Abstract
Many quality improvement strategies have focused on improving blood pressure control, and these strategies can target the patient, the provider, and/or the system. Strategies that seem to have the biggest effect on blood pressure outcomes are team change, patient education, facilitated relay of clinical information, and promotion of self‐management. Barriers to effective blood pressure control can affect the patient, the physician, the system, and/or “cues to action.”We review the barriers to achieving blood pressure control and describe current and potential creative strategies for optimizing blood pressure control. These include home‐based disease management, combined patient and provider education, and automatic decision support systems. Future research must address which components of quality improvement interventions are most successful in achieving blood pressure control.
Many quality improvement (QI) strategies have focused on improving blood pressure control. QI strategies can target the patient, the provider, the system or any combination of these. To achieve optimum blood pressure control, it is important to know which QI strategies or combinations of QI strategies are most effective. Then we can determine how to implement effective strategies in clinical practice.
EVIDENCE FOR QI STRATEGIES AND BLOOD PRESSURE CONTROL
In a prior systematic review, 1 we addressed the questions of whether QI strategies are effective in producing clinically significant reductions in blood pressure and which QI strategies are most effective in achieving blood pressure reduction.
We defined a QI strategy as follows: an intervention aimed at reducing the quality gap (the difference between health care processes or outcomes observed in practice and those potentially obtainable based on current professional knowledge) for a group of patients representative of those encountered in routine practice. 2 We classified QI strategies into 9 categories: 4 of these categories focused on the provider, 3 focused on the patient, and 2 focused on the system. The categories and their descriptions are described in Table I. In the analysis, we included trials, controlled before‐and‐after studies, and interrupted time series. We included studies that reported quantitative blood pressure outcomes, either actual change in blood pressure or change in the percent age of individuals with blood pressure within a target blood pressure range.
Table I.
Classification of Quality Improvement Strategies
| Type of Strategy | Definition/Example |
|---|---|
| Provider‐Focused | |
| Provider education | Materials given to providers about appropriate care for patients |
| Provider reminders | Prompts to perform specific actions |
| Provider audit and feedback | Clinical performance information given to providers |
| Facilitated relay of clinical data | Clinical data collected from patients and transmitted to the provider; data not provided in clinical visits (eg, transmission of home blood pressure readings) |
| Patient‐Focused | |
| Patient education | Materials given to patients |
| Patient reminders | Prompts to keep appointments or adhere to regimens |
| Promotion of self‐management | Providing access to resources that help patients in self‐management (eg, providing a home blood pressure kit) |
| System‐Focused | |
| Team change | Creation of new roles, new team members, disease management |
| Financial incentives | Changes in reimbursement |
IMPACT OF QI STRATEGIES ON BLOOD PRESSURE CONTROL
We identified 44 studies that included 57 comparisons of QI strategies (some articles had more than one intervention). The studies are listed in detail in our prior publication. 1 A table with comparative details about the studies including setting, type(s) of QI strategies used, and outcomes evaluated is available from the authors by request. The majority of studies evaluated more than one QI strategy (median of 3), which made it difficult to determine which individual QI strategy was more effective. In addition, there was no clear association between increasing the number of strategies and impact on blood pressure control.
Almost all QI interventions were associated with some reduction in blood pressure. The most frequently used strategies were team change and patient education (in combination with other strategies). Team change was used in 36 of the 57 comparisons, and patient education was used in 28 of the 57 comparisons. Strategies that seemed to have the biggest effect on blood pressure outcomes were team change, patient education, facilitated relay of clinical information, and promotion of self‐management. The impact of the different strategies is reported in Table II.
Table II.
