Abstract
The purposes of this study were to determine whether there is a significant correlation between the perceived and actual stroke risk among hypertensive patients and to identify patient characteristics associated with inaccurate estimation of stroke risk. The authors performed a cross‐sectional analysis of 296 men with hypertension who were enrolled in the Veterans Study to Improve the Control of Hypertension (V‐STITCH). A patient's actual stroke risk was calculated using the Framingham stroke risk (FSR); patients' perceived risk was measured according to a self‐reported 10‐point risk scale. The median 10‐year FSR was 16%, but the median perceived risk score was 5 (range, 1 [lowest] to 10 [highest]). There was no significant correlation between patients' perceived risk of stroke and their calculated FSR (Spearman ρ=−0.08; P=.16; 95% confidence interval, −0.19 to 0.03). Patients who underestimated their stroke risk were significantly less likely to be worried about their blood pressure than patients with accurate risk perception (12.4% vs 69.6%; P<.0001). The lack of correlation between hypertensive patients' perceived stroke risk and FSR supports the need for better patient education on the risks associated with hypertension.
Stroke is the third most common cause of death and the most common cause of disability in the United States. The World Health Organization reports that 62% of cerebrovascular disease can be linked to inadequate blood pressure (BP) control. 1 Hypertension is the most frequent primary diagnosis in America, 2 and the relationship between BP and stroke is continuous, beginning at a systolic BP level as low as 115 mm Hg. 3 In spite of effective therapies, however, target BP was achieved in only 37% of patients with hypertension in 2003 and 2004, 4 well below the goal of 50% set by Healthy People 2010. 5 Poor patient adherence to pharmacologic and behavioral treatment recommendations as well as physician inertia contribute to inadequate BP control. 6 , 7 , 8 , 9
One concept that may be important in better understanding adherence in hypertensive patients is perceived risk of adverse outcomes such as stroke. 10 Lower perceived risk has been associated with poorer adherence to recommended health behaviors. 11 , 12 In addition, a person's beliefs about his or her perceived risk of a disease figure prominently in models of health behavior (eg, Health Belief Model), which assume that perceived risk is essential in motivating behavior. 13 , 14 , 15 Overall, patients tend to underestimate their own risk 16 ; Weinstein 17 , 18 refers to this underestimation as an “optimistic bias.”
Although behavioral theories incorporate perceived risk as an important component, they do not account for the accuracy of patient risk perceptions. 19 , 20 Previous studies showed that patients at high risk for stroke are frequently unable to identify stroke risk factors. 21 , 22 , 23 , 24 More recent data suggest that patient recognition of stroke risk factors, including BP, has improved significantly. 9 , 25 In one recent survey, >90% of hypertensive patients identified elevated BP as a risk factor for heart attacks, strokes, and heart failure. 9 However, even when patients can identify stroke risk factors, it is unknown whether this knowledge is adequately personalized into accurate stroke risk perception. Thus, the current study adds to the existing literature by examining the relationship between hypertensive patients' perceived personal risk for stroke and their actual stroke risk estimated by the Framingham stroke risk (FSR) profile. The aims of the current study were to assess the correlation between perceived and actual stroke risk in patients with hypertension and to identify variables related to inaccurate stroke risk perceptions.
PATIENTS AND METHODS
Data for this study came from the baseline evaluation of patients enrolled in the Veteran Study to Improve the Control of Hypertension (V‐STITCH) between March 2002 and April 2003. V‐STITCH was a 4‐year clinical trial that evaluated both patient and provider interventions in a primary care setting to improve BP control among patients with hypertension. 26 This study was approved by the Durham Veterans Affairs Institutional Review Board.
Patient Selection
Potential participants were identified through the Durham Veterans Affairs Medical Center (VAMC) electronic medical records and were required to (1) have a diagnosis of hypertension based on an outpatient ICD‐9 code of 401.0, 401.1, or 401.9; (2) receive primary care through Durham VAMC; and (3) have filled a prescription for antihypertensive medication in the previous year. Of the initial pool of 4017 potential veteran participants, the research assistants approached 816 patients. Because recruitment occurred at patients' primary care visits, these patients were selected from the available pool based on the schedule of primary care appointments. Patients were recruited consecutively until the target sample size for the primary study hypothesis was achieved. Of the 816 approached, 190 refused and 38 were excluded; a total of 588 patients were enrolled between March 2002 and April 2003.
