Abstract
Few studies have examined the characteristics of patients presenting with hypertensive urgency, factors contributing to their presentation, or their management. The time and cost associated with treatment are unknown. Retrospective analysis of 50 emergency department patients with hypertensive urgency (symptomatic blood pressure (BP) elevation focusing on systolic BP >180 mm Hg or diastolic BP >110 mm Hg) was performed. The hospital database was queried to determine the cost of the average treat‐and‐release visit. The mean age was 54.3±15.6 years; 64% were female; 46% were black; 90% had diagnosed hypertension. The mean presenting BP was 198±27.6/109±17.3 mm Hg; 66% had systolic BP >180 mm Hg, and 38% had diastolic BP >110 mm Hg. Initially, 30% were not on antihypertensives, and 28% were on monotherapy. Headache (42%) and dizziness (30%) were most frequently reported symptoms. Presentation was most often attributed to running out of medication (16%). IV and oral labetalol were given to 28% and 24% of patients, respectively. Fifty‐six percent of patients had no change in baseline therapy at discharge. The average emergency department stay was 5 hours 17 minutes ± 4 hours 27 minutes. The average cost for similar visits in 2004 was $1543 per visit. Emergency department visits for hypertensive urgency are related mostly to noncompliance. Labetalol was the most frequently used therapy. Management in the primary care office could result in substantial cost savings.
Hypertensive crisis, a rapid, inappropriate, symptomatic elevation in blood pressure (BP), is a common clinical occurrence that accounts for as many as 3% of all emergency department (ED) visits. 1 , 2 The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) 3 divides hypertensive crisis into two categories: hypertensive emergency and hypertensive urgency. Hypertensive emergency is characterized by a severe elevation in BP in conjunction with end‐organ damage. 4 The organ systems most commonly affected include the cardiovascular, renal, and central nervous systems. Hypertensive urgency, on the other hand, does not have associated acute progressive end‐organ damage, but may impose risk of damage if not treated over several hours. 5 , 6
By definition, hypertensive emergency is a true medical emergency requiring immediate BP control in the inpatient setting, whereas BP elevation in hypertensive urgency can be reduced more slowly, and inpatient treatment is not necessarily required. 7 , 8
Hypertensive urgency frequently presents with symptoms such as headache, epistaxis, fatigue, psychomotor agitation, dyspnea, chest pain, and vertigo. 2 An elevation in BP in the absence of symptoms is sometimes referred to as hypertensive pseudocrisis. 9 Patients with urgency are often chronic hypertensives who are either noncompliant or inadequately treated, 6 although as many as 28% of patients presenting with hypertensive urgency may not have a previous diagnosis of hypertension. 2
Hypertensive urgency affects as many as 1% of individuals with hypertension. 10 Severe BP elevation can be alarming to both the patient and the physician. For many reasons, both medical and social, patients with hypertensive urgency frequently present or are referred to the ED for treatment. Unfortunately, there are scant data available to determine the characteristics of these patients, or to track their course of treatment in this setting. There has also been little research into the cost of treating these patients in the ED. The purpose of this study was to evaluate the characteristics of patients with hypertensive urgency presenting to the ED, and to determine the course of treatment of those who were managed in the ED without full inpatient admission. In addition, we set out to determine the cost of treat‐and‐release visits for hypertensive urgency in the ED setting.
There is no set BP cutoff for hypertensive urgency in the JNC 7, likely due to the fact that “a severe elevation in BP” is relative, depending on an individual patient's baseline BP. In the literature, it is frequently arbitrarily defined as a diastolic BP (DBP) >120 mm Hg 11 , 12 , 13 , 14 , 15 , 16 or a systolic BP (SBP) >200–210 mm Hg, 17 , 18 sometimes without regard to symptomatology. For our study, we chose to include patients who more closely fit the criteria as defined by JNC 7, and therefore studied patients with symptomatic BP elevation at any level, with a focus on those with SBP >180 mm Hg or DBP >110 mm Hg.
