Abstract
Epidemiologic evidence indicates that African Americans are at greater risk for hypertension compared with other ethnic groups in the United States. The prevalence of hypertension is estimated to be approximately 37% for this group, compared with 20%–25% for non‐Hispanic whites. Hypertension seems to follow a more malignant course in African Americans, possibly as a result of the higher prevalence of concomitant cardiovascular risk factors in this population. Compared with white persons with hypertension, these patients are at increased risk for left ventricular hypertrophy, heart failure, and end‐stage renal disease. Data suggest that ethnicity may influence the response to certain types of antihypertensive medication. Additional data indicate that more aggressive use of combination therapy may improve clinical outcomes among high‐risk hypertensive patients. Based on these findings, recommendations are made for the optimal clinical management of hypertension in African‐American patients.
Epidemiologic studies indicate that diastolic blood pressure (DBP) and systolic blood pressures (SBP) are positively correlated with the risk of cardiovascular (CV) events and renal failure. 1 , 2 , 3 Furthermore, these data suggest that blood pressure (BP) averaged over the course of many years is a more valuable predictor of CV risk than any single point in time BP measurement. 3
Although the etiological basis of hypertension remains unclear, the mechanisms by which this disorder contributes to the development of cardiovascular disease (CVD) are becoming increasingly well characterized. Briefly, endothelial dysfunction is thought to underlie hypertension and other CV risk factors. 4 Most importantly, endothelial dysfunction is accompanied by a decrease in nitric oxide bioavailability with resultant impairment in vasodilatory ability. 4 Alterations in the arterial wall and autonomic function precede the onset of disease. 5 If elevated BP persists, structural changes occur in the left ventricle and blood vessels, with increased amounts of collagen being laid down and stiffening of the ventricular wall. 6 Left ventricular hypertrophy or changes in ventricular chamber geometry develop, with ensuing changes in diastolic and systolic ventricular function, left atrial enlargement, decreased atrial contraction, and finally heart failure. 7 Understanding the etiologic causation of hypertension provides insight to how health care providers can properly manage patients, especially those at higher risk, like African Americans.
HEART DISEASE IN AFRICAN AMERICANS
Morbidity and mortality due to hypertension and hypertension‐related disorders are clearly more common among African Americans than among whites or other ethnic groups (Table I). 8 , 9 , 10 In part, this disparity may be attributable to differences among ethnic groups in the natural history of hypertension. Data from the 1999–2000 National Health and Nutrition Examination Survey (NHANES) indicate that the prevalence of hypertension is approximately 33.5% in African Americans and approximately 29% in non‐Hispanic whites. 11 Moreover, hypertension emerges earlier among African‐Americans than in non‐Hispanic whites; 29.5% of African‐American men between the ages of 35 and 44 years have hypertension, compared with only 14.3% of white men of the same age. 8
Table I.