Effect of QI Strategies on Blood Pressure Control
| Type of QI | Median Reduction in SBP, mm Hg | Median Reduction in DBP, mm Hg | Median Absolute Increase in Proportion of Patients in Whom SBP in a Certain Range Was Achieved | Median Absolute Increase in Proportion of Patients in Whom DBP in a Certain Range Was Achieved |
|---|---|---|---|---|
| Provider‐Focused | ||||
| Provider reminders | 1.2 [1.0, 1.9] n=6 | 0.3 [−0.2, 1.7] n=6 | NA n=0 | 4.5 [2.0, 7.0] n=2 |
| Facilitated relay of clinical data | 8.0 [2.5, 12.3] n=16 | 1.8 [−0.1, 4.5] n=18 | 25.1 [17.0, 34.2] n=4 | 2.0 [1.6, 5.0] n=5 |
| Audit and feedback | 1.5 [1.2, 1.7] n=3 | 0.6 [0.4, 1.0] n=4 | −3.5 [−5.7, −1.4] n=2 | 2.0 [1.7, 4.3] n=6 |
| Provider education | 3.3 [1.2, 5.4] n=11 | 0.6 [−0.7, 3.4] n=16 | 10.9 [1.4, 13.1] n=6 | 3.5 [1.7, 11.3] n=6 |
| Patient‐Focused | ||||
| Patient education | 8.1 [3.3, 11.8] n=18 | 3.8 [0.6, 6.7] n=21 | 19.2 [11.4, 33.2] n=8 | 17.0 [11.4, 24.5] n=7 |
| Promotion of self‐management | 3.3 [2.6, 10.1] n=9 | 2.8 [0.4, 6.7] n=13 | 13.4 n=1 | 9.4 [5.3, 11.4] n=3 |
| Patient reminders | 3.3 [2.3, 4.5] n=5 | 0.4 [−2.4, 5.0] n=9 | NA n=0 | 2.0 [1.1, 9.4] n=5 |
| System‐Focused | ||||
| Team change | 9.7a [4.2, 14.0] n=20 | 4.2a [0.2, 6.8] n=24 | 21.8 [9.0, 33.8] n=12 | 17.0 [5.7, 24.5] n=7 |
| Financial incentives | −13.3 n=1 | 0.0 [−2.0, 2.5] n=3 | NA n=0 | 4.2 [−1.1, 9.4] n=2 |
| All comparisons | 4.5 [1.5, 11.0] n=33 | 2.1 [−0.2, 5.0] n=43 | 16.2 [10.3, 32.2] n=14 | 6.0 [1.5, 17.5] n=16 |
| Abbreviations: DBP, diastolic blood pressure; QI, quality improvement; SBP, systolic blood pressure; Values in brackets are interquartile rangeb and n = number of comparisons. a P<.05 for Mann Whitney analyses of reductions in SBP and DBP comparing studies with the QI strategy to those without it. No comparable statistical analyses were feasible for proportion of patients in whom a certain SBP or DBP range was achieved. bWhen n=2, brackets show the actual results of each study rather than interpolated interquartile range. Reprinted with permission from Walsh et al. 1 | ||||
All of the team change strategies involved assigning some of the responsibilities for the patient's care to someone other than the physician. The other providers included pharmacists, nurses, physician assistants, and work site physicians. In some studies, all responsibilities for hypertension care were transferred to the other provider; in other studies the physician and the provider shared responsibility; and in others the physician retained full responsibility for interacting with the patient, but the other provider provided some type of support. We defined these team change strategies as “all communication transferred,”“shared responsibility,” and “doctor‐focused,” respectively. 1
An example of “all communication transferred” involved a pharmacist meeting with the patient, making medication adjustments and dose changes, and then communicating with the patient's physician. 3 , 4 , 5 , 6 An example of “shared responsibility” was a pharmacist providing evidence‐based treatment recommendations to a patient's physician 7 , 8 , 9 and counseling the patient on nonpharmacologic blood pressure reduction strategies, but not actually adjusting the medications. Finally, an example of the “doctor‐focused” intervention involved the pharmacist providing support such as prompts or supports to the provider, but the provider still being the only one directly interacting with the patient. 10 , 11 , 12 Other features of team change interventions that were common were having a standard algorithm for adding drugs 13 , 14 and the inclusion of home blood pressure monitoring. 15 , 16 , 17
Not only was team change the most commonly used QI intervention but it also appeared to have the biggest impact on blood pressure. In the studies that included team change as a QI component, the median reduction in systolic blood pressure was 9.7 (interquartile range: 4.2, 14.0) mm Hg, and the median reduction in diastolic blood pressure was 4.2 (interquartile range: 0.2, 6.8) mm Hg. 1
In summary, QI strategies can lead to improved blood pressure control. Many studies included more than one strategy, making it difficult to determine which strategy was most effective. QI interventions that included team change seemed to have the biggest impact on blood pressure outcomes. Common features of successful team change strategies included transferring some of the patient's care to someone other than the physician, having a standard protocol for adding drugs, and including home blood pressure monitoring.
