Abstract
Home blood pressure monitoring (HBPM) overcomes many of the limitations of traditional office blood pressure (BP) measurement and is both cheaper and easier to perform than ambulatory BP monitoring. Monitors that use the oscillometric method are currently available that are accurate, reliable, easy to use, and relatively inexpensive. An increasing number of patients are using them regularly to check their BP at home, but although this has been endorsed by national and international guidelines, detailed recommendations for their use have been lacking. There is a rapidly growing literature showing that measurements taken by patients at home are often lower than readings taken in the office and closer to the average BP recorded by 24‐hour ambulatory monitors, which is the BP that best predicts cardiovascular risk. Because of the larger numbers of readings that can be taken by HBPM than in the office and the elimination of the white‐coat effect (the increase of BP during an office visit), home readings are more reproducible than office readings and show better correlations with measures of target organ damage. In addition, prospective studies that have used multiple home readings to express the true BP have found that home BP predicts risk better than office BP (class IIa; level of evidence A). This call‐to‐action article makes the following recommendations: (1) It is recommended that HBPM should become a routine component of BP measurement in the majority of patients with known or suspected hypertension; (2) Patients should be advised to purchase oscillometric monitors that measure BP on the upper arm with an appropriate cuff size and that have been shown to be accurate according to standard international protocols. They should be shown how to use them by their healthcare providers; (3) Two to 3 readings should be taken while the subject is resting in the seated position, both in the morning and at night, over a period of 1 week. A total of ≥12 readings are recommended for making clinical decisions; (4) HBPM is indicated in patients with newly diagnosed or suspected hypertension, in whom it may distinguish between white‐coat and sustained hypertension. If the results are equivocal, ambulatory BP monitoring may help to establish the diagnosis; (5) In patients with prehypertension, HBPM may be useful for detecting masked hypertension; (6) HBPM is recommended for evaluating the response to any type of antihypertensive treatment and may improve adherence; (7) The target HBPM goal for treatment is <135/85 mm Hg or <130/80 mm Hg in high‐risk patients; (8) HBPM is useful in the elderly, in whom both BP variability and the white‐coat effect are increased; (9) HBPM is of value in patients with diabetes, in whom tight BP control is of paramount importance; (10) Other populations in whom HBPM may be beneficial include pregnant women, children, and patients with kidney disease; and (11) HBPM has the potential to improve the quality of care while reducing costs and should be reimbursed.
The standard method for the measurement of blood pressure (BP) in clinical practice has traditionally been to use readings taken with the auscultatory technique by a physician or nurse in a clinic or office setting. Although such measurements are likely to remain the cornerstone for the diagnosis and management of hypertension for the foreseeable future, it is becoming increasingly clear that they often give inadequate or even misleading information about a patient's true BP status. All clinical measurements of BP may be regarded as surrogate estimates of the “true” BP, which may be regarded as the average level over prolonged periods of time. In the past 30 years, there has been an increasing trend to supplement office or clinic readings with out‐of‐office measurements of BP, taken either by the patient or a relative at home (home or self‐monitoring [home BP monitoring; HBPM]) or by an automated recorder for 24 hours (ambulatory blood pressure monitoring [ABPM]).
Of the 2 methods, HBPM has the greatest potential for being incorporated into the routine care of hypertensive patients in the same way that home blood glucose monitoring performed by the patient has become a routine part of the management of diabetes. The currently available monitors are relatively reliable, easy to use, inexpensive, and accurate and are already being purchased in large numbers by patients. Despite this, their use has been only cursorily endorsed in current guidelines for the management of hypertension, and there have been no detailed recommendations in regard to the manner in which they should be incorporated into routine clinical practice. In addition, despite the fact that there is strong evidence that HBPM can predict clinical outcomes and improve clinical care, the cost of the monitors is not generally reimbursed. It is the purpose of this call‐to‐action article to address the issues of the incorporation of HBPM into the routine management of hypertensive patients and its reimbursement. A full version of the article has been published elsewhere. 1
CURRENT USAGE OF HBPM
The use of HBPM has been recommended by several national and international guidelines for the management of hypertension and has been increasing steadily over the past few years. A recent Gallup poll of hypertensive patients found the following:
-
•
The number of patients monitoring their BP at home has increased steadily over the past 5 years, being 38% in 2000 and 55% in 2005, an increase of 17%.
-
•
The proportion of patients owning a monitor has increased from 49% in 2000 to 64% in 2005.
-
•
Of patients who do not own monitors, 14% said that expense was the reason.
