Abstract
Malignant hypertension may present with retinopathy, choroidopathy, and optic neuropathy. Flame‐shaped retinal hemorrhages, an early finding, are due to smooth muscle necrosis and bleeding along the nerve fiber layer. Cotton‐wool spots, or cytoid bodies, are not exudates, but rather are retinal infarcts. Hypertensive optic neuropathy is a late finding. Optical coherence tomography is a relatively new imaging technique for evaluating retinal thickness and the location of pathology in patients with malignant hypertension.
A 35‐year old African‐American man presented with blurry vision in both eyes and headaches of 2 weeks' duration. He was not on medication and denied any health problems. His blood pressure (BP) was 236/146 mm Hg. What do Figures 1 and 2 reveal?
Figure 1.
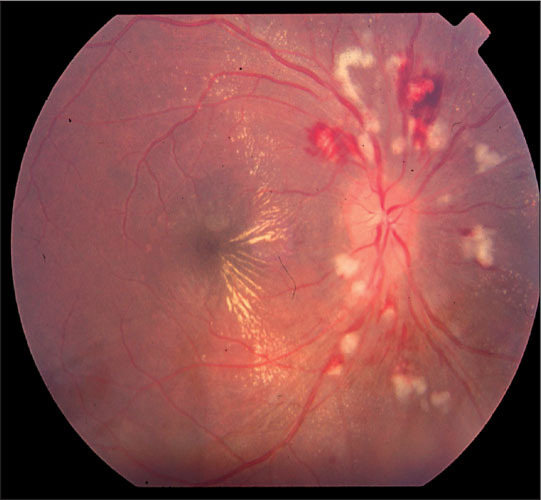
Retina, right eye. Blurring of the optic disc margin and extensive cotton‐wool spots, or nerve fiber layer infarcts, are seen surrounding the optic nerve. Flame‐shaped hemorrhages, diffuse exudates, and a hemimacular star are also present. An exudative retinal detachment was seen on clinical examination extending through the fovea. (Note: This cannot be appreciated on the two‐dimensional view.)
Figure 2.
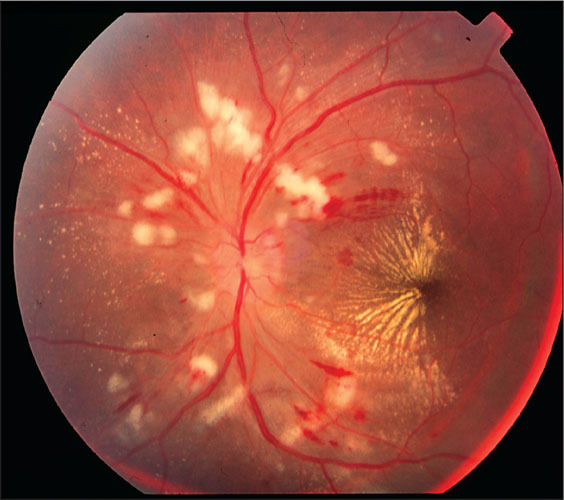
Retina, left eye. Blurring of the optic nerve head and diffuse peripapillary cotton‐wool spots, flame‐shaped, hemorrhages, diffuse exudates, and. a macular star. Intraretinal hemorrhages are noted in the nasal fovea, or central part, of the macula.
Hypertensive retinopathy is associated with systemic arterial hypertension. As more and more Americans are diagnosed with hypertension every year, it is important for clinicians to be aware of the acute and chronic changes seen in a funduscopic examination. In cases of malignant hypertension with grade 4 hypertensive retinopathy, patients have greatly elevated BP in association with ocular pathology including blurring of the optic disk margin (papilledema) with cotton‐wool spots, retinal hemorrhages, and retinal hard exudates. 1 These are important clues to ongoing systemic vascular involvement. A classic, but nonspecific, finding is a macular star of lipid that forms in association with optic nerve‐head swelling. The macular scar can be seen with chronic hypertension without malignant hypertension. In addition to extremely high Bps, patients with malignant hypertension present with evidence of cardiac, cerebral, and renal disorders due to vascular damage. 2 Changes in the retina may result in vision loss or blurry vision.
