Abstract
Antihypertensive treatment regimen persistence and compliance were measured using a retrospective cohort study of pharmacy claims data. Newly treated patients receiving monotherapy with angiotensin II receptor blockers (ARBs), angiotensin‐converting enzyme inhibitors (ACEIs), calcium channel blockers (CCBs), β‐blockers (BBs), or diuretics were followed for 1 year (N=242,882). A higher proportion of ARB patients (51.9%) were persistent in taking prescribed medication compared with those in the ACEI (48.0%), BB (40.3%), CCB (38.3%), and diuretic groups (29.9%). Compared with patients receiving diuretics, those receiving ARBs (hazard ratio [HR], 0.593; P<.0001), ACEIs (HR, 0.640; P<.0001), CCBs (HR, 0.859; P<.0001), and BBs (HR, 0.819; P<.0001) were all less likely to discontinue therapy. Compliance was similar in ACEI and ARB patients, but patients receiving ARBs and ACEIs had better compliance than those receiving BBs, CCBs, or diuretics. The lesser degree of compliance and persistence observed in patients receiving diuretics compared with other antihypertensive medications may have public health as well as cost implications.
The prevalence of hypertension has continued to rise over the past decades, reaching 31.3% for 1999–2000, 1 possibly as the result of better detection and more specific definitions. Only 37% of all patients with hypertension and only 57% of those receiving antihypertensive medication in the United States currently have controlled blood pressure (BP). 2 This is an improvement over prior years, as the National Health and Nutrition Examination Survey (NHANES) III indicated that during the time period of 1991 to 1994, only 22.7% of hypertensive patients had their BP controlled. 3 The current rate remains well below the Healthy People 2010 goal of 50%, set by the US Department of Health and Human Services, however. 4
In 2003, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure was published (JNC 7), which included the recommendation of thiazide diuretics for treatment of most patients with uncomplicated hypertension, either alone or in combination with drugs from other antihypertensive classes. 5 JNC 7 recommended that thiazide diuretics be used as first‐step therapy for hypertension management in the absence of high‐risk conditions. Despite these recommendations, the use of diuretics as first‐step therapy in hypertension has remained less common than might be expected, 6 especially since they are available at a low cost.
This recommendation of first‐step diuretic use was based on data from many clinical trials, including the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), 7 which reported that diuretics were equal to or more effective in preventing cardiovascular complications of high BP than other medications. Clinical data on long‐term antihypertensive medication use has largely been obtained in controlled clinical trials, where patient medication was provided, patients had protocol‐mandated visit schedules, and medication consumption was monitored. Patient compliance and persistence in trials such as ALLHAT 7 may vary substantially from real‐world patient compliance. 8 , 9 , 10 In studies conducted in usual‐care settings, improved persistence or compliance with antihypertensive therapy has been associated with decreasing the long‐term consequences of untreated hypertension, 11 as well as a reduction in health care resource use 12 , 13 , 14 , 15 and hospitalization rates. 13
The purpose of this study was to compare 1‐year persistence and compliance rates for the major classes of commonly used antihypertensive medications in a cohort of patients previously naive to antihypertensive medication. To our knowledge, the current study is the first report to include a drug class‐level comparison of compliance and persistence of commonly prescribed antihypertensive therapies in a large US pharmacy claims database.
METHODS
This retrospective, longitudinal cohort study employed administrative pharmacy claims data to examine drug utilization in patients previously naive to antihypertensive therapy who started therapy with an angiotensin‐converting enzyme inhibitor (ACEI), angiotensin receptor blocker (ARB), calcium channel blocker (CCB), β‐blocker (BB), or diuretic. The administrative pharmacy claims database from MedImpact, a large national pharmacy benefits manager that administers prescription benefit coverage to approximately 27 million persons across the United States, was used in this study. MedImpact's database comprised employer corporations; unions; managed care organizations; health plans; insurance carriers; third‐party administrators; and local, state, and federal employee programs, and the age distribution of patients in the MedImpact database is comparable to that of the US population as estimated by US Census 2000 data.
Patients older than 18 years were identified for study cohort inclusion if they filled at least 1 prescription for a target medication during the 3‐year study identification period of January 1, 2001, through December 31, 2003. For each patient, the index drug was the first prescription filled within the identification period, and the index date was the date of the first fill. Participants included in the study cohort were required to be continuously benefit‐eligible for at least 6 months preceding and 12 months following the index date. The study was limited to patients who recently started treatment with antihypertensive therapy; thus, patients were required to have no claims for any target antihypertensive medications during the 6 months before their index date.
