Abstract
An improvement in the awareness and treatment of hypertension in the United States has occurred, resulting in the best control rates in the world, which unfortunately are far below the goals of Healthy People 2000 or 2010. This failure to achieve blood pressure (BP) goals is attributed to many factors, including an aging population, higher prevalence of kidney disease and obesity, high salt intake, physician inertia to increase dose and number of antihypertensive medications prescribed, and patient nonadherence with medication regimens. Resistant hypertension is defined as a failure to achieve goal BP in patients who adhere to full doses of an appropriate antihypertensive regimen of 3 drugs that includes a diuretic. The problem of resistant hypertension is projected to increase as the population ages. Efforts on the part of the Veterans Administration hospitals and others clearly indicate that a system can be implemented to help increase the percentage of persons in whom BP goal is achieved and reduce the prevalence of resistant hypertension. Medications specific to the problem of resistant hypertension are also under development. This review analyzes the status of hypertension control in the United States, the frequency of associated diseases, and adherence to guidelines; it further discusses strategies to reduce the prevalence of resistant hypertension.
Primary hypertension is a complex disease with a wide range of factors involved in its etiology. 1 The relative importance of these factors can vary substantially among hypertensive individuals; thus, efficacy of treatment regimens may vary among subgroups of patients. 2 The presence of an increased number of risk factors such as obesity, older age, and stage 3 kidney disease (estimated glomerular filtration rate [eGFR] <60 mL/min) in a given individual contributes to a lower likelihood of achieving the blood pressure (BP) goal even with multiple drugs (ie, resistant hypertension). The guidelines of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) define resistant hypertension as the failure to achieve goal BP in patients who are adhering to full doses of an appropriate regimen of at least 3 antihypertensive drugs that includes a diuretic. 2
In recent decades, both net and age‐adjusted prevalence ratios of hypertension have continued to increase and current control rates are not acceptable. 3 , 4 In the most recent assessment of National Health and Nutrition Examination Survey (NHANES) rates, however, there is hope. When compared with 1999–2000, there were some increases in the overall awareness and treatment rates of hypertension, 5 and BP control rates increased from 29% in 1999–2000 to 37% in 2003–2004. There was also a large number of individuals at goal BP in the group most prone to difficult‐to‐treat hypertension (ie, age older than 60 years). This optimism needs to be tempered with the fact that we need to work harder to achieve BP goals in more patients to reduce cardiovascular risk. One such model to achieve BP goals is the Veterans Administration health care system. 6 This or some similar model needs to be implemented. In addition, the population continues to age, and the prevalence of associated morbidities, such as obesity, type 2 diabetes, and chronic kidney disease, is increasing. 7 , 8 Thus, success in future attainment of BP goals appears as a major challenge that depends on renewed efforts of physicians to diagnose and aggressively treat high BP, improvements in patients' compliance, and possibly development of newer drugs with new and complementary mechanisms of action.
This review discusses the status of hypertension management in the United States, as well as the unique problems associated with resistant hypertension. Further, it focuses on resistant hypertension in the United States by outlining strategies to improve hypertension treatment and control under such conditions.
CURRENT STATE OF BP MANAGEMENT IN THE UNITED STATES
Hypertension Control
According to NHANES data, both the net and age‐adjusted prevalence of hypertension in the US adult population increased during the past decade, and more than 60 million adults in the United States were estimated to have hypertension in 2000. 4 , 9 Updated estimates of the prevalence by an American Heart Association assessment of NHANES data put the prevalence in 2004 at 72 million. 10 The proportion of adults with hypertension who are aware of their disease, receive antihypertensive treatment, and have a BP level <140/90 mm Hg has considerably improved from 1976 to 2000 (Table I). 3 , 4 Current control rates for hypertension in the United States are improving slowly (Figure 1), ranging from around 30% of the total hypertensive population to about 58% among patients on antihypertensive medication. Inadequate systolic BP (SBP) control is the main culprit responsible for poor control rates, a variable that primarily drives cardiovascular event rates in individuals aged 50 years and older. 11 Overall, BP control levels are below the Healthy People goal of 50%, which was originally set for 2000 and then extended to 2010. 2 In Europe, similar data suggest a worse situation, with control rates <10% in several countries. 12 , 13 , 14
Table I.
