Abstract
Resistant hypertension is defined as blood pressure (BP) that remains uncontrolled in spite of the use of ≥3 antihypertensive medications. Stricter BP goals, higher obesity rates, older age, and increased use of exogenous BP‐elevating substances are related to an increasing prevalence of resistant hypertension. The evaluation of patients with resistant hypertension is focused on identifying contributing and secondary causes of hypertension, including hyperaldosteronism, obstructive sleep apnea, chronic kidney disease, renal artery stenosis, and pheochromocytoma. Hyperaldosteronism is now recognized as the most common cause of resistant hypertension, and all patients with resistant hypertension should be screened with a plasma aldosterone/renin ratio even if the serum potassium level is normal. Treatment includes removal of contributing factors, appropriate management of secondary causes, and use of effective multidrug regimens. Recent studies indicate that the addition of spironolactone to standard treatment induces significant BP reduction in most patients with resistant hypertension.
Resistant hypertension is defined as a blood pressure (BP) level that remains above goal in spite of the use of 3 antihypertensive medications in effective doses, usually including a diuretic. Patients who are intolerant of diuretics and have uncontrolled BP on regimens of 3 drugs from other classes are also considered to have resistant hypertension. The BP goal is <140/90 mm Hg in the general population of hypertensive patients and <130/80 mm Hg in high‐risk hypertensive patients, including those with diabetes, chronic kidney disease (CKD), or coronary heart disease. Patients in whom ≥4 medications are required to control BP are also considered to have resistant hypertension.
Factors that predispose to antihypertensive treatment resistance include population characteristics, such as older age and higher obesity rates, as well as provider characteristics, including inadequate attention to systolic BP (SBP) elevations and more aggressive BP goals.
PSEUDORESISTANCE
Pseudoresistance is the appearance of lack of BP control caused by inaccurate measurement of BP, inappropriate drug choices/doses, nonadherence to prescribed therapy, or white‐coat effect. Identification of pseudoresistance avoids overtreatment and excessive and expensive evaluation.
Clinical inertia, defined as the provider's failure to increase therapy when the treatment goal is not reached, is a major contributor to suboptimal medical treatment, resulting in uncontrolled hypertension. Lack of knowledge of treatment guidelines, underestimation of cardiovascular risk, and the use of spurious reasons to avoid intensification of therapy (eg, physician perception [without patient input] that the patient will not accept more medications) are common causes of clinical inertia.
Poor adherence to prescribed medication regimens is a common problem in patients with high BP and a common cause of uncontrolled hypertension. There is evidence that poor adherence is less common among patients who are seen by hypertension specialists. High cost of treatment, poor relations between doctor and patient, complex medical regimens, and adverse effects of medical therapy are additional causes of poor adherence.
White‐coat effect, the difference between office BP and ambulatory or home BP measurements can be calculated as the mean office BP minus mean daytime ambulatory BP. Ambulatory and home BP monitoring are important methods to evaluate patients with uncontrolled BP and to assess true treatment resistance in clinical practice.
CONTRIBUTING FACTORS
Volume Expansion
Volume expansion related to excessive dietary sodium, sodium retention secondary to CKD, and/or failure to use diuretics appropriately can cause resistant hypertension (Table I). Diuretics are the cornerstone of treatment in patients whose BP cannot be controlled with multiple agents from other drug classes, and dietary salt reduction is useful adjunctive treatment in patients with resistant hypertension.
Table I.
Contributing Factors of Resistant Hypertension
| Contributing factors |
| Volume expansion |
| Excess sodium intake |
| Volume retention secondary to chronic kidney disease |
| Inadequate diuretic therapy |
| Obesity |
| Exogenous substances |
| Nonsteroidal anti‐inflammatory agents |
| Oral contraceptives |
| Alcohol |
| Corticosteroids |
| Anabolic steroids |
| Sympathomimetic agents (nasal decongestants, diet pills, cocaine) |
| Caffeine |
| Cyclosporine |
| Erythropoietin |
| Chemotherapeutic agents |
| Antidepressants |
Obesity
Obesity is common in patients with resistant hypertension. Data from the Hypertension and Diabetes Risk Screening and Awareness (HYDRA) study, a cross‐sectional study of 45,125 primary care patients, showed that those with a body mass index >40 kg/m2 had a higher prevalence of hypertension, as well as a 5.3‐ and 3.2‐fold higher probability of requiring 4 or 3 antihypertensive drugs, respectively, to achieve BP control compared with patients with normal weight (body mass index ≤25 kg/m2). Increased sodium and fluid retention, sympathetic activation, and stimulation of the renin‐angiotensin‐aldosterone system (RAAS) appear to contribute to high BP in obese persons.
