Abstract
Cardiovascular abnormalities are frequently the cause, as well as the effect, of elevated blood pressure. As such, early cardiovascular disease (CVD) may be established before identifiable blood pressure thresholds are crossed. To identify individuals at risk for CVD at an earlier point in the disease process, as well as to avoid labeling persons as hypertensive who are at low risk for CVD, the Hypertension Writing Group proposes incorporating the presence or absence of cardiovascular risk factors, early disease markers, and target organ damage into the definition and classification scheme of hypertension. To describe both the complexity and progressive nature of hypertension, the following definition is proposed: “Hypertension is a progressive cardiovascular syndrome arising from complex and interrelated etiologies. Early markers of the syndrome are often present before blood pressure elevation is observed; therefore, hypertension cannot be classified solely by discrete blood pressure thresholds. Progression is strongly associated with functional and structural cardiac and vascular abnormalities that damage the heart, kidneys, brain, vasculature, and other organs and lead to premature morbidity and death.” Classification of hypertension must involve assessing global cardiovascular risk to situate an individual's risk for CVD and events along a continuum. As knowledge of early CVD continues to evolve, the approach to classifying individuals along that continuum can be expected to evolve accordingly. The four categories currently used to classify hypertension are normal, prehypertension, and stages 1 and 2 hypertension. The population identified with prehypertension includes a subgroup with early CVD. We believe it would be preferable to classify all individuals as either normal or hypertensive, based on their cardiovascular evaluation, using the four categories of normal and stages 1, 2, and 3 hypertension.
Currently, hypertension is diagnosed when an individual crosses an established blood pressure (BP) threshold. Hypertension‐related cardiovascular disease (CVD), however, is a complex process that begins before BP values reach levels currently used to define hypertension. This insight is derived primarily from epidemiologic data indicating that the risk of adverse outcomes, including target organ damage and cardiovascular and renal morbidity and mortality, increases linearly at all BP values. 1 , 2 , 3 , 4 , 5 , 6 , 7 The current definition and classification of hypertension, based on the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7), relies primarily on BP thresholds for the diagnosis and treatment of the disorder. The problem with a threshold‐based definition of hypertension is that it fails to identify a large group of individuals who have subclinical CVD that may precede chronic BP elevations.
Definition and classification systems for hypertension have evolved over several decades and will undoubtedly continue to change as we gain additional insight into early CVD. While discrete BP categories have been used consistently in designing clinical trials, promulgating regulatory documents, and gathering epidemiologic data, the incorporation of global cardiovascular risk into the definition of hypertension has proven less consistent. The Hypertension Writing Group (HWG) proposes to expand the current definition and classification of hypertension by integrating additional preclinical and clinical cardiovascular manifestations (Table I). The purpose of this paper is to present the case that to be clinically relevant, the definition and classification of hypertension requires the integration of global cardiovascular risk assessment. Moreover, we believe that in the future, it is likely that BP will be viewed as a continuous risk factor to be considered in the context of total cardiovascular risk.
Table I.
Hypertension Writing Group Definition and Classification of Hypertension*
| Classification | Normal | Stage 1 Hypertension | Stage 2 Hypertension | Stage 3 Hypertension |
|---|---|---|---|---|
| Descriptive category | Normal BP or rare BP | Occasional or | Sustained BP elevations | Marked and sustained BP |
| (BP pattern and | elevations | intermittent BP | OR | elevations |
| CVD status) | AND | elevations | Evidence of progressive | OR |
| No identifiable CVD** | OR | CVD** | Evidence of advanced | |
| Risk factors or markers | CVD** | |||
| suggesting early CVD** | ||||
| Cardiovascular risk | None | ≥1 risk factor present | Multiple risk factors | Multiple risk factors |
| factors | present | present | ||
| (see Table II) | ||||
| Early disease markers | None | 0–1 | ≥2 | ≥2 present with evidence |
| (see Table III) | of CVD | |||
| Target organ disease | None | None | Early signs present | Overtly present with or |
| (see Table IV) | without CVD events | |||
| *This paradigm expands on the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) definition and classification of hypertension by classifying individuals by blood pressure (BP) level or cardiovascular status; however, priority is given to cardiovascular status; **cardiovascular disease (CVD) designation is determined by the constellation of risk factors, early disease markers, and target organ disease as listed in Tables II–IV. BP categories are shown in the Figure. | ||||
Improving clinical care for individuals with hypertension involves the coordination of two simultaneous goals: lowering BP and protecting the heart, vasculature, and target organs. By expanding the definition of hypertension to include other markers of cardiovascular status, we call attention to the enormous unmet need regarding the optimal prevention and treatment of this ubiquitous disorder. This change in focus is necessary and has important implications for research, drug development, public health efforts, patient education, and clinical management.
