; df=l, p=0.01).
Figure 1.
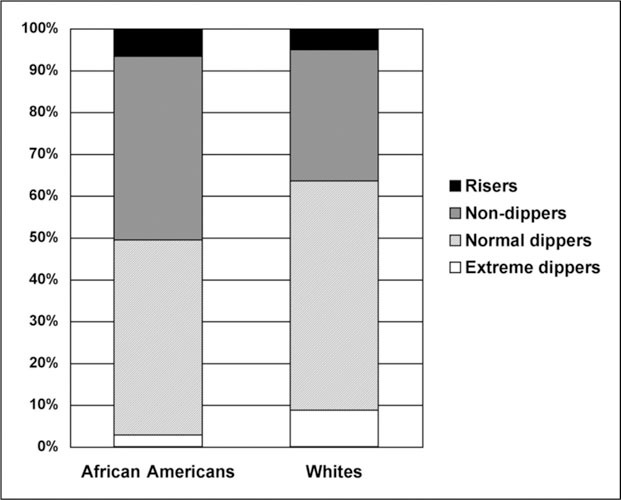
Distribution of blood pressure dipping status in African Americans and whites
The distribution of morning BP surge for the two groups is summarized in Figure. On average, African Americans exhibited a 3.8 mm Hg (SE=1.4) smaller morning BP surge than whites (22.7 mm Hg vs. 26.5 mm Hg; both SE=1.0; t=2.61; p=0.01). Controlling for gender, age, and BMI, the difference in adjusted average morning BP surge between the two groups narrowed to 2.5 mm Hg (SE=1.5) and was no longer statistically significant (23.5 mm Hg for African Americans, 25.9 mm Hg for whites; SE=1.0 and 1.1, respectively; p=0.10). If we use the maximum morning SBP instead of the average to compute the morning BP surge, the unadjusted and adjusted differences between African Americans and whites are not significant (unadjusted mean difference is −1.6 mm Hg; SE=2.0; p=0.42; difference adjusted for sex, age, and BMI is 0.2 mm Hg; SE=2.1; p=0.92). We repeated the analysis separately for men and women and found a significant racial difference in morning BP surge for males (4.8 mm Hg greater for whites; SE=2.2; p=0.03), but not for women (2.3 mm Hg greater for whites; SE=1.9; p=0.23); however, this difference between genders did not approach statistical significance (p=0.41).
Figure 2.
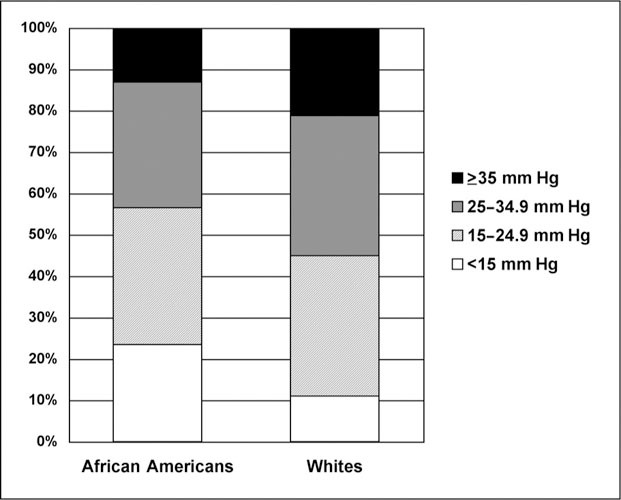
Distribution of morning blood pressure surge in African Americans and whites
Dipping and morning blood surge are highly correlated: the more one's BP declined at night, the more it rose in the morning (r=0.55, p<0.0001). When we additionally controlled for nocturnal dipping status, the difference between African Americans and whites in the adjusted average morning BP surge further diminished to 1.1 mm Hg (24.3 mm Hg and 25.5 mm Hg, respectively; p=0.39).