We included in the present study only the 296 patients who did not have a history of stroke based on ICD‐9 codes of 431 through 434 and had complete data for both the FSR and the perceived risk variable. All data included in the present study were taken from a face‐to‐face interview with a research assistant at the time of enrollment or by review of the patient's medical records.
Measures
Covariates. Age, race, education level, and current exercise status were obtained by patient self‐report. Race was dichotomized as white or nonwhite. Education was categorized as <12th grade or >12th grade. The Rapid Estimate of Adult Literacy in Medicine (REALM) was used to measure patient literacy. 27 Limited literacy was defined as a REALM score of 0 to 60 and corresponds with a reading level <9th grade. Financial situation was assessed by asking patients to report whether they had enough money after paying bills for special things; enough to pay bills but not to purchase extra things; enough money to pay bills by cutting back on things; or difficulty paying bills no matter what was done. The last 2 answers were categorized as “inadequate income.” 28
Hypertension knowledge was measured by 10 questions that assessed patients' knowledge about hypertension facts (eg, high BP can cause kidney problems: true or false). 29 One point was assigned for each correct answer, and 0 points for each incorrect or missing answer. A total score was calculated by summing all 10 of the responses. Patients with a score of 9 or 10 were categorized as having high hypertension knowledge. Patients' beliefs about the seriousness of high BP was measured by asking, “How serious do you think having high BP is?” The answer choices were (1) very serious, (2) serious, (3) a little serious, and (4) not at all serious. The first 2 responses were categorized as believing that hypertension is serious. Worry about high BP was measured by asking, “How worried are you about your high BP?” Answers were rated on a scale from 1 to 10, where 1 indicated that the patient was definitely not worried about high BP and 10 indicated that the patient was extremely worried about high BP. Patients with scores of 6 through 10 were categorized as being more worried about hypertension.
Medication adherence was assessed by the Morisky self‐report scale, which consists of 4 statements describing nonadherence to medication. 30 Participants were asked to indicate the extent to which they agreed with each statement by rating their agreement on a 4‐point scale (strongly agree, agree, disagree, strongly disagree). Patients were categorized as nonadherent if they indicated agreement (ie, reported either “strongly agree” or “agree”) or answered “don't know” or “refused” to any of the 4 subscale items. 31
Framingham Stroke Risk. Stroke risk was assessed for each participant based on the adjusted FSR according to D'Agostino and colleagues. 32 The risk factors included in this risk estimate were age, treated systolic BP, diabetes mellitus, cigarette smoking, cardiovascular disease (CVD), atrial fibrillation, and left ventricular hypertrophy (LVH). These variables were combined to produce the FSR, which estimates a patient's 10‐year stroke probability. The FSR was used to represent the patient's actual risk of stroke. Clinic nurses measured seated resting BP at the time of enrollment with IVAC/Alaris automated devices, models 4200s and 4410s/4415s (Alaris Medical Products, Dublin, OH). History of CVD was obtained from the electronic medical record using ICD‐9 codes for coronary artery disease (410–414.xx), congestive heart failure (425.xx and 428.xx), and peripheral vascular disease (443.9). LVH and atrial fibrillation were determined by review of 12‐lead electrocardiography (ECG); the presence or absence of these risk factors was based on a cardiologist's interpretation of the ECG results. Because ECG was not routinely performed as a part of V‐STITCH, patients were included if they had a resting ECG within 2 years of study enrollment. BP control was defined according to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). 2
Perceived Risk. Perceived stroke risk was assessed by a single survey item that asked each patient, “How would you rate your likelihood of having a stroke as a result of high BP?” Responses were rated on a scale from 1 to 10 where 1 indicated that the patient thought he or she was not going to have a stroke as a result of having high BP and 10 indicated that the patient thought he or she was definitely going to have a stroke as a result of high BP. The item was similar to one used in other studies. 29 , 33