BP AND CVD RISK
The Dynamic Nature of BP
The body's ability to regulate BP is a complex, moment‐to‐moment hemodynamic activity that attempts to match tissue perfusion with metabolic demands. Circulatory responses and BP homeostasis directly depend on the coordinated activity and a balance of many interacting BP control mechanisms—in particular, the sympathetic nervous system, the renin‐angiotensin‐aldosterone system, and the vasodilatory system (e.g., prostaglandins and nitric oxide) as well as the kidney itself.
In effect, optimal arterial BP provides sufficient force to maintain circulation without causing damage to the heart and vasculature. Optimal BP may vary among different individuals and in the same person according to circumstances; correspondingly, chronic BP levels above optimal for an individual are those levels that may cause damage to the vasculature. Typically, a rise in resting BP above optimal levels is a sign of inappropriately increased vascular tone or stiffness, which may be aggravated by chronic structural remodeling of the large or small arteries.
Whereas BP is dynamic and variable, clinic BP measurements tend to be more static in nature. Thus, it is helpful to consider BP patterns rather than discrete BP thresholds. Serial home measurements under differing conditions provide more information than single measurements; in some cases, ambulatory BP monitoring may be indicated. Hemodynamically, moreover, the information revealed by systolic BP (SBP) or pulse pressure is intrinsically different from that of diastolic BP (DBP) or mean BP. SBP is dependent on cardiac output and the degree of stiffness of the large central arteries; DBP is closely related to the state of constriction of small blood vessels. 8 The rise in SBP typically associated with aging generally occurs as a response to progressive stiffening of the large arteries (arteriosclerosis); these SBP elevations often result in a widened pulse pressure. In individuals older than 50, elevated SBP and widened pulse pressure are recognized as more important markers of CVD than elevated DBP. 9 , 10 , 11
CVD Risk Factors
High BP is one of several interacting risk factors that contribute to premature CVD. The importance of risk factors other than elevated BP is well described in JNC 7; these risk factors are summarized in Table II. Age and overweight/obesity are the two most important risk factors for the development and progression of hypertension. The metabolic syndrome is a cluster of three or more risk factors—including obesity, insulin resistance, dyslipidemia, and hypertension—that are recognized to further increase the risk of atherosclerotic CVD. 12
Table II.
Cardiovascular Risk Factors
| Increasing age (continuous variable) |
| Elevated blood pressure (≥140/90 mm Hg)* |
| Overweight/obesity (BMI ≥24 kg/m2) |
| Abdominal obesity |
| Waist circumference >40 in for men or >35 in for women* |
| Dyslipidemia |
| Elevated LDL cholesterol (≥130 mg/dL) |
| Low HDL cholesterol (<40 mg/dL for men and <50 mg/dL for women)* |
| Elevated triglycerides (≥150 mg/dL)* |
| Elevated fasting blood glucose (≥100 mg/dL), insulin resistance, or diabetes* |
| Smoking |
| Family history of premature CVD (younger than 50 in men, younger than 60 in women) |
| Sedentary lifestyle |
| Elevated high‐sensitivity C‐reactive protein |
| BMI=body mass index; LDL=low‐density lipoprotein; HDL=high‐density lipoprotein; CVD=cardiovascular disease; *components of the metabolic syndrome 12 |
HIGH BP: A MOVING TARGET
The specified thresholds for defining high BP have been lowered repeatedly since techniques for noninvasive measurement of BP were developed more than a century ago. Since 1977, the National High Blood Pressure Education Program (NHBPEP) has issued seven reports from the JNC, and in each report, there was a significant change toward lower threshold values in the definition and staging of high DBP, high SBP, or both. 11 , 13 , 14 , 15 , 16 , 17 , 18 Prior to 1984, a DBP level >105 mm Hg was the only established criterion for the diagnosis of hypertension. When the third report of the JNC was issued in 1984, 15 “isolated systolic hypertension” was defined as SBP >160 mm Hg. In JNC 7, 11 BP levels <120/80 mm Hg are called “normal” and BP values ≥120/80 mm Hg and <140/90 mm Hg are classified as “prehypertension.” The designation of prehypertension represents a very large population, recently estimated to be as high as 40% among men and 23% among women in the United States. 19 Compared with individuals with BP levels ≥140/90 mm Hg, the relative risk of cardiovascular events occurring in individuals with prehypertension is small; however, the absolute number of cardiovascular events occurring in this sizeable population is actually quite large. 3 , 20 , 21
