Abstract
Alterations in the circadian rhythm of blood pressure, Alterations in the circadian rhythm of blood pressure, risk. Estimates of the magnitude of the blood pressure surge on rising vary depending on technique and population, but it is usually around 10–30 mm Hg systolic and 7–23 mm Hg diastolic. The magnitude of the surge increases with age, alcohol consumption, and smoking and is greater in whites. Blood pressure variations and morning plasma aldosterone are closely correlated. A high morning surge is linked to increased target organ damage as well as strokes and other cardiovascular complications. Therapeutic options exist to reduce the magnitude of the morning blood pressure surge—notably, the use of drugs with a long duration of action, the use of medications that specifically antagonize the morning surge (such as α blockers), and the administration of drugs upon awakening but before rising.
Blood pressure (BP) variation is a phenomenon that has been well known for many years, which to date has mainly been considered in relation to its consequences for the reliability of measurements. However, this variability also appears to be linked to the cardiovascular complications of hypertension, independent of the average BP level. Ambulatory techniques for monitoring BP are now facilitating the investigation of this phenomenon, in particular its circadian component. Two aspects of this circadian variation have been the subject of studies; however, results may seem contradictory. The loss of the nyctohemeral cycle of BP (nondipper profile) is accompanied by increased cardiovascular risk. The excessive morning BP surge, on rising, also appears to increase risk. This report summarizes the available data on the morning BP surge and its consequences and examines the relationship of the risks of this surge with the dangers of the nondipper profile.
CIRCADIAN VARIATIONS OF BP
The development of automatic monitoring has led to the description of the circadian variation of BP. We must recall the pioneering work of Richardson and colleagues 1 who, with the assistance of an automatic device using the oscillometric method and the simultaneous recording of the electroencephalogram (EEG), wrote: “The pressure fell before EEG evidence of sleep, fell further during sleep and rose sharply in the morning after the subject woke.” Fundamentally important observations were made by the use of continuous, uninterrupted, intra‐arterial measurements using methodology developed by the Oxford team, 2 , 3 which clearly showed that BP was at its lowest during nighttime and rose in the morning to reach its highest values at midmorning. 4 These studies suggested that a BP surge in the early morning before waking was the result of an internal clock. This notion has been widely held for many years, but is an artifact that results from the likelihood that individuals who were studied awakened at different times. When the results are expressed in relation to the time of waking rather than the time of day, there is no longer any marked BP surge preceding this arousal. 5 , 6
Several studies 7 , 8 (such as Richardson's initial report) have shown that the essential mechanism of the morning BP surge is waking and, undoubtedly even more important, rising. 9 , 10
IMPORTANCE OF THE PRESSURE SURGE ON RISING
Several methods of measuring BP on rising have been described. For many years, we have asked patients who are fitted with ambulatory BP monitoring devices to measure BP on rising in the morning, at the point when they put their feet on the floor, and in the evening, just after going to bed. The initial aim was to accurately evaluate these two points, which are essential for calculating pressure averages during activity and at rest. 11 , 12 This method can be used to calculate the BP surge on rising as the difference between the measurement taken on rising and the last measurement recorded by the apparatus in the previous half hour during sleep. In a population of normotensive subjects, the increase in BP on rising measured in this way is on average 11 mm Hg for systolic BP (SBP) and 12 mm Hg for diastolic BP. 6 In a population of hypertensive patients it is basically similar: 14 mm Hg for systolic pressure and 12 mm Hg for diastolic pressure, but with extremes that can reach 80 mm Hg for systolic pressure. 13 , Figure 1 shows the distribution of the SBP surge values on rising in a population of 507 untreated hypertensive patients.
Figure 1.