Hypertension‐Related Epidemiology, Morbidity, and Mortality in African Americans*
| Epidemiology |
| Hypertension |
| Affects 37% of all African Americans |
| Develops at an earlier age |
| More often severe |
| Higher prevalence of multiple cardiovascular |
| disease risk factors |
| Obesity |
| Inactivity |
| Dyslipidemia |
| African American status predictor of lack of |
| awareness of hypertensive condition |
| More frequent left ventricular hypertrophy |
| Morbidity |
| 32% of African Americans have treated, but |
| uncontrolled, hypertension |
| More frequent hospitalization for heart failure |
| 1.3 times more frequent nonfatal stroke |
| 4.2 times more frequent end‐stage renal disease |
| Begin dialysis at an earlier age |
| Mortality |
| More frequent premature death** from heart |
| disease |
| 1.8 times more frequent fatal stroke |
| Higher rate of hypertension‐related mortality |
| 1.5 times more frequent death from heart disease |
| *Where relevant, in comparison with United States non‐Hispanic whites; **premature death is defined as that occurring at ≤65 years. Sources: 2003 Heart and Stroke Statistical Update. 9 Men and heart disease: an atlas of racial and ethnic disparities in mortality. 10 Am J Hypertens. 2000;13:103–104. 8 Yancy CW. Heart failure in African Americans: a cardiovascular engima. J Card Fail. 2000;6:183–186. |
The high prevalence of additional risk factors for CVD may contribute to the more severe course of hypertension in African Americans (Table I). 9 Epidemiologic studies have demonstrated that the interaction of multiple CV risk factors, such as hypertension, dyslipidemia, obesity, and diabetes, results in multiplicative, rather than merely additive, increases in global CV risk. 12
The high incidence of hypertension‐related disease among African Americans illustrates the impact of this confluence of risk factors. African Americans are more frequently hospitalized for heart failure 13 and have a higher prevalence of left ventricular hypertrophy than whites. 14 Moreover, they have a higher incidence of end‐stage renal disease (ESRD) 15 and require dialysis for ESRD at a substantially younger median age than whites (57 and 67 years, respectively) (Table I). 16
The incidence of death due to CVD in African‐American men aged ≤65 years is almost double that of non‐Hispanic white men (40% vs. 21%, respectively). An even greater disparity is observed between African‐American women and white women (22% vs. 8%, respectively). 10 , 17 Regardless of age, persons in this group die from heart disease 1.5 times more often than whites. 9 Moreover, there are profound differences in the incidence of CVD subcategories (Table I). For example, death is most often attributable to ischemic heart disease in white men; however, hypertension occurs more often in African‐American men. 10
THE PHARMACOLOGIC MANAGEMENT OF HYPERTENSION IN AFRICAN AMERICANS: CLINICAL EVIDENCE
Results from recently completed clinical trials that enrolled significant numbers of African Americans provide valuable data on which to base treatment decisions and form the foundation of the seventh iteration of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC) guidelines and enlarge the recommendations of the JNC VI report. 18 Together, the JNC 7 guidelines 19 and the trials reviewed here provide the information necessary to make evidence‐based treatment recommendations.
The Heart Outcomes Prevention Evaluation (HOPE) Study
The results of HOPE study highlight the influence of the renin‐angiotensin system on hypertension outcomes. 20 A total of 9297 patients aged ≥55 years with evidence of CVD or diabetes plus one additional CV risk factor were randomized to therapy based on the angiotensin‐converting enzyme (ACE) inhibitor ramipril (10 mg/d) or other medications plus a placebo for a mean of 5 years. Concomitant antihypertensive medication was permitted, if deemed clinically necessary for adequate BP control, as were medications for comorbid CV conditions, such as antiplatelet and hypolipidemic agents. A large majority of patients received at least one to two other medications in both groups of patients. The primary outcome measure was the composite of myocardial infarction, stroke, and death from CVD. Each component of the composite measure was also analyzed separately. Treatment in the ramipril‐based group was associated with a significant 22% reduction in the primary composite outcome measure (Figure 1) and significant reductions in the risks of nonfatal myocardial infarction (20%), stroke (32%), and death from CVD (26%), specific to the diabetic population tested in this cohort. 20 The incidence of new‐onset diabetes was also significantly reduced in the ramipril group (34%). 20 Reductions in risk were observed despite only small differences in BP between groups (2‐3 mm Hg). 20 A small group of patients who were studied with ambulatory BP monitoring did, however, show a greater difference in BP between the two groups of patients. Although modest decreases in BP might account for up to 40% of the reduction in the rate of stroke and 25% of the reduction in the rate of myocardial infarction, the authors argue that the remainder of the benefit may be attributable to additional effects on the heart or the vasculature by the ACE inhibition. Specifically, they suggest that these effects may be related to the beneficial influence of the ACE inhibitor on vasoconstriction, endothelial function, atherosclerotic progression, and left ventricular hypertrophy, among other non‐BP related effects. 20 Importantly, synergistic reductions in CV risk were observed in patients taking concomitant statins, antiplatelet agents, or aspirin. 20
Figure 1.