TECHNIQUES FOR PERFORMING HBPM
When HBPM was first used, BP was measured with the auscultatory technique, but this has now been almost completely supplanted by the use of oscillometric devices specifically designed for use by patients in the home. These are mostly fully automatic, so that the patient only needs to wrap the cuff around the upper arm and press a button for the machine to take a reading and display the values for systolic and diastolic pressure on a screen. Some require the patient to inflate the cuff manually.
Arm Monitors
Monitors that measure the BP in the brachial artery with a cuff placed on the upper arm continue to be the most reliable and have the additional advantage that the brachial artery pressure is the measure that has been used in all the epidemiological studies of high BP and its consequences. For the majority of patients, this is the preferred type of monitor.
Wrist Monitors
Wrist monitors are not recommended for routine clinical use.
Testing and Validation of Monitors
Patients should be advised to use only monitors that have been validated for accuracy and reliability according to standard international testing protocols. Unfortunately, only a few of the devices that are currently on the market have been subjected to proper validation tests, such as the Association for the Advancement of Medical Instrumentation and British Hypertension Society protocols, and several devices have failed the tests. An up‐to‐date list of validated monitors is available on the Dabl Educational Web site (http://www.dableducational.org) and the British Hypertension Society Web site (http://www.bhsoc.org/default.stm).
Checking Monitors for Accuracy
When patients get their own monitor, it is very important to have them bring it into the clinic to check their technique as well as the accuracy of the monitor.
Patient Education
It is critical that patients should be educated in the proper use of home monitors. Automated oscillometric devices are much easier to use than auscultatory monitors but still require some training. Patients should be advised to only purchase monitors that have been validated according to standard protocols (see above), and their upper arm circumference should be measured so that they can be advised if they need a large cuff. They should be told that readings should be taken when they are sitting quietly after resting for 5 minutes, with the arm supported on a flat surface, such that the upper arm is supported at the level of the heart. The patient's back should be supported, and both feet should be flat on the floor. The cuff should be positioned so that its mid portion lies over the brachial artery. Most patients find it easiest to measure BP in the nondominant arm, and this should be encouraged unless there is a marked difference between the 2 arms, which is relatively rare in the absence of obstructive arterial disease. The patient should not have indulged within the 30 minutes preceding the measurement in activities such as smoking, drinking coffee, or exercising, which are likely to affect BP. It is recommended that at least 2 and preferably 3 readings be taken at 1 time and the value for each reading written down, unless the device has a memory that stores the readings automatically. The interval between readings can be as little as 1 minute. Readings should routinely be taken first thing in the morning (preferably before the subject takes medications) and at night before the subject goes to bed. The frequency of readings can be determined by the physician. Patients should not be encouraged to take readings at other times, such as when they think they are under stress or that their BP is high. Patients need not routinely keep diaries, but it may be helpful to record if they missed taking their medications. Patients should be advised that the variability of readings is high and that individual high or low readings have little significance.
Once a monitor has been purchased, it is recommended that the patient should bring it into the office to verify both the patient's technique and the accuracy of the device. This procedure should be repeated annually. Unlike aneroid and mercury devices, however, it has been found that the accuracy of the measurement of the cuff pressure does not deteriorate over time with oscillometric monitors.
CONTRAINDICATIONS TO HBPM
There are some patients in whom HBPM is contraindicated. The oscillometric method may not work well in patients who have atrial fibrillation or other arrhythmias such as frequent ectopic beats. In such patients, it may be worth checking the ability of a monitor to measure BP in the clinic by comparing the monitor readings against those taken with the auscultatory method.
Some patients may become obsessed about taking readings. The inherent variability of BP means that there will inevitably be some high readings, which in anxious patients may exacerbate their anxiety, leading to further increases of BP and effectively setting up a vicious cycle. In such patients frequent checking of their BP should be discouraged, and in extreme cases it should be discontinued altogether.
INFORMATION PROVIDED BY HBPM
HBPM as an alternative to the office BP reading can no longer be overlooked as a significant adjunct to assessment and treatment of individuals with hypertension.
Information Is Reliable and Reproducible
One of the advantages of HBPM is that large numbers of readings can be used to define a patient's BP level. Findings suggest that home BP measurements are more reproducible over time than office BP.
Another aspect of the reliability of HBPM is the accuracy of patients in reporting the readings displayed by the monitors. Some patients may tend to make their home readings look better than they really are, and for this reason the use of monitors with memory is encouraged.
Number of Home BP Measurements Needed to Ensure a Reliable Estimate of True BP
Two recent analyses have recommended taking between 8 and 15 readings in total, and we recommend following the last set of European Society of Hypertension guidelines to take at least 2 morning and 2 evening readings every day for 1 week but to discard the readings of the first day, which gives a total of 12 readings on which to make clinical decisions. Patients should be instructed to record all the readings that they take.