METHODS
This retrospective study was performed at Strong Memorial Hospital, a large, urban, tertiary care medical center in western New York. It comprised 50 patients who presented to the ED and met our criteria for hypertensive urgency between January 1, 2004 and May 31, 2004. Charts for review were identified by having “hypertension, unspecified” as the primary diagnosis code. (Hypertensive urgencies treated in the ED at our institution are coded as International Classification of Diseases, Ninth Revision [ICD‐9] 401.9.) Patients with incomplete records, complicating medical problems requiring a full hospital admission, documented pregnancy, end‐stage renal disease, or hypertensive emergency were excluded.
Data recorded included patient age, race/ethnicity, sex, previous history of hypertension, other medical history, previous treatment for hypertension, compliance with previous treatment, BP at triage, associated signs or symptoms of severe hypertension, therapy instituted, tests ordered, BP at discharge, duration of ED visit, therapy for discharge, and documentation of arranged outpatient follow‐up.
Data were recorded by the investigators without unique identifiers, and the data analysis was performed after all the records had been examined and the data collection was completed.
The hospital charges database was queried to determine the average cost of a treat‐and‐release visit for patients with hypertensive urgency during the 2004 fiscal year.
RESULTS
During the 5‐month study period, 107 charts were identified as having 401.9 (hypertension, unspecified) as the primary ICD‐9 code. Of these, 66 charts were randomly reviewed to identify 50 patients who met our criteria for hypertensive urgency. Of the 16 cases that were excluded, six had incomplete or missing records, four were admitted to the hospital for an unrelated malady, three met criteria for hypertensive emergency, two had renal failure requiring hemodialysis, and one was status post‐renal allograft transplant.
The baseline characteristics of the patients are shown in Table I. The mean age of the group was 54.3±15.6 years. Women made up 64% of the study group. The major racial breakdown was 46% black and 44% white.
Table I.
Baseline Characteristics (N=50)
| Demographics | n (%) |
|---|---|
| Age (yr) | |
| <40 | 11 (22) |
| 40–49 | 7 (14) |
| 50–59 | 11 (22) |
| 60–69 | 14 (28) |
| 70–79 | 5 (10) |
| ≥80 | 2 (4) |
| Gender | |
| Male | 18 (36) |
| Female | 32 (64) |
| Race/Ethnicity | |
| Black | 23 (46) |
| White | 22 (44) |
| Hispanic | 4 (8) |
| Asian | 1 (2) |
| Medical History | |
| Hypertension | 45 (90) |
| Hyperlipidemia | 7 (14) |
| Diabetes | 5 (10) |
| Coronary artery disease | 2 (4) |
| Cerebrovascular disease | 2 (4) |
| Clinical Presentation | |
| Triage blood pressure (mm Hg) | |
| Systolic >180 | 33 (66) |
| Diastolic >110 | 19 (38) |
| Systolic >180 and diastolic >110 | 17 (34) |
| Presenting symptoms | |
| Headache | 21 (42) |
| Dizziness | 15 (30) |
| Visual changes | 7 (14) |
| Chest discomfort | 7 (14) |
| Nausea | 5 (10) |
| Epistaxis | 3 (6) |
| Fatigue | 2 (4) |
| Psychomotor agitation | 2 (4) |
| Other | 6 (12) |
Forty‐five patients (90%) had a known diagnosis of hypertension. Analysis of the initial BP revealed that 66% had an SBP >180 mm Hg, and 38% had a DBP >110 mm Hg. Of note, 34% of the patients had both a DBP >110 mm Hg and an SBP >180 mm Hg. Fifteen patients (30%) had symptomatic BP elevation with a presenting SBP <180 mm Hg or DBP <110 mm Hg. The mean BP at presentation was 198±27.6/109±17.3 mm Hg.
The most frequent presenting symptoms, in decreasing order, were: headache, dizziness, visual changes and chest discomfort, nausea, epistaxis and fatigue, and psychomotor agitation.
A review of the subjects' medications (Table II) demonstrated that 30% were on no medication at the time of evaluation, 28% were on monotherapy, and 26% were on two antihypertensive medications. Beta blockers (including α/β blockers) and diuretics were each taken by 28% of the patients studied, with calcium channel blockers, angiotensin‐converting enzyme (ACE) inhibitors, and angiotensin receptor blockers being taken by 26%, 22%, and 16% of patients, respectively.