Analyses
For both sample comparisons, we used t tests to compare continuous variables and chi‐square to compare categoric variables except when the expected or observed cell frequency was <5 patients, in which case Fisher's exact test was used. We compared the characteristics of the 296 patients included in the current analysis with those of the remaining 292 patients enrolled in the trial but excluded from this analysis. To evaluate the relationship between patients' perceived risk and FSR, we examined the scatterplot of these variables and calculated the Spearman rank‐order correlation coefficient. We then categorized patients' perceived risk and FSR as low or high. The median perceived stroke risk score was 5; therefore, low perceived risk was categorized as a score of 1 to 5 and high perceived risk as a score of 6 to 10. We defined high actual stroke risk as a 10‐year FSR >20%; low actual stroke risk was defined as a 10‐year FSR <20%. This classification of high and low actual stroke risk is based on the convention used in the National Cholesterol Education Program treatment guidelines, which defines high cardiovascular risk as a 10‐year cardiovascular FSR >20%. 28 , 34
Based on the definitions of high and low perceived risk and actual risk (FSR), we further categorized patients according to their accuracy of risk perceptions. Patients with low FSR were categorized as accurate estimators if they perceived their risk as low or risk overestimators if they perceived their risk as high. Similarly, patients with high FSR were categorized as accurate estimators if they perceived their risk as high or risk under‐estimators if they perceived their risk as low. The odds of inaccurate risk perception were compared between patients with high and low FSR using the Mantel‐Haenszel test. We compared the characteristics of patients with accurate vs inaccurate (ie, overestimators in the low FSR group and underestimators in the high FSR group) risk perceptions in analyses stratified by high vs low FSR. No adjusted analyses were performed due to the small numbers of patients in each cell. Two‐sided P values were used with α set at .05 for rejecting the null hypothesis. All statistical analyses were performed using SAS software, version 9.1 (SAS Institute, Inc, Cary, North Carolina).
RESULTS
Of the 588 veterans enrolled in V‐STITCH, 296 were included in the current analysis. The remaining 292 patients were excluded for the following reasons: 233 patients were missing recent ECG results; 35 patients had a prior history of stroke; 33 patients were missing the perceived risk variable; 23 patients were missing either baseline systolic BP or diabetic status; and 10 female patients were excluded because we believed that the group of participants in our sample was insufficient to make meaningful inferences about stroke risk perceptions in women. Patients included in this study were more likely to report inadequate income (odds ratio [OR], 1.5; 95% confidence interval [CI], 1.0–2.2) and have high hypertension knowledge (OR, 1.5; 95% CI, 1.1–2.1) compared with those excluded. There were no statistically significant differences between patients included and excluded with regard to age, race, education level, literacy, current exercise, belief in the seriousness of hypertension, worry about hypertension, medication nonadherence, perceived stroke risk, presence of diabetes, or BP control (P>.05).
Patient characteristics for the total sample and according to low and high Framingham stroke risk are shown in Table I. All of the patients were male and 59% were white. The majority of nonwhite patients (93%) were black. The median 10‐year FSR was 16% (interquartile range, 10%–26%), and the median perceived risk score was 5 (interquartile range, 2–6; range, 1 [lowest] to 10 [highest]). Patients with high FSR were significantly more likely than those with low FSR to have inaccurate risk perception (OR, 8.8; 95% CI, 5.0–15.3). Patients with a low FSR were significantly more likely than those at high risk to have high hypertension knowledge (73.4% vs 52.9%; P=.004). In addition, patients with high FSR were significantly more likely than those with low FSR to be older and have higher systolic BP, concurrent CVD, atrial fibrilation, and LVH.
Table I.