Information About True BP Level
BP fluctuates continuously in a 24‐hour period, and the variability is influenced by neural, mechanical, and humoral factors. Patients should be advised that BP can change by ≥20 mm Hg between readings and should not be concerned about this. It is difficult to determine true BP level on the basis of 1 or 2 BP measurements at the time of an office visit. HBPM is a simple and inexpensive way to obtain a large number of readings, representative of usual BPs over long periods of time, that are unaffected by the white‐coat effect or other factors influencing variability that are present in the office.
Information About BP at Different Times of the Day
The pattern of BP change over the day may vary considerably from one patient to another, depending on their daily routine and medications. There is some evidence that the morning pressure may be a better predictor of risk than the evening pressure. For these reasons, it is generally recommended that patients should take readings both in the early morning and at night. The main limitation of home monitors in comparison with 24‐hour ambulatory monitors is that nighttime readings cannot be taken.
HBPM DIAGNOSING HYPERTENSION
The diagnosis of hypertension may be expedited by HBPM, particularly in individuals with stage 1 hypertension (BP 140/90 to 160/100 mm Hg), in which the elevation of BP is relatively modest (typically those without diabetes, chronic kidney disease, or target organ damage). Often individuals with white‐coat hypertension may make multiple office visits over a prolonged period of months before the diagnosis of hypertension is established. Home BP is usually lower than office BP (as a result of the white‐coat effect) and may suggest a diagnosis of white‐coat hypertension. However, in ≈10% of patients it may be higher, indicating a possible diagnosis of masked hypertension. There is increasing evidence that home BP may provide a better prediction of risk than office BP, and therefore any discrepancies between office and home BP should be taken seriously.
EVALUATION OF WHITE‐COAT HYPERTENSION AND THE WHITE‐COAT EFFECT
White‐coat hypertension is defined as high BP occurring only in a medical care setting and that has been reported in as many as 20% of patients in whom hypertension has been diagnosed by office BP. The phenomenon that leads to it is called the white‐coat effect, which is usually defined as the difference between the office BP and the BP measured at home or during the day by ABPM, and which has been attributed to anxiety, a hyperactive alerting response, or a conditioned response. The white‐coat effect is typically positive and is present in the majority of hypertensive patients, but in some patients with low office BP it may be negative (home BP higher than office BP). If the HBP is normal (<135/85 mm Hg), a diagnosis of white‐coat hypertension may be considered.
White‐coat hypertension is more common in the elderly and is generally associated with a relatively benign prognosis similar to that seen in truly normotensive subjects, as shown by several prognostic studies comparing office BP and ambulatory BP. However, there have been reports of higher cardiovascular disease (CVD) event rates that are similar to those seen in patients with sustained hypertension. The implication of these results is that out‐of‐office monitoring should be conducted long term in all patients diagnosed with white‐coat hypertension and that the prognosis is intermediate between true normotension and sustained hypertension.
ALGORITHM FOR USE OF HBPM IN CLINICAL PRACTICE
An algorithm that uses both HBPM as an initial screening test and ABPM to make the definitive diagnosis is shown in the Figure. The rationale for this is that the exclusive reliance on office BP for making therapeutic decisions may lead to both undertreatment and overtreatment in individual patients because of both the inherent variability of BP and the white‐coat effect. As originally proposed, this algorithm would only be applied to patients who have a persistently high clinic BP (>140/90 mm Hg), but it might also be applicable to those with high‐normal BP (eg, a patient who has had some readings >140/90 but on rechecking has a slightly lower level), in whom masked hypertension may be suspected. In addition, in patients with diabetes or kidney disease, it may be used if the clinic BP is ≥130/80 mm Hg. In patients who have evidence of target organ damage that is thought to be the result of hypertension, it may be decided to start treatment on the basis of the high clinic BP, although HBPM is still valuable for monitoring the response to treatment. Numerous studies have shown that even subclinical markers of organ damage such as microalbuminuria or left ventricular hypertrophy have been shown to increase CVD risk, as reviewed in the recent European guidelines on the management of hypertension, which may justify more aggressive treatment.
Figure.