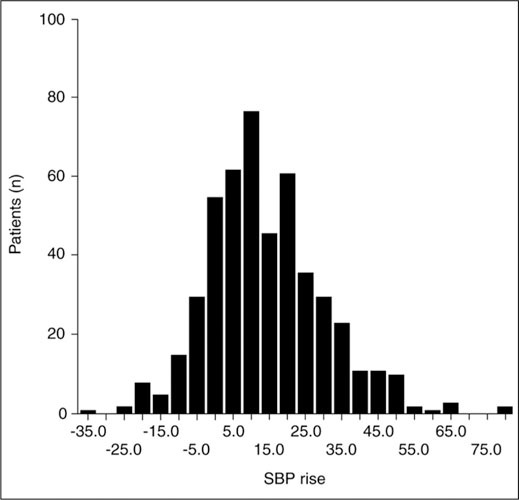
Distribution of the systolic blood pressure (SBP) surge on rising in a population of 507 untreated hypertensive subjects. Data derived from J Hypertens. 2004;22:1113–1118. 13
Since 1996, we have been using an ambulatory BP monitoring device equipped with a positioning sensor (Diasys Integra, Novacor, France), which automatically records BP at the point when the patient gets up. The results obtained are similar to those produced by manual monitoring. 13 One of the advantages of an automatic sensor is that it also allows any effects of a siesta to be taken into consideration.Rising after a siesta is also accompanied by a BP surge, although this is smaller. 14 Another approach consists of defining the morning BP as the average of the pressures over a certain period (2–4 hours) after rising and the BP preceding rising as the average over an identical duration before rising. The morning surge is then defined as the difference between these two averages. 10 , 15 A third approach is based on defining the minimum nighttime BP as the average of three measurements: the lowest and the two measurements on either side of this. The BP surge on rising is then calculated as the difference between the average of the measurements in the 2 hours following rising and the minimum BP. These different methods of calculation produce estimates of the pressure surge on risings that are significantly different (Table I).
Table I.
Magnitude of the Blood Pressure (BP) Surge (mm Hg) on Rising Reported in Normotensives and Hypertensives Using Different Techniques
| Normotensives | Hypertensives | |||||
|---|---|---|---|---|---|---|
| N | SBP | DBP | N | SBP | DBP | |
| Rising BP/pre‐awakening BP (one measure) | ||||||
| Gosse et al. 6 , 13 | 233 | 11±14 | 12±13 | 507 | 14±16 | 12±12 |
| Baumgart and Rahn 60 | 111 | 14 | 13 | 109 | 16 | 13 |
| Morning BP (2 h)/pre‐awakening BP (2 h) | ||||||
| Kario et al. 15 | — | — | — | 466 | 9±14 | 6.5±9 |
| Morning BP (4 h)/pre‐awakening BP (4 h) | ||||||
| Leary et al. 10 | — | — | — | 420 | 23±13 | 15±10 |
| Morning BP (2 h)/lowest night BP | ||||||
| Kario et al. 15 | — | — | — | 466 | 29±13 | 17±10 |
| Gosse et al. 16 | — | — | — | 1419 | 29±13 | 24±10 |
| Data are mean or mean ± SD. SBP=systolic BP; DBP=diastolic BP | ||||||
The BP surge on rising does not seem to be influenced by gender. 13 , 16 In our experience, the SBP surge on rising is loosely correlated with age. In a large pooled analysis of 1419 patients with hypertension, we found that the magnitude of the SBP surge increased from 26 mm Hg in patients younger than 46 to 31 mm Hg in patients 60 years of age or older. 16 No such increase was observed in diastolic BP surge. Ethnicity, alcohol consumption, smoking status, and duration of sleep also affected both SBP and diastolic BP.