Trends in Awareness, Treatment, and Control of Hypertension in the US Adult Population From 1976 to 2004
| NHANES II (1976–1980) | NHANES III Phase 1 (1988–1991) | NHANES III Phase 2 (1991–1994) | NHANES (1999–2000) | NHANES (2003–2004) | |
|---|---|---|---|---|---|
| Awareness | 51 | 73 | 68 | 70 | 76 |
| Treatment | 31 | 55 | 52 | 59 | 65 |
| Control | 10 | 29 | 23 | 31 | 37 |
| Control among those treated | 32 | 55 | 44 | 53 | 57 |
| Abbreviation: NHANES, National Health and Nutrition Examination Survey. Combined data from Burt et al, 3 Hajjar and Kotchen, 4 and Ong et al. 5 Numbers represent percentages of patients among all adults aged 18–74 years with hypertension, defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg or use of antihypertensive medication. | |||||
Figure 1.
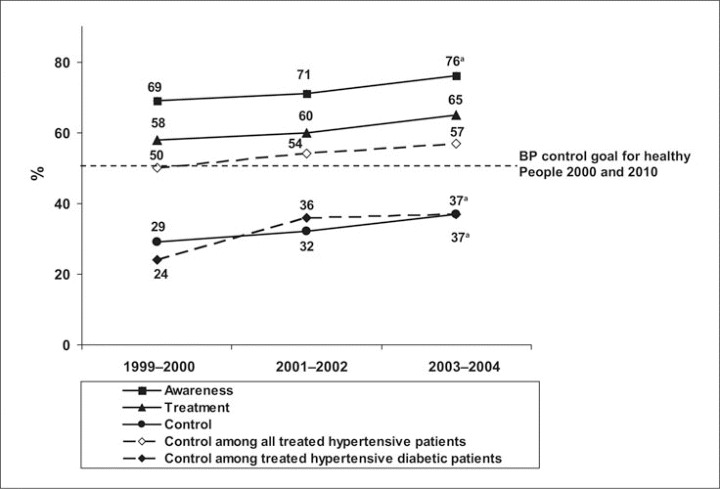
Comparison of hypertension awareness, treatment, and control in the United States in 14,653 patients from the National Health and Nutrition Examination Survey database. Note differences in control between all treated hypertensive patients and treated hypertensive diabetic patients. BP indicates blood pressure. aP<.05 for the difference between 1999–2000 and 2003–2004. Modified from Ong et al. 5
A 2007 national online survey of 1245 hypertensive individuals indicates, however, that an improvement in knowledge about and treatment of hypertension is occurring in the United States. More than 90% of respondents were aware that elevated BP is a major risk factor for cardiovascular disease. 15 The majority of participants discovered that they had elevated BP levels on a routine examination, and more than two‐thirds identified 120/80 mm Hg as an optimal BP level. More than 50% were involved in some lifestyle change to control BP, and >90% were taking medication. More than 60% reported that their BP was controlled (<140/90 mm Hg) at the last physician visit. Control rates as reported by respondents were >60% based on last BP recorded; however, between 31% and 40% of patients (based on differences in ethnic groups) were continued on the same therapy despite elevated BP levels, a clear indication that lack of physician adherence to therapy may be a major factor in patients with so‐called difficult‐to‐treat hypertension. These data are consistent with the most recent 2003–2004 NHANES data and suggest that dealing with physician inertia may be an important variable in achieving higher BP control rates. 5
This trend in improving BP control rates is seen in clinical trials as well. In the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) study 16 (mean follow‐up of 4.8 years), in 48% of patients on losartan plus a diuretic and 45% on atenolol plus a diuretic both an SBP level <140 mm Hg and diastolic BP level (DBP) <90 mm Hg were achieved. In the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), 17 ≥3 drugs were required in 27.3% of the participants, but in 68% of patients in the chlorthalidone group, 66.3% in the amlodipine group, and 61.2% in the lisinopril group, BP goal was achieved at 5 years. In the more recent International Verapamil‐Trandorapril Study (INVEST), 18 in 65% of the patients in the calcium‐antagonist arm and 64% in the non‐calcium antagonist arm, the goal for SBP was reached and DBP goal was reached in 88.5% compared with 88.1% at 24 months of follow‐up. Of note, these levels of control were achieved with the use of 3.2 drugs on average. Similarly, other major trials have used multiple drug therapy (Figure 2) to achieve control in a majority of patients. Recent data from the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension (ACCOMPLISH) trial 19 indicate that a strategy of starting with fixed‐dose combination BP‐lowering therapy yields a higher percentage of BP control earlier.