HISTOPATHOLOGY
Malignant hypertension causes pathologic changes that can be divided into three different categories: retinopathy, choroidopathy, and optic neuropathy. Retinopathy is usually the earliest finding in malignant hypertension and is manifested by arteriolar constriction, occlusion, ischemia, and resultant smooth muscle necrosis. This is followed by loss of autoregulation, vasodilation, and downstream transmission of high BP. Focal intraretinal peri‐arteriolar transudates are specific to, and some of the earliest findings in, malignant hypertension. These transudates result from leakage of the pre‐capillary arterioles and accumulation of fluid in the deep retina. Focal intraretinal periarteriolar transudates closely resemble cotton‐wool spots but are histologically different, as they occur in the outer retina. 1 , 3 Endothelial cell damage leads to loss of the blood–retinal barrier and leakage of plasma proteins into the retina with formation of hard exudates. A “macular star” is an uncommon finding that results from exudates collecting in the outer plexiform layer (or Henle's layer) in the retina. The orientation of neurons becomes much more oblique in the foveal region, or central part, of the macula, leading to the star pattern as the exudates accumulate in the outer plexiform layer. 1 Cotton‐wool spots (or cytoid bodies) are the result of focal areas of ischemia within the nerve fiber layer, leading to loss of axoplasmic flow and edema. The term “soft exudate” should not be used, since cotton‐wool spots are due to retinal infarctions rather than exudation. Retinal hemorrhages result from the breakdown of the inner blood–retinal barrier. Bleeding follows the path of the nerve fiber layer and results in flame‐shaped hemorrhages and bleeding within the retina (i.e., intraretinal hemorrhages). 1
The effects of acute elevations in BP more frequently affect the choroid that supplies blood vessels to the retina than the retina itself for several reasons. First, the choroid vessels have a very short course with minimal branching, leading to transmission of the BP downstream. Second, the choroid does not autoregulate the BP as well as the retinal vessels. The transmission of acute rises in BP leads to choroidal ischemia and retinal pigment epithelium necrosis, producing Elschnig spots. 4 Elschnig spots initially appear deep within the retina and are gray‐yellow in appearance; over time they become hyperpigmented. Retinal pigment epithelium functions in maintaining retinal attachment, and loss of the retinal pigment epithelium leads to serous retinal detachment. 1 , 5
Hypertensive optic neuropathy is a late finding in malignant hypertension. The presence of papilledema distinguishes malignant hypertension from accelerated hypertension. Optic disc edema with blurring of the optic nerve head margins is a common finding. The etiology of the edema is debated, with some experts believing that increased intracranial pressure leads to optic nerve swelling, while others feel that optic nerve head ischemia results in optic nerve edema. 1 , 6
OPTICAL COHERENCE TOMOGRAPHY
Optical coherence tomography (OCT) is a relatively new imaging technique that produces non‐invasive, high‐resolution, cross‐sectional images of optical reflectivity (Figures 3 and 4). OCT is similar to ultrasonographic imaging, except that it uses light instead of sound waves to produce a two‐dimensional image of optical scattering from tissue microstructures. 7 OCT is valuable in evaluating retinal thickness and locating the pathology. OCT allows clinicians to obtain a histologic evaluation of the retina in a clinical setting.
Figure 3.
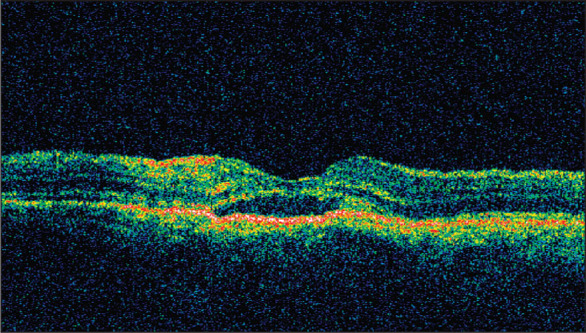
Optical coherence tomography, right eye. Foveal depression can be appreciated in the center of the photo. The area of hyporeflectance deep to the retina and superficial to the choroid is consistent with fluid and a subfoveal retinal detachment. Red and orange in the most superficial layers and middle retinal areas are areas of hyperreflectance and are consistent with hard exudates.