DISCUSSION
Compared to whites, mortality from all causes is higher for African Americans, and death from hypertension contributes most to the racial disparity in potential life‐years lost. 15 The morning BP surge appears to have important consequences for cardiovascular morbidity. We therefore examined whether a difference exists in morning BP surge between African Americans and whites that might partially explain why African Americans are at greater risk for stroke and other cardiovascular morbidity than whites. Before adjusting for potential confounders, African Americans in our sample had a 3.8 mm Hg lower morning BP surge than whites, a difference that is in the opposite direction to what we anticipated based on the hypothesis that differences in morning BP surge might account for part of the racial difference in stroke risk. After controlling for age, gender, and BMI, the difference in morning BP surge between middle‐aged African Americans and whites was 37% smaller and no longer statistically significant. After further controlling for nocturnal dipping status, the difference became negligible. Given that the unadjusted racial difference is in the wrong direction, and can be largely accounted for by sample differences in sex, age, BMI, and nocturnal dipping, we conclude that morning BP surge is unlikely to account for differences in cardiovascular disease rates between middle‐aged African Americans and whites.
Our sample was middle‐aged, with an average age of 47 years, and included both hypertensive and normotensive participants. Prior studies demonstrating morning BP surge to be associated with cardiovascular morbidity have focused largely on elderly hypertensive patients. 9 , 10 Therefore, it is possible that morning BP surge differences exist between elderly, hypertensive African Americans and whites and such differences may be clinically important. Nonetheless, the disparity in stroke rates between African Americans and whites is greatest among the young and middle‐aged. 5 Specifically, in individuals less than 65 years old, African Americans have two to five times the risk of stroke. For individuals aged 45–54 years, the risk of stroke in African Americans is 2.6 times that for whites. After age 65, stroke risk is still elevated in African Americans, but the difference is comparatively attenuated (1.3–1.8 times the risk relative to whites). These facts highlight the relevance of our findings, because the ages represented in our sample reflect the years when the stroke disparity is greatest between African Americans and whites.
Based on this study, it is much more plausible that racial differences in dipping rather than in morning BP surge contribute to the excess risk for cardiovascular disease in African Americans. We found that whites were more likely to be dippers and less likely to be non‐dippers compared to African Americans. While disparate conclusions have been reached regarding the relationship between race and diurnal BP patterns, a meta‐analysis 12 (18 studies and 2852 participants) found that SBP and diastolic BP were significantly higher during both the day and night in African Americans compared to whites. Moreover, the same meta‐analysis demonstrated that African Americans experienced less of a fall in both SBP and diastolic BP at night compared to whites. Interestingly, the effect of race on nocturnal BP dipping was not found for non‐American blacks, raising the possibility that the racial nocturnal BP differences noted in American samples (such as ours) may reflect psychosocial and socioeconomic influences rather than genetic differences. For example, Shapiro et al. 16 have demonstrated that cynical hostility is a significant predictor of both awake and sleep BP in blacks but not whites.
A lack of nocturnal dipping is associated with an increased risk of cardiovascular mortality. In the Ohasama study, which examined 1542 Japanese participants, there was a significant relationship between non‐dipping BP status (using a definition similar to that used in our study) and cardiovascular mortality at a mean follow‐up of 4.1 years 17 and 9.2 years. 18 Similar findings in other prospective studies 19 suggest that the higher stroke incidence and risk of cardiovascular mortality observed in African Americans may be explained in part by a lack of nocturnal dipping.
Limitations
Our study may have limited generalizability due to the relatively small sample size derived from four hospitals in New York City. In this context, race and socioeconomic status are substantially confounded. Had we found significant racial differences in morning BP surge after controlling for sex, age, and BMI, we would have been concerned about the potential role of socioeconomic status. In the absence of such a difference, however, there is less reason to be concerned about confounding.
Morning BP was determined using the time of awakening, without accounting for morning physical activity levels. We used only “time of awakening” in our definition in an effort to replicate the surge definition used by Kario et al. 10 when they demonstrated that morning BP surge is an independent risk factor for both silent cerebral infarcts and clinical stroke events. Leary et al. 20 have demonstrated that the magnitude of the morning surge is associated with the level of physical activity upon waking; additionally, they demonstrated the morning surge in BP in response to physical activity was increased in patients with higher BP readings at clinic visits. Although we did not measure physical activity, morning BP surge was defined using all BP readings for the first 2 hours of wakefulness—that is, our BP surge does not merely reflect increases in BP resulting from wakefulness alone. In addition, there was no statistical difference in awake SBP between the two racial groups. Thus, it is unlikely that measurement of physical activity would have affected our observation that little or no difference exists in surge levels between African Americans and whites. We cannot, however, exclude the possibility that measuring physical activity levels would have affected our observations.
CONCLUSION
This is the first report to our knowledge to examine morning BP surge differences between African Americans and whites. Our finding of little or no difference, after adjustment for confounders, does not support morning BP surge as a potential mediator of the differential stroke rates between middle‐aged African Americans and whites.