Exogenous Substances
Use of a variety of prescription drugs and other exogenous substances is commonly related to resistant hypertension (Table I), and a history of use of these agents should be queried in all patients with resistant hypertension. Withdrawal of these agents can reduce or even normalize BP in some patients.
Nonsteroidal anti‐inflammatory drugs (NSAIDs), including selective cyclooxygenase (COX) 2 inhibitors, are a common cause of uncontrolled BP and renal impairment in hypertensive patients. NSAIDs increase the BP through volume and sodium retention, likely due to inhibition of vasodilating prostaglandins in the kidney.
All NSAIDs appear to elevate mean BP (Figure 1) and antagonize the BP‐lowering effects of antihypertensive drugs. The selective COX‐2 inhibitors are also associated with BP elevation. A meta‐analysis of 45,451 patients enrolled in 19 randomized controlled trials showed that COX‐2 inhibitors elevate BP by an average of ≈4/1 mm Hg compared with placebo and by ≈3/1 compared with NSAIDs. The BP‐elevating effects are dose‐related, and some agents appear to have greater effects than others. For example, in the Multinational Etoricoxib and Diclofenac Arthritis Long‐Term (MEDAL) program, which randomized 34,701 patients with osteoarthritis or rheumatoid arthritis to etoricoxib or diclofenac, patients assigned to etoricoxib discontinued the study due to hypertension more frequently than did those assigned to diclofenac. If analgesics are necessary in hypertensive patients, medications such as tramadol or hydrocodone and nerve block are useful alternatives. If NSAIDs or COX‐2 inhibitors are needed, minimal effective doses should be prescribed. Providers must ask all hypertensive patients about use of pain control medications to avoid this form of iatrogenic resistant hypertension.
Figure 1.
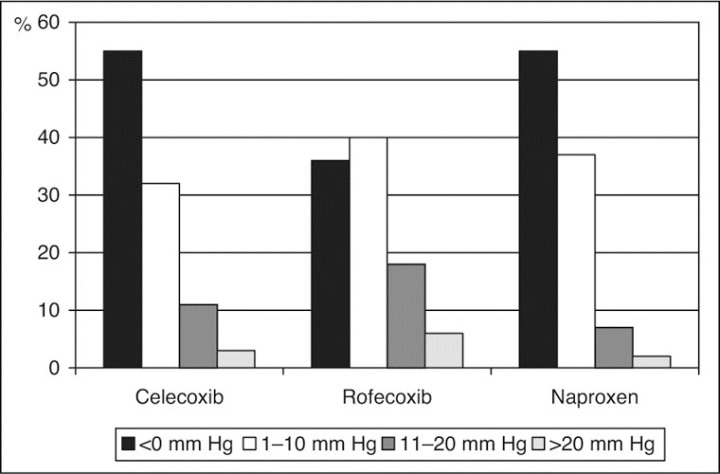
Effects of celecoxib, rofecoxib, and naproxen on changes in 24‐hour mean systolic blood pressure after 6 weeks of therapy. From Sowers et al.13
Oral contraceptives induce small increases in BP in the entire population of users, with frank hypertension occurring in fewer patients and resistant hypertension in very few patients. The Nurses' Health Study prospectively followed 68,297 normotensive premenopausal female nurses for development of hypertension for 4 years. Current oral contraceptive users had an 80% increased risk of developing hypertension compared with those who had never used them, but this increased risk resolved almost completely with withdrawal of the medication. Further, oral contraceptive use in persons with underlying hypertension is associated with uncontrolled BP. A cross‐sectional study evaluating the association between oral contraceptives and BP control in 171 hypertensive women found that oral contraceptive users had poorer BP control and tended to have more severe hypertension than users of other contraceptive methods or nonusers. Combined (estrogen/progestin) oral contraceptives are more often associated with BP increases than progestin‐only oral contraceptives.