Figure 4.
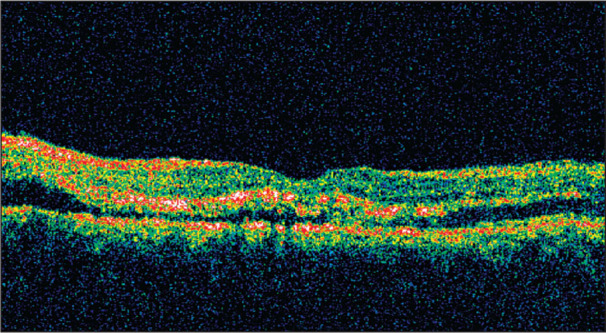
Optical coherence tomography, left eye. Area of reflectivity (dark area) in the subretinal space is consistent with subretinal fluid and an exudative retinal detachment. The areas of hyperreflectance (red and orange) in the middle retinal areas are consistent with hard exudates. These areas show localization of the hard exudates in the outer plexiform layer (or Henle's layer) of the retina.
To our knowledge, this is the second report of OCT demonstrating subretinal fluid due to an exudative retinal detachment caused by malignant hypertension. 8 Subretinal fluid can accumulate from three sources: incompetent retinal vasculature, choroidal or retinal pigment epithelial ischemia/infarction, or disc edema. In our patient, the etiology of the subretinal fluid is unclear and could be better defined with the use of fluorescein angiography.
RISK FACTORS FOR MALIGNANT HYPERTENSION
Malignant hypertension affects less than 1% of people with high BP. This emergency is more common in young adults, especially African‐American men. Other risk factors for malignant hypertension include renovascular hypertension, collagen vascular disorders, toxemia of pregnancy, and drugs such as cocaine, monoamine oxidase inhibitors, and oral contraceptives.
TREATMENT OF MALIGNANT HYPERTENSION
Malignant hypertension is accompanied by acute end‐organ damage such as retinopathy, encephalopathy, intracranial hemorrhage, renal failure, aortic dissection, 9 rupture of an abdominal aneurysm, 10 pulmonary edema, and acute myocardial infarction. 2 These patients require hospitalization and usually parenteral drug therapy. Within a matter of months, the fundus abnormalities that have been described will resolve as BP is lowered, but there may be permanent vision loss due to irreversible vascular shutdown. 3
References
- 1. Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension, V: hypertensive optic neuropathy. Ophthalmology. 1986;93:74–87. [DOI] [PubMed] [Google Scholar]
- 2. Prisant LM, Carr AA, Hawkins DW. Treating hypertensive emergencies. Controlled reduction of blood pressure and protection of target organs. Postgrad Med. 1993;93:92–96,. 101–104, 108–110. [DOI] [PubMed] [Google Scholar]
- 3. Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension, IV: focal intraretinal periarteriolar transudates. Ophthalmology. 1986;93:60–73. [DOI] [PubMed] [Google Scholar]
- 4. Bourke K, Patel MR, Prisant LM, et al. Hypertensive choroidopathy. J Clin Hypertens (Greenwich). 2004;6:471–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254:1178–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Luo BP, Brown GC. Update on the ocular manifestations of systemic arterial hypertension. Curr Opin Ophthalmol. 2004;15:203–210. [DOI] [PubMed] [Google Scholar]
- 7. Tso MO, Jampol LM. Pathophysiology of hypertensive retinopathy. Ophthalmology. 1982;89:1132–1145. [DOI] [PubMed] [Google Scholar]
- 8. Suzuki M, Minamoto A, Yamane K, et al. Malignant hypertensive retinopathy studied with optical coherence tomography. Retina. 2005;25:383–384. [DOI] [PubMed] [Google Scholar]
- 9. Prisant LM, Nalamolu VRP. Aortic dissection. J Clin Hypertens (Greenwich). 2005;7:367–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Prisant LM, Mondy JS III. Abdominal aortic aneurysm. J Clin Hypertens (Greenwich). 2004;6:85–89. [DOI] [PMC free article] [PubMed] [Google Scholar]