Figure 2.

Number of blood pressure (BP) medications needed to achieve systolic BP goal in large clinical trials. Most of the trials involved patients with multiple risk factors or comorbidities. CKD indicates chronic kidney disease; HOT, Hypertension Optimal Treatment trial; UKPDS, United Kingdom Prospective Diabetes Study; ALLHAT, Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial; INVEST, International Verapamil‐Trandolapril Study; MDRD, Modification of Diet in Renal Disease study; ABCD, Appropriate Blood Pressure Control in Diabetes trial; AASK, African American Study of Kidney Disease and Hypertension; IDNT, Irbesartan in Diabetic Nephropathy Trial; RENAAL, Reduction in Endpoints in NIDDM With the Angiotensin II Antagonist Losartan study.
While overall control rates are improving, they remain far below the goals in one group of patients with hypertension—those with diabetes or kidney disease or who are prone to kidney disease (ie, blacks and Hispanic persons). 20 , 21 Analyses of the NHANES database as well as the recent Kidney Early Evaluation Program (KEEP) database of >80,000 persons screened with kidney disease indicate that control rates for a BP goal of <130/80 mm Hg are <35%. 22 , 23 , 24 , 25 In 3258 Framingham offspring cohort members, the age‐ and sex‐adjusted prevalence of cardiovascular disease risk factors and their treatment and control were examined between 1998 and 2001 among persons with and without kidney disease. Those with kidney disease had a higher prevalence of hypertension (71.2% vs 42.7%; P<.001) and hypertension treatment (86.0% vs 72.5%; P<.001), but it was less likely that optimal BP control (<130/80 mm Hg) was reached in their cases (27.0% vs 45.5%; P<.001). 23 A separate study of patients with diabetes demonstrated that participants aged 20 years and older with previously diagnosed diabetes in either NHANES III (n=1265) or NHANES 1999–2000 (n=441) only had a control rate of 35.8% for the target SBP of <130 mm Hg and DBP<80 mm Hg. 22 Moreover, 40.4% had hypertensive BP levels (SBP ≥140 or DBP ≥90 mm Hg). Clearly, this trend in achievement of BP goals is improving in this subgroup but is lagging behind the general population (Figure 1). It should be noted, however, that goal BP levels for these patients have been set at lower levels (from <140/90 to <130/80 mm Hg) only in the past few years.
There is a difference between resistant hypertension and poor control rates in patients with stage 2 hypertension who may be underdosed or have inappropriate combinations of antihypertensive medication used to lower BP. As noted above, ≥2 drugs are required in >75% of patients with hypertension to achieve a BP goal. Initiating 2‐drug antihypertensive therapy will achieve BP control faster. 26 Moreover, addition of a second drug to monotherapy may not achieve goal BP levels over the same period of time. 24 Thus, as supported by the JNC 7, patients whose BP is 20/10 mm Hg above goal BP (ie, either 130/80 mm Hg for patients with diabetes or kidney disease or 140/90 mm Hg for the general population) should be started on combination therapy initially.
Resistant Hypertension
The prevalence of resistant hypertension has never been examined properly in an adequate sample of the overall hypertensive population. 27 , 28 Prevalence ranges from around 5% in general practice, with little selection of patients, to 50% or higher in specialty clinics. 27 , 29
As shown in Table II, various factors contribute to the failure to achieve BP goals and thus produce the perception of resistant hypertension, which may not be truly resistant. 2 , 27 , 30 , 31 The following factors should be considered before labeling hypertension as resistant: inadequate BP measurement technique (single readings, wrong position, use of inadequate cuff sizes); the presence of heavily calcified or arteriosclerotic arteries that cannot be fully compressed (in some elderly individuals), 32 which can result in overestimation of intra‐arterial BP; and pseudoresistance, noted in patients with an elevated BP under appropriate treatment in the office but with normal BP at home or with the use of ambulatory BP monitoring, what is referred to as white‐coat hypertension.
Table II.