Menopausal hormone therapy has minimal effects on BP and is not contraindicated in either normotensive or hypertensive women. Nevertheless, all hypertensive women treated with menopausal hormone therapy should have their BP measured initially and then at 3‐ to 6‐month intervals depending on the difficulty of control.
Heavy alcohol ingestion increases the risk of uncontrolled hypertension, and its cessation promotes BP reduction and improves adherence to treatment. In a cross‐sectional analysis, men with excessive alcohol intake (>4 drinks/d) had 50% higher probability of poor BP control. Moderation in alcohol consumption (<2 drinks/d) is recommended as a lifestyle modification in the general population, especially in patients with hypertension, and complete cessation should be advised in heavy drinkers.
Other exogenous substances that contribute to hypertension, such as corticosteroids, sympathomimetic agents, erythropoietin, and antidepressants, should be avoided in patients with high BP and discontinued if at all possible in those with uncontrolled BP. In persons for whom these substances are essential, more frequent BP evaluations and increased doses and/or numbers of antihypertensive medications may be required.
SECONDARY HYPERTENSION
The prevalence of secondary hypertension is greater in patients with resistant hypertension than in the general hypertensive population. The most common secondary causes of resistant hypertension are hyperaldosteronism, CKD, renal artery stenosis, and obstructive sleep apnea (OSA) (Table II). The prevalence of secondary hypertension increases with age, mainly due to increases in CKD, OSA, and renal artery stenosis.
Table II.
Secondary Causes of Hypertension
| Hyperaldosteronism |
| Obstructive sleep apnea |
| Chronic kidney disease |
| Renal artery stenosis |
| Pheochromocytoma |
| Central nervous system tumors |
| Coarctation of the aorta |
| Thyroid diseases |
Hyperaldosteronism
Hyperaldosteronism is the most common cause of secondary hypertension and is a frequent contributor to treatment resistance. Hypokalemia and adrenal tumors are no longer required for the diagnosis of hyperaldosteronism. In fact, a substantial proportion of patients with hyperaldosteronism have normal potassium levels. Experimental and clinical data indicate that the cardiorenal effects of aldosterone excess are dependent on concomitant high dietary salt intake.
Because of its high prevalence in this patient group, all patients with resistant hypertension, even those with normokalemia, should be evaluated for hyperaldosteronism. Measurement of the plasma aldosterone concentration (PAC)/plasma renin activity (PRA) ratio (≥20) has sufficient sensitivity and specificity to serve as an effective screening test for hyperaldosteronism. Demonstration of increased 24‐hour urinary excretion of aldosterone confirms the diagnosis of hyperaldosteronism (Figure 2).
Figure 2.
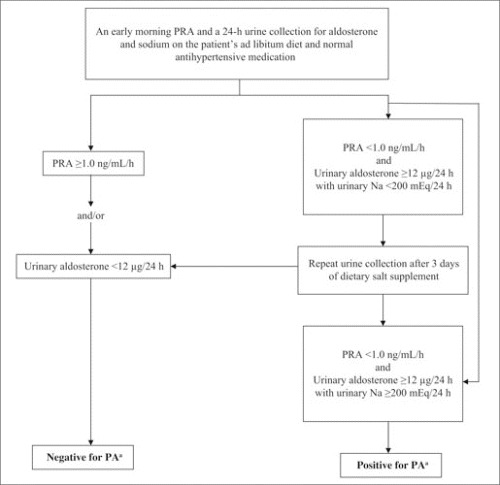
Flow chart for confirmatory testing for primary aldosteronism (PA). aIn patients with resistant hypertension and plasma aldosterone concentration/plasma renin activity (PRA) ratio ≥20. Na indicates sodium. Adapted from Nishizaka et al.14
After confirmation of biochemical hyperaldosteronism, thin‐cut abdominal computed tomography is recommended to identify adrenal tumors. Even in the setting of confirmed biochemical hyperaldosteronism, CT imaging has poor specificity for identifying functional aldosterone‐producing adenomas. Adrenal vein sampling can confirm or exclude lateralization of aldosterone excretion, consistent with a unilateral adenoma.