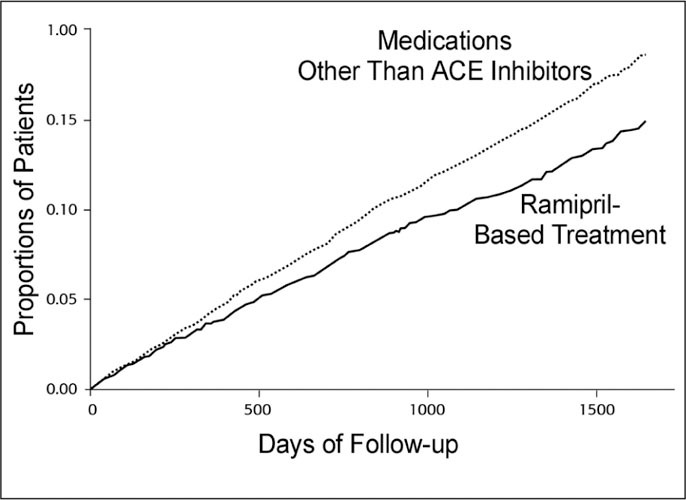
The Heart Outcomes Prevention Evaluation Study: Kaplan‐Meier estimates of composite outcome of myocardial infarction, stroke, or death from cardiovascular causes with ramipril or placebo. Compared with the placebo group, the relative risk of the composite outcome with ramipril was 0.78 (95% confidence interval, 0.70–0.86; p<0.001). Reprinted with permission of the Massachusetts Medical Society from N Engl J Med. 2000;342:145– 153.20
HOPE enrolled few African Americans. The presence of multiple CV risk factors in this patient population, however, may suggest that an ACE inhibitor‐based treatment program may also benefit African Americans, although this has not been demonstrated.
The African American Study of Kidney Disease and Hypertension (AASK)
AASK explicitly examined the impact of several drug classes on the progression of hypertensive renal disease in African Americans. 21 , 22 , 23 AASK enrolled 1094 hypertensive African Americans with mild to moderate renal disease (glomerular filtration rate [GFR] of 20–65 mL/min per 1.73 m 2 ) who were considered at high risk for progressing to hypertensive ESRD. The study used a 3 x 2 factorial design in which patients were randomized to a usual mean arterial pressure target of 102–107 mm Hg (approximately 140/90 mm Hg) or to a low mean arterial pressure target of ≤92 mm Hg (≤25/75 mm Hg), then further randomized to treatment with the sustained‐release βblocker metoprolol, the ACE inhibitor ramipril, or the dihydropyridine calcium channel blocker (CCB) amlodipine. If necessary to achieve BP targets, second‐line antihypertensive agents were added in the following order: furosemide, doxazosin, clonidine, hydralazine, and minoxidil. A large percentage of patients required the use of other agents, especially diuretics, to achieve the goal BPs. The primary outcome measure was the rate of change in GFR; the main secondary outcome measure was the composite of death, ESRD onset, and significant declines in GFR (defined as a ≥50% or ≥25 mL/min per 1.73 m 2 reduction in GFR from baseline).
