Abstract
There are some common genetic heritages between human and mammals. Human tail, though rare is one of the most noticeable. Till the date, around 60 cases reported in the literature. A true human tail is a benign vestigial caudal cutaneous structure composed of adipose, connective tissue, muscle, vessels and nerves. A true human tail can be distinguished from a pseudotail as the latter is commonly associated with underlying spinal dysraphism, which requires specialised management. We report a case series of four caudal appendages. Two clients were infants, while others two were toddler and presented with cutaneous appendage arising from the lumbosacral region. Out of four, only one had associated spinal dysraphism and neurological manifestation while others did not have spinal dysraphism and neurological manifestation. The appendage was removed by the surgical excision. Clinicians should emphasise the use of ’true tail’ and ’pseudo-tail’ as the specific disparate terms as the clinical, radiological and histological findings of these conditions differs significantly, along with the management strategies and outcomes.
Keywords: Human tail, pseudo-tail, spinal dysraphism, true tail
INTRODUCTION
A human baby having caudal appendage resembling a tail generates an unusual amount of interest, excitement and anxiety.[1] Caudal appendage or human tail is a curious and rare congenital anomaly with a prominent lesion from the lumbosacral region thought to be an evidence of a man's descent from or relation to other animals, while it has been made a subject of superstition. True human tail is a rare event with fewer than 40 cases reported in the literature.[2,3,4] Human tail is probably the most remarkable cutaneous sign of an underlying spinal dysraphism.[5] Sometimes, human tail may not be associated with spinal dysraphism.
Rarity of the case and its interesting presentation led us to report this case.
CASES REPORTS
Case 1
A 5-month-female infant, with uneventful antenatal period had normal vaginal delivery from multipara mother presented with a tail of 16 cm × 3.5 cm at base, tapering towards end at lumbosacral region. Neurological and physical developments were normal for her age. There were no other associated anomalies. All vital parameters including head circumference were normal. At the lumbosacral region, in the midline, a straight 16 cm × 3.5 cm at base, tapering towards end tail was present. Tail was covered by the normal skin. However, no movements of tail were observed [Figure 1a-c]. No bony or cartilaginous element was palpable. Gluteal symmetry was maintained. Spinal magnetic resonance imaging (MRI) was normal (signal intensity equivalent to that of skin and no evidence of neural elements in tail). In prone position under general anaesthesia, a transverse elliptical incision was given around the base of tail. Skin and subcutaneous tissues are dissected. At surgery, there was no evidence of tail leading inward from the appendage. Thoracolumbar fascia was intact. Complete excision was performed. Microscopically, central core contains the lobules of mature adipose tissue separated by septae. Nerve bundles and small vessels were seen within fibroadipose tissue. Post-operative period was uneventful with acceptable cosmetic scar. There is no neurological deficit after 1 year of follow-up. Now, child can walk and have no urinary and faecal incontinence.
Figure 1.

(a-c) True tail caudal appendages (case 1)
Case 2
Two and half years old male child with uneventful antenatal period presented with painless swelling at the lower back which increases in size gradually and have two finger like projection of soft tissue. On examination, soft-tissue mass measure approximately 9 cm × 7 cm and is located at the lumbosacral region at midline. Two fingers such as projections (soft-tissue caudal appendages) present over the mass just above gluteal cleft and fused together at their base [Figure 2a and b]. Gluteal cleft is symmetrical. No bony or cartilaginous element was palpable. Neurological and physical developments were normal for his age. The patient bowel and bladder habit is normal with no urinary and faecal incontinence. There was no limping gait, and lower limb is symmetrical. Other systemic evaluation was normal. Ultrasound of lower back and X-ray lumbosacral spine are normal. However, spinal MRI was not performed due to unaffordability of the patient for MRI. At surgery, the patient was kept prone position. Transverse elliptical incision was given encircling two fingers like projection. There was no evidence of tail leading inward from the appendage and extent superficial to thoracolumbar fascia. There was no connection with the spinal cord. Complete excision done. Cut section of the mass shows yellowish fatty tissues. Microscopically, adipose tissues, collagen fibres and vascular channels of various sizes were observed. Post-operative period was uneventful with no any neurological complications. The patient is doing well and going school regularly.
Figure 2.