The term prehypertension was developed primarily to describe early risk for CVD in a large population, but it does not adequately identify the relevant subgroup that is at moderate‐to‐high risk of sustaining cardiovascular events before reaching chronic BP levels ≥140/90 mm Hg. In reality, any single cardiovascular risk factor taken in isolation has limited biologic significance or prognostic value. On one hand, sporadic BP elevations may occur in individuals in the absence of early CVD. This may lead to assigning an illness diagnosis to individuals who are at low risk for CVD. On the other hand, clinic BP levels <140/90 mm Hg may be a contributory factor in individuals who have a stroke or myocardial infarction. This distinction was evident in survival data for the cohort of individuals in the Second National Health and Nutrition Examination Survey (NHANES II) 22 population who met the JNC 7 classification for prehypertension (BP between 120/80 and 139/89 mm Hg and no previous diagnosis of hypertension). Calculated as a survival curve over 12.8 years, individuals with prehypertension at baseline had a significantly increased risk for allcause and cardiovascular mortality compared with individuals with normal BP at baseline. When the data were adjusted for the presence of risk factors, however, mortality was not increased in individuals who had prehypertension without any additional cardiovascular risk factors.
Throughout most of the world today, “high blood pressure” is defined as chronic elevations in BP ≥140/90 mm Hg. There is substantial—but not universal—consensus that for patients with diabetes and chronic kidney disease, BP should be maintained at levels <130/80 mm Hg. 11 , 23 , 24 One proposed strategy that could encompass more individuals with subclinical CVD would be to lower the treatment threshold for all adults to SBP <130 mm Hg or <120 mm Hg. However, any strategy based on BP measurements alone, without considering other signs of cardiovascular risk, is not recommended since it would involve treating a very large number of individuals who are not at significant risk of cardiovascular events. Undoubtedly, a more appropriate and cost‐effective strategy would be to identify those individuals with early hypertensive CVD who have a moderate‐to‐high risk of cardiovascular events. Focusing attention on this group may also shed light on the larger public health concern of preventing hypertension and its devastating consequences.
Although epidemiologic data demonstrate a positive, continuous, and graded relationship between BP and risk of CVD, these data do not help to identify the subgroup of patients with early cardiac and vascular disease—nor is there conclusive evidence that earlier intervention or lower achieved BP levels would lead to improved clinical outcomes. At present, limited data from large‐placebo‐controlled, randomized clinical trials suggest that antihypertensive treatment may confer clinically important benefits to diverse populations at high cardiovascular risk with BP levels <140/90 mm Hg. 25 , 26 , 27 In the Heart Outcomes Prevention Evaluation (HOPE) study, 25 angiotensin‐converting enzyme (ACE) inhibitor‐based treatment compared with a regimen that did not include an ACE inhibitor reduced the incidence of cardiovascular events and death from any cause among more than 9000 high‐risk patients with or without elevated BP (mean BP at entry, 139/79 mm Hg). In the Perindopril Protection Against Recurrent Stroke Study (PROGRESS), 26 treatment with both perindopril and indapamide significantly reduced the risk of recurrent stroke by 43% in more than 6000 patients. In PROGRESS at baseline, most subjects were receiving preventive therapies, including antihypertensive agents, and about half had BP <140/90 mm Hg. In the Comparison of Amlodipine vs. Enalapril to Limit Occurrences of Thrombosis (CAMELOT) study, 27 1991 patients with angiographically documented coronary artery disease and an average baseline BP of 129/78 mm Hg showed a reduced incidence of cardiovascular events by 31% with an amlodipine‐based (10 mg/d) but not an enalapril‐based (20 mg/d) treatment program. Additional investigation of BP‐lowering therapies in high‐risk populations with BP levels <140/90 mm Hg are needed before clinical recommendations can be made.