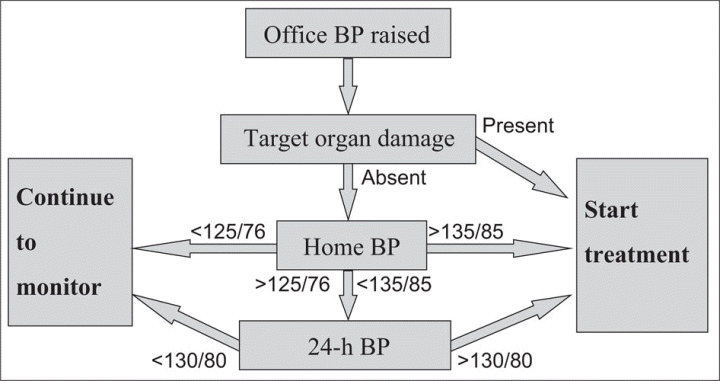
Schema for evaluating BP status of hypertensive patients, which can be used in patients in whom the decision to start treatment may be uncertain on the basis of the office BP, which may be just above or below the cutoff point defining adequate control. HBPM may be used to aid the diagnosis if necessary in conjunction with ABPM.
In those in whom the decision to start treatment remains unclear, HBPM is an appropriate next step, with the goal of obtaining a minimum of 12 readings taken both in the morning and at night over a period of 7 days. If the average value is >135/85 mm Hg, there is a high probability (85%) that the ambulatory BP will also be high, and a decision to start treatment can be made. If the home BP is <125/76 mm Hg, the probability of missing a diagnosis of true hypertension is quite low. Because BP varies with time, whichever method of measurement is used, a diagnosis of white‐coat hypertension is not cast in stone, and all patients in whom the diagnosis is made require long‐term monitoring of BP, for which HBPM is ideally suited.
EVALUATION OF MASKED HYPERTENSION
HBPM may also be useful in detecting masked hypertension, also known as reverse white‐coat hypertension or isolated home or isolated ambulatory hypertension. Masked hypertension occurs when a patient's office BP is <140/90 mm Hg but ambulatory or home readings are in the hypertensive range (typically >135/85 mm Hg). It conveys the same cardiovascular risk as sustained hypertension, and therefore it is important that it is detected.
The prevalence of masked hypertension may be ≈10% in the general population, but at the present time there is no consensus in regard to how it should be detected or treated in people who have not been diagnosed as hypertensive. However, in patients with treated hypertension that is thought to be well controlled (ie, an office BP <140/90 mm Hg), it may be equally common. This high prevalence in patients whose BP appears to be controlled by conventional clinical criteria makes the case that HBPM should be used routinely in treated hypertensive patients.
EVALUATION OF PREHYPERTENSION
Approximately 28% of American adults, or 59 million people, have prehypertension, defined as a BP in the range of 120 to 139/80 to 89 mm Hg. These people were previously defined as having high‐normal BP. Because this is normally diagnosed with office BP, some will have white‐coat hypertension. Regular and consistent monitoring of BP should begin during prehypertension to establish the need for treatment or help to establish a firm baseline for determining response and change. Limited information is available on the use of HBPM in this situation, but it is ideally suited to these needs. One study (the Tecumseh study) found that in prehypertensive individuals diagnosed by office readings, home BP (average of 14 readings, 7 days with morning and afternoon or evening readings) was more predictive than office BP of future BP status after 3 years, even when the same number of measurements was used for both methods.
EVALUATION OF RESISTANT HYPERTENSION
HBPM may be helpful for evaluating resistant hypertension in patients exhibiting high office BP under antihypertensive therapy. Patients who appear to be refractory to treatment in the clinic or office may have adequately controlled home BP and consequently require less intensification of drug treatment than those whose home BP is also high.
HBPM for Predicting Cardiovascular Risk
HBPM has been shown to be useful in predicting target organ damage, CVD mortality, and CVD events.
Other investigators have used cross‐sectional designs to evaluate the usefulness of HBPM in patients with diabetes. Researchers examined whether BP elevations in the morning detected by were more predictive than office BPs for microvascular (nephropathy and retinopathy) and macrovascular complications (coronary heart disease and cerebral vascular disease) in patients with type 2 and type 1 diabetes. In both groups, home BP but not office BP was strongly related to nephropathy. There were no significant differences between the groups for the other measures of target organ damage.
Five prospective studies (all with several publications) have compared the prediction of morbid events with the use of both conventional office BP and home BP (Table 1). Three were based on population samples, and 2 recruited hypertensive patients. Four studies found that home BP was the stronger predictor of risk. The fifth found that both BP measures predicted risk.
Table I.