Acknowledgements: The authors gratefully acknowledge the support of the National Heart, Lung, and Blood Institute (HL‐47540).
References
- 1. Sacco RL, Boden‐Albala B, Gan R, et al. HauserWA. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998; 147: 259–268. [DOI] [PubMed] [Google Scholar]
- 2. Broderick J, Brott T, Kothari R, et al. The Greater Cincinnati/Northern Kentucky stroke study: preliminary first‐ever and total incidence rates of stroke among blacks. Stroke. 1998; 29: 415–421. [DOI] [PubMed] [Google Scholar]
- 3. Bruno A, Carter S, Qualls C, et al. Incidence of spontaneous intracerebral hemorrhage among Hispanics and non‐Hispanic whites in New Mexico. Neurology. 1996; 47: 405–408. [DOI] [PubMed] [Google Scholar]
- 4. Otten MW Jr, Teutsch SM, Williamson DF, et al. The effect of known risk factors on the excess mortality of black adults in the United States. JAMA. 1990; 263: 845–850. [PubMed] [Google Scholar]
- 5. Kissela B, Schneider A, Kleindorfer D, et al. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke. 2004; 35: 426–431. [DOI] [PubMed] [Google Scholar]
- 6. Sacco RL. Preventing stroke among blacks: the challenges continue. JAMA. 2003; 289: 3005–3007. [DOI] [PubMed] [Google Scholar]
- 7. Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989; 79: 733–743. [DOI] [PubMed] [Google Scholar]
- 8. White WB. Cardiovascular risk and therapeutic intervention for the early morning surge in blood pressure and heart rate. Blood Press Monit. 2001; 6: 63–72. [DOI] [PubMed] [Google Scholar]
- 9. Kuwajima I, Mitani K, Miyao M, et al. Cardiac implications of the morning blood pressure surge in elderly hypertensive patients: relation to arising time. Am J Hypertens. 1995; 8: 29–33. [DOI] [PubMed] [Google Scholar]
- 10. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003; 107: 1401–1406. [DOI] [PubMed] [Google Scholar]
- 11. Kario K, Pickering TG, Matsuo T, et al. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001; 38: 852–857. [DOI] [PubMed] [Google Scholar]
- 12. Profant J, Dimsdale JE. Race and diurnal blood pressure patterns. A review and meta‐analysis. Hypertension. 1999; 33: 1099–1104. [DOI] [PubMed] [Google Scholar]
- 13. Hebert LA, Agarwal G, Ladson‐Wofford SE, et al. Nocturnal blood pressure in treated hypertensive African Americans compared to treated hypertensive European Americans. J Am Soc Nephrol. 1996; 7: 2130–2134. [DOI] [PubMed] [Google Scholar]
- 14. Omboni S, Parati G, Palatini P, et al. Reproducibility and clinical value of nocturnal hypertension: prospective evidence from the SAMPLE study. J Hypertens. 1998; 16: 733–738. [DOI] [PubMed] [Google Scholar]
- 15. Wong MD, Shapiro MF, Boscardin WJ, et al. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002; 347: 1585–1592. [DOI] [PubMed] [Google Scholar]
- 16. Shapiro D, Goldstein IB, Jamner LD. Effects of cynical hostility, anger out, anxiety, and defensiveness on ambulatory blood pressure in black and white college students. Psychosom Med. 1996; 58: 354–364. [DOI] [PubMed] [Google Scholar]
- 17. Ohkubo T, Imai Y, Tsuji I, et al. Relation between nocturnal decline in blood pressure and mortality. The Ohasama Study. Am J Hypertens. 1997; 10: 1201–1207. [DOI] [PubMed] [Google Scholar]
- 18. Ohkubo T, Hozawa A, Yamaguchi J, et al. Prognostic significance of the nocturnal decline in blood pressure in subjects with and without high 24‐hour blood pressure: The Ohasama study. J Hypertens. 2002; 20: 2183–2189. [DOI] [PubMed] [Google Scholar]
- 19. Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994; 24: 793–801. [DOI] [PubMed] [Google Scholar]
- 20. Leary AC, Struthers AD, Donnan PT, et al. The morning surge in blood pressure and heart rate is dependent on levels of physical activity after waking. J Hypertens. 2002; 20: 865–870. [DOI] [PubMed] [Google Scholar]