Patient Characteristics by FSR
| Descriptive Characteristic | All Patients (N=296) | Low FSR (n=192) | High FSR (n=104) | P Value a |
|---|---|---|---|---|
| Demographics | ||||
| Mean age, y (SD) | 63.9 (10.9) | 60.2 (9.6) | 70.9 (9.5) | <.0001 |
| Nonwhite | 119 (40.2) | 79 (41.2) | 40 (38.5) | .72 |
| Education level <12th grade | 160 (54.1) | 98 (51.0) | 62 (59.6) | .16 |
| Literacy level <9th grade | 104 (35.1) | 61 (31.8) | 43 (41.4) | .15 |
| Inadequate income | 74 (25.0) | 54 (28.1) | 20 (19.2) | .09 |
| Current exerciser | 160 (54.1) | 103 (53.7) | 57 (54.8) | .85 |
| Knowledge, beliefs, and adherence | ||||
| High hypertension knowledge | 196 (66.2) | 141 (73.4) | 55 (52.9) | .0004 |
| Believe hypertension is serious | 266 (89.9) | 176 (91.7) | 90 (86.5) | .12 |
| More worried about hypertension | 94 (31.8) | 68 (35.4) | 26 (25.0) | .07 |
| Medication nonadherence | 105 (35.5) | 64 (33.3) | 41 (39.4) | .30 |
| Stroke risk | ||||
| Mean systolic blood pressure, mm Hg (SD) | 137.9 (17.2) | 133.6 (16.6) | 145.9 (15.5) | <.0001 |
| Mean diastolic blood pressure, mm Hg (SD) | 75.0 (11.3) | 75.7 (11.2) | 73.7 (11.5) | .15 |
| Blood pressure controlled | 135 (45.6) | 109 (56.8) | 26 (25.0) | <.0001 |
| Diabetes | 126 (42.6) | 74 (38.5) | 52 (50.0) | .06 |
| Cardiovascular disease | 166 (56.1) | 77 (40.1) | 89 (85.6) | <.0001 |
| Current smoker | 71 (24.0) | 43 (22.4) | 28 (26.9) | .38 |
| Atrial fibrillation | 9 (3.0) | 1 (0.5) | 8 (7.7) | .0012 |
| Left ventricular hypertrophy | 52 (17.6) | 17 (8.9) | 35 (33.7) | <.0001 |
| Abbreviation: FSR, Framingham stroke risk. Values are presented as No. (%) unless otherwise indicated. Variables with missing data: race=3; income=3; literacy=12; hypertension serious=1; hypertension worry=1. All missing values included in calculation of proportions, but not in chi‐square. a P value for comparison between low‐and high‐actual risk groups. | ||||
We plotted patients' perceived stroke risk against the FSR in the Figure. There was no evidence of a correlation between patients' perceived risk of stroke and their 10‐year FSR (Spearman's ρ=−0.08; P=.16). The 95% CI for the correlation coefficient ranged from −0.19 to 0.03.
Figure.
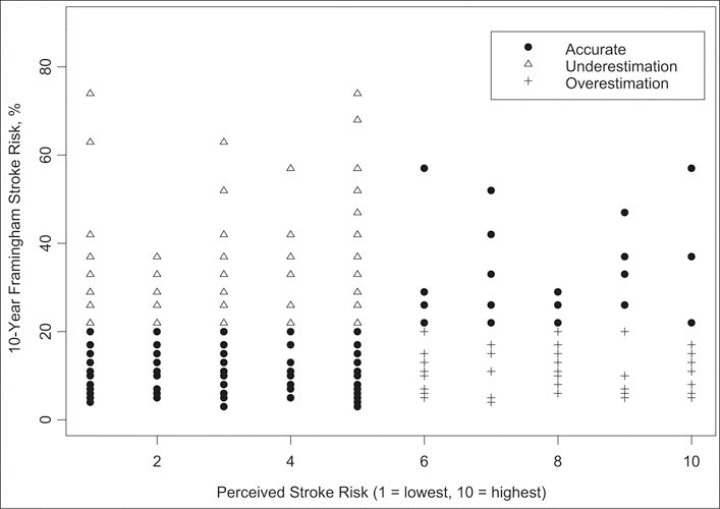
Scatterplot of 10‐year Framingham stroke risk and perceived stroke risk. Patients' stroke risk perceptions were defined as accurate, underestimation (high Framingham risk, low perceived risk), or underestimation (low Framingham risk, high perceived risk).
Among patients with low FSR, 71% reported low perceived risk and were categorized as having accurate risk perception (n=137); 29% reported high perceived risk and were categorized as risk overestimators (n=55) (Table II). Compared with patients with accurate risk estimation, low‐FSR patients who overestimated their risk were significantly more likely to be younger (mean age difference, 3.9 years; 95% CI, 0.9–6.9 years) and worried about their BP (67.3% vs 22.6%; P<.0001). There was no significant difference in the modifiable health behaviors of exercise, medication adherence, or smoking.
Table II.