Table II.
Outpatient Medications and Compliance With Care
| Medications/Compliance | n (%) |
|---|---|
| Number of antihypertensives at baseline | |
| None | 15 (30) |
| 1 | 14 (28) |
| 2 | 13 (26) |
| 3 | 5 (10) |
| ≥4 | 2 (4) |
| Current antihypertensive(s) | |
| β Blockers | 14 (28)* |
| Diuretics | 14 (28) |
| Calcium channel blockers | 13 (26) |
| Angiotensin‐converting enzyme inhibitors | 11 (22) |
| Angiotensin receptor blockers | 8 (16) |
| Clonidine | 2 (4) |
| α Blockers | 1 (2) |
| Factors contributing to blood pressure elevation | |
| Ran out of medication | 8 (16) |
| Recent medication change | 7 (14) |
| Noncompliance | 6 (12) |
| No primary medical doctor (PMD) | 2 (4) |
| No visit to PMD in >1 year | 2 (4) |
| Recent diagnosis of hypertension | 1 (2) |
| *Four patients in this group were on combination α/β blockers. | |
Patients running out of medication contributed to 16% of the ED visits that we reviewed. Recent medication changes were cited in 14% of the cases, and noncompliance in 12%. Lack of a primary medical doctor (PMD) was noted by only two patients.
Table III details the medications that were administered in the ED. The IV and p.o. α/β blocker labetalol was administered to 28% and 24% of the patients, respectively. Acetaminophen, β blockers, diuretics, and ACE inhibitors were administered to 16%, 14%, 12%, and 10% of the patients, respectively, while calcium channel blockers, clonidine, and p.o. narcotics were all given to 8% of the patients. Table IV lists the laboratory tests that were most frequently ordered, which included chemistries (72%), complete blood counts (70%), urinalyses (44%), troponins (32%), and coagulation studies (22%). Electrocardiograms (ECGs) were obtained on 70% of the patients, and chest x‐rays and head computed tomograms in 24% and 12% of the cases. No tests, procedures, or radiographic studies were ordered on 10% of the patients that were seen.
Table III.
Emergency Department Medication Administration (N=50) (n [%])
| Medication | p.o. | IV |
|---|---|---|
| α/β Blockers | 12 (24) | 14 (28) |
| β Blockers | 7 (14) | 0 |
| Diuretics | 6 (12) | 0 |
| Angiotensin‐converting enzyme inhibitors | 5 (10) | 0 |
| Calcium channel blockers | 4 (8) | 1 (2) |
| Clonidine | 4 (8) | ‐ |
| Angiotensin receptor blockers | 1 (2) | ‐ |
| Nitroglycerin | 3 (6)* | 0 |
| Narcotics | 4 (8) | 1 (2) |
| Acetaminophen | 8 (16) | ‐ |
| Aspirin | 2 (4) | ‐ |
| Nonsteroidal anti‐inflammatories | 1 (2) | 3 (6) |
| Benzodiazepines | 3 (6) | 1 (2) |
| *Nitroglycerin was administered topically in two cases and sublingually in the other. | ||
Table IV.
Diagnostic Tests and Procedures Performed in the Emergency Department
| Test/Procedure | n (%) |
|---|---|
| Laboratory | |
| Complete blood cell count | 35 (70) |
| Chemistry | 36 (72) |
| Prothrombin/partial thromboplastin time | 11 (22) |
| Thyroid function | 5 (10) |
| Troponin | 16 (32) |
| Antinuclear antibody | 1 (2) |
| Erythrocyte sedimentation rate | 2 (4) |
| Amylase/lipase | 3 (6) |
| Lipid profile | 1 (2) |
| Urinalysis | 22 (44) |
| Toxicology screen | 2 (4) |
| Procedures | |
| Electrocardiogram | 35 (70) |
| Lumbar puncture | 1 (2) |
| Fasting blood glucose | 3 (6) |
| Radiography | |
| Chest x‐ray | 12 (24) |
| Computed tomography | 6 (12) |
| Magnetic resonance imaging/angiogram | 1 (2) |
| None | 5 (10) |
The mean reduction in SBP achieved over the course of the visit was 41±30.0 mm Hg and the mean DPB reduction was 19±20.8 mm Hg. The mean BP at discharge was 158±23.2/90±18.8 mm Hg. Figure 1 shows a breakdown of the time patients spent in the ED. The average length of stay in the ED was 5 hours 17 minutes ± 4 hours 27 minutes. Five patients were admitted to the ED observation unit for monitoring before discharge.