DEFINITION AND CLASSIFICATION OF HYPERTENSION
Based on the foregoing discussion, HWG has developed the following definition of hypertension:
Hypertension is a progressive cardiovascular syndrome arising from complex and interrelated etiologies. Early markers of the syndrome are often present before blood pressure elevation is observed; therefore, hypertension cannot be classified solely by discrete blood pressure thresholds. Progression is strongly associated with functional and structural cardiac and vascular abnormalities that damage the heart, kidneys, brain, vasculature, and other organs, and lead to premature morbidity and death.
The four categories currently used to classify hypertension in JNC 7 are normal, prehypertension, and stages 1 and 2 hypertension. We propose instead to classify patients as either normal or hypertensive, as determined by their cardiovascular risk profile. The progression of hypertension—from early to progressive to advanced—may be best represented as stages 1, 2, and 3 hypertension. Each stage of hypertension is described by BP patterns and the presence or absence of cardiovascular risk factors, early markers of hypertensive CVD, and target organ damage.
Our classification amplifies the JNC 7 definition, as shown in the Figure and Table I. In contrast to the JNC 7 definition, we afford even greater priority to risk factors and early markers of CVD, target organ damage, and overt CVD than to observed BP patterns. These four categories are further described in the following pages.
Figure.
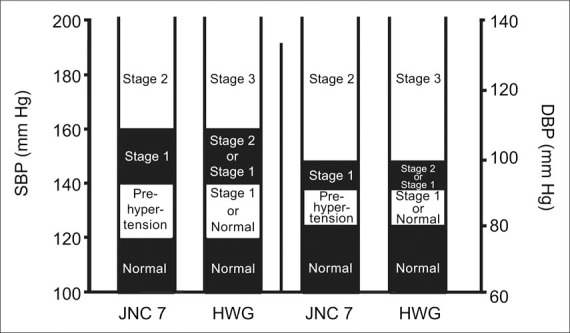
The evolution of blood pressure categories from those proposed in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) 11 to those proposed by the Hypertension Writing Group (HWG). As a result, individuals classified as having prehypertension using JNC 7 are reclassified as having normal or stage 1 hypertension, people classified as having stage 1 hypertension are reclassified as having stage 1 or 2 hypertension, and people classified as having stage 2 hypertension are reclassified as having stage 3 hypertension. In addition, blood pressure levels are considered only one criterion used to classify persons with hypertension; classification also considers cardiovascular status (as shown in Table I ). SBP=systolic blood pressure; DBP=diastolic blood pressure
HWG Normal
Individuals without hypertension have no cardiovascular risk factors (Table II), identifiable early markers (Table III), or target organ damage (Table IV). Their resting BP levels are usually <120/80 mm Hg; however, occasional higher BP levels (even ≥140/90 mm Hg) may occur in these individuals. Some individuals designated as having prehypertension by JNC 7 will be classified as normal in this paradigm.
Table III.
Early Markers of Hypertensive Cardiovascular Disease*
| System | Physiologic Alteration |
|---|---|
| Blood | Loss of nocturnal blood pressure dipping |
| pressure | Exaggerated blood pressure responses to exercise |
| Salt sensitivity | |
| Widened pulse pressure | |
| Cardiac | Left ventricular hypertrophy (mild) |
| Increased atrial filling pressure | |
| Decreased diastolic relaxation | |
| Vascular | Increased central arterial stiffness or pulse wave velocity |
| Small artery stiffness | |
| Increased systemic vascular resistance | |
| Increased wave reflection and systolic pressure augmentation | |
| Increased carotid intima‐media thickness | |
| Coronary calcification | |
| Endothelial dysfunction | |
| Renal | Microalbuminuria (urinary albumin excretion of 30–300 mg/d) |
| Elevated serum creatinine | |
| Reduced estimated glomerular filtration rate (60–90 mL/min) | |
| Retinal | Hypertensive retinal changes |
| *Some of these abnormalities may arise due to factors other than hypertension, e.g., heart failure may be present due to or valvular disease. | |
Table IV.