Accuracy of Risk Estimation for Patients With 10‐Year Framingham Stroke Risk ≤20%
| Descriptive Characteristic | Overestimate (n=55) | Accurate Estimate (n=137) | P Value |
|---|---|---|---|
| Demographics | |||
| Mean age, y (SD) | 57.3 (7.7) | 61.3 (10.1) | .004 |
| Nonwhite | 22 (40.0) | 57 (41.6) | .79 |
| Education level ≤12th grade | 28 (50.9) | 70 (51.1) | .98 |
| Literacy level <9th grade | 18 (32.7) | 43 (31.4) | .98 |
| Inadequate income | 21 (38.2) | 33 (24.1) | .11 |
| Current exerciser | 30 (54.6) | 73 (53.3) | .87 |
| Knowledge, beliefs, and adherence | |||
| High hypertension knowledge | 44 (80.0) | 97 (70.8) | .19 |
| Believe hypertension is serious | 53 (96.4) | 123 (89.8) | .24 |
| More worried about hypertension | 37 (67.3) | 31 (22.6) | <.0001 |
| Medication nonadherence | 17 (30.9) | 47 (34.3) | .65 |
| Stroke risk | |||
| Mean systolic blood pressure, mm Hg (SD) | 137.0 (14.7) | 132.2 (17.2) | .07 |
| Mean diastolic blood pressure, mm Hg (SD) | 77.2 (10.8) | 75.1 (11.3) | .25 |
| Blood pressure controlled | 28 (50.9) | 81 (59.1) | .30 |
| Diabetes | 21 (38.2) | 53 (38.7) | .95 |
| Cardiovascular disease | 26 (47.3) | 51 (37.2) | .20 |
| Current smoker | 11 (20.0) | 32 (23.4) | .61 |
| Atrial fibrillation | 0 (0.0) | 1 (0.7) | 1.0 |
| Left ventricular hypertrophy | 7 (12.7) | 10 (7.3) | .26 |
| Values are presented as No. (%) unless otherwise indicated. | |||
Among patients with high FSR, 22.1% reported high perceived risk and were categorized as having accurate risk perception (n=23); 77.9% reported low perceived risk and were categorized as risk underestimators (n=81) (Table III). Compared with patients with accurate risk estimation, high‐FSR patients who underestimated their risk were significantly less likely to be worried about their BP (12.4% vs 69.6%; P<.0001) and have LVH diagnosed by ECG (27.2% vs 56.5%; P=.009).
Table III.
Accuracy of Risk Estimation for Patients with 10‐Year Framingham Stroke Risk >20%
| Descriptive Characteristic | Underestimate (n=81) | Accurate Estimate (n=23) | P Value |
|---|---|---|---|
| Demographics | |||
| Mean age, y | 71.2 (10.1) | 69.8 (7.0) | .54 |
| Nonwhite race | 31 (38.3) | 9 (39.1) | .99 |
| Education level <12th grade | 48 (59.3) | 14 (60.9) | .89 |
| Literacy level <9th grade | 33 (40.7) | 10 (43.5) | .74 |
| Inadequate income | 15 (18.5) | 5 (21.7) | .88 |
| Current exerciser | 44 (54.3) | 13 (56.5) | .85 |
| Knowledge, beliefs, and adherence | |||
| High hypertension knowledge | 41 (50.6) | 14 (60.9) | .38 |
| Believe hypertension is serious | 68 (84.0) | 22 (95.7) | .19 |
| More worried about hypertension | 10 (12.4) | 16 (69.6) | <.0001 |
| Medication nonadherence | 33 (40.7) | 8 (34.8) | .61 |
| Stroke risk | |||
| Mean systolic blood pressure, mm Hg (SD) | 146.8 (16.2) | 142.7 (12.6) | .27 |
| Mean diastolic blood pressure, mm Hg (SD) | 73.7 (11.7) | 73.9 (11.3) | .92 |
| Blood pressure controlled | 20 (24.7) | 6 (26.1) | .89 |
| Diabetes | 37 (45.7) | 15 (65.2) | .10 |
| Cardiovascular disease | 70 (86.4) | 19 (82.6) | .65 |
| Current smoker | 25 (30.9) | 3 (13.0) | .11 |
| Atrial fibrillation | 6 (7.4) | 2 (8.7) | 1.0 |
| Left ventricular hypertrophy | 22 (27.2) | 13 (56.5) | .009 |
| Values are presented as No. (%) unless otherwise indicated. | |||
DISCUSSION
In this sample of hypertensive men, no significant correlation was found between patients' perceived and actual stroke risk estimated with the FSR score. Compared with patients with lower FSR, patients with the highest calculated FSR were less knowledgeable about hypertension and more likely to inaccurately estimate their stroke risk. The accuracy of patients' stroke risk perception was significantly associated with their level of worry about hypertension. In spite of extensive effort to increase public awareness of stroke risk, this study suggests that patients with hypertension may not adequately translate their personal vascular risk factors into an accurate estimation of stroke risk.