Prospective Studies Relating Home BP and Office BP to CV Events and Mortality
| Study | Population Studied | No. of Subjects | Home BP schedule | Outcome | |||
|---|---|---|---|---|---|---|---|
| Days | AM | PM | Total | ||||
| Ohasama 2 | Population | 1789 | 28 | 1 | 0 | 28 | Strokes and mortality predicted better by HBPM |
| SHEAF 3 | Treated hypertensive patients | 4939 | 4 | 3 | 3 | 24 | CV morbidity and mortality predicted better by HBPM |
| PAMELA 4 | Population | 2051 | 1 | 1 | 1 | 2 | CV and total mortality predicted better by HBPM |
| Belgian 5 | Referred | 391 | 1 | 3 | 0 | 3 | Combined CV events predicted better by HBPM |
| Didima 6 | Population | 662 | 3 | 2 | 2 | 12 | CV events predicted by both HBPM and by office BP |
| Abbreviations: BP, blood pressure; CV, cardiovascular; HBPM, home blood pressure monitoring; PAMELA, Pressioni Arteriose Monitorate E Loro Associazioni; SHEAF, Self‐Measurement of Blood Pressure at Home in the Elderly: Assessment and Follow‐up. | |||||||
INFORMATION ABOUT BP CONTROL
HBPM has the ability to provide information about BP control outside the office setting. One study found that 9% of patients with normal office BP had elevated home BP (ie, masked hypertension) and had twice the risk of CVD events as the group in whom both office and home BP were controlled.
USE OF HBPM TO GUIDE AND EVALUATE TREATMENT
HBPM may provide important information about the responsiveness of individuals to antihypertensive treatment. Studies of the effects of placebo drugs have found that they have little effect on home BP, in contrast to their much larger effect on office BP. By having patients take readings both in the early morning and in the evening, the adequacy of BP control throughout the day (and the trough‐to‐peak ratio) can be assessed. Thus, HBPM may be regarded as the method of choice for monitoring the effects of antihypertensive treatment.
USE OF HBPM AS AN INTERVENTION FOR IMPROVING MEDICATION ADHERENCE AND BP CONTROL
Although most of the attention paid to HBPM is for its value as a diagnostic tool, there is increasing evidence that it may also serve as an intervention to improve BP control. Success with behavioral or lifestyle interventions in patients with chronic conditions is often improved by encouraging the patient to become actively involved in his or her care, which may include self‐monitoring. In the case of obesity, 75% of people who are successful with long‐term weight loss report weighing themselves regularly.
Effects on Medication Adherence
If HBPM does improve BP control, a potential mechanism is by improved medication adherence, which is supported by recent evidence. The data on the effects of HBPM on patients' medication‐taking behavior are mixed but suggest that HBPM should be considered a useful adherence‐enhancing strategy, especially when used in combination with other approaches such as patient counseling, patient reminders, and use of nurse case managers.
Effects on BP Control
There is also evidence that HBPM is associated with better BP control. A meta‐analysis of 18 randomized controlled trials that compared HBPM with usual care found that HBPM resulted in better BP control and greater achievement of BP targets than usual BP measurement in the healthcare system. Although these BP effects were small (2.2/1.9 mm Hg), the implications from a prognostic standpoint and as a population‐based strategy are significant. Taken together, these findings suggest that HBPM on its own will not necessarily result in better BP control, but it has the potential to do so if the data are communicated regularly to the healthcare providers and appropriate action is taken. Further study is needed in this area.
NEED FOR HBPM IN SPECIAL POPULATIONS
The Elderly
Because there are also potential hazards of excessive BP reduction in older people, the case for using out‐of‐office monitoring such as HBPM is very strong. The difference between the office systolic BP and home BP (the white‐coat effect) increases progressively with age, so that office BP tends to overestimate the out‐of‐office BP more in older than in younger people. The variability of systolic home BP readings also increases with age. HBPM can also be used to detect orthostatic BP changes if readings are taken with the subject both sitting and standing.
Patients With Diabetes
BP control is one of the most important aspects of managing patients with diabetes, and as in patients without diabetes, the home BP is superior to the office BP for predicting the 24‐hour BP level. There are at present no official guidelines for the home BP level equivalent to an office BP of 130/80 mm Hg in patients with diabetes, although 1 study used 125/75 mm Hg. Although there is less evidence for the benefits of HBPM in patients with diabetes, existing data are entirely consistent with observations in those without diabetes, and because there is strong evidence that aggressive reduction of BP is more effective in patients with diabetes in lowering CVD risk, a strong case can be made for the wider use of HBPM in patients with diabetes.