The 3‐year interim results of AASK were reported in 2001. 21 Among patients with a urinary protein to creatinine ratio of >0.22, the mean rate of decline in GFR was 36% slower in the ramipril group than in the amlodipine‐based treatment patients (p=0.006). Furthermore, the risk of the composite of death, onset of ESRD, and significant decline in GFR was 48 % lower. 21 Based on these results, and additional data showing that protein excretion increased significantly in amlodipine patients with or without baseline proteinuria, the amlodipine arm of the trial was prematurely terminated. The investigators suggest that dihydropyridine CCBs, such as amlodipine, may cause declines in systemic arterial pressure but with concomitant increases in intraglomerular pressure, with pressure‐related glomerular injury that potentially contribute to worsening proteinuria and a more rapid decline in GFR. 21
Additional analysis after 4 years of treatment showed that neither of the two remaining drug groups nor target BP significantly influenced the rate of GFR decline in the overall study population. 23 However, treatment in the ACE inhibitor groups was associated with a significant, 22% lower risk of the composite clinical outcome compared with the combined metoprolol and amlodipine groups (Figure 2). 23 Patients in the metopolol group had a better outcome than the amlodipine patients when specific end points were considered. The rate of GFR decline was also not related to the degree of BP lowering. This finding was of great interest in view of findings from other studies suggesting that a lower BP goal is necessary to achieve benefit in patients with renal disease. Overall, patients enrolled in AASK were successful in achieving BP targets: among patients randomized to the low BP target group, the percentage of patients who achieved a BP <140/90 mm Hg increased from 20.0% at baseline to 78.9% after 14 months of treatment. 22 Among patients randomized to the usual target BP group, the corresponding percentages increased from 21.5% at baseline to 41.8% after 14 months.
Figure 2.
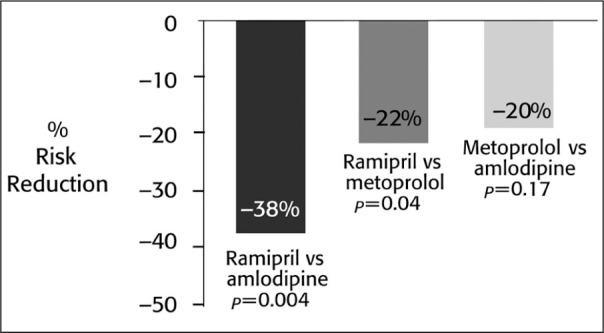
Clinical events in The African American Study of Kidney Disease and Hypertension trial. Data represent reductions in risk of the composite clinical outcomes (glomerular filtration rate declines of ≥50% from baseline or 25 mL/min per 1.73 m2, end‐stage renal disease, or death). Source: JAMA. 2002;288:2421–2431 23
The Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)
ALLHAT enrolled 42,418 patients, of whom approximately 35% were African American. 24 This trial compared the effects of newer antihypertensive regimens, including amlodipine, the peripheral α‐adrenergic blocker doxazosin, and the ACE inhibitor lisinopril, with those of the thiazide‐type diuretic chlorthalidone on the incidence of fatal coronary heart disease and nonfatal myocardial infarction in patients at high risk of a CV event. 24 Secondary end points included all‐cause mortality,stroke, and other coronary heart disease and CVD events. Patients aged ≥55 years with hypertension plus at least one additional CV risk factor were randomized to 8 years of antihypertensive therapy; a subset of moderately hypercholesterolemic participants who were eligible for lipid‐lowering treatment (n=10,355) were further randomized to receive either pravastatin or usual care. 24 Due to an unacceptably large excess of heart failure in the doxazosin‐based arm of the trial compared with the diuretic group, this part of the study was terminated early. 25
Analysis of the primary clinical end points after approximately 5 years of treatment failed to reveal a significant difference between either amlodipine and chlorthalidone or between lisinopril and chlorthalidone. 24 Decreases in SBP were significantly larger with chlorthalidone than with no lisinopril. Differences in both DBP and SBP were less than 2 mm Hg among patients with amlodipine and chlorthalidone. The antihypertensive effects of lisinopril were less than those of chlorthalidone; possibly because of the large numbers of African‐American patients in the study (a difference of 5 mm Hg SBP in these patients between the ACE inhibitor and the diuretic compared with about a 1 mm Hg SBP difference in the white patients.) 24 Differences also emerged among treatments in the frequency of stroke. With chlorthalidone and amlodipine, roughly 5.5% of patients experienced a stroke during follow‐up. In contrast, a significantly greater percentage of patients treated with lisinopril experienced a stroke (6.4%). 24 The difference in the incidence of stroke was largely attributable to a 40% excess risk of stroke in African Americans treated with lisinopril compared with patients on chlorthalidone (Figure 3). 24 A similar pattern was observed in the cumulative frequency of all CVD events (Figure 3). For the study population as a whole, the relative risk of a CVD event was comparable between amlodipine and chlorthalidone, but was greater with lisinopril. The difference in risk of a CVD event associated with lisinopril was particularly apparent in African‐American participants and was not similarly observed in other patients. 24 Compared with chlorthalidone, both amlodipine and lisinopril were associated with significantly greater risks of heart failure than chlorthalidone—this was especially true in the CCB/diuretic comparison. 24
Figure 3.