Figure 1.
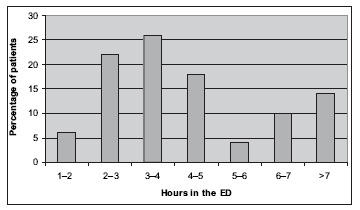
A percentage breakdown of the number of hours spent in the emergency department (ED) for a visit for hypertensive urgency. Five of the seven visits longer than 7 hours included admission to the observation unit.
Most (56%) of the patients who were seen had no change in their current medical regimen at the time of discharge (Figure 2), although 37% of this group of patients were either noncompliant or had run out of medication. New antihypertensives were started in 36% of the patients, and an increase in the dose of an existing antihypertensive medication was made in 8% of the cases. Two patients left against medical advice before a therapeutic plan was devised. Labetalol and hydrochlorothiazide (HCTZ) were the most frequently prescribed medications at discharge, representing 38.9% and 33.3% of all discharge prescriptions, respectively. Captopril, clonidine, amlodipine, metoprolol, and diltiazem each represented 5.6% of the prescriptions written.
Figure 2.
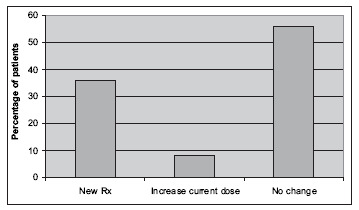
A review of the discharge management decision from the emergency department that included a new antihypertensive medication prescription, an increase in the current dose of medications that the patient was already prescribed, or no change in the patient's antihypertensive regimen.
Follow‐up appointments were scheduled for 22% of the patients who were seen (Figure 3), whereas recommendations for follow‐up either with the PMD or in the medicine clinic were given to 68%. The PMD was notified about the visit 42% of the time. Return instruction were provided to 64% of the patients. The two patients who left against medical advice left before follow‐up or return instructions could be provided.
Figure 3.
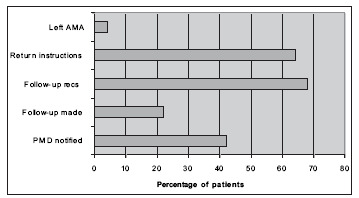
Discharge management from the emergency department (ED) showing the percentage of patients who received, instructions about symptoms that should prompt return to the ED, the percentage who received recommendations (recs) for follow‐up vs. those for which a follow‐up appointment was actually made, and the percentage of patients whose primary medical doctor (PMD) was contacted regarding the ED visit. AMA=against medical advice
There were 215 treat‐and‐release visits to the ED with a primary diagnosis code 401.90 during 2004 at our institution. A query of the database showed that the average cost per visit was $1543.
DISCUSSION
Despite the prevalence of hypertensive urgency in the ED, very few studies have looked in detail at the characteristics of the patients who present, and how they are managed. The two largest series that we came across were those by Zampaglione et al. 2 carried out in the ED of the Martini Hospital in Turin, Italy, and Martin et al. 5 carried out in a university‐affiliated hospital in Brazil. Compared with these studies, our study had a smaller sample size (50 vs. 341 in Zampaglione et al. and 273 in Martin et al.), but looked more closely at the characteristics of the patients, their underlying care, and their course of treatment in the ED. The mean age of our patients was 54.3±15.6 years compared with 60±14 years in Zampaglione et al. and 49.9±18.6 years in Martin et al. The presenting SBP in our group was 198±27.6 mm Hg, compared with 210±27 mm Hg in Zampaglione et al. and 191±26.9 mm Hg in Martin et al., and the initial DBP was 109±17.3 mm Hg vs. 126±10 mm Hg and 126.6±14.4 mm Hg, respectively. The ratio of men to women was fairly consistent with the other two studies, but our population was more racially diverse, and we had significantly fewer patients with previously unknown hypertension (10% vs. 28% and 19.8%), which may be a reflection of the level of access to health care in the populations studied. Compared with the population of the city of Rochester, 19 women (64% vs. 52.2%) and African Americans (46% vs. 40.7%) were overrepresented among patients presenting with hypertensive urgency.