Hypertensive Target Organ Damage and Overt Cardiovascular Disease
| System | Evidence of Target Organ Damage and Cardiovascular Disease |
|---|---|
| Cardiac | Left ventricular hypertrophy (moderate to severe) |
| Systolic or diastolic cardiac dysfunction | |
| Symptomatic heart failure | |
| Myocardial infarction | |
| Angina pectoris | |
| Ischemic heart disease or prior revascularization | |
| Vascular | Peripheral arterial disease |
| Carotid arterial disease | |
| Aortic aneurysm | |
| Wide pulse pressure (>65 mm Hg) | |
| Renal | Albuminuria (urinary albumin excretion >300 mg/d) |
| Chronic kidney disease (estimated GFR <60 mL/min) or ESRD | |
| Cerebrovascular | Stroke |
| Transient ischemic attack | |
| GFR=glomerular filtration rate; ESRD=end‐stage renal disease | |
HWG Stage 1 Hypertension: Characterized by Global Risk Factors and Early CVD Markers
HWG stage 1 hypertension includes the subgroup of individuals with JNC 7 prehypertension who also exhibit cardiovascular risk factors (Table II) or early disease markers (Table III), but who do not show any evidence of target organ damage (Table IV). This is the earliest identifiable stage of hypertensive disease and generally arises from circulatory, vascular, or renal adaptations to environmental or genetic stimuli. This stage is often characterized by early signs of functional or structural changes in the heart and small arteries. BP levels are usually between 120/80 and 139/89 mm Hg; however, BP values ≥140/90 mm Hg may be occasionally or intermittently observed.
A large percentage of individuals with persistent resting BP levels between 120/80 and 139/89 mm Hg and who have one or more traditional risk factors for CVD have a very high lifetime risk of eventually developing sustained BP levels ≥140/90 mm Hg. 28 Several tools have been developed that can identify individuals in this group who are at moderate or high cardiovascular risk. 29 , 30 , 31 , 32 , 33 For example, the Framingham Heart Study risk equation 33 estimates the CVD risk over 5 years based on seven risk factors—age, sex, SBP, total cholesterol, high‐density lipoprotein cholesterol, smoking, and diabetes. When several risk factors are present, they interact to greatly increase the risk of cardiovascular and renal disease. At present, our best strategy in this population is to: 1) assess for the presence of risk factors listed in Table II (although the role of high‐sensitivity C‐reactive protein is still evolving); 2) initiate comprehensive treatment for those diagnosed with dyslipidemia or diabetes; and 3) suggest lifestyle changes for modifiable risk factors such as smoking, overweight, and inactivity. In addition to persons with diabetes and renal disease, it is reasonable to assume that other high‐risk individuals may benefit at this stage from antihypertensive therapies, although further investigation is needed before comprehensive clinical recommendations can be made.
Identifying hypertension in persons with highrisk profiles but with BP levels <140/90 mm Hg offers the advantage of helping both providers and patients to recognize that a disease state already exists. Moreover, without designating these individuals as hypertensive, it is less likely that appropriate investigation and intervention trials will be undertaken. HWG stage 1 hypertension is a critical stage to investigate on two fronts: first, to bring into the clinic setting specific and sensitive cost‐effective tests that can detect early CVD markers (Table III) and second, to determine whether early vascular derangements can be attenuated or reversed before the onset of target organ damage or overt CVD. Clinical trials should be designed to determine whether treatments to lower BP or prevent BP increases will slow the progression of CVD in people with HWG stage 1 hypertension.
HWG Stage 2 Hypertension: Characterized by Diffuse Disease Markers
Individuals with HWG stage 2 hypertension (JNC 7 stage 1 hypertension) frequently have chronic resting BP levels ≥140/90 mm Hg and may intermittently have much higher BP levels. Individuals with two or more disease markers (Table III) or evidence of early target organ damage such as left ventricular hypertrophy (Table IV) are included in this group regardless of BP levels. Management of HWG stage 2 hypertension is well described. 11
HWG stage 2 hypertension indicates that progressive disease has developed as a consequence of persistent functional and structural changes in BP control mechanisms and in the heart and vasculature. Some of the early target organ damage characteristic of this stage of hypertension can be detected with specialized or research studies, which should be evaluated further to determine their potential utility and cost effectiveness in clinical settings. Risk factors that are associated with HWG stage 2 hypertension, if not attenuated, continue to contribute to progressive target organ disease.