Pregnancy
The accurate measurement of BP during pregnancy is one of the most important aspects of prenatal care, and preeclampsia, which is the most common cause of maternal and fetal death, can develop quite rapidly. The situation in pregnancy is essentially dynamic: BP first falls and then rises, and therefore the best way of detecting an abnormal pattern that presages preeclampsia may be to monitor its changes very frequently throughout the course of pregnancy. Thus, the earliest manifestation of preeclampsia is a failure to decrease BP, or a premature increase of BP, during the second trimester. HBPM is theoretically ideal for monitoring changes in BP during pregnancy because it is the best technique for providing multiple readings recorded at the same time of day over prolonged periods of time. Several monitors have been validated for use in pregnant women. Although some studies have been done to show that HBPM is practical and has the potential to reduce clinic visits, the extent to which it will improve the evaluation and management of hypertension during pregnancy has yet to be shown.
White‐coat hypertension is not uncommon and may lead to unnecessary early termination of pregnancy. This should be detectable with the use of HBPM.
Chronic Kidney Disease
Hypertension is highly prevalent in patients with chronic kidney disease and also in the dialysis population, but the BP is very variable, and measurements made in dialysis centers give a poor prediction of clinical outcomes. HBPM has been advocated in these patients but thus far has been used infrequently. Despite the fact that arterial stiffness is greatly increased in such patients, oscillometric monitors may still be accurate in patients with endstage renal disease. HBPM has been shown to be superior to measurements made in the dialysis unit for predicting ambulatory hypertension.
Children
Increasing attention is being paid to the issue of hypertension in children, particularly because, with the epidemic of obesity, it is likely that its prevalence will increase. The phenomenon of white‐coat hypertension occurs in children just as in adults, and therefore it makes sense to use out‐of‐office monitoring in addition to clinic measurements, but the normal home BP values in children are not well established. Thus, HBPM appears to be of great potential value in children when the proper cuff size is used, although more studies are needed in this area.
COST‐EFFECTIVENESS OF HBPM
The potential for HBPM to be cost‐effective for the diagnosis and management of hypertension has received little attention. In principle, there are 2 types of situations in which it is used: (1) for the diagnosis of hypertension and hence the need for treatment, for which monitoring need only be done for a limited period of time; and (2) for the evaluation of treatment, for which long‐term monitoring is appropriate. Other potential advantages for use of HBPM are a reduced need for office/clinic visits but with increased need for alternative communication by telephone or telemetry, as well as more accurate assessment of overtreatment and the opportunity of reducing medication in some patients.
In contrast to HBPM, it has been shown that use of ABPM can be cost‐effective when applied to the diagnosis of hypertension (specifically white‐coat hypertension). If HBPM and ABPM were fully equivalent with regard to detection of white‐coat hypertension, then any difference in cost between the 2 methods would be a basis for choosing the one that costs less. Currently, Medicare reimburses ABPM for patients with suspected white‐coat hypertension. This requires the patient to meet the following criteria: (1) office BP >140/90 mm Hg on at least 3 separate clinic/office visits with 2 separate measurements made at each visit; (2) at least 2 BP measurements taken outside the office that are <140/90 mm Hg; and (3) no evidence of end‐organ damage. The charges allowed by the Centers for Medicare & Medicaid Services for ABPM in the United States to confirm the diagnosis of white‐coat hypertension vary from ≈$70 to ≈$105. This reimbursement (Current Procedural Terminology code 93784) includes both the monitoring procedure for ≥24 hours, per se, and an interpretation provided by the physician.
There is no recognized Current Terminology code for HBPM (without the memory and computational equivalents to ambulatory monitoring) and no systematic basis for how reimbursement might be developed. However, several known costs and likely factors allow for an argument that HBPM be considered for reimbursement if incorporated into a systematic plan for management of individual hypertensive patients. These are summarized below.
Cost of Home BP Devices
Many devices for HBPM are available for purchase by consumers who want to take their own BP or measure that of others in their household or at screening sites. Devices are available at drug stores and many other sources. Purchase through Web sites is firmly established and was reviewed in 2005. Prices vary from <$50 to ≈$100. It is recommended that the best devices for HBPM have electric inflation of cuffs, oscillometric detection, and memory. These recommendations are based on 2 concerns: (1) errors that may be introduced by self‐inflation of the cuff and (2) selection bias that may affect the recording and reporting of pressures if patients choose the values to report. Thus, the out‐of‐pocket cost to a patient for purchase of a recommended device for HBPM will be in the range of $80 to $100 unless reimbursement is provided from that patient's health insurance provider or the cost is offset by an incentive, such as a taxfree purchase. Buying a large adult cuff, which is not standard, may add to the overall cost.
Costs and Savings Related to Implementation and Use of HBPM
In theory, incorporation of HBPM into treatment of hypertension may appear to lessen the cost of care. Some reports lend support to the simple view that HBPM can reduce costs for treatment of hypertension (reduced visits and perhaps less medication) while increasing or at least maintaining the effectiveness of treatment for prevention of CVD, given the relatively low cost of purchase for a home BP device.