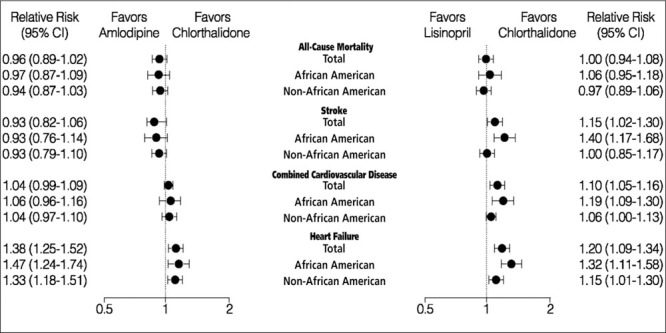
The Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial: relative risk for stroke and combined cardiovascular disease (amlodipine vs. chlorthalidone and lisinopril vs. chlorthalidone). Data shown represent relative risk compared with chlorthalidone; *p=0.01 for interaction; CI=confidence interval Adapted with permission from JAMA. 2002;288:2981–2997.24
The relatively poor secondary outcomes with amlodipine and lisinopril, paired with comparable primary clinical outcomes and significantly better BP control with chlorthalidone, support the JNC 7 recommendation to use diuretics as first‐line antihypertensive treatment. 19
These results of ALLHAT favor the use of chlorthalidone; however, it should be noted that there was a significantly higher frequency of elevated cholesterol levels (>240 mg/dL), decreased potassium levels (<3.5 mg/dL), and elevated fasting blood glucose levels (>126 mg/dL) among patients treated with chlorthalidone compared with the other groups. 24 Outcomes in both diabetic and non‐diabetic patients were similar with benefit noted in the patients in the diuretic group. Although between‐treatment differences in cholesterol and fasting glucose levels might not influence outcomes over the relatively short ALLHAT study period, some investigators speculate that long‐term differences in these parameters might affect CV outcomes.
Smaller Studies in African‐American Patients with Hypertension
Several smaller studies have compared the efficacy of antihypertensive agents in African Americans. 26 , 27 In a short‐term, double‐blind, forced‐titration study, the safety and efficacy of the β blocker atenolol, the ACE inhibitor captopril, and the sustained‐release formulation of the nondihydropyridine CCB verapamil were compared in 345 African‐American patients with moderate hypertension (DBP 95–114 mm Hg). 26 Patients were initially randomized to 4 weeks of therapy with low doses of each antihypertensive. During the second 4‐week treatment phase, half of these patients received a higher dose of the assigned drug, whereas the other half continued at the initial dose. Response to treatment was prospectively defined as a DBP <90 mm Hg or a ≥10 mm Hg reduction in DBP. Decreases in SBP and DBP were greater with verapamil than with the other agents during both treatment periods of the study. 26 At low doses, fewer patients achieved target BPs with captopril than with atenolol or verapamil (44% vs. 55% and 65%, respectively). A significant dose‐related increase in the number of patients responding to therapy was observed with verapamil (low dose, 61%; high dose, 83%), but was not observed for either of the other two treatments. 26 These results were not unexpected in view of abundant data suggesting that a CCB or diuretic is more effective in lowering BP in this population than a β blocker or ACE inhibitor when used as monotherapy.