IMPLEMENTING SUCCESSFUL QI STRATEGIES IN CLINICAL PRACTICE
If QI strategies work in improving blood pressure control, why are they not used more? How do we decide which strategy to use and when to use it?How do we decide which strategy will work best in a particular clinical setting? What are the barriers to effective implementation of QI strategies?
Overcoming the Barriers to Achieving Blood Pressure Control
Since QI strategies can target the patient, the physician, or the system, it is important to consider the impact of all these factors on achieving the goal of blood pressure control. The provision and receipt of preventive care takes place within the patient‐physician interaction. The Systems Model of Clinical Preventive Care focuses on the interaction between the patient and the physician within the context of the health care system. 18 The patient and the physician are affected by health care system factors and by certain cues to action (such as symptoms or reminders). Barriers can occur at any level, including at the level of the patient, the physician, or the system or in cues to action (Figure).
Figure.
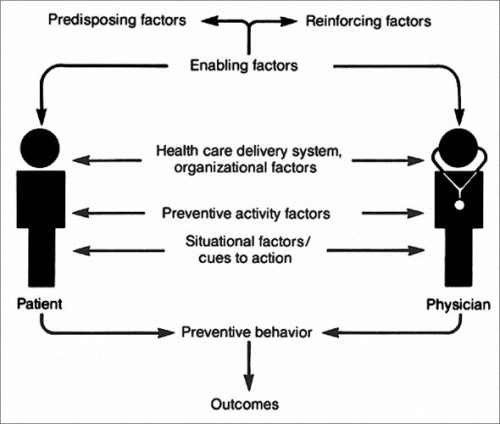
A Systems Model of Clinical Preventive Care: a model whereby patients and physicians are affected by predisposing, enabling, and reinforcing factors. Each of them is also influenced by the system and by various cues to action. Together, the patient and the physician interact to achieve the desired result, in this case, well controlled blood pressure. Reprinted with Permission from Walsh and McPhee. 18
Patient Barriers. Many patient barriers to hypertension control have been described. These barriers include not thinking that treating high blood pressure is important, not taking medication as directed, not knowing target blood pressure levels, or being reluctant to add another medication to an existing regimen. 19 , 20 , 21
Provider Barriers. Provider barriers include uncertainty about conflicting recommendations, being willing to accept an elevated systolic blood pressure, not viewing hypertension control as a priority, distraction by multiple other health issues, and lack of time. 21 , 22 , 23 An interesting study of comments provided by primary care providers as they saw patients with hypertension in clinic revealed barriers as perceived by the providers. 24 In this study, clinicians commonly reported that they did not intensify the antihypertensive regimen when the blood pressure level was above target because recorded blood pressure values were not representative of the patients' typical blood pressure; hypertension was not a clinical priority for the visit; or patients were nonadherent to medications already prescribed. Lack of awareness is another potential barrier. In another recent study, physicians significantly overestimated their adherence to blood pressure treatment guidelines, which suggests that physicians are not aware of how well they are or are not doing. 25
Systems Barriers. Often, the health care system is not organized in such a way as to facilitate efficient care. In a recent meta‐analysis of interventions to increase the use of adult immunization and cancer screening services, rates of cancer screening were most likely to improve when some type of organizational change occurred, which often involved taking some of the responsibility for the preventive activity out of the hands of the physician or simplifying the physician's task. 26 Similarly, we found that the QI interventions that had the most impact on blood pressure control were those that involved team change, including assigning some of the responsibility for the patient's care to someone other than the physician. 1
Sometimes there is resistance to the team change approach. Models for primary care such as the Chronic Care Model 27 and the Medical Home 28 stress the importance of continuity of care as well as the effective use of teams. However, there is concern that increased use of teams may result in decreased contact with the primary care provider, which may lessen patients' satisfaction with their primary care relationship. 29 , 30 In addition, such a systems change requires the coordination of efforts of many people to ensure success.