Patient drug utilization was studied for the 12 months following each patient's index prescription, and all analyses were performed for monotherapy to the specific index drug class. Patients who added additional medication(s) to the index drug class were included in the study; however, utilization metrics were calculated and are reported for the index drug regimen only. Utilization metrics are defined in Table I and included persistence, medication possession ratio (MPR), adherence (MPR >80%), and time to therapy discontinuation. Therapy discontinuation was defined relative to the index medication class as ending therapy and not receiving a subsequent fill within 60 days after exhausting the supply from the prior prescription. One‐year persistence was defined as the percentage of patients remaining on therapy who did not discontinue therapy with the index class. The MPR was used to assess therapy compliance. This study evaluated compliance with initially prescribed monotherapy; therefore, patients who received prescription fills for >1 antihypertensive medication on their study index date were excluded from the analysis, as were patients who received a prescription claim for an antihypertensive drug other than an ARB, ACEI, BB, CCB, or diuretic.
Table I.
Study Utilization Metrics and Definitions
| Days to therapy discontinuationa | The date of fill for the last prescription during the 12‐month study follow‐up before therapy discontinuation,a minus the index fill date, plus the days' supply of the last fill date. For patients who did not discontinue therapy with the index medication class during the study period, this was measured as the last prescription fill date plus days' supply of that prescription fill, minus the index fill date. |
| Persistence | At monthly intervals post‐index fill date (ie, month 2, 3, 4 …) and for the 12‐month study period overall, the percentage of individuals remaining on therapy who did not discontinuea therapy with the index class. |
| MPR | The sum of days' supply for all prescription fills of the index hypertension class during the follow‐up period, divided by the duration of the follow‐up period (365 days), multiplied by 100 to express as a percentage. |
| Adherence | The percentage of individuals having an MPR >80.0% and no occurrence of discontinuationa of the index class of hypertension medication. |
| aDiscontinuation is defined as ending therapy with the target medication class and not receiving a fill for the target medication within 60 days after exhausting the days supply from the prior prescription. Abbreviation: MPR, medication possession ratio. | |
The RxRisk methodology 16 was employed to assess the presence of other comorbid conditions. RxRisk uses the presence of pharmacy claims during the 6 months before the index date for medications used to treat specific conditions to identify the presence of that comorbidity (eg, a pharmacy claim for an oral antidiabetic agent is used to identify the presence of diabetes). RxRisk categories of disease‐specific states were used (eg, diabetes or no diabetes) to describe patient clinical characteristics and for adjustment of statistical comparisons for the presence of comorbid conditions.
Propensity score adjustment was performed to control for potential study selection bias resulting from provider treatment assignment. A multinomial regression model was used to estimate the probability of choosing the observed treatment choice based on patient characteristics, including patient age, sex, RxRisk disease categories, and type of benefit coverage (ie, commercial health maintenance organization [HMO], Medicaid, Medicare, or self‐insured). The inverse of this probability, or propensity score weight, was subsequently used in study multivariable logistic and linear regressions. For continuous variables, multiple variable linear regression techniques were used in pairwise comparisons of means adjusted for independent variables, which included propensity weight, patient age, patient sex, RxRisk disease categories, type of benefit coverage, average co‐pay, and concurrent cardiovascular disease‐related medications used (ie, other antihypertensive drugs not equal to the initial therapy subsequent to the index prescription date; digitalis, nitrates, antiplatelet agents, and antihyperlipidemics). Pairwise multiple logistic regression was used to calculate odds ratios to compare persistence and adherence, adjusted for the same independent variables, using diuretics as the referent group. While these techniques were used for statistical comparisons adjusting for important covariates, for descriptive purposes, crude means and proportions are included in the text and the tables, as statistical adjustment did not substantially alter any of these values.
Multivariable survival analysis techniques were used to analyze drug class persistence. Cox proportional hazards regression was used to calculate hazard ratios (Hrs), assessing differences in therapy discontinuation between classes of antihypertensive medications studied, adjusted for the same covariates used for the linear regressions listed above. The event modeled was discontinuation of therapy with the index medication class, and diuretics were used as the reference drug category. All study analyses were performed using SAS software version 9.1.3 (SAS Institute, Inc, Cary, NC).