The distribution of hypertensive urgency according to age group was somewhat bimodal, and showed a higher prevalence in patients aged 50–69 and patients younger than 40 years of age. This was an interesting finding, because hypertension is more prevalent in the older population, but hypertensive urgency is a problem that occurs with significant frequency even in younger individuals. Noncompliance was reported in 12% of the patients, and a further 16% reported not having taken their medication because they had recently run out, thereby suggesting that more than one quarter of the visits might have been prevented if the patients had actually been on therapy. An astounding 30% of the patients were not on any antihypertensive therapy at baseline, and the reasons for this included complaints related to side effects, lack of a PMD, not having seen a physician in several years, and frank noncompliance. The majority were taking one or two medications, and of those whose medication doses were actually recorded, few were on maximal therapeutic doses. This finding is in accord with the report that hypertension is inadequately treated in approximately 69% of patients in the United States. 20 Beta blockers, diuretics, and calcium channel blockers were the most frequently prescribed medications in our population.
The symptoms at presentation comprised mainly headaches and dizziness, as was also found in the study by Martin et al. 5 Twelve percent of the patients underwent computed axial tomography of the head, presumably to rule out stroke. Diagnostic tests comprised mainly chemistries, complete blood counts, and ECGs, which were performed in almost three quarters of the patients. Troponins were checked in about one third of the patients, although chest discomfort was reported in only 14% of patients. Interestingly, 10% of the patients that were seen did not have any documented diagnostic tests performed. This raises the question of the necessity for ED care in these cases.
Treatment was primarily in the form of labetalol, with IV formulations used more often than oral forms. Labetalol is a fast‐acting combined α and β receptor antagonist with an onset of action within 2–5 minutes administered IV, and 15–30 minutes when given orally. 21 , 22 Following β blockers, HCTZ was the next most commonly used antihypertensive agent, which is interesting, since it is a medication with a slow onset of action and a longer duration of action. 23 Twenty‐five percent of patients receiving HCTZ did not receive any additional antihypertensive therapy. Although the BP reduction in hypertensive urgency does not need to be achieved with the same rapidity as hypertensive emergency, the general recommendations are to reduce the BP over a period of somewhere between 4 and 48 hours to avoid the development of end organ damage. 7 , 8 , 24
The exact timing of BP reduction in hypertensive urgency, and the most appropriate method, has not been studied prospectively or clearly defined. No one has looked specifically at morbidity and mortality outcomes in patients treated with IV vs. oral medications, or even at outcomes related to treatment in the physician's office vs. the ED or an inpatient unit. Some authorities argue that BP reduction can be achieved on an outpatient basis, and that acute alterations in BP with IV medications are gratifying to the physician, but potentially more harmful to the patient because of the risk of relative hypotension leading to ischemic brain damage, myocardial infarction, or renal infarction. 8 , 24 , 25 On the other hand, recent studies have shown that the use of IV medications such as labetalol, urapidil, and enalaprilat have not been associated with an increased risk of severe complications. 17 , 26 , 27
No studies have looked at the incidence of progression from hypertensive urgency to emergency to determine whether an aggressive treatment strategy with IV medications is necessary. It has been suggested that patients who have adequate follow‐up can tolerate lowering of their BP over 24–48 hours with oral medications, and that those who do not, should be monitored and have their BP reduced over 4–6 hours. 8 , 25 , 28 A study by Hirschl et al. 29 showed that patients treated initially with an IV antihypertensive agent benefited from therapy with an oral agent before discharge to avoid recurrent hypertensive episodes 12 hours after discharge. This study reinforces the need for continued therapy beyond the ED setting. It is interesting that in our study, 56% of the patients who were treated in the ED did not have any changes made to their current antihypertensive regimens. Although 37% in this group were noncompliant or had run out of medication, 63% were taking their prescribed therapy at the time of presentation, and only 11 % were on three or more antihypertensives. Those who did receive new medications were predominantly prescribed either labetalol or HCTZ.