Patients at high risk for stroke based on their FSR were significantly more likely to have inaccurate risk perceptions than patients at lower risk, a phenomenon known as “unrealistic optimism.” 17 Others have reported that poor risk factor recognition is particularly common in those with a higher burden of chronic disease 35 and among patients with lower socioeconomic status relative to their peers. 36 In a national telephone survey, 68% of respondents indicated that hypertension was not a “serious health concern,” and nearly half did not know their BP despite the fact that the vast majority had a measurement within 4 months of the survey. 37 A more recent survey found, however, that >90% of patients are aware of the health risks of hypertension 9 ; however, as noted, increased recognition may not be enough for patients to translate information on risk factors into an accurate estimate of their personal risk.
The patient variable most strongly associated with inaccurate risk perception was patient worry about hypertension. Patients who were more worried about their BP had higher perceived risk of stroke. Because of the limitations of the sample size and number of other variables considered, we were not able to determine whether this association persisted after adjusting for other potential confounders. It is potentially interesting, however, because worry and higher perceived vulnerability for a disease are associated with an increase in preventive health behavior such as changes in diet and exercise. 11 , 38 While high levels of worry can contribute to patient anxiety, in high‐risk patients this may be an unavoidable component of promoting accurate risk perception.
There are a number of potential limitations to consider when interpreting the results of our study. First, it was conducted only in male veterans with hypertension. It is possible that these findings do not generalize to women or nonveteran populations. While others have reported that women are more likely to correctly identify at least one stroke risk factor when compared with men (OR, 1.54), both men and women have significant difficulty identifying stroke risk factors. 21 , 23 In spite of this limitation, the study sample included men with hypertension as well as 40% racial minorities and is therefore directly relevant to understanding stroke risk perceptions in patients who are at highest risk. In addition, one would anticipate that a sample of patients who are at high risk for stroke and receiving regular primary care would be more aware of their risk than a community sample, which may therefore lead to less discordance between objective and perceived risk.
Second, the measures used in this study may not adequately capture perceived and actual stroke risk. The item used to report perceived risk asked respondents about their chances of having a stroke as a result of high BP, while the FSR reports the risk of stroke from any cause. All patients had hypertension and were recruited into the study to improve BP control, so we believe it is unlikely that they would alter their perception of stroke risk based on distinguishing the specific contributing cause. In addition, the scale of measurement for the perceived risk variable did not specify any units or time frame for risk, while the FSR provided a 10‐year probability. Patients may differ in how they define high or low 10‐year stroke risk. Even with these differences, we would have expected to detect some correlation in the continuous variables of perceived and actual risk if any existed. We chose to define high FSR as >20% over 10 years because we believed most practitioners would accept this convention based upon similar standards in cardiovascular disease. 34 A lower threshold for high absolute risk would have resulted in even more patients who underestimated their risk.
A limitation of the FSR is that calculated risks may be inaccurate in ethnic/racial minorities because this model was developed in a predominantly white population. 32 However, the stroke risk factors included in the FSR are widely accepted as the most important predictors of risk in all groups of patients. Similarly, the FSR may also not be accurately calibrated for current stroke risk because of the significant advances in risk reduction since the initial development of this model. While calibrating the model to current standards of care may reduce the magnitude or the calculated risk, a better calibrated model would unlikely change the lack of correlation with perceived risk that we observed.