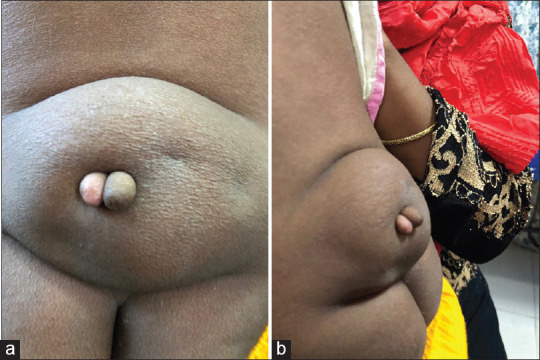
(a and b) Two finger like projection present over the mass just above gluteal cleft and fused together at their base (case 2)
Case 3
A 11-month-old male infant, delivered vaginally from nulliparous mother with uneventful antenatal period presented with painless swelling at the lower back which increases in size gradually. On examination, single pedunculated soft-tissue (caudal appendages) mass approx. 4 cm × 2 cm is located at midline in the lumbosacral region [Figure 3a-c]. There is slight deviation of gluteal cleft towards left. No bony or cartilaginous element was palpable. Neurological and physical developments were normal for his age. Head circumference was normal. There were no other associated anomalies. Ultrasound of the lower back and brain was normal, and X-ray lumbosacral spines are normal. However, spinal MRI was not performed due to financial constrain. The patient was positioned prone, and transverse elliptical incision was given. Skin and subcutaneous tissues were dissected. There was no evidence of tail leading inward from the appendage. Thoracolumbar fascia was found intact. Complete excision was done. Cut section shows yellowish fatty tissues. Microscopically, adipose tissues, collagen fibres and vascular channels of various size were observed. Post-operative period was uneventful with acceptable cosmetic scar. Now, the patient is 2 years old and has good control of bladder and bowel habit and is walking and has no other problem in follow-up.
Figure 3.

(a-c) Single pedunculated soft-tissue (caudal appendages) mass located at midline in the lumbosacral region (case 3)
Case 4
Three years male child with no antenatal check up presented with swelling at lower back since birth which gradually increases in size along with limping gait and stool and urinary incontinence. On examination, diffuse soft-tissue mass approx. 7 cm × 5 cm is located at midline in the lumbosacral region. Single soft-tissue caudal appendages (finger like) protruding from the surface of an underlying diffuse soft swelling [Figure 4]. Spinal MRI revealed subcutaneous component of spinal lipoma at the level of L4/5 tethering into spine. Anal opening was patulous. Child underwent resection of appendage along with intradural lipoma and release of tethered cord with the help of neurosurgeon. Incision was given transversely over the lump and circumferential dissection done. Intradural extention identified and opened. Tethered cord released and excision of lipoma done. Histopathology revealed fibro-adipose tissue with blood vessels and nerve twigs. Post-operative period was uneventful with acceptable cosmetic scar. The patient is under regular follow-up, however, his neurological manifestations are still not improving.
Figure 4.

Image shows finger like protruding from the surface of an underlying diffuse soft swelling (case 4)
DISCUSSION
Human tail is a caudal, vestigial, midline protrusion with skin covering a combination of muscle and adipose tissue.[3] It have been described as resembling a finger, sausage, penis, pigtail or elephant's trunk. Movement has been described in 7 cases, often precipitated by crying or coughing. Incidence is more in male than female. The length of tail varies from 2 to 20 cm.[6]
At the 4th week of the embryological life, sclerotomes are developed from somites, which begin to enfold the neural tube. In the fourth through 6th week, during the formation of vertebrae, the embryo has a tail that was formed by the 10–12 caudal vertebrae. At the end of the 6th week, vertebrae become the main support of the embryo on the axial plan. After this week, aforementioned caudal–coccygeal vertebrae start to dissolve by the phagocytes. At the end of the 8th week, except a few proximal caudal vertebrae, they all vanish. Remaining proximal vertebrae of the caudal level regress, and after birth, they fuse and form the coccyx. If this fusion was to be interrupted, the resulting deficit reveals as the “human tail” formation. This was the main theory to explain the pathophysiology since the 1900s.[7] In 1989, Gaskill and Marlin[8] suggested that these lesions may develop from the neuroectoderm, and they may be formed by the dermal sinus tracts, which extend out of the skin, as an alternative theory. Studies on ’dermal sinuses’ and ’limited dorsal myeloschisis’ by Pang et al. in 2013 also supported this theory.[9] This theory is also consistent with high rates of spinal dysraphism (50%) and tethered cord (81%) concomitance.[7,8,9] Considering the number and variety of accompanying anomalies (lipomyelomeningocele, myelocele, tethered cord, lipoma, anal atresia, horse-shoe kidney, congenital heart disease and teratoma), it is suggested that there might be multiple pathologies causing this formation.[10,11] In cases accompanying both lipomyelomeningocele and tethered cord, such as the presented case, there are both primary and secondary neurulation defects. Both stages may be responsible for the formation of the tail.
Human tails have been classified by different authors. Dao and Netsky sorted human tails into two categories as true tails and pseudo-tail according to their embryological origins.[12] According to this classification, true tails are formed by embryological remnants and include muscle, adipose and connective tissues but no vertebrae in their structure. Pseudo-tails are lesions that have an underlying pathology such as spinal column and coccygeal malformations (lipoma or teratoma).[13] In 1998, Lu et al. suggested different criteria for true tail pseudo-tail classification. He referred coccygeal and a gluteal benign lesion as true tails and suggested that basic excision was sufficient for its treatment. He described pseudo-tails as tail like lesions, accompanied by spinal dysraphism, and explained that these tail like lesions have ectodermal origins caused by the concomitant spinal dysraphism.[14] This clinically helpful classification is used worldwide. In 2016, a new classification that divided human tails into five groups: soft-tissue caudal appendages, bony caudal appendages, bony caudal prominence, true tails, and other caudal appendages was suggested.[15] Still, all of these classifications have more value for embryology than for clinical practice.