Medical therapy with mineralocorticoid receptor antagonists is appropriate for treatment of primary aldosteronism not amenable to surgery or, alternatively, as initial treatment in all patients with a high PAC/PRA ratio. The search for adenoma can be reserved for those patients whose hypertension or hypokalemia remains poorly controlled on medical therapy. Laparoscopic adrenalectomy should be considered in patients with unilateral adenoma whose BP is difficult to control medically.
Obstructive Sleep Apnea
OSA, characterized by preserved and increased respiratory effort despite partial or complete occlusion of the upper airway, is a common finding in patients with resistant hypertension. Our clinic reported that 85% of patients with resistant hypertension have OSA, defined as an apnea‐hypopnea index of ≥5 events/h. OSA should be evaluated with overnight polysomnography in patients with OSA symptoms, such as daytime sleepiness and nonrestorative sleep.
There is an association between aldosterone excess, obesity, and sleep apnea. Stimulation of aldosterone release by visceral fat, excessive sodium retention stimulated by sympathetic activation, and hypoxemia are possible underlying mechanisms. Continuous positive airway pressure (CPAP) treatment is the gold standard for management of OSA; however, the role of CPAP in the treatment of hypertension is not well established. While a cause‐and‐effect relationship between OSA and resistant hypertension cannot be inferred, patients with resistant hypertension and OSA should be treated with CPAP and encouraged to lose weight.
Chronic Kidney Disease
CKD is a common cause of resistant hypertension and a consequence of poor BP control over time. Fluid retention, excessive activation of the RAAS, and use of concomitant medicines such as NSAIDs are related to treatment resistance in patients with impaired renal function. All patients with resistant hypertension should have their glomerular filtration rate estimated by use of the Modification of Diet in Renal Disease formula or Cockcroft‐Gault equation because serum creatinine level is an unreliable marker of CKD, particularly in elderly patients. Albuminuria value should also be assessed. Blockade of the RAAS in patients with CKD reduces cardiovascular risk, improves BP control, and reduces proteinuria and progression to end‐stage renal disease.
Renal Artery Stenosis
Renovascular disease is a common finding in hypertensive patients with multiple risk factors and extrarenal atherosclerotic disease, particularly among patients with resistant hypertension. The vast majority (90%) of renal artery lesions are atherosclerotic in etiology, and the prevalence increases with age. Patients with resistant hypertension and known atherosclerotic disease, declining renal function, or a history of flash pulmonary edema have an increased likelihood of atherosclerotic renal arterial disease and should be evaluated for renal artery stenosis. The choice of treatment for atherosclerotic renal lesions is controversial because of a lack of strong evidence in favor of either medical treatment or revascularization.
Pheochromocytoma
The prevalence of pheochromocytoma in the general hypertensive population is low (0.1%–0.6%), but the diagnosis and treatment are extremely important because of difficult‐to‐control hypertension, the possibility of precipitating hypertensive crisis if the tumor is stimulated, and the possibility that the tumor could be malignant. Headache, palpitations, and sweating are the most common findings. All patients with resistant hypertension and symptoms typical of pheochromocytoma should be screened. Plasma free metanephrine is the best screening test for pheochromocytoma, and surgical removal is the appropriate treatment.
TREATMENT OF RESISTANT HYPERTENSION
Treatment of the patient with resistant hypertension includes removal of contributing factors, appropriate diagnosis and treatment of secondary causes, and use of effective multidrug regimens. Nonpharmacologic therapies, such as weight loss, exercise, dietary salt reduction, and moderation of alcohol intake should be encouraged in all patients. Interfering substances should be withdrawn or at least down‐titrated as possible, and OSA should be treated.
Factors related to poor adherence need to be addressed. Discussing the cost and adverse effects of medications, numbers of pills, and the objectives of treatment can improve patient adherence. Multidisciplinary teams, including nurses, pharmacists, nutritionists, psychologists, and fitness trainers can improve treatment results.