Compared with white patients, African Americans may require two to four‐fold higher doses of certain antihypertensives to achieve comparable declines in BP. 27 One study compared the antihypertensive efficacy of the ACE inhibitor trandolApril (1 mg/d, 2 mg/d, and 4 mg/d) in 207 white and 91 African‐American patients. While 6 weeks of trandolApril treatment significantly lowered BP in both groups, trandolApril 1 mg/d was sufficient to produce an average 6 mm Hg decrease in sitting DBP in whites, whereas African‐American patients required 4 mg/d to achieve a similar response. 27 Interestingly, laboratory monitoring indicated that decreases in ACE activity at each trandolApril dose were similar between the two groups. These findings add further information that high BP is less responsive to ACE inhibition in African Americans than in whites. 27
IMPLICATIONS FOR THE TREATMENT OF AFRICAN AMERICANS WITH HYPERTENSION
The adequate control of hypertension is an important element in the drive to reduce CV and renal morbidity and mortality in African Americans. A reanalysis of data from NHANES III 28 provides a detailed picture of the current awareness and treatment patterns of hypertension in this population. According to this analysis, a greater percentage of African Americans (32%) than whites (29%) had treated, but uncontrolled, hypertension. 28 Multivariate analysis indicated that race was one of the highly significant predictors for lack of awareness of hypertension. 28 Most of these patients had health insurance and a usual source of care. 28 These findings suggest that untreated or uncontrolled hypertension may be related to factors such as lack of awareness or underuse of available care as well as a tendency to undertreat elevated SBP if it occurs in the presence of a DBP ≤90 mm Hg. 29
Based on findings from HOPE, ALLHAT, AASK, and other key clinical trials, the JNC 7 guidelines recommend lower target BPs and lower thresholds for treatment initiation than earlier guidelines (Table II). 19 These guidelines recommend an initial emphasis on diet and lifestyle changes, including reduction of sodium intake and exercise. 19 Thiazide diuretics are recommended for first‐line antihypertensive therapy, but the guidelines emphasize that the majority of patients require two or more agents to achieve adequate BP control. 19 For higher‐risk patients, such as many African Americans, combination therapy should be considered firstline treatment at a lower BP threshold. In patients at the highest risk of CV events (SBPs & 160 mm Hg or DBP ≥100 mm Hg) or in many patients with diabetes or renal disease, antihypertensive combination therapy should be considered first‐line therapy (Table II). 19 Combination therapy should also be used in patients with uncomplicated hypertension, even in the absence of other prominent CV risk factors, if adequate BP control is not attained with the first‐line agent.
Table II.
Recommendations for Treating African‐American Patients With Hypertension
| Goal blood pressure |
| <140/90 mm Hg or <130/80 for those with |
| diabetes or chronic kidney disease |
| Lifestyle changes |
| Weight loss (use DASH diet) |
| Increase activity |
| Emphasize dietary potassium |
| Patient and family obtain CPR training |
| Pharmacotherapy |
| Diuretic and β blockers as step 1 treatments |
| Begin combination therapy at a lower threshold |
| Uncomplicated cases: 150/100 mm Hg |
| With complications: 145/90 mm Hg |
| One of the drugs should be a diuretic |
| CPR=cardiopulmonary resuscitation; DASH=Dietary Approaches to Stop Hypertension; ESRD=end‐stage renal disease Sources: JAMA. 2003;289:2560–2572 19 ; Douglas JG, Bakris GL, Epstein M, et al. Management of high blood pressure in African Americans: consensus statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med. 2003;163:525–541. |