Cues to Action
Cues to action are triggers such as a chart flag for the physician to perform a preventive activity and include reminders to the patient and/or the clinician that the patient needs some focus on blood pressure at the visit.
A successful QI intervention will address multiple barriers, including patient‐perceived and physician‐perceived barriers; will use systems changes to simplify the process for the physician; and will include reminders or cues to action.
Current and Potential Examples of Successful Strategies
Since the publication of our systematic review, several studies have been published that creatively address patient, physician, and systems barriers simultaneously to achieve QI. One recent study focused on combined patient and physician education. Physicians received either (1) provider education alone, (2) provider education and provider alerts, or (3) provider education, provider alerts, and patient education. All providers received electronic mail with a direct link to the JNC Hypertension management guidelines. 31 Those who received a provider alert also received electronic notifications of the patient's last 3 blood pressures measurements. The patient education component consisted of a letter with advice about medical and lifestyle blood pressure treatments. The addition of patient education had a significant impact over provider education or provider education plus provider alerts. 32 Thus, targeting both the patient and the physician can have a significant impact over targeting the physician alone.
A suggested approach that focuses on patient, provider, and systems barriers but that has yet to be tested focuses on home‐based disease management. In this scenario, rather than the patient periodically visiting the physician, the management would shift to the home: health information technology would be used to monitor and transmit patients' home blood pressure measurements, and team members such as nurses, pharmacists, and physician assistants would make patient care and management decisions with physician oversight. In this model, more patients can be managed than in the current system. In addition, the intensity of the intervention could be adjusted as needed. Patients would assume responsibility for their hypertension and play an important role in its management. 33
An example of an intervention that takes place in the patient's home is the Hypertension Intervention Nurse Telemedicine Study (HINTS), in which patients receive (1) usual care, (2) nurse‐administered tailored behavioral intervention, (3) nurse‐administered medication management according to a decision support system, or (4) a combination of the 2 interventions. The behavioral intervention is tailored to patient needs regarding adherence with medication regimens and health behaviors. Blood pressure control will be measured as the outcome. This intervention includes a patient dimension (tailored behavioral intervention and medication management) as well as a systems change (the nurse plays a bigger role in hypertension control). 34
An innovative tool to assist primary care providers in adhering to hypertension guidelines is the Assessment and Treatment of Hypertension, Evidence‐Based Automation Decision Support System (ATHENA‐HTN). 35 , 36 ATHENA‐HTN is an automatic guideline‐based decision support system designed to be integrated with an existing electronic health record system to display recommendations for management of hypertension to primary care providers as they are seeing patients. It has been integrated with the Computerized Patient Record System (CPRS) at the Department of Veterans Affairs (VA) and is in use at several large VA medical centers. ATHENA‐HTN is also being used in HINTS, described above, in a study arm in which nurses monitoring patients' home blood pressure use the ATHENA‐HTN system to prepare potential medication changes for review/authorization by a physician. This system could also be used in pharmacist‐managed hypertension programs. Automated decision support systems such as ATHENA‐HTN can be part of an overall hypertension QI strategy that includes roles for several members of the interdisciplinary team.
CONCLUSIONS
Although we have made progress in hypertension control, we still have not reached the Healthy People 2010 goal of blood pressure control in at least 50% of individuals with hypertension. 37 Barriers to hypertension control can occur at the level of the patient, the provider, or the system. QI strategies can be patient‐focused, provider‐focused, or system‐focused; QI strategies that target several of these simultaneously and those that include team change are most likely to be successful. In addition, taking some of the responsibility out of the hands of the physician is associated with improved blood pressure control.