Other Cost Considerations
There are several hidden or offsetting factors that should be taken into account when the actual costs for use of HBPM are calculated. First, there are costs related to the necessary validation of each device and training of each patient in proper use of each device for measurement of BP and recording and/or transmission of measurements, which are not well established. Next, there are costs related to the review of HBPM data and advice to patients regarding change in treatment. There is need for some calculation of equivalency to ensure reimbursement for the provider, should office/clinic visits be replaced by an HBPM strategy that still requires the time and resources of the provider. Here, differences in medical care systems may be relevant. Those who practice in fee‐for‐service modes may be reluctant to give up the reimbursements related to office visits unless some incentive is evident. By contrast, those with high‐volume capitated practices may welcome a strategy that reduces office/clinic visits but reimburses for hypertensive patients enrolled and managed by HBPM. Going further, it might be suggested that providers expanding use of HBPM be given incentives for this effort, should outcome studies justify this approach.
It should be recognized that the long‐term cost of care for hypertension is dominated by costs for drug treatment rather than for visits to providers or testing. However, costs for the first year of management tend to be higher than for subsequent years (more tests and visits). Drug choices then determine the greatest fraction of costs, so that over a 5‐year period the cost for treatment of a patient may vary from $1700 to $3000. In general, emphasis on guideline‐based drug selection (diuretics and β‐blockers initially) is associated with lower combined treatment costs. Thus, use of HBPM to reduce cost of treatment will be most effective when implemented to detect white‐coat hypertension and reduce the need for drug treatment, as has been shown for ABPM.
The impact of HBPM for overall cost of management for hypertensives in community practice who are placed on drug treatment is less certain. If telemedicine methods are used, what will the costs be for receiving and processing information? Who will pay for such services? Can the methods be made so efficient that there is minimal demand for time by the provider? What financial incentives are available to support providers for their responsibilities? These questions pose the need for research in the healthcare systems that link patients with hypertension to physicians and practices via the various financial structures that pay for medical care. Without such research, the actual impact of HBPM on cost‐effectiveness for prevention of CVD cannot be calculated.
PART II: ACTION PLAN
Given the amount of accumulated evidence about the value of HBPM, it is time to make HBPM a part of routine management of hypertensive patients, especially those with diabetes, coronary heart disease, chronic kidney disease, suspected nonadherence, or a substantial white‐coat effect. Table 2 provides recommendations for its use.
Table II.
Summary of Recommendations for HBPM
| Procedure | Recommendation |
|---|---|
| Technical aspects of BP measurement | Measure BP: |
| • No tobacco or caffeine for 30 minutes preceding measurement | |
| • After 5 minutes rest | |
| • With arm at heart level; back supported and feet flat on the ground | |
| • On nondominant arm (or arm with the highest BP) | |
| BP monitor | • Use a fully automated device with an upper arm cuff that has been validated by BHS, AAMI, or International Protocol for the Validation of Automated BP Measuring Devices |
| • Monitors with memory that are able to store measurements are preferred | |
| Training of patients | • Patients should be trained by their health care provider, and the monitor readings checked against mercury |
| • Education content: hypertension and cardiovascular risk, BP measurement procedure, use of a validated monitor, cuff size, protocols for measuring BP, interpretation of BP readings, and monitor for their use only | |
| • Reevaluate patient technique and the accuracy of the device annually | |
| Target BP goal | • 135/85 mm Hg, or 130/80 mm Hg if patient has diabetes, coronary heart disease, or chronic kidney disease (Class IIa; Level of Evidence B) |
| Frequency and schedule of measurement | Initial values (when patients begin HBPM): |
| • Base decisions on a 7‐day measurement period with 2–3 measurements each morning and 2 to 3 measurements in the evening at prestipulated times (an average of 12 morning and evening measurements) | |
| • Exclude first‐day measurements from the analyses; take average of these values as the reference parameter in the subsequent dose‐titration phase | |
| Dose‐titration phase (titration of initial dose and adjustment of therapy): | |
| • All measurements should be made under identical conditions and at the same times of day as the initial values | |
| • HBPM data should be ascertained as trough values (ie, before medication is taken) in the morning and again at night | |
| • Use the average of BPs measured over 2 to 4 weeks to assess the effect of treatment | |
| Long‐term observation: | |
| • For stable normotensive (controlled) patients, patients should conduct HBPM a minimum of 1 week per quarter (an average of 12 morning and evening measurements under conditions described above) | |
| • Measurement should be made more frequently in patients with poor compliance | |
| Abbreviations: AAMI, Association for the Advancement of Medical Instrumentation; BHS, British Hypertension Society; BP, blood pressure; HBPM, home blood pressure monitoring. | |
Additionally, because HBPM is part of evidence‐based care, it should be reimbursed. Regular use of HBPM will improve the quality and cost of delivering care to the 72 million people with hypertension and should lead to improved control of hypertension. Reimbursement is critically important to hypertensive patients and to their providers. Cost should not be a barrier to patients receiving the documented benefits of HBPM. Reimbursement will improve access to recommended health care for the impoverished, isolated, medically vulnerable, and/or disadvantaged minority groups. Improved access may contribute to reductions in hypertension‐related disparities among disproportionately affected groups.