Major strengths of this study include focusing on patients with hypertension who are at greatest need for risk reduction as well as a large representation of ethnic minorities. In addition, this study explores several patient factors potentially related to inaccurate risk perception. Prior studies have often focused on correct identification of risk factors, while this study compared a patient's personalized risk perception on a numeric scale with a well‐validated model of actual stroke risk. We acknowledge that the definitions for high risk used in this analysis (FSR >20% and perceived risk 6–10) may not match many patient or provider standards for high risk. We repeated the analysis using alternative cutoffs for high risk (FSR >15% and perceived risk 7–10). While this sensitivity analysis increased the proportion of patients categorized as high‐risk, the associations with accurate risk perceptions were unchanged. It is important to note that the primary analysis examined the correlation of these variables on a continuous scale and was therefore not sensitive to definitions of high or low risk.
To design effective interventions for risk reduction in hypertensive patients, researchers and clinicians need to understand the patient's perception of his or her risk. Developing tailored patient education materials that incorporate personal risk could be a promising strategy to correct inaccurate perceptions. Interventions that increase the accuracy of patients' risk perceptions may ultimately motivate individuals to engage in risk reduction behaviors.
Acknowledgment:
This research was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service, investigator initiative grants 20‐034 as well as an Established Investigator Award to Dr Bosworth from the American Heart Association. Dr Powers was supported by a fellowship training grant through the Agency for Healthcare Research and Quality (T32 HS000079). The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1. World Health Report 2002: Reducing Risks, Promoting Health Life. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 2. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2571. [DOI] [PubMed] [Google Scholar]
- 3. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: A meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 4. Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. [DOI] [PubMed] [Google Scholar]
- 5. Healthy People 2010. Conference edition (2 volumes). 2000. [Google Scholar]
- 6. Bosworth HB, Oddone EZ, Weinberger M. Patient Treatment Adherence: Concepts, Interventions, and Measurement. Mahwah, NJ: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- 7. DiMatteo MR, Giordani PJ, Lepper HS, et al. Patient adherence and medical treatment outcomes: A meta‐analysis. Med Care. 2002;40:794–811. [DOI] [PubMed] [Google Scholar]
- 8. Berrigan D, Dodd K, Troiano RP, et al. Patterns of health behavior in US adults. Prev Med. 2003;36:615–623. [DOI] [PubMed] [Google Scholar]
- 9. Moser M, Franklin SS. Hypertension management: Results of a new national survey for the hypertension education foundation: Harris Interactive. J Clin Hypertens (Greenwich). 2007;9:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Horne R. Representations of medication and treatment: advances in theory and measurement. In: Petrie KJ, Weinman J, eds. Perceptions of Health and Illness: Current Research and Applications. Australia: Harwood Academic Publishers; 1997:155–187. [Google Scholar]
- 11. McCaul KD, Branstetter AD, Schroeder DM, et al. What is the relationship between breast cancer risk and mammography screening? A meta‐analytic review. Health Psychol. 1996;15:423–429. [DOI] [PubMed] [Google Scholar]
- 12. Lerman C, Kash K, Stefanek M. Younger women at increased risk for breast cancer: perceived risk, psychological well‐being, and surveillance behavior. J Natl Cancer Inst Monogr. 1994;(16):171–176. [PubMed] [Google Scholar]
- 13. Weinstein ND. Testing four competing theories of health‐protective behavior. Health Psychol. 1993;12:324–333. [DOI] [PubMed] [Google Scholar]
- 14. Janz NK, Becker MH. The health belief model: A decade later. Health Educ Q. 1984;11:1–47. [DOI] [PubMed] [Google Scholar]
- 15. Rogers RW. Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In: Cacioppo JT, Petty RE, eds. Social Psychophysiology: A Sourcebook. New York, NY: Guilford Press; 1983:153–176. [Google Scholar]