RESULTS
The final study cohort consisted of 242,882 patients newly started on antihypertensive monotherapy. Table II summarizes the population descriptive characteristics. Mean cohort age was 54.5 years, and 56.9% were female. Overall, 34.1% of patients studied started anithypertensive therapy with a BB, followed by ACEI (32.4%), CCB (14.9%), diuretic (14.4%), and ARB (4.2%). Diuretic patients were more likely to be female (70.1%) compared with patients initially treated with an ARB (51.7%), ACEI (48.8%), CCB (60.8%), or BB (57.8%). Most patients (66.1%) had coverage through an HMO; and patients using ARBs were more likely to be self‐insured. Patient co‐payment for ARBs was highest, followed by CCBs, ACEIs, BBs, and diuretics. About 78% of the study population had at least 1 comorbid condition with hypertension. Patients with diabetes were more likely to be prescribed an ACEI or ARB than other antihypertensive medication classes.
Table II.
Study Cohort Characteristics
| Characteristics | Initial Antihypertensive Monotherapy (N=242,882) | ||||
|---|---|---|---|---|---|
| ARB (n=10,245) | ACEI (n=78,616) | CCB (n=36,246) | BB (n=82,841) | Diuretics (n=34,934) | |
| Total cohort, % | 4.2 | 32.4 | 14.9 | 34.1 | 14.4 |
| Mean age, ± SD, y | 56.2+14.6 | 55.8+15.1 | 56.2+17.5 | 52.7+16.2 | 53.6+15.3 |
| Female, % | 51.7 | 48.8 | 60.8 | 57.8 | 70.1 |
| RxRiska | |||||
| Anxiety and tension, bipolar disorder, depression, psychotic illness, ADD, % | 1577 (15.4) | 11,612 (14.8) | 6553 (18.1) | 17,352 (20.9) | 6413 (18.4) |
| Asthma, allergic rhinitis, % | 587 (5.7) | 4700 (6.0) | 2766 (7.6) | 3471 (4.2) | 2590 (7.4) |
| Cardiac disease, coronary and peripheral vascular disease, heart disease, hypertensionb, % | 921 (9.0) | 6563 (8.3) | 3569 (9.8) | 6418 (7.7) | 2012 (5.8) |
| Gastric acid disorder, IBS, % | 735 (7.2) | 5876 (7.5) | 2830 (7.8) | 6903 (8.3) | 2768 (7.9) |
| Rheumatoid arthritis, gout, % | 474 (4.6) | 2735 (3.5) | 1583 (4.4) | 2471 (3.0) | 1273 (3.6) |
| Diabetes, % | 716 (7.0) | 10830 (13.8) | 1103 (3.0) | 1871 (2.3) | 843 (2.4) |
| Thyroid disease, % | 614 (6.0) | 4208 (5.4) | 1875 (5.2) | 4321 (5.2) | 2193 (6.3) |
| Primary Market Segment | |||||
| HMO, % | 6192 (60.4) | 50,368 (64.1) | 21,592 (59.6) | 57,932 (69.9) | 24,562 (70.3) |
| Medicaid, % | 442 (4.3) | 11,000 (14.0) | 4673 (12.9) | 9154 (11.1) | 4103 (11.8) |
| Medicare, % | 703 (6.9) | 8156 (10.4) | 5035 (13.9) | 5972 (7.2) | 2285 (6.5) |
| Self‐insured, % | 2908 (28.4) | 9092 (11.6) | 4946 (13.7) | 9783 (11.8) | 3984 (11.4) |
| Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ADD, attention deficit disorder; ARB, angiotensin II receptor blocker; BB, β‐blocker; CCB, calcium channel blocker; HMO, health maintenance organization; IBS, irritable bowel syndrome; SD, standard deviation. aThe 49 RxRisk categories were consolidated into 21 categories; the 7 most prevalent groups are presented here. bThe hypertension category does not include the target medications digitalis, nitrates, antiplatelet medications, or antihyperlipidemics. | |||||
Use of other cardiovascular disease‐related medications by index drug class is included in Table III. Patients starting therapy with ARBs (30.5%) and diuretics (30.0%) were most likely to use another class of antihypertensive medication during the 12‐month study follow‐up. Patients whose index hypertension medication was an ACEI or ARB were more likely to use other (nonantihypertensive) cardiovascular disease related‐medications during the study period than patients using other drug classes. The most commonly used cardiovascular disease‐related medications were antihyperlipidemic drugs, as 27.0% of study patients had claims for these medications during the study period.
Table III.