HWG Stage 3 Hypertension: Overt CVD
Untreated individuals with HWG stage 3 hypertension (JNC 7 stage 2 hypertension) usually have chronic resting BP levels ≥140/90 mm Hg; marked elevations to levels >160/100 mm Hg are not uncommon. These BP levels may also be present in hypertensive individuals who are not adequately treated. All individuals with clinical evidence of overt target organ damage (Table IV) or CVD are included in this category, as well as those who have already sustained cardiovascular events.
HWG stage 3 hypertension is an advanced stage of the hypertensive continuum in which overt target organ disease is often pervasive and cardiovascular events may have already occurred. Aging and the persistence of other identifiable risk factors continue to exacerbate the risk of morbidity and mortality. While management strategies for this phase of hypertension are well described, 11 reaching this stage means that damage to target organs as well as overt cardiorenal disease has already occurred. Antihypertensive treatments are highly recommended in this group, regardless of BP levels (e.g., in patients with heart failure, postmyocardial infarction, poststroke, and those with proteinuria). Evaluation and appropriate treatments for all identified CVDs should be maintained, and efforts to attenuate any modifiable risk factors should be continued.
IMPLICATIONS FOR CLINICAL PRACTICE
This clinical paradigm offers a more risk‐based approach to identifying those individuals with any level of BP who have a reasonable likelihood of developing future cardiovascular events. By utilizing global cardiovascular risk, including BP levels, to classify individuals along the continuum of hypertension, we propose to reclassify individuals currently described as prehypertensive as either normal or as having stage 1 hypertension. This will immediately assist both providers and patients in offering sufficient criteria to determine which patients are normal and which have early hypertensive CVD. Defining hypertension as a complex cardiovascular disorder associated with, but not exclusively defined by, high BP levels is a transitional strategy that is intended to pave the way for further research and clinical investigations aimed at detecting and treating disease at an earlier phase.
Although recommendations for antihypertensive treatments have been promulgated for some highrisk patients without BP levels ≥140/90 mm Hg (i.e., those with diabetes and renal disease), major clinical recommendations for treating the very large population with stage 1 hypertension must await results from clinical investigations that use this classification scheme. To date, one large‐scale, randomized clinical trial for the treatment of individuals with HWG stage 1 hypertension (high‐risk patients with BP levels <140/90 mm Hg) is underway. 34 The efficacy of lifestyle changes must also be evaluated in this population. In addition, further investigations are needed to validate the reliability and utility of early disease markers and to establish their cost effectiveness for clinical practice.
References
- 1. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA. 1996;275:1571–1576. [PubMed] [Google Scholar]
- 2. Klag MJ, Whelton PK, Randall BL, et al. Blood pressure and end‐stage renal disease in men. N Engl J Med. 1996;334:13–18. [DOI] [PubMed] [Google Scholar]
- 3. Vasan RS, Larson MG, Leip EP, et al. Impact of high‐normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291–1297. [DOI] [PubMed] [Google Scholar]
- 4. Lewington S, Clarke R, Qizilbash N, et al, for the Prospective Studies Collaboration. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 5. Fesler P, Du Cailar G, Ribstein J, et al. Heterogeneity of cardiorenal characteristics in normotensive subjects. Hypertension. 2004;43:219–223. [DOI] [PubMed] [Google Scholar]
- 6. Sarnak MJ, Greene T, Wang X, et al. The effect of a lower target blood pressure on the progression of kidney disease: long‐term follow‐up of the Modification of Diet in Renal Disease study. Ann Intern Med. 2005;142:342–351. [DOI] [PubMed] [Google Scholar]
- 7. Jackson R, Lawes CM, Bennett DA, et al. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual's absolute cardiovascular risk. Lancet. 2005;365:434–441. [DOI] [PubMed] [Google Scholar]
- 8. Izzo JL Jr. Arterial stiffness and the systolic hypertension syndrome. Curr Opin Cardiol. 2004;19:341–352. [DOI] [PubMed] [Google Scholar]