Possible Causes of Resistant Hypertension
| Improper blood pressure measurement |
| Physician inertia (failure to change or increase dose regimens when not at goal) |
| Related to antihypertensive medication |
| Inadequate doses |
| Inappropriate combinations |
| Pseudoresistance |
| Patient nonadherence |
| Adverse effects of medication |
| Costs of medication |
| Inconvenient dosing schedules |
| Inadequate patient education |
| Memory or psychiatric problems |
| Drug‐induced |
| Nonsteroidal anti‐inflammatory drugs; cyclooxygenase‐2 inhibitors |
| Cocaine, amphetamines, other illicit drugs |
| Sympathomimetics (decongestants, anorectics) |
| Oral contraceptive hormones |
| Adrenal steroid hormones |
| Cyclosporine and tacrolimus |
| Erythropoietin |
| Licorice (including some chewing tobacco) |
| Selected over‐the‐counter dietary supplements and medicines (eg, ma haung, bitter orange) |
| Identifiable causes of hypertension |
| Volume overload |
| Excess sodium intake |
| Volume retention from kidney disease |
| Inadequate diuretic therapy |
| Associated conditions |
| Chronic kidney disease |
| Obesity |
| Sleep apnea |
| Diabetes |
| Excess alcohol intake |
One in 4 patients referred for apparent resistant hypertension turns out to have normal BP when ambulatory measurements are used. 33 Limited patient adherence to a properly dosed antihypertensive regimen is another important cause of perceived resistant hypertension. Limited adherence may relate to various factors such as medication adverse effects, complicated dosing schedules, presence of memory deficits, or high cost of medication, particularly relevant in countries without public health systems (eg, the United States).
From the list of factors associated with resistant hypertension, studies show that a suboptimal antihypertensive regimen appears to be a primary cause in a majority of patients. 29 Systematic use of drugs that interfere with antihypertensive drug mechanisms such as nonsteroidal anti‐inflammatory drugs or sympathomimetics (nasal vasoconstrictors, anorectics) can also contribute to development of resistant hypertension. In addition, the presence of an identifiable medical cause of hypertension must be considered, as it has been estimated that about 10% of patients with “resistant” hypertension have previously undiagnosed identifiable hypertension. 34 The most common medical cause of secondary hypertension is renal parenchymal disease.
BP control rates in patients with type 2 diabetes are about 20% below that of the general population (Figure 1). The concept of physician inertia (ie, underdosing and underutilizing medications especially diuretics, when patients' BP is not at goal) has been emphasized repeatedly. 35
Another factor that may contribute to lack of BP goal achievement in patients with type 2 diabetes is the number of antihypertensive medications needed to reach BP goal in many cases of diabetic nephropathy (Figure 2). In randomized clinical trials of people with diabetes and/or kidney disease, however, this does not appear to be a major barrier to achieving BP control rates of at least 50% or more. 19 , 36 , 37 , 38 Thus, physician inertia and failing to educate patients on the importance of achieving goals, both of which are addressed in trials, are important factors to consider.
Most cases of resistant hypertension are seen in the elderly, especially those with isolated systolic hypertension, and in patients with nephropathy (eGFR <60 mL/min). 28 , 30 , 39 Obesity, a common finding in patients with resistant hypertension, can interfere with BP control through various mechanisms (eg, relative reductions in active drug levels, severe insulin resistance and hyperinsulinemia, or presence of obstructive sleep apnea). 40
A key factor in persons with kidney disease and obesity relates to high sodium ingestion. Most hypertensive patients have an inordinately high dietary salt intake, with processed foods being the most common source in Western societies. 41 In addition, an important and generally unrecognized factor related to “resistance” is volume overload in individuals with early kidney disease. Thus, to optimize the approach to achieving BP goals, these patients must be counseled properly on a low‐sodium diet, and the doses of antihypertensive medications must be appropriate for morbidly obese patients. Last, appropriate doses of diuretics are important in this setting. Specifically, in patients with an eGFR <50 mL/min, the use of thiazide diuretics, especially in low doses, is inadequate and inappropriate to achieve BP reduction. In these patients, either furosemide 2 or 3 times daily or a longer‐acting loop diuretic such as torosemide should be given to ensure adequate volume control. Thus, if an appropriately dosed diuretic is used along with appropriately dosed agents such as calcium antagonists and blockers of the renin‐angiotensin system and BP goal is still not achieved, the hypertension can be considered to be truly resistant.