The strongest predictor for the morning surge was BP variability during sleep expressed by the SD of individual measurements: the lowest quartile of BP variability during sleep had a BP surge of 25/20 mm Hg compared with 33/29 mm Hg in the highest quartile (Figure 2). 16 Similar results have been observed previously, along with a strong link to the difference in BP level between activity and rest. 13 Although the surge is accompanied by an increase in cardiac rate, there is no significant correlation between the variations in BP and heart rate on rising. 13 , 16 We also found a significant correlation between BP and the level of morning plasma aldosterone, but none with cortisol. A preliminary study shows that the SBP surge on rising could be associated with a degree of hostility. 17
CONSEQUENCES OF BP SURGE ON RISING
The morning period is accompanied by a peak in incidence of cardiovascular complications. Ischemic changes on Holter electrocardiographic 18 recordings, episodes of unstable angina, 19 vascular cerebral accidents, 20 , 22 , 23 , 24 myocardial infarction, and sudden death 25 , 26 have all been observed. The period that follows rising is accompanied by an increased risk of cardiovascular complications of 30%–40% in comparison with other periods of the day 27 ; it is therefore logical to associate this with the sudden and daily BP surge on rising. This hypothesis is reinforced by demonstrating the parallelism between BP, activity, and the incidence of cardiovascular events, with a dual peak found in countries where siestas are a normal custom. 24 , 28 , 29 Another disconcerting fact is that the morning BP surge seems to be highest on Mondays; this is also reflected in the incidence of cardiovascular complications. 30 It is difficult, however, to prove that the BP surge is directly responsible. In fact, the morning period is accompanied by various changes that could also play a role in the increase of cardiovascular events: activation of the sympathetic nervous system, 31 , 32 , 33 , 34 increase in cortisol, increase in platelet aggregability, 35 activation of the angiotensin‐renin system, and reduction in endothelial function. 36 , 37 A few studies have provided some proof of the relationship between BP surge and increased cardiovascular events. The BP surges on rising may affect left ventricular mass and the degree of left ventricular hypertrophy independent of the average BP over 24 hours. 13 , 38 , 39 , 40 , 41 , 42 The BP surges may also contribute to increasing the carotid artery intima‐media thickness. 43 , 44 This correlation between the BP surge in the morning and target organ damage, independent of the average BP level over 24 hours, provides indirect proof that the daily BP surge may have hemodynamic consequences. Two studies have now reported a connection between the SBP surge on rising and the incidence of cardiovascular complications in the hypertensive subject, independent of the average BP level over 24 hours. 13 , 15 , 45 , 46
MORNING RISER AND NONDIPPER: CAN THE TWO CONCEPTS BE RECONCILED?
Subjects presenting a profile of a nondipper type, with lack of a BP decrease during sleep, do not present any significant BP surge on rising although their cardiovascular risk is clearly increased. 46 The contradiction is only apparent, rather than real; both BP elevation and high BP variability should be considered factors in evaluating risk. Morning BP can rise moderately without any significant increase in variability (moderate morning riser hypertensive), may surge extremely on rising (extreme morning riser) with increased BP variability during sleep and when awake, or permanently stay at an elevated BP level (permanent riser/nondipper), which also appears to be connected to increased variability (Table II). The risk appears to be increased between the first and the second and
Table II.
Comparison of Blood Pressure (mm Hg) According to Dipper and Riser Status in Patients With Essential Hypertension 16
| Dipper/Moderate Riser (n=3 57) | Dipper/Extreme Riser (n=595) | Nondipper (n=25 5) | |
|---|---|---|---|
| 24‐H mean | 145/92 | 147/92 | 151/93* |
| Wake mean | 153/99 | 156/99** | 152/94† |
| Sleep mean | 130/80 | 128/77 | 147/90* |
| Nighttime low | 124/74 | 118/69** | 136/81*,† |
| Early morning mean | 144/94 | 157/100** | 155/97* |
| Morning surge | 20/21 | 40/31** | 19/16† |
| Wake variability | 10.6/8.2 | 11.6/8.7** | 11.6/9.1* |
| Sleep variability | 8.7/7.6 | 9.9/8.3** | 10.1/8.1* |
| Dipper=sleep mean systolic blood pressure (SBP) <90% of wake mean SBP and sleep mean diastolic blood pressure (DBP) <90% of wake mean DBP; moderate riser=morning surge (SBP) <28 mm Hg (median); extreme riser=morning surge (SBP) ≥28 mm Hg (median); nondipper=sleep mean SBP ≥90% of wake mean SBP and sleep mean DBP ≥90% of wake mean DBP; *p<0.0001 in test regarding SBP between nondipper and dipper/moderate riser; **p<0.0001 in test regarding SBP between dipper/extreme riser and dipper/moderate riser; † p<0.0001 in test regarding SBP between nondipper and dipper/extreme riser. Data derived from J Hypertens. 2006;24(suppl 4):S301.16 | |||
probably between the second and the third groups (Figure 3). However, this hypothesis remains to be confirmed in larger groups of patients.