It is recommended that patients be reimbursed for the purchase of a monitor prescribed by their healthcare provider (physician and/or nurse practitioner) and that providers be reimbursed for services related to HBPM (ie, initial patient education regarding correct HBPM technique; yearly or as‐needed assessments to validate that individuals self‐measure their BP accurately; interpretation of BPs stored in the monitor memory; in‐person, telephone, and/or e‐mail consultation to deliver medical advice‐based analysis of BP reports generated from the monitor). Monitors should be renewable after 5 years or if they are shown to be inaccurate.
Disclosures:
Dr Pickering has received research grants from Omron Healthcare and Microlife and serves on the Speakers' Bureau of (and/or has received honoraria from) Boehringer‐Ingelheim and Omron Healthcare. Dr Houston Miller has received research grants from the National Heart, Lung, and Blood Institute; serves on the Speakers' Bureau of (and/or has received honoraria from) Merck, Inc; and is a consultant for/serves on the advisory board of Pfizer and CV Therapeutics. Dr Artinian has received research grants from Wayne State University Center for Health Research Summer Research Initiative, the National Center of Nursing Research, and the National Center on Minorities and Health Disparities. Dr Goff is a consultant for/serves on the advisory board of Pfizer.
The American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association make every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
This statement was approved by the American Heart Association Science Advisory and Coordinating Committee on January 7, 2008; by the American Society of Hypertension on January 2, 2008; and by the Preventive Cardiovascular Nurses Association on December 28, 2007.
This article has been copublished in Journal of the American Society of Hypertension, Journal of Clinical and Journal of Cardiovascular Nursing.
Expert peer review of AHA Scientific Statements is conducted at the AHA National Center. For more on AHA statements and guidelines development, visit http://www. americanheart.org/presenter.jhtml?identifier=3023366.
Copies:
This document is available on the World Wide Web sites of the American Heart Association (my.americanheart.org), the American Society of Hypertension (www.ash‐us.org), and the Preventive Cardiovascular Nurses Association (http://www.pcna.net). A single reprint is available by calling 800‐242‐8721 (US only) or by writing the American Heart Association, Public Information, 7272 Greenville Ave, Dallas, TX 75231‐4596. Ask for reprint No. 71‐0443. A copy of the document is also available at http://www.americanheart.org/presenter.jhtml?identifier=3003999 by selecting either the “topic list” link or the “chronological list” link. To purchase additional reprints, call 843‐216‐2533 or e‐mail kelle.ramsay@wolterskluwer.com.
Permissions:
Multiple copies, modification, alteration, enhancement, and/or distribution of this document are not permitted without the express permission of the American Heart Association. Instructions for obtaining permission are located at http://www.americanheart.org/presenter.jhtml?identifier=4431. A link to the “Permission Request Form” appears on the right side of the page.
© 2008 American Heart Association, Inc, the American Society of Hypertension, and the Preventive Cardiovascular Nurses Association.
References
- 1. Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008: Epub ahead of print. May 22, 2008. 10.1161/HYPERTENSIONAHA.107.189011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population‐based observation in Ohasama. J Hypertens. 1998;16:971–975. [DOI] [PubMed] [Google Scholar]
- 3. Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self‐measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342–1349. [DOI] [PubMed] [Google Scholar]
- 4. Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, Mancia G. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow‐up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–1783. [DOI] [PubMed] [Google Scholar]
- 5. Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:801–807. [DOI] [PubMed] [Google Scholar]
- 6. Oikawa T, Obara T, Ohkubo T, Kikuya M, Asayama K, Metoki H, Komai R, Murai K, Hashimoto J, Totsune K, Imai Y; J‐HOME Study Group . Characteristics of resistant hypertension determined by self‐measured blood pressure at home and office blood pressure measurements: the J‐HOME study. J Hypertens. 2006;24:1737–1743. [DOI] [PubMed] [Google Scholar]