The more aggressive use of combination therapy is based on findings from the ALLHAT study showing that many patients require multiple antihypertensive agents to achieve adequate BP control. 24 Further research is necessary to determine which antihypertensive drug combinations are most effective, safe, and well tolerated in a variety of clinical situations. Clinical experience indicates that the addition of β blockers to diuretic therapy (or the reverse) or the use of an ACE inhibitor or angiotensin‐receptor blocker with a diuretic provides additional BP reduction. 30 Other combinations, such as pairings of β blockers with ACE inhibitors or CCBs, have not received as much study. Newer agents, such as carvedilol, which exerts dual α‐ and β‐adrenergic blockade, have proved useful when used as monotherapy and may be quite effective when combined with other agents. 31 , 32 Certain advantages are inherent to combination therapy, particularly when the combination is contained within a single formulation. First, the use of two or more antihypertensive agents may result in additive or synergistic reductions in BP. Second, combination therapy may reduce the incidence of dose‐related adverse events by permitting the use of lower doses of each agent. Improved tolerability and ease of administration may, in turn, increase patient compliance and lead to more consistent control of hypertension. 33
CONCLUSIONS
African‐American patients with hypertension present treatment challenges that have not been adequately addressed by previous approaches to antihypertensive therapy. The more severe course of hypertension in these patients, accompanied by the greater likelihood of the presence of multiple CV risk factors, warrants a more aggressive treatment algorithm. Since the publication of JNC VI in 1997, 18 available data have allowed the formulation of more effective management strategies for hypertensive African Americans. The key to appropriate management of this high‐risk patient population is the acceptance of lower target BPs and lower thresholds for the use of combination therapy, and the consideration of combination therapy as a first‐line treatment option in high‐risk patients.
References
- 1. Psaty BM, Furberg CD, Kuller LH, et al. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: the cardiovascular health study. Arch Intern Med. 2001;161:1183–1192. [DOI] [PubMed] [Google Scholar]
- 2. Sesso HD, Stampfer MJ, Rosner B, et al. Systolic and diastolic blood pressure, pulse pressure, and mean arterial pressure as predictors of cardiovascular disease risk in men. Hypertension. 2000;36:801–807. [DOI] [PubMed] [Google Scholar]
- 3. Vasan RS, Massaro JM, Wilson PW, et al. Antecedent blood pressure and risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2002;105:48–53. [DOI] [PubMed] [Google Scholar]
- 4. Vogel RA. Cholesterol lowering and endothelial function. Am J Med. 1999;107:479–487. [DOI] [PubMed] [Google Scholar]
- 5. Zion AS, Bond V, Adams RG, et al. Low arterial compliance in young African American males. Am J Physiol Heart Circ Physiol. In press. [DOI] [PubMed] [Google Scholar]
- 6. Lund‐Johansen P. Evolution of hypertension. In: Messerli FH, eds. ABC's of Anti‐Hypertensive Therapy. Philadelphia, PA: Raven Press; 1994:5–14. [Google Scholar]
- 7. Vasan RS, Levy D. The role of hypertension in the pathogenesis of heart failure. A clinical mechanistic overview. Arch Intern Med. 1996;156:1789–1796. [PubMed] [Google Scholar]
- 8. Wolz M, Cutler J, Roccella EJ, et al. Statement from the National High Blood Pressure Education Program: prevalence of hypertension. Am J Hypertens. 2000;13:103–104. [DOI] [PubMed] [Google Scholar]
- 9. American Heart Association . 2003 Heart and Stroke Statistical Update. Available at: http://www.americanheart.org/statistics. Accessed February 3, 2004.
- 10. Barnett E, Casper ML, Halverson JA, et al. Centers for Disease Control and Prevention. Men and heart disease: an atlas of racial and ethnic disparities in mortality. Available at: http://www.cdc.gov/cvh/mensatlas/index.htm. Accessed February 3, 2004.