Concurrent Use of CVD‐Related Medications by Index Class
| Concomitant CVD‐Related Medication | Initial Antihypertensive Monotherapy (N=242,882) | ||||
|---|---|---|---|---|---|
| ARB (n=10,245; 4.2%) | ACEI (n=78,616; 32.4%) | CCB (n=36,246; 14.9%) | BB (n=82,841; 34.1%) | Diuretics (n=34,934; 14.4%) | |
| Other antihypertension medication | 3125 (30.5) | 19,359 (24.6) | 10,293 (28.4) | 17,160 (20.7) | 10,479 (30.0) |
| ARB | — | 5188 (6.6) | 1147 (3.2) | 1683 (2.0) | 915 (2.6) |
| ACEI | 521 (5.1) | — | 4624 (12.8) | 9220 (11.1) | 5218 (14.9) |
| CCB | 814 (8.0) | 5875 (7.5) | — | 5168 (6.2) | 2176 (6.2) |
| BB | 907 (8.9) | 7970 (10.1) | 4100 (11.3) | — | 3941 (11.3) |
| Diuretics | 686 (6.7) | 6271 (8.0) | 2607 (7.2) | 4922 (5.9) | — |
| ARB and diuretics | 951 (9.3) | 1091 (1.4) | 556 (1.5) | 620 (0.8) | 451 (1.3) |
| ACEI and diuretics | 61 (0.6) | 1989 (2.5) | 457 (1.3) | 634 (0.8) | 879 (2.5) |
| BB and diuretics | 32 (0.3) | 143 (0.2) | 101 (0.3) | 133 (0.2) | 89 (0.3) |
| ACEI and CCB | 95 (0.9) | 723 (0.9) | 673 (1.9) | 382 (0.5) | 255 (0.7) |
| Other CVD medication | 3787 (37.0) | 30,372 (38.6) | 11,104 (30.6) | 26,544 (32.0) | 7683 (22.0) |
| Digitalis | 376 (3.7) | 3016 (3.8) | 1623 (4.5) | 2570 (3.1) | 498 (1.4) |
| Nitrates | 525 (5.1) | 4626 (5.9) | 2809 (7.8) | 8730 (10.5) | 907 (2.6) |
| Antiplatelet medications | 357 (3.5) | 3145 (4.0) | 1515 (4.2) | 4641 (5.6) | 503 (1.4) |
| Antihyperlipidemic medications | 3310 (32.3) | 26,223 (33.4) | 8070 (22.3) | 21,248 (25.7) | 6712 (19.2) |
| Values are expressed as No. (%). Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BB, β‐blocker; CCB, calcium channel blocker; CVD, cardiovascular disease. | |||||
Patients starting therapy with ARBs were the most persistent compared with those receiving other antihypertensive classes at 12 months; 51.9% of ARB patients were persistent with their index therapy, compared with 48.0% of ACEI patients, 40.3% of BB patients, 38.3% of CCB patients, and 29.9% of diuretic patients (Table IV). After adjustment for covariates and compared with diuretic users, patients receiving an ARB were 52% more likely to be persistent, patients receiving an ACEI were 43% more likely to be persistent, and those receiving a CCB or BB were both 25% more likely to be persistent.
Table IV.
Unadjusted Persistence and Compliance Metrics of Antihypertensive Monotherapy
| Anti‐HTN Drug | Persistence, No. (%) | Mean Days to Therapy Discontinuation± SD | Mean MPR ± SD | Adherence: MPR >80%, No. (%) |
|---|---|---|---|---|
| ARB (n=10,245) | 5315 (51.9) | 236.9±141.5 | 58.9±33.9 | 3945 (38.5) |
| ACEI (n=78,616) | 37,700 (48.0) | 225.0±143.1 | 59.2±34.3 | 30,806 (39.2) |
| CCB (n=36,246) | 13,895 (38.3) | 190.3±147.4 | 50.9±36.1 | 11,612 (32.0) |
| BB (n=82,241) | 33,416 (40.3) | 195.5±148.1 | 52.2±36.0 | 27,457 (33.1) |
| Diuretics (n=34,934) | 10,449 (29.9) | 164.5±141.8 | 44.5±34.5 | 8449 (24.2) |
| Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BB, β‐blocker; CCB, calcium channel blocker; HTN, hypertension; MPR, medication possession ratio; SD, standard deviation. | ||||
The mean MPR was similar for ACEI (59.2) and ARB (58.9) patients (Table IV). Adjusted for covariates, the mean MPR for patients receiving ARBs and ACEIs were not significantly different. ARB and ACEI patients had significantly higher MPRs than those receiving BBs, CCBs, and diuretics, however, all at a P value of <.0001 (data not shown). The percentage of patients classified as adherent was similar for patients receiving ACEIs (39.2%) and ARBs (38.5%) (Table IV). Furthermore, compared with diuretic patients, ARB patients were 41% more likely to be adherent; ACEI patients, 39% more likely to be adherent; and CCB and BB patients, 23% more likely to be adherent after adjusting for covariates.