Promising interventions target the patient, the provider, and the health care system. Creative strategies focus on increasing patient involvement in blood pressure control and include home‐based disease management, combined patient and provider education, and automated decision support systems. Future research should continue to creatively address which components of QI interventions are most successful in achieving blood pressure control.
Disclosures:
The Assessment and Treatment of Hypertension, Evidence‐Based Automation Decision Support System is jointly owned by the Department of Veterans Affairs and Stanford University.
References
- 1. Walsh JM, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44(7):646–657. [DOI] [PubMed] [Google Scholar]
- 2. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies: Volume 1—Series Overview and Methodology. Structured Abstract. Rockville, MD: Agency for Health Research and Quality; 2004. [PubMed] [Google Scholar]
- 3. Blenkinsopp A, Phelan M, Bourne J, et al. Extended adherence support by community pharmacists for patients with hypertension: a randomised controlled trial. Int J Pharm Pract. 2000;8:3165–3175. [Google Scholar]
- 4. Campbell NC, Ritchie LD, Thain J, et al. Secondary prevention in coronary heart disease: a randomised trial of nurse led clinics in primary care. Heart. 1998;80(5):447–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Curzio JL, Rubin PC, Kennedy SS, et al. A comparison of the management of hypertensive patients by nurse practitioners compared with conventional hospital care. J Hum Hypertens. 1990;4(6):665–670. [PubMed] [Google Scholar]
- 6. Garcia‐Pena C, Thorogood M, Armstrong B, et al. Pragmatic randomized trial of home visits by a nurse to elderly people with hypertension in Mexico. Int J Epidemiol. 2001;30(6):1485–1491. [DOI] [PubMed] [Google Scholar]
- 7. Bogden PE, Abbott RD, Williamson P, et al. Comparing standard care with a physician and pharmacist team approach for uncontrolled hypertension. J Gen Intern Med. 1998;13(11):740–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Borenstein JE, Graber G, Saltiel E, et al. Physician‐pharmacist comanagement of hypertension: a randomized, comparative trial. Pharmacotherapy. 2003;23(2):209–216. [DOI] [PubMed] [Google Scholar]
- 9. Carter BL, Barnette DJ, Chrischilles E, et al. Evaluation of hypertensive patients after care provided by community pharmacists in a rural setting. Pharmacotherapy. 1997;17(6):1274–1285. [PubMed] [Google Scholar]
- 10. Goldberg HI, Wagner EH, Fihn SD, et al. A randomized controlled trial of CQI teams and academic detailing: can they alter compliance with guidelines? Jt Comm J Qual Improv. 1998;24(3):130–142. [DOI] [PubMed] [Google Scholar]
- 11. McGhee SM, McInnes GT, Hedley AJ, et al. Coordinating and standardizing long‐term care: evaluation of the west of Scotland shared‐care scheme for hypertension. Br J Gen Pract. 1994;44(387):441–445. [PMC free article] [PubMed] [Google Scholar]
- 12. Siscovick DS, Strogatz DS, Wagner EH, et al. Provider‐oriented interventions and management of hypertension. Med Care. 1987;25(3):254–258. [DOI] [PubMed] [Google Scholar]
- 13. Krishan I, Davis CS, Nobrega FT, et al. The Mayo three‐community hypertension control program. IV. Five‐year outcomes of intervention in entire communities. Mayo Clin Proc. 1981;56(1):3–10. [PubMed] [Google Scholar]
- 14. Solomon DK, Portner TS, Bass GE, et al. Clinical and economic outcomes in the hypertension and COPD arms of a multicemeter outcomes study. J Am Pharm Assoc (Wash). 1998;38(5);574–585. [DOI] [PubMed] [Google Scholar]
- 15. Earp JA, Ory MG, Strogatz DS. The effects of family involvement and practitioner home visits on the control of hypertension. Am J Public Health. 1982;72(10):1146–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Logan AG, Milne BJ, Flanagan PT, et al. Clinical effectiveness and cost‐effectiveness of monitoring blood pressure of hypertensive employees at work. Hypertension. 1983;5(6):828–836. [DOI] [PubMed] [Google Scholar]