- 11. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. [DOI] [PubMed] [Google Scholar]
- 12. Kannel WB. Importance of hypertension as a major risk factor in cardiovascular disease. In: Genest J, Kolw F, Kunchel O, eds. Hypertension: Physiopathology and Treatment. New York, NY: McGraw Hill; 1977:888–910. [Google Scholar]
- 13. Ghali JK, Cooper R, Ford E. Trends in hospitalization rates for heart failure in the United States, 1973–1986. Evidence for increasing population prevalence. Arch Intern Med. 1990;150:769–773. [PubMed] [Google Scholar]
- 14. Afzal A, Ananthasubramaniam K, Sharma N, et al. Racial differences in patients with heart failure. Clin Cardiol. 1999;22:791–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Neal L, Greene EL. Pathophysiology of chronic progressive renal disease in the African American patient with hypertension. Am J Med Sci. 2002;323:72–77. [DOI] [PubMed] [Google Scholar]
- 16. National Institutes of Health . US Renal Data System:USRDS 2001 Annual Data Report. Chapter 1: incidence and prevalence of ERSD. Available at http://www.usrds.org/2001pdf/01.pdf. Accessed February 3, 2004. [Google Scholar]
- 17. Casper ML, Barnett E, Halverson JA, et al. Women and heart disease: an atlas of racial and ethnic disparities in mortality. Available at: http://www.cdc.gov/cvh/womensatlas/index.htm. Accessed February 3, 2004. [PubMed]
- 18. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure . The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–2446. [DOI] [PubMed] [Google Scholar]
- 19. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 20. Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin‐converting enzyme inhibitor, ramipril, on cardiovascular events in high‐risk patients. The Heart Outcomes Prevention Evaluation Study Investigator. N Engl J Med. 2000;342:145–153. [DOI] [PubMed] [Google Scholar]
- 21. Agodoa LY, Appel L, Bakris GL, et al. Effect of ramipril vs amlodipine on renal outcomes in hypertensive nephrosclerosis: a randomized controlled trial. JAMA. 2001;285:2719–2728. [DOI] [PubMed] [Google Scholar]
- 22. Wright JT Jr, Agodoa L, Contreras G, et al. Successful blood pressure control in the African American Study of Kidney Disease and Hypertension. Arch Intern Med. 2002;162:1636–1643. [DOI] [PubMed] [Google Scholar]
- 23. Wright JT, Bakris G, Greene T. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease. Results from the AASK trial. JAMA. 2002;288:2421–2431. [DOI] [PubMed] [Google Scholar]
- 24. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group . Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–2997. [DOI] [PubMed] [Google Scholar]
- 25. Pressel SL, Davis BR, Wright JT, et al. Operational aspects of terminating the doxazosin arm of The Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Control Clin Trials. 2001;22:29–41. [DOI] [PubMed] [Google Scholar]
- 26. Saunders E, Weir MR, Kong BW, et al. A comparison of the efficacy and safety of a beta‐blocker, a calcium channel blocker, and a converting enzyme inhibitor in hypertensive blacks. Arch Intern Med. 1990;150:1707–1713. [PubMed] [Google Scholar]
- 27. Weir MR, Gray JM, Paster R, et al. Differing mechanisms of action of angiotensin‐converting enzyme inhibition in black and white hypertensive patients. The TrandolApril Multicenter Study Group. Hypertension. 1995;26:124–130. [DOI] [PubMed] [Google Scholar]
- 28. Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. [DOI] [PubMed] [Google Scholar]
- 29. Hyman DJ, Pavlik VN, Vallbona C. Physician role in lack of awareness and control of hypertension. J Clin Hypertens (Greenwich). 2000;2:324–330. [PubMed] [Google Scholar]
- 30. Chalmers J, MacMahon S, Mancia G, et al. 1999. World Health Organization‐International Society of Hypertension guidelines for the management of hypertension. Guidelines Sub‐Committee of the World Health Organization. Clin Exp Hypertens. 1999;21:1009–1060. [DOI] [PubMed] [Google Scholar]
- 31. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. US Carvedilol Heart Failure Study Group. N Engl J Med. 1996;334:1349–1355. [DOI] [PubMed] [Google Scholar]
- 32. Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344:1651–1658. [DOI] [PubMed] [Google Scholar]
- 33. Skolnik NS, Beck JD, Clark M. Combination antihypertensive drugs: recommendations for use. Am Fam Physician. 2000;61:3049–3056. [PubMed] [Google Scholar]