ARB patients had the longest time (days) to therapy discontinuation (mean = 236.9 days), compared with patients utilizing other drug classes (Table IV). Cox proportional hazards modeling was used to examine therapy discontinuation, using patients taking a diuretic as the reference group and controlling for independent demographic and clinical variables. Compared with patients who started diuretic therapy, patients who began antihypertensive monotherapy with ARBs (HR, 0.59; P<.0001), ACEIs (HR, 0.64; P<.0001), CCBs (HR, 0.86; P<.0001), or BBs (HR, 0.82; P<.0001) were all significantly less likely to discontinue their index therapy. Patients who used additional antihypertensive medications, with the exception of those who added an ACEI or ACEI/diuretic combinations, during the year subsequent to the index prescription were also more likely to discontinue the index medication class. As shown in the Figure, most patients who discontinued index therapy did so within the first 30 days of starting therapy, and the differences between index drug classes observed at 12 months post‐index date were largely evident at 1 month post‐index date.
Figure.
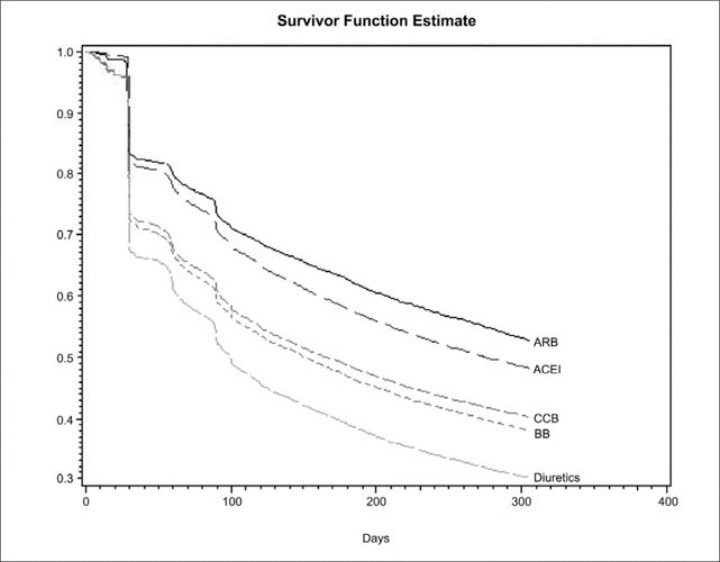
Time to therapy discontinuation of antihypertension monotherapy: 1‐year assessment (adjusted survival analysis). This depicts the proportion of study patients by antihypertensive medication class who remained persistent with index therapy (y axis) during the year subsequent to the index study claim (days subsequent to index date depicted on x axis). ARB patients were most likely to remain on therapy, closely followed by ACEI patients. Diuretic patients were least likely to remain on the index monotherapy regimen. ARB indicates angiotensin II receptor blocker; ACEI, angiotensin‐converting enzyme inhibitor; CCB, calcium channel blocker; BB, β‐blocker.
DISCUSSION
This retrospective study found that patient persistence and compliance with newly initiated monotherapy differed for the 5 major classes of commonly used antihypertensive medications. Specifically, initiating therapy with a diuretic was associated with worse persistence at 12 months post‐therapy initiation compared with starting therapy with an ARB, ACEI, CCB, or BB. Overall, utilization metrics were highest for ARBs and slightly lower for ACEIs, followed by BBs and CCBs and, last, diuretics. These findings are consistent with other reports of better persistence with specific ARBs as compared with other antihypertensive agents. Previous studies of specific ARBs have demonstrated better persistence with valsartan as compared with amlodipine or lisinopril 10 or better persistence with ARBs compared with ACEIs, CCBs, BBs, and diuretics. 9 An antihypertensive class comparison of 46,458 patients in a Canadian health care database found that patients taking ARBs, as a class, had the highest persistence as compared with those receiving ACEIs, BBs, CCBs, and diuretics. 17 Caro and colleagues 18 also found that the choice of initial antihypertensive medication class had a significant impact on patient persistence, though ARBs were not studied.