Figure 3.

Diagrammatic representation of the modes of blood pressure surge over 24 hours
THERAPEUTIC APPLICATIONS
If we accept the possible causal link between the BP surge on rising and the occurrence of cardiovascular complications, we must then consider this surge as a therapeutic target. This is all the more important given that antihypertensive medications are usually taken in the morning, after rising. Consequently, the BP surge on rising occurs at the time when the treatment taken the previous day may be less effective. Several strategies have been proposed to date:
-
•
Administration of treatment in the evening rather than the morning. So far, this strategy has not produced very convincing results for controlling BP on rising. 47 , 48 , 49 , 50 , 51 , 52 , 53
-
•
The use of an extended‐action drug, taken in the morning, but whose effect continues for longer than 24 hours 54 , 55 , 56 , 57
-
•
The use of drugs that are more specifically effec tive against the BP surge on rising, such as a blockers 58 and central α2 agonists 59
-
•
The administration of drugs on awakening, before rising 60 , 61
The relative advantages of these different strategies is difficult to evaluate. To date, one single study appears to favor a benefit linked directly with reducing the morning BP peak, with the observation of a significant correlation between the decrease in this peak and the reduction of the carotid artery intimamedia thickness. 43 Whatever the case, the morning period should receive special attention when antihypertensive strategies are evaluated.
References
- 1. Richardson DW, Honour AJ, Fenton GW, et al. Variation in arterial pressure throughout the day and night. Clin Sci. 1964;26:445–460. [PubMed] [Google Scholar]
- 2. Bevan AT, Honour AJ, Stott FH. Direct arterial pressure recording in unrestricted man. Clin Sci. 1969;36:329–344. [PubMed] [Google Scholar]
- 3. Goldberg AD, Raftery EB, Green HL. The Oxford continuous blood‐pressure recorder—technical and clinical evaluation. Postgrad Med J. 1976;52(suppl 7):104–109. [PubMed] [Google Scholar]
- 4. Millar‐Craig MW, Bishop CN, Raftery EB. Circadian variation of blood‐pressure. Lancet. 1978;1:795–797. [DOI] [PubMed] [Google Scholar]
- 5. Floras JS, Jones JV, Johnston JA, et al. Arousal and the circadian rhythm of blood pressure. Clin Sci Mol Med Suppl. 1978;4:395s–397s. [DOI] [PubMed] [Google Scholar]
- 6. Gosse P, Lamaison C, Roudaut R, et al. Ambulatory blood pressure monitoring. Values in normotensive patients and suggestions for interpretation. Thérapie. 1991;46:305–309. [PubMed] [Google Scholar]
- 7. Mancia G, Ferrari A, Gregorini L, et al. Blood pressure and heart rate variabilities in normotensive and hypertensive humans beings. Circ Res. 1983;53:96–104. [DOI] [PubMed] [Google Scholar]
- 8. Baumgart P, Walger P, Fuchs G, et al. Twenty‐four‐hour blood pressure is not dependent on endogenous circadian rhythm. J Hypertens. 1989;7:331–334. [PubMed] [Google Scholar]
- 9. Khoury AF, Sunderajan P, Kaplan NM. The early morning rise in blood pressure is related mainly to ambulation. Am J Hypertens. 1992;5:339–344. [DOI] [PubMed] [Google Scholar]
- 10. Leary AC, Struthers AD, Donnan PT, et al. The morning surge in blood pressure and heart rate is dependent on levels of physical activity after waking. J Hypertens. 2002;20:865–870. [DOI] [PubMed] [Google Scholar]
- 11. Gosse P, Ansoborlo P, Lemetayer P, et al. Daytime and nighttime ambulatory blood pressures should be calculated over the true sleep/waking cycle and not over arbitrary periods. Am J Hypertens. 1996;9:269–272. [DOI] [PubMed] [Google Scholar]