Pharmacologic Treatment
Full doses of appropriate combinations, such as an angiotensin‐converting enzyme (ACE) inhibitor angiotensin receptor blocker (ARB), calcium channel blocker, or a thiazide diuretic are generally very effective and well tolerated. Long‐acting thiazide diuretics are effective in most patients with resistant hypertension. Chlorthalidone is long‐lasting and more effective in reducing BP than hydrochlorothiazide. Patients treated with 25 mg/d of chlorthalidone have been shown to have greater SBP reduction (12.4 vs 7.4 mm Hg by ambulatory blood pressure monitoring) than patients treated with 50 mg/d of hydrochlorothiazide despite similar office BP reduction. Loop diuretics are preferable in patients with CKD and creatinine clearance <30 mL/min.
Mineralocorticoid receptor antagonists promote significant additional BP reduction independent of aldosterone/renin levels in the general population of patients with resistant hypertension (Figure 3). Our group has described the effect of low‐dose (12.5–25 mg/d) spironolactone in patients with uncontrolled BP on an average of 4 medications, including an ACE inhibitor or ARB and a diuretic. After 6 months of follow‐up, SBP was reduced by 25 mm Hg and diastolic BP (DBP) by 12 mm Hg. BP reductions were similar in patients with and without hyperaldosteronism and was not predicted by baseline PAC or PRA or by 24‐hour urinary aldosterone excretion. Data from the Anglo‐Scandinavian Cardiac Outcomes Trial‐Blood Pressure Lowering Arm (ASCOT‐BPLA) also demonstrated a significant BP‐lowering effect of spironolactone as fourth‐line therapy. SBP and DBP were reduced by 21.9 and 9.5 mm Hg, respectively, with spironolactone treatment in 1411 participants unselected for PAC and PRA levels.
Figure 3.
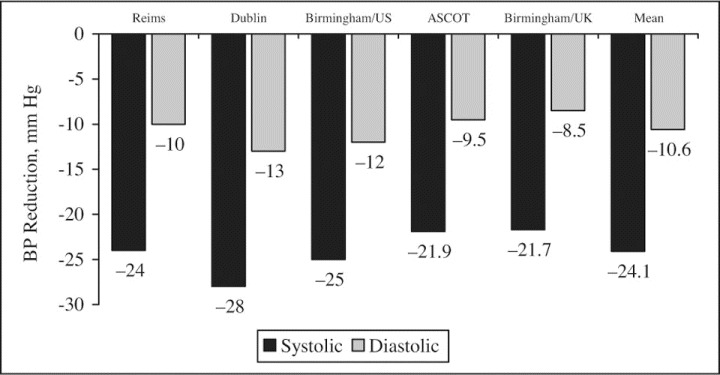
Blood pressure (BP) reduction effect of spironolactone observed in studies of patients with resistant hypertension. From Pimenta et al.15
Spironolactone was generally well tolerated in our studies, although breast tenderness occurred in about 10% of the men. The more selective mineralocorticoid receptor antagonist eplerenone is better tolerated than spironolactone and has been shown to effectively reduce BP. Hyperkalemia with or without acute renal insufficiency was uncommon in spite of concomitant using of an ACE inhibitor or ARB, but older patients and those with CKD or diabetes are at increased risk for developing hyperkalemia. Serum potassium and creatinine levels should be monitored in patients treated with mineralocorticoid receptor antagonists, particularly if they are receiving concomitant ACE inhibitor or ARB therapy. Potassium supplementation or salt substitutes that contain potassium should be discontinued or reduced in patients who are started on mineralocorticoid receptor antagonists.
Darusentan, a selective endothelin type A receptor antagonist, has been tested in patients with resistant hypertension and shown to decrease SBP by 11.5 mm Hg and DBP by 6.3 mm Hg compared with placebo after 10 weeks of follow‐up. However, more data on BP, as well as hypertension‐related target‐organ damage and cardiovascular events, and more safety data are needed before endothelin receptor antagonists can be employed in the routine treatment of patients with resistant hypertension. Such agents are currently in phase II clinical trials.