Perhaps the most striking study finding was that for all drug utilization metrics studied, diuretics were consistently an outlier compared with other antihypertensive classes. Results were consistently worse for diuretics than for other classes, despite diuretics having the lowest average patient co‐pay amount. Although significant (P=.0090), the magnitude of the effect of patient co‐pay amount as a predictor of therapy discontinuation in the Cox proportional hazards model was marginal. Compared with patients receiving diuretics, patients who had recently begun ARB therapy were 52% more likely (odds ratio [OR], 1.52; 95% confidence interval [CI], 1.49–1.54), and those who had recently begun ACEI therapy 43% more likely (OR, 1.43; 95% CI, 1.41–1.43) to be persistent at 12 months following the start of antihypertensive medication use. In our study of a national pharmacy claims database with 242,882 patients newly treated with antihypertensive medications over 2 years, this difference may have important implications. For example, if diuretic patients had demonstrated persistence comparable to ARB patients, an additional 7682 patients (22% of the entire new‐start diuretic cohort) would have remained on therapy at 1 year. In addition, the duration of medication usage before therapy discontinuation was 72.4 days longer in ARB patients and 60.5 days longer in ACEI patients as compared with diuretics.
Class‐specific differences in patient antihypertensive medication compliance and persistence may have important health care cost implications. Studies have consistently demonstrated an increase in total health care expenditures for patients who are noncompliant with prescribed hypertension therapy regimens in usual‐care settings. 12 , 13 , 14 , 15 In a Medicaid population, McCombs and colleagues 12 demonstrated that patients with interrupted antihypertensive drug therapy used an additional $873 per patient in health care costs during the first year. A recent study using administrative claims data for both managed care organization and traditional fee‐for‐service patients from a large pharmacy benefits manager found that greater patient compliance with antihypertensive therapy was associated with both lower medical costs and decreased risk of hospitalization. 13
An important question raised by this study is whether differences in persistence have more long‐term implications in the future treatment of patients who discontinue therapy with initially prescribed monotherapy. Other studies have shown a link between persistence and adverse effects from the treatment medication. 19 , 20 Consistent with this study's persistence results, ARBs have generally been found to have the best tolerability profile of antihypertensive therapeutic classes. 21 , 22 , 23 In our study population, the index medication was a patient's first exposure to antihypertensive medication of any kind. Failure to tolerate initial antihypertensive medication may also influence whether and when a different medication is started following the initial therapy cessation.
Using a Canadian database, another study by Bourgault and associates 24 found that compared with those receiving ARBs, patients using ACEIs, CCBs, BBs, or diuretics had a higher likelihood of therapy discontinuation, with the highest likelihood of discontinuation associated with diuretics (HR, 1.92; 95% CI, 1.73–2.14). Furthermore, in the year following discontinuation of index therapy, 54% to 75% of patients who discontinued began a second course of antihypertensive treatment. While 75% of patients who originally discontinued ARB therapy later began a second course of treatment, patients who initially used and discontinued a BB (54%) or a diuretic (59%) were the least likely to restart antihypertensive therapy. 24 Further research is needed to understand the effect of persistence with initial antihypertensive therapy on subsequent patient management in a US population.
Limitations
Claims‐based retrospective studies such as this provide useful insight into patient behavior in a usual‐care setting that is difficult to assess in a structured clinical trial. The use of pharmacy claims to evaluate metrics such as persistence and compliance is valuable because many methods of evaluating patient medication consumption are subject to patient recall bias, which is not a limitation of claims‐based studies.
Though the current study provides insight into patient drug‐taking behavior in a natural setting, it has some important limitations. Medical claims information was not available to confirm patient diagnosis of hypertension, and some of the medications studied had multiple indications in addition to hypertension. Therefore, some of the patients studied may not have had a diagnosis of hypertension, and it is difficult to predict the impact of this limitation. While the study design, a retrospective database analysis using administrative pharmacy claims, has advantages for evaluating medication persistence and compliance, patients were not randomized to treatment. Consequently, selection bias resulting from the physician's choice of initial antihypertensive therapy based on consideration of patient clinical characteristics may play a role in study findings. Although the propensity score weighting used in the statistical analyses controlled for this to some extent, we cannot rule out the possibility that factors that were not available for analysis, such as patient BMI and smoking status, may have played a role in either provider agent selection or acted as study confounders.