- 12. Peixoto Filho AJ, Mansoor GA, White WB. Effects of actual versus arbitrary awake and sleep times on analyses of 24‐h blood pressure. Am J Hypertens. 1995;8:676–680. [DOI] [PubMed] [Google Scholar]
- 13. Gosse P, Lasserre R, Minifie C, et al. Blood pressure surge on rising. J Hypertens. 2004;22:1113–1118. [DOI] [PubMed] [Google Scholar]
- 14. Bursztyn M, Mekler J, Ben‐Ishay D. The siesta and ambulatory blood pressure: is waking up the same in the morning and afternoon? J Hum Hypertens. 1996;10:287–292. [PubMed] [Google Scholar]
- 15. Kario K, Pickering T, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–1406. [DOI] [PubMed] [Google Scholar]
- 16. Gosse P, Shumacher H, Lacouriciere Y, et al. Effect of patient characteristics on the magnitude of the early morning blood pressure surge [abstract]. J Hypertens. 2006;24(suppl 4):S301. [Google Scholar]
- 17. Pasic J, Shapiro D, Motivala S, et al. Blood pressure morning surge and hostility. Am J Hypertens. 1998;11:245–250. [DOI] [PubMed] [Google Scholar]
- 18. Mulcahy D, Keegan J, Cunningham D, et al. Circadian variation of total ischaemic burden and its alteration with anti anginal agents. Lancet. 1988;2:755–759. [DOI] [PubMed] [Google Scholar]
- 19. Behar S, Reicher‐Reiss H, Goldbourt U, et al. Circadian variation in pain onset in unstable angina pectoris. Am J Cardiol. 1991;67:91–93. [DOI] [PubMed] [Google Scholar]
- 20. Argentino C, Toni D, Rasura M, et al. Circadian variation in the frequency of stroke. Stroke. 1990;21:387–389. [DOI] [PubMed] [Google Scholar]
- 21. Marler JR, Price TR, Clark GL, et al. Morning increase in onset of ischemic stroke. Stroke. 1989;20:473–476. [DOI] [PubMed] [Google Scholar]
- 22. Sloan MA, Price TR, Foulkes MA, et al. Circadian rhythmicity of stroke onset. Intracerebral and subarachnoid hemorrhage. Stroke. 1992;23:1420–1426. [DOI] [PubMed] [Google Scholar]
- 23. Vermeer SE, Rinkel GJ, Algra A. Circadian fluctuations in onset of subarachnoid hemorrhage. New data on aneurysmal and perimesencephalic hemorrhage and a systematic review. Stroke. 1997;28:805–808. [DOI] [PubMed] [Google Scholar]
- 24. Stergiou GS, Vemmos KN, Pliarchopoulou KM, et al. Parallel morning and evening surge in stroke onset, blood pressure, and physical activity. Stroke. 2002;33:1480–1486. [DOI] [PubMed] [Google Scholar]
- 25. Muller JE, Stone PH, Turi ZG, et al. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985;31:1315–1322. [DOI] [PubMed] [Google Scholar]
- 26. Willich SN, Goldberg RJ, Maclure M, et al. Increased onset of sudden cardiac death in the first three hours after awakening. Am J Cardiol. 1992;70:65–68. [DOI] [PubMed] [Google Scholar]
- 27. Elliot WJ. Cyclic and circadian variations in cardiovascular events. Am J Hypertens. 2001;14:291S–295S. [DOI] [PubMed] [Google Scholar]
- 28. Bursztyn M, Ginsberg G, Hammerman‐Rozenberg R, et al. The siesta in the elderly: risk factor for mortality? Arch Intern Med. 1999;159:1582–1586. [DOI] [PubMed] [Google Scholar]
- 29. Bursztyn M, Ginsberg G, Stessman J. The siesta and mortality in the elderly: effects of rest without sleep and daytime sleep duration. Sleep. 2002;25:187–191. [DOI] [PubMed] [Google Scholar]
- 30. Murakami S, Otsuka K, Kubo Y, et al. Repeated ambulatory monitoring reveals a Monday morning surge in blood pressure in a community‐dwelling population. Am J Hypertens. 2004;17(12 part 1):1179–1183. [DOI] [PubMed] [Google Scholar]