The average length of stay in the ED was over 5 hours, and the average charge for treat‐and‐release visits coded as hypertensive urgency during the 2004 fiscal year was $1546. Certainly, the time and cost of treating hypertensive urgency is not a trivial matter, and in this regard, patients presenting to the office with an elevated BP with minimal symptoms, and without concern for impending end organ damage should probably not be sent to the ED for management. Treatment of these patients in the primary care setting with conservative BP control and close follow‐up is probably a reasonable approach that would result in substantial cost savings.
Studies prospectively evaluating the optimal treatment of patients presenting to the ED with hypertensive urgency looking at end points of morbidity and mortality, treatment efficacy, and cost are warranted. There is currently no evidence‐based approach to the treatment of this very common problem. Our study provides important insight into the practice that is common at our institution, but it is difficult to know how practice varies from region to region, and among institutions. Our study is limited in this respect, but we feel it is an important first step in evaluating the underlying factors that may contribute to the presentation of these patients, and it gives us the opportunity to examine our therapeutic approach based on what is currently known. In addition, this study provides important information about the cost of treating hypertensive urgency, and directs us to think about more cost‐effective strategies for approaching this problem.
CONCLUSIONS
Our data reveal that hypertensive urgency is a problem seen mainly in patients with a known diagnosis of hypertension, who are either noncompliant or have recently not had access to medication. The majority are probably undertreated. Treatment in the ED consists mainly of labetalol, and the outpatient therapeutic regimen remains largely unchanged at the time of discharge. Follow‐up care is often recommended and less frequently scheduled, and the primary care physician is often not informed of the problem. An evidence‐based approach is needed to help us improve the effectiveness and cost efficiency of our current practice in the management of this important problem.
References
- 1. Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25: 305–313. [DOI] [PubMed] [Google Scholar]
- 2. Zampaglione B, Pascale C, Marchisio M, et al. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension. 1996;27: 144–147. [DOI] [PubMed] [Google Scholar]
- 3. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289: 2560–2572. [DOI] [PubMed] [Google Scholar]
- 4. Houston M. Hypertensive emergencies and urgencies: pathophysiology and clinical aspects. Am Heart J. 1986;111: 205–210. [DOI] [PubMed] [Google Scholar]
- 5. Martin J, Higashiama E, Garcia E, et al. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol. 2004;83: 131–136. [DOI] [PubMed] [Google Scholar]
- 6. Calhoun DA, Oparil S. Treatment of hypertensive crisis. N Engl J Med. 1990;323: 1177–1183. [DOI] [PubMed] [Google Scholar]
- 7. Cherney D, Straus S. Management of patients with hypertensive urgencies and emergencies: a systematic review of the literature. J Gen Intern Med. 2002;17: 937–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gegenhuber A, Lenz K. Hypertensive emergency and urgency. Herz. 2003;28: 717–724. [DOI] [PubMed] [Google Scholar]
- 9. Severe symptomless hypertension [editorial]. Lancet. 1989;2: 1369–1370. [PubMed] [Google Scholar]