It is also possible that study results may have been influenced by advertising or promotional campaigns, which may stress the benefits of newer therapies as compared with older, generic therapies such as diuretics. There may be patients who are symptom‐free and have well‐controlled BP whose medication is changed because of an “ask your doctor” advertisement or a promotional visit from a drug representative or a medical symposium. It is also possible that provider or patient geographic region may have influenced study findings, and this was not included in our study. Study persistence and compliance were measured by patient prescription refill patterns and not the amount of actual drug consumed by the patient; however, other studies have shown that these are highly correlated and have supported the use of pharmacy claims data for the evaluation of medication utilization. 25 , 26 Finally, since our study did not include fixed‐combination agents, it is possible that we overestimated discontinuation for patients who, in fact, switched from monotherapy with a single agent to that agent as a component of the fixed‐combination regimen. The observed differences in the frequency of concomitant use of other antihypertensive medications (Table III) may have influenced the compliance rates for several cohorts; however, the degree to which this influenced each cohort's compliance rates was not determined.
Prescribers should consider all sources of information, including information from clinical trials, hypertension treatment guidelines, and results of studies of patient medication‐taking behavior in the real world, given the differences in adherence various antihypertensive treatment options.
CONCLUSIONS
This observational study found that among patients who began new antihypertensive monotherapy, patients receiving ARBs were the most persistent (52%), followed by those taking ACEIs (48%), BBs (40%), CCBs (38%), and diuretics (30%). The difference between ARB and ACEI patients' persistence results is small; on average, ARB patients remained on therapy 12 days longer than ACEI patients. For all utilization metrics studied, ARBs and ACEIs performed best, followed by BBs and CCBs and, last, diuretics. In fact, diuretics consistently performed the most poorly on all utilization metrics; on average, patients remained on therapy 2.5 months longer with an ARB, and 2 months longer with an ACEI, than a diuretic. Utilization statistics, however, may have overestimated discontinuation of diuretics in patients who were switched from monotherapy with this index drug to a fixed‐combination regimen. These findings may have important implications, particularly because research has suggested that a significant proportion of those patients who discontinue initially prescribed monotherapy may experience an extended lapse in their hypertension treatment. 24 Further research is warranted to determine the relationship between therapy persistence in a real‐world setting and hypertension control and to elucidate the impact of a lack of persistence with initially prescribed antihypertensive therapy on long‐term hypertension control and outcomes.
Acknowledgements and disclosures:
Dr Preblick and Ms Frech‐Tamas are employed by Novartis Pharmaceuticals Corporation, the maker of several antihypertensive drugs including an angiotensin II receptor blocker. Dr Patel, Ms Remigio‐Baker, Dr Thiebaud, and Dr Mehta have no conflicts of interest to disclose at present. Dr Thiebaud and Ms Remigio‐Baker were employees during the time of data analysis and manuscript preparation but are no longer employed with MedImpact. Ms Remigio‐Baker is currently employed by Hollis Eden Pharmaceuticals. Dr Thiebaud is currently employed by Pfizer Health Solutions. At the time of the study, Dr Mehta was a fellow with Scott & White, the University of Texas at Austin and Novartis; she is currently employed by WellPoint NextRx, West Hills, CA. Portions of this study were presented as a poster at the Academy of Managed Care Pharmacy's 2005 Educational Conference, Nashville, TN, October 5–8, 2005. This study was funded by Novartis Pharmaceuticals Corporation.
References
- 1. Fields LE , Burt VL , Cutler JA , et al. The burden of adult hypertension in the United States 1999 to 2000: a rising tide . Hypertension . 2004. ; 44 : 398 – 404 . [DOI] [PubMed] [Google Scholar]
- 2. Ong KL , Cheung BMY , Man YB , et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004 . Hypertension . 2007. ; 49 : 69 – 75 . [DOI] [PubMed] [Google Scholar]
- 3. Hajjar I , Kotchen TA . Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000 . JAMA . 2003. ; 290 : 199 – 206 . [DOI] [PubMed] [Google Scholar]