- 31. Furlan R, Guzzetti S, Crivellaro W, et al. Continuous 24‐hour assessment of the neural regulation of systemic arterial pressure and RR variabilities in ambulant subjects. Circulation. 1990;81:537–547. [DOI] [PubMed] [Google Scholar]
- 32. Panza JA, Epstein SE, Quyyumi AA. Circadian variation in vascular tone and its relation to alpha‐sympathetic vasoconstrictor activity. N Engl J Med. 1991;325:986–990. [DOI] [PubMed] [Google Scholar]
- 33. Dodt C, Breckling U, Derad I, et al. Plasma epinephrine and norepinephrine concentrations of healthy humans associated with nighttime sleep and morning arousal. Hypertension. 1997;30:71–76. [DOI] [PubMed] [Google Scholar]
- 34. Schofl C, Becker C, Prank K, et al. Twenty‐four‐hour rhythms of plasma catecholamines and their relation to cardiovascular parameters in healthy young men. Eur J Endocrinol. 1997;137:675–683. [DOI] [PubMed] [Google Scholar]
- 35. Oshchepkova EV, Lazareva NV, Filatova LV, et al. Morning rise of systolic blood pressure (by 24‐hour ambulatory monitoring) and platelet aggregability in essential hypertension patients [in Russian]. Ter Arkh. 2000;72:47–51. [PubMed] [Google Scholar]
- 36. Etsuda H, Takase B, Uehata A, et al. Morning attenuation of endothelium‐dependent, flow‐mediated dilation in healthy young men: possible connection to morning peak of cardiac events? Clin Cardiol. 1999;22:417–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Otto ME, Svatikova A, Barretto RB, et al. Early morning attenuation of endothelial function in healthy humans. Circulation. 2004;109:2507–2510. [DOI] [PubMed] [Google Scholar]
- 38. Drayer JI, Weber MA, DeYoung JL. BP as a determinant of cardiac left ventricular muscle mass. Arch Intern Med. 1983;143:90–92. [PubMed] [Google Scholar]
- 39. Gosse P, Ansoborlo P, Lemetayer P, et al. Left ventricular mass is better correlated with arising blood pressure than with office or occasional blood pressure. Am J Hypertens. 1997;10:505–510. [DOI] [PubMed] [Google Scholar]
- 40. Kuwajima I, Mitani K, Miyao M, et al. Cardiac implications of the morning surge in blood pressure in elderly hypertensive patients: relation to arising time. Am J Hypertens. 1995;8:29–33. [DOI] [PubMed] [Google Scholar]
- 41. Ikeda T, Gomi T, Shibuya Y, et al. Morning rise in blood pressure is a predictor of left ventricular hypertrophy in treated hypertensive patients. Hypertens Res. 2004;27:939–946. [DOI] [PubMed] [Google Scholar]
- 42. Polonia J, Amado P, Barbosa L, et al. Morning rise, morning surge and daytime variability of blood pressure and cardiovascular target organ damage. A cross‐sectional study in 743 subjects. Rev Port Cardiol. 2005;24:65–78. [PubMed] [Google Scholar]
- 43. Marfella R, Siniscalchi M, Nappo F, et al. Regression of carotid atherosclerosis by control of morning blood pressure peak in newly diagnosed hypertensive patients. Am J Hypertens. 2005;18:308–318. [DOI] [PubMed] [Google Scholar]
- 44. Zakopoulos NA, Tsivgoulis G, Barlas G, et al. Time rate of blood pressure variation is associated with increased common carotid artery intima‐media thickness. Hypertension. 2005;45:505–512. [DOI] [PubMed] [Google Scholar]
- 45. Gosse P, Cipriano C, Bemurat L, et al. Prognostic significance of blood pressure measured on rising. J Hum Hypertens. 2001;15:413–417. [DOI] [PubMed] [Google Scholar]
- 46. White WB. Ambulatory blood pressure monitoring: dippers compared with non‐dippers. Blood Press Monit. 2000;5(suppl 1):S17–S23. [PubMed] [Google Scholar]