- 10. Bechgaard P, Kopp H, Nielson J. One thousand hypertensive patients followed from 16–22 years. Acta Med Scand. 1956;312(suppl):175–183. [DOI] [PubMed] [Google Scholar]
- 11. Habib GB, Dunbar LM, Rodrigues R, et al. Evaluation of the efficacy and safety of oral nicardipine in the treatment of urgent hypertension: a multinational, randomized, double‐blind, parallel, placebo‐controlled trial. Am Heart J. 1995;129: 917–923. [DOI] [PubMed] [Google Scholar]
- 12. Komsuoglu B, Sengun B, Bayram A, et al. Treatment of hypertensive urgencies with oral nifedipine, nicardipine, and captopril. Angiology. 1991;42: 447–454. [DOI] [PubMed] [Google Scholar]
- 13. Jaker M, Atkin S, Soto M, et al. Oral nifedipine vs. oral clonidine in the treatment of urgent hypertension. Arch Intern Med. 1989;149: 260–265. [PubMed] [Google Scholar]
- 14. Panacek EA, Bednarczyk EM, Dunbar LM, et al. Randomized, prospective trial of fenoldopam vs. sodium nitroprusside in the treatment of acute severe hypertension. Acad Emerg Med. 1995;2: 959–965. [DOI] [PubMed] [Google Scholar]
- 15. Pilmer BL, Green JA, Panacek EA, et al. Fenoldopam mesylate versus sodium nitroprusside in the acute management of severe systemic hypertension. J Clin Pharmacol. 1993;33: 549–553. [DOI] [PubMed] [Google Scholar]
- 16. Reisin E, Huth M. Intravenous fenoldopam versus sodium nitroprusside in patients with severe hypertension. Hypertension. 1990;15(suppl I):I59–I62. [DOI] [PubMed] [Google Scholar]
- 17. Hirschl MM, Seidler D, Zeiner A, et al. Intravenous urapidil versus sublingual nifedipine in the treatment of hypertensive urgencies. Am J Emerg Med. 1993;11: 653–656. [DOI] [PubMed] [Google Scholar]
- 18. Wallin JD, Fletcher E, Ram CV, et al. Intravenous nicardipine for the treatment of severe hypertension: a doubleblind, placebo‐controlled multicenter trial. Arch Intern Med. 1989;149: 2662–2669. [PubMed] [Google Scholar]
- 19. US Census Bureau. American fact finder: Census 2000, Rochester, New York.Available at: http:factfinder.census. gov. Accessed October 10, 2005. [Google Scholar]
- 20. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States,. 1988–2000. JAMA. 2003;290: 199–206. [DOI] [PubMed] [Google Scholar]
- 21. Kanto J, Allonen H, Kleimola T, et al. Pharmacokinetics of labetalol in healthy volunteers. Int J Clin Pharmacol Ther Toxicol. 1981;19: 41–44. [PubMed] [Google Scholar]
- 22. McNeil JJ, Louis WJ. Clinical pharmacokinetics of labetalol. Clin Pharmacokinet. 1984;9: 157–167. [DOI] [PubMed] [Google Scholar]
- 23. Lutterodt A, Nattel S, McLeod PJ. Duration of antihypertensive effect of a single daily dose of hydrocholothizide. Clin Pharmacol Ther. 1980;27: 324–327. [DOI] [PubMed] [Google Scholar]
- 24. Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest. 2000;118: 214–227. [DOI] [PubMed] [Google Scholar]
- 25. Ram CV. Immediate management of severe hypertension. Cardiol Clin. 1995;13: 579–591. [PubMed] [Google Scholar]
- 26. Huey J, Thomas JP, Hendricks DR, et al. Clinical evaluation of intravenous labetalol in the treatment of hypertensive urgency. Am J Hypertens. 1988;1: 284S–289S. [DOI] [PubMed] [Google Scholar]
- 27. Hirschl MM, Binder M, Bur A, et al. Clinical evaluation of different doses of intravenous enalaprilat in patients with hypertensive crises. Arch Intern Med. 1995;155: 2217–2223. [PubMed] [Google Scholar]
- 28. Grossman E, Ironi An, Messerli FH. Comparative tolerability profile of hypertensive crisis treatments. Drug Saf. 1998;19: 99–122. [DOI] [PubMed] [Google Scholar]
- 29. Hirschl M, Herkner H, Bur A, et al. Course of blood pressure within the first 12 h of hypertensive urgencies. J Hypertens. 1998;16: 251–255. [DOI] [PubMed] [Google Scholar]