- 17. Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy. 2000;20(11):1384–1389. [DOI] [PubMed] [Google Scholar]
- 18. Walsh JM, McPhee SJ. A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Q. 1992;19(2):157–175. [DOI] [PubMed] [Google Scholar]
- 19. Dean SC, Kerry SM, Cappuccio FP, et al. Pilot study of potential barriers to blood pressure control in patients with inadequately controlled hypertension. Fam Pract. 2007;24(3):259–262. [DOI] [PubMed] [Google Scholar]
- 20. Oliveria SA, Chen RS, McCarthy BD, et al. Hypertension knowledge, awareness, and attitudes in a hypertensive population. J Gen Intern Med. 2005;20(3):219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician‐related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162(4):413–420. [DOI] [PubMed] [Google Scholar]
- 22. Ferrari P, Hess L, Pechere‐Bertschi A, et al. Reasons for not intensifying antihypertensive treatment (RIAT): a primary care antihypertensive intervention study. J Hypertens. 2004;22(6):1221–1229. [DOI] [PubMed] [Google Scholar]
- 23. Mottur‐Pilson C, Snow V, Bartlett K. Physician explanations for failing to comply with “best practices”. Eff Clin Pract. 2001;4(5):207–213. [PubMed] [Google Scholar]
- 24. Lin ND, Martins SS, Chan AS, et al. Identifying barriers to hypertension guideline adherence using clinician feedback at the point of care. AMIA Annu Symp Proc. 2006:494–498. [PMC free article] [PubMed] [Google Scholar]
- 25. Steinman MA, Fischer MA, Shlipak MG, et al. Clinician awareness of adherence to hypertension guidelines. Am J Med. 2004;117(10):747–754. [DOI] [PubMed] [Google Scholar]
- 26. Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta‐analysis. Ann Intern Med. 2002;136(9):641–651. [DOI] [PubMed] [Google Scholar]
- 27. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20(6):64–78. [DOI] [PubMed] [Google Scholar]
- 28. Medical Home Initiatives for Children With Special Needs Project Advisory Committee . Policy statement: organizational principles to guide and define the child health care system and/or improve the health of all children. Pediatrics. 2004;113(5 suppl):1545–1547. [PubMed] [Google Scholar]
- 29. Rodriguez HP, Rogers WH, Marshall RE, et al. Multidisciplinary primary care teams: effects on the quality of clinician‐patient interactions and organizational features of care. Med Care. 2007;45(1):19–27. [DOI] [PubMed] [Google Scholar]
- 30. Wagner EH, Reid RJ. Are continuity of care and teamwork incompatible? Med Care. 2007;45(1):6–7. [DOI] [PubMed] [Google Scholar]
- 31. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 32. Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145(3):165–175. [DOI] [PubMed] [Google Scholar]
- 33. Ho PM, Rumsfeld JS. Beyond inpatient and outpatient care: alternative model for hypertension management. BMC Public Health. 2006;6:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bosworth HB, Olsen MK, McCant F, et al. Hypertension Intervention Nurse Telemedicine Study (HINTS): testing a multifactorial tailored behavioral/educational and a medication management intervention for blood pressure control. Am Heart J. 2007;153(6):918–924. [DOI] [PubMed] [Google Scholar]
- 35. Goldstein MK, Coleman RW, Tu SW, et al. Translating research into practice: organizational issues in implementing automated decision support for hypertension in three medical centers. J Am Med Inform Assoc. 2004;11(5):368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Goldstein MK, Hoffman BB, Coleman RW, et al. Patient safety in guideline‐based decision support for hypertension management: ATHENA DSS. Proc AMIA Symp. 2001:214–218. [PMC free article] [PubMed] [Google Scholar]
- 37. Healthy People 2010 Web site . http://www.healthypeople.gov/. Accessed September 7, 2007.