- 47. Fogari R, Malacco E, Tettamanti F, et al. Evening vs morning isradipine sustained release in essential hypertension: a double‐blind study with 24 h ambulatory monitoring. Br J Clin Pharmacol. 1993;35:51–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nold G, Strobel G, Lemmer B. Morning versus evening amlodipine treatment: effect on circadian blood pressure profile in essential hypertensive patients. Blood Press Monit. 1998;3:17–25. [PubMed] [Google Scholar]
- 49. White WB, Mansoor GA, Pickering TG, et al. Differential effects of morning and evening dosing of nisoldipine ER on circadian blood pressure and heart rate. Am J Hypertens. 1999;12(8 pt 1):806–814. [DOI] [PubMed] [Google Scholar]
- 50. Hermida RC, Calvo C, Ayala DE, et al. Administration time‐dependent effects of valsartan on ambulatory blood pressure in hypertensive subjects. Hypertension. 2003;42:283–290. [DOI] [PubMed] [Google Scholar]
- 51. Glasser SP, Neutel JM, Gana TJ, et al. Efficacy and safety of a once daily graded‐release diltiazem formulation in essential hypertension. Am J Hypertens. 2003;16:51–58. [DOI] [PubMed] [Google Scholar]
- 52. Kuroda T, Kario K, Hoshide S, et al. Effects of bedtime vs. morning administration of the long‐acting lipophilic angiotensin‐converting enzyme inhibitor trandolapril on morning blood pressure in hypertensive patients. Hypertens Res. 2004;27:15–20. [DOI] [PubMed] [Google Scholar]
- 53. Kitahara Y, Saito F, Akao M, et al. Effect of morning and bedtime dosing with cilnidipine on blood pressure, heart rate, and sympathetic nervous activity in essential hypertensive patients. J Cardiovasc Pharmacol. 2004;43:68–73. [DOI] [PubMed] [Google Scholar]
- 54. Ishimitsu T, Minami J, Kawano Y, et al. Amlodipine, a long‐acting calcium channel blocker, attenuates morning blood pressure rise in hypertensive patients. Clin Exp Pharmacol Physiol. 1999;26:500–504. [DOI] [PubMed] [Google Scholar]
- 55. Eguchi K, Kario K, Shimada K. Comparison of candesartan with lisinopril on ambulatory blood pressure and morning surge in patients with systemic hypertension. Am J Cardiol. 2003;92:621–624. [DOI] [PubMed] [Google Scholar]
- 56. White WB, Weber MA, Davidai G, et al. Ambulatory blood pressure monitoring in the primary care setting: assessment of therapy on the circadian variation of blood pressure from the MICCAT‐2 Trial. Blood Press Monit. 2005;10:157–163. [DOI] [PubMed] [Google Scholar]
- 57. Gosse P, Neutel J, Schumacher H, et al. Reduction of early morning blood pressure surge with telmisartan compared with ramipril in mild‐to‐moderate hypertensive patients [abstract]. J Hypertens. 2005;23(suppl 2):S375. [Google Scholar]
- 58. Kawano Y, Tochikubo O, Watanabe Y, et al. Doxazosin suppresses the morning increase in blood pressure and sympathetic nervous activity in patients with essential hypertension. Hypertens Res. 1997;20:149–156. [DOI] [PubMed] [Google Scholar]
- 59. Hashimoto J, Chonan K, Aoki Y, et al. Therapeutic effects of evening administration of guanabenz and clonidine on morning hypertension: evaluation using home‐based blood pressure measurements. J Hypertens. 2003;21:805–811. [DOI] [PubMed] [Google Scholar]
- 60. Baumgart P, Rahn KH. Morning rise in blood pressure: before or following awakening? [in German]. Klin Wochenschr. 1990;68:320–323. [DOI] [PubMed] [Google Scholar]
- 61. Kawano H, Ashizawa N, Toda G, et al. Administration of nifedipine CR immediately after awakening prevents a morning surge in hypertensive patients. Case report of three cases. Blood Press Suppl. 2003;1:44–48. [DOI] [PubMed] [Google Scholar]