- 4. US Department of Health and Human Services . Healthy People 2010 . 2nd ed. Washington, DC : US Government Printing Office; ; 2000. . [Google Scholar]
- 5. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report . JAMA . 2003. ; 289 : 2560 – 2572 . [DOI] [PubMed] [Google Scholar]
- 6. Morgan S , Bassett KL , Wright JM , et al. First‐line first? Trends in thiazide diuretic prescribing for hypertensive seniors . PLoS Med . 2005. ; 2 ( 4 ): e80 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group . Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs diuretic . JAMA . 2002. ; 288 : 2981 – 2997 . [DOI] [PubMed] [Google Scholar]
- 8. Pablos‐Mendez A , Barr G , Shea S . Run‐in periods in randomized trials . JAMA . 1998. ; 279 : 222 – 225 . [DOI] [PubMed] [Google Scholar]
- 9. Conlin PR , Gerth WC , Fox J , et al. Four‐year persistence patterns among patients initiating therapy with the angiotensin II receptor antagonist losartan versus other antihypertensive drug classes . Clin Ther . 2001. ; 23 : 1999 – 2010 . [DOI] [PubMed] [Google Scholar]
- 10. Wogen J , Kreilick CA , Livornese RC , et al. Patient adherence with amlodipine, lisinopril, or valsartan therapy in a usual‐care setting . J Manag Care Pharm . 2003. ; 9 : 424 – 429 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cramer JA . Consequences of intermittent treatment for hypertension: the case for medication compliance and persistence . Am J Manag Care . 1998. ; 4 : 1563 – 1568 . [PubMed] [Google Scholar]
- 12. McCombs JS , Nichol MB , Newman CM , et al. The costs of interrupting antihypertensive drug therapy in a Medicaid population . Med Care . 1994. ; 32 : 214 – 226 . [DOI] [PubMed] [Google Scholar]
- 13. Sokol MC , McGuigan KA , Verbrugge RR , et al. Impact of medication adherence on hospitalization risk and healthcare cost . Med Care . 2005. ; 43 : 521 – 530 . [DOI] [PubMed] [Google Scholar]
- 14. Rizzo JA , Simons WR . Variations in compliance among hypertensive patients by drug class: implications for health care costs . Clin Ther . 1997. ; 19 : 1446 – 1457 . [DOI] [PubMed] [Google Scholar]
- 15. Caro JJ , Speckman JL . Existing treatment strategies: does noncompliance make a difference ? J Hypertens Suppl . 1998. ; 16 : S31 – S34 . [PubMed] [Google Scholar]
- 16. Fishman PA , Goodman MJ , Hornbrook MC , et al. Risk adjustment using automated ambulatory pharmacy data: the RxRisk model . Med Care . 2003. ; 41 ( 1 ): 84 – 99 . [DOI] [PubMed] [Google Scholar]
- 17. Marentette MA , Gerth WC , Billings DK , et al. Antihypertensive persistence and drug class . Can J Cardiol . 2002. ; 18 : 649 – 656 . [PubMed] [Google Scholar]
- 18. Caro JJ , Speckman JL , Salas M , et al. Effect of initial drug choice on persistence with antihypertensive therapy: the importance of actual practice data . CMAJ . 1999. ; 160 : 41 – 46 . [PMC free article] [PubMed] [Google Scholar]
- 19. Burnier M , Hess B , Greminger P , et al. Determinants of persistence in hypertensive patients treated with irbesartan: results of a postmarketing survey . BMC Cardiovasc Disord . 2005. ; 5 : 13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Grégoire JP , Moisan J , Guibert R , et al. Determinants of discontinuation of new courses of antihypertensive medications . J Clin Epidemiol . 2002. ; 55 : 728 – 735 . [DOI] [PubMed] [Google Scholar]
- 21. Black HR , Graff A , Shute D , et al. Valsartan, a new angiotensin II antagonist for the treatment of essential hypertension: efficacy, tolerability and safety compared to an angiotensin‐converting enzyme inhibitor, lisinopril . J Hum Hypertens . 1997. ; 11 : 483 – 489 . [DOI] [PubMed] [Google Scholar]
- 22. Corea L , Cardoni O , Fogari R , et al. Valsartan, a new angiotensin II antagonist for the treatment of essential hypertension: a comparative study of the efficacy and safety against amlodipine . Clin Pharmacol Ther . 1996. ; 60 : 341 – 346 . [DOI] [PubMed] [Google Scholar]
- 23. Gregoire JP , Moisan J , Guibert R , et al. Tolerability of antihypertensive drugs in a community‐based setting . Clin Ther . 2001. ; 23 : 715 – 726 . [DOI] [PubMed] [Google Scholar]
- 24. Bourgault C , Senecal M , Brisson M , et al. Persistence and discontinuation patterns of antihypertensive therapy among newly treated patients: a population‐based study . J Hum Hypertens . 2005. ; 19 : 607 – 613 . [DOI] [PubMed] [Google Scholar]
- 25. Christensen DB , Williams B , Goldberg HI , et al. Comparison of prescription and medical records in reflecting patient antihypertensive drug therapy . Ann Pharmacother . 1994. ; 28 : 99 – 104 . [DOI] [PubMed] [Google Scholar]
- 26. Choo PW , Rand CS , Inui TS , et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy . Med Care . 1999. ; 37 : 846 – 857 . [DOI] [PubMed] [Google Scholar]