This study revealed both true tail and pseudo-tail patients. Patients with true tail did not have neurological manifestation while patient with pseudo-tail had neurological manifestation. The role of preoperative radiography seems mandatory in such cases. Potential tethered cord and accompanying spina bifida occult should always be kept in mind.[5] One of patient had neurological manifestation due to accompanying spina bifida and even after excision of tail and untethering of cord, patient neurological component is not improving. As two of our patients could not afford MRI, considering basic investigations (ultrasound of back and brain and spinal X-ray), our clinical experience and reviewing published literatures helped us to take decision about excision of human tail without spinal MRI.
CONCLUSION
It is recommended that a careful physical examination, along with adequate radiographic imaging of lumbosacral vertebrae help in diagnosing true or false tail. Resection can be easily accomplished with excellent cosmetic and functional results until and unless there is neurological manifestation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ledley FD. Evolution and the human tail: A case report. N Engl J Med. 1982;306:1212–5. doi: 10.1056/NEJM198205203062006. [DOI] [PubMed] [Google Scholar]
- 2.Alashari M, Torakawa J. True tail in a newborn. Pediatr Dermatol. 1995;12:263–6. doi: 10.1111/j.1525-1470.1995.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 3.Shad J, Biswas R. An infant with caudal appendage. BMJ Case Rep. 2012;2012:bcr1120115160. doi: 10.1136/bcr.11.2011.5160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pillai MK, Nair ST. A true human tail in a neonate: Case report and literature review. Sultan Qaboos Univ Med J. 2017;17:e109–11. doi: 10.18295/squmj.2016.17.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canaz G, Akkoyun N, Emel E, Cevik OM, Baydin S, Gokcedag A. A rare case of “Human Tail” associated with lipomyelomeningocele and tethered cord. J Pediatr Neurosci. 2018;13:241–4. doi: 10.4103/jpn.JPN_74_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lundberg GD, Parsons RW. A case of a human tail. Am J Dis Children. 1962;104:72–3. doi: 10.1001/archpedi.1962.02080030074010. [DOI] [PubMed] [Google Scholar]
- 7.Tubbs RS, Malefant J, Loukas M, Jerry Oakes W, Oskouian RJ, Fries FN. Enigmatic human tails: A review of their history, embryology, classification, and clinical manifestations. Clin Anat. 2016;29:430–8. doi: 10.1002/ca.22712. [DOI] [PubMed] [Google Scholar]
- 8.Gaskill SJ, Marlin AE. Neuroectodermal appendages: The human tail explained. Pediatr Neurosci. 1989;15:95–9. doi: 10.1159/000120450. [DOI] [PubMed] [Google Scholar]
- 9.Pang D, Zovickian J, Wong ST, Hou YJ, Moes GS. Limited dorsal myeloschisis: A not-so-rare form of primary neurulation defect. Childs Nerv Syst. 2013;29:1459–84. doi: 10.1007/s00381-013-2189-2. [DOI] [PubMed] [Google Scholar]
- 10.Park SH, Huh JS, Cho KH, Shin YS, Kim SH, Ahn YH, et al. Teratoma in human tail lipoma. Pediatr Neurosurg. 2005;41:158–61. doi: 10.1159/000085876. [DOI] [PubMed] [Google Scholar]
- 11.Donovan DJ, Pedersen RC. Human tail with noncontiguous intraspinal lipoma and spinal cord tethering: Case report and embryologic discussion. Pediatr Neurosurg. 2005;41:35–40. doi: 10.1159/000084863. [DOI] [PubMed] [Google Scholar]
- 12.Dao AH, Netsky MG. Human tails and pseudo-tail. Human Pathol. 1984;15:449–53. doi: 10.1016/s0046-8177(84)80079-9. [DOI] [PubMed] [Google Scholar]
- 13.Dubrow TJ, Wackym PA, Lesavoy MA. ’Detailing the human tail’. Ann Plast Surg. 1988;20:340–4. doi: 10.1097/00000637-198804000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Lu FL, Wang PJ, Teng RJ, Yau KI. The human tail. Pediatr Neurol. 1998;19:230–3. doi: 10.1016/s0887-8994(98)00046-0. [DOI] [PubMed] [Google Scholar]
- 15.Wilkinson CC, Boylan AJ. Proposed caudal appendage classification system; spinal cord tethering associated with sacrococcygeal eversion. Childs Nerv Syst. 2017;33:69–89. doi: 10.1007/s00381-016-3208-x. [DOI] [PubMed] [Google Scholar]