CONCLUSIONS
Resistant hypertension, defined as uncontrolled BP in spite of the use of at least 3 antihypertensive medications, is an increasingly common problem. Hyperaldosteronism, obesity, volume expansion, and OSA are common findings in patients with resistant hypertension. Mineralocorticoid receptor antagonists are an effective therapeutic option for the treatment of resistant hypertension even in the absence of demonstrable aldosterone excess.
Disclosures:
Dr Oparil has received grants‐in‐aid from Abbott Laboratories, AstraZeneca, Aventis, Biovail, Boehringer Ingelheim, Bristol‐Myers Squibb, Forest Laboratories, GlaxoSmithKline, Novartis, Merck, Pfizer, Sankyo Pharma, Sanofi‐Synthelabo, and Schering‐Plough; has served as consultant for Bristol‐Myers Squibb, Daiichi Sankyo, Merck, Novartis, Pfizer, Sanofi Aventis, and The Salt Institute; and is a member of Board of Directors for Encysive Pharmaceuticals.
Suggested Reading
- • . Calhoun DA. Resistant or difficult‐to‐treat hypertension. J Clin Hypertens (Greenwich). 2006;8:181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • . Campese VM, Mitra N, Sandee D. Hypertension in renal parenchymal disease: Why is it so resistant to treatment? Kidney Int. 2006;69:967–973. [DOI] [PubMed] [Google Scholar]
- • . Chapman N, Dobson J, Wilson S, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007;49:839–845. [DOI] [PubMed] [Google Scholar]
- • . Seventh Report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- • . Cushman WC, Ford CE, Cutler JA, et al; ALLHAT Collaborative Research Group . Success and predictors of blood pressure control in diverse North American settings: The Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393–404. [DOI] [PubMed] [Google Scholar]
- • . Haddy FJ. Role of dietary salt in hypertension. Life Sci. 2006;79:1585–1592. [DOI] [PubMed] [Google Scholar]
- • . Lloyd‐Jones DM, Evans JC, Larson MG, et al. Differential control of systolic and diastolic blood pressure: factors associated with lack of blood pressure control in the community. Hypertension. 2000;36:594–599. [DOI] [PubMed] [Google Scholar]
- • . Logan AG, Perlikowski SM, Mente A, et al. High prevalence of unrecognized sleep apnoea in drug‐resistant hypertension. J Hypertens. 2001;19:2271–2277. [DOI] [PubMed] [Google Scholar]
- • . Okonofua EC, Simpson KN, Jesri A, et al. Therapeutic inertia is an impediment to achieving the healthy people 2010 blood pressure control goals. Hypertension. 2006;47:345–351. [DOI] [PubMed] [Google Scholar]
- • . Pimenta E, Calhoun DA. Primary aldosteronism: diagnosis and treatment. J Clin Hypertens (Greenwich). 2006;8:887–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • . Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education. Ann Intern Med. 2006;145:165–175. [DOI] [PubMed] [Google Scholar]
- • . White WB. Cardiovascular effects of the cyclooxygenase inhibitors. Hypertension. 2007;49:408–418. [DOI] [PubMed] [Google Scholar]
- • . Sowers JR, White WB, Pitt B, et al; Celecoxib Rofecoxib Efficacy and Safety in Comorbidities Evaluation Trial (CRESCENT) Investigators . The effects of cyclooxygenase‐2 inhibitors and nonsteroidal anti‐inflammatory therapy on 24‐hour blood pressure in patients with hypertension, osteoarthritis and type 2 diabetes. Arch Intern Med. 2005;165(2):161–168. [DOI] [PubMed] [Google Scholar]
- • . Nishizaka MK, Pratt‐Ubunama M, Zaman MA, et al. Validity of plasma aldosterone‐to‐renin activity ratio in African American and white subjects with resistant hypertension. Am J Hypertens. 2005;18(6):805–812. [DOI] [PubMed] [Google Scholar]
- • . Pimenta E, Calhoun DA. Resistant hypertension and aldosteronism. Curr Hypertens Rep. 2007;9(5):353–359. [DOI] [PubMed] [Google Scholar]