- 9. Franklin SS, Khan SA, Wong ND, et al. Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham Heart Study. Circulation. 1999;100:354–360. [DOI] [PubMed] [Google Scholar]
- 10. Izzo JL Jr, Levy D, Black HR. Clinical advisory statement: importance of systolic blood pressure in older Americans. Hypertension. 2000;35:1021–1024. [DOI] [PubMed] [Google Scholar]
- 11. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 12. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program. (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 13. Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure . Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure: a cooperative study. JAMA. 1977;237:255–261. [PubMed] [Google Scholar]
- 14. The 1980 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1980;140:1280–1285. [PubMed] [Google Scholar]
- 15. The 1984 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1984;144:1045–1057. [PubMed] [Google Scholar]
- 16. The 1988 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1988;148:1023–1038. [PubMed] [Google Scholar]
- 17. The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153:154–183. [PubMed] [Google Scholar]
- 18. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–2446. [DOI] [PubMed] [Google Scholar]
- 19. Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164:2126–2134. [DOI] [PubMed] [Google Scholar]
- 20. Cohn JN. Arteries, myocardium, blood pressure and cardiovascular risk: towards a revised definition of hypertension. J Hypertens. 1998;16(12 pt 2):2117–2124. [PubMed] [Google Scholar]
- 21. Neaton JD, Wentworth D, for the Multiple Risk Factor Intervention Trial Research Group. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Arch Intern Med. 1992;152:56–64. [PubMed] [Google Scholar]
- 22. Mainous AG III, Everett CJ, Liszka H, et al. Prehypertension and mortality in a nationally representative cohort. Am J Cardiol. 2004;94:1496–1500. [DOI] [PubMed] [Google Scholar]
- 23. Kidney Disease Outcomes Quality Initiative (K/DOQI) . K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1–S290. [PubMed] [Google Scholar]
- 24. American Diabetes Association . Hypertension management in adults with diabetes. Diabetes Care. 2004;27:S65–S67. [DOI] [PubMed] [Google Scholar]
- 25. The Heart Outcomes Prevention Evaluation Study Investigators . Effects of an angiotensin‐converting‐ enzyme inhibitor, ramipril, on cardiovascular events in high‐risk patients. N Engl J Med. 2000;342:145–153. [DOI] [PubMed] [Google Scholar]
- 26. PROGRESS Collaborative Group . Randomised trial of a perindopril‐based blood‐pressure‐lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001; 358:1033–1041. [DOI] [PubMed] [Google Scholar]
- 27. Nissen SE, Tuzcu EM, Libby P, et al, for the CAMELOT Investigators. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure. The CAMELOT study: a randomized controlled trial. JAMA. 2004;292:2217–2225. [DOI] [PubMed] [Google Scholar]
- 28. Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle‐aged women and men: the Framingham Heart Study. JAMA. 2002;287:1003–1010. [DOI] [PubMed] [Google Scholar]
- 29. Wilson PWF, D'Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. [DOI] [PubMed] [Google Scholar]
- 30. Voss R, Cullen P, Schulte H, et al. Prediction of risk of coronary events in middle‐aged men in the Prospective Cardiovascular Múnster Study (PROCAM) using neural networks. Int J Epidemiol. 2002;31:1253–1262. [DOI] [PubMed] [Google Scholar]
- 31. Conroy RM, Pyöráälä K, Fitzgerald AP, et al, on behalf of the SCORE project group. Estimation of ten‐year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. [DOI] [PubMed] [Google Scholar]
- 32. de Visser CL, Bilo HJ, Thomsen TF, et al. Prediction of coronary heart disease: a comparison between the Copenhagen risk score and the Framingham risk score applied to a Dutch population. J Intern Med. 2003;253:553–562. [DOI] [PubMed] [Google Scholar]
- 33. Grundy SM, Pasternak R, Greenland P, et al. AHA/ACC scientific statement: assessment of cardiovascular risk by use of multiple‐risk‐factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. J Am Coll Cardiol. 1999;34:1348–1359. [DOI] [PubMed] [Google Scholar]
- 34. Julius S, Nesbitt S, Egan B, et al, for the TROPHY study group. Trial of preventing hypertension: design and 2‐year progress report. Hypertension. 2004;44:146–151. [DOI] [PubMed] [Google Scholar]