- 16. Avis NE, Smith KW, McKinlay JB. Accuracy of perceptions of heart attack risk: What influences perceptions and can they be changed? Am J Public Health. 1989;79:1608–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Weinstein ND. Why it won't happen to me: perceptions of risk factors and susceptibility. Health Psychol. 1984;3:431–457. [DOI] [PubMed] [Google Scholar]
- 18. Weinstein ND. Unrealistic optimism about susceptibility to health problems: Conclusions from a community‐wide sample. J Behav Med. 1987;10:481–500. [DOI] [PubMed] [Google Scholar]
- 19. Lipkus IM, Kuchibhatla M, McBride CM, et al. Relationships among breast cancer perceived absolute risk, comparative risk, and worries. Cancer Epidemiol Biomarkers Prev. 2000;9:973–975. [PubMed] [Google Scholar]
- 20. Kershaw TS, Ethier KA, Niccolai LM, et al. Misperceived risk among female adolescents: Social and psychological factors associated with sexual risk accuracy. Health Psychol. 2003;22:523–532. [DOI] [PubMed] [Google Scholar]
- 21. Treiber FA, Kamarck T, Schneiderman N, et al. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosom Med. 2003;65:46–62. [DOI] [PubMed] [Google Scholar]
- 22. Ferris A, Robertson RM, Fabunmi R, et al. American Heart Association and American Stroke Association national survey of stroke risk awareness among women. Circulation. 2005;111:1321–1326. [DOI] [PubMed] [Google Scholar]
- 23. Pancioli AM, Broderick J, Kothari R, et al. Public perception of stroke warning signs and knowledge of potential risk factors. JAMA. 1998;279:1288–1292. [DOI] [PubMed] [Google Scholar]
- 24. Muller‐Nordhorn J, Nolte CH, Rossnagel K, et al. Knowledge about risk factors for stroke: A population‐based survey with 28,090 participants. Stroke. 2006;37:946–950. [DOI] [PubMed] [Google Scholar]
- 25. Kraywinkel K, Heidrich J, Heuschmann PU, et al. Stroke risk perception among participants of a stroke awareness campaign. BMC Public Health. 2007;7:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bosworth HBHB, Olsen MKMK, Goldstein MKMK, et al. The veterans' study to improve the control of hypertension (V‐STITCH): Design and methodology. Contemp Clin Trials. 2005;26:155–168. [DOI] [PubMed] [Google Scholar]
- 27. Parker RM, Baker DW, Williams MV, et al. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10:537–541. [DOI] [PubMed] [Google Scholar]
- 28. Bosworth HB, Bastian LA, Kuchibhatla MN, et al. Depressive symptoms, menopausal status, and climacteric symptoms in women at midlife. Psychosom Med. 2001;63:603–608. [DOI] [PubMed] [Google Scholar]
- 29. Bosworth HB, Dudley T, Olsen MK, et al. Racial differences in blood pressure control: potential explanatory factors. Am J Med. 2006;119(1):70.e9–70.e15. [DOI] [PubMed] [Google Scholar]
- 30. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self‐reported measure of medication adherence. Med Care. 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- 31. Lowry KP, Dudley TK, Oddone EZ, et al. Intentional and unintentional nonadherence to antihypertensive medication. Ann Pharmacother. 2005;39:1198–1203. [DOI] [PubMed] [Google Scholar]
- 32. D'Agostino RB, Wolf PA, Belanger AJ, et al. Stroke risk profile: Adjustment for antihypertensive medication. The Framingham study. Stroke. 1994;25:40–43. [DOI] [PubMed] [Google Scholar]
- 33. Bosworth HB, Olsen MK, Dudley T, et al. The take control of your blood pressure (TCYB) study: Study design and methodology. Contemp Clin Trials. 2007;28:33–47. [DOI] [PubMed] [Google Scholar]
- 34. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 35. Bjerrum L, Hamm L, Toft B, et al. Do general practitioner and patient agree about the risk factors for ischaemic heart disease? Scand J Prim Health Care. 2002;20:16–21. [DOI] [PubMed] [Google Scholar]
- 36. Ford ES, Jones DH. Cardiovascular health knowledge in the United States: Findings from the National Health Interview Survey, 1985. Prev Med. 1991;20:725–736. [DOI] [PubMed] [Google Scholar]
- 37. Egan BM, Lackland DT, Cutler NE. Awareness, knowledge, and attitudes of older Americans about high blood pressure: Implications for health care policy, education, and research. Arch Intern Med. 2003;163:681–687. [DOI] [PubMed] [Google Scholar]
- 38. Ransford HE. Race, heart disease worry and health protective behavior. Soc Sci Med. 1986;22:1355–1362. [DOI] [PubMed] [Google Scholar]