Status of Hypertension Treatment in Hard‐to‐Manage Hypertension
Despite the efforts to translate evidence‐based medicine in the field of hypertension into clear recommendations for clinical practice, 2 many physicians in the United States are reluctant to adhere to updated guidelines. 42 This attitude can be a major cause of the high prevalence of resistant hypertension. A previous survey of a national sample of primary care physicians showed that at a time when JNC VI guidelines clearly recommended treatment of BP levels ≥140/90 mm Hg, 43 for middle‐aged patients with uncomplicated hypertension 43% of physicians would start treatment only if SBP was >160 mm Hg and 33% if DBP was >95 mm Hg. In patients without complications who were receiving treatment, 33% of physicians would not intensify therapy for a persistent SBP of 158 mm Hg and 25% for a DBP of 94 mm Hg. Of note, 41% of the physicians were not familiar with JNC guidelines. Moreover, in spite the recommendations for initiating therapy with a diuretic or a β‐blocker, angiotensin‐converting enzyme (ACE) inhibitors were the most common first‐step drug. 44 Similarly, in a study in a large Midwestern health system, primary care physicians on average reported that 150 mm Hg was the lowest SBP level at which they would recommend pharmacologic treatment. 45 At 93% of patient visits, SBP values were ≥140 mm Hg, but pharmacologic therapy was initiated or changed at only 38% of visits. The most cited reasons for this related to the fact that physicians were satisfied with the patients' BP levels.
In addition, both primary care physicians and those involved in the treatment of elderly persons are generally less aggressive when treating hypertension. Another nationwide physician survey reported that 25% believed that hypertension treatment in an 85‐year‐old patient has more risks than benefits. 46 These physicians were significantly more likely to recommend lifestyle modifications, start antihypertensive therapy at a lower BP level, and target a lower BP goal in 65‐year‐old patients compared with 85‐year‐old patients. Again, diuretics were less likely to be used as first‐step drugs in older patients, despite clear recommendations and abundant data on benefit. 43
SUGGESTED APPROACH TO REDUCE THE INCIDENCE OF RESISTANT HYPERTENSION
A reasonable approach for evaluating resistant hypertension has been put forth by Moser and Setaro 29 (Figure 3). There are still some specific issues to be addressed.
Figure 3.

An approach to improve blood pressure (BP) control in resistant hypertension. NSAIDs indicates nonsteroidal anti‐inflammatory drugs. Reproduced with permission from Moser and Setaro. 29
In many obese patients, sleep apnea is an unappreciated identifiable cause of hypertension. 47 Obstructive sleep apnea appears to predispose individuals to autonomic imbalance characterized by sympathetic overactivity and altered barore‐flex mechanisms as well as alterations in vascular function. Treatment of symptomatic obstructive sleep apnea, particular if it is severe, is associated with improvements in BP, both during sleep and wakefulness; there may also be additional gains in individuals who are hypertensive and/or have hypertension that is resistant to antihypertensive medications. Plasma aldosterone levels are also elevated in persons with sleep apnea. 48 In a recent study, 71 consecutive patients referred for resistant hypertension (BP uncontrolled on 3 medications) and 29 control participants were prospectively evaluated by measurement of early morning plasma aldosterone concentration and renin level and by overnight, attended polysomnography. The study showed that obstructive sleep apnea was present in 85% of individuals with resistant hypertension. In these patients, plasma aldosterone levels strongly correlated with the magnitude of hypertension, but renin levels did not. 48 Similar data regarding BP responsive to aldosterone receptor blockade have been noted in obese African Americans without sleep apnea. 49 Thus, in addition to weight loss, the use of aldosterone antagonists might be useful in such situations.
In obese patients, weight reduction is the obvious, important step, but it usually is a complex issue. Long‐term weight reduction, which is necessary to sustain BP control, is currently not successful in >80% of overweight or obese hypertensive patients. 50 Use of an appropriately selected and dosed diuretic to decrease volume overload remains a cornerstone of therapy. 2 Thiazide diuretics become less effective when glomerular filtration rate (GFR) falls below 50 mL/min/1.73 m2, with the exception of chlorthalidone that can still be effective with GFR levels at 40 mL/min. If the physician is not aware of these associations, certain patients may not receive an appropriate diuretic regimen. Further, if a loop diuretic (usually furosemide) is used, it should be dosed at least twice daily. Furosemide has a short duration of action (3–6 hours), thus leaving the patient to reaccumulate volume that was just diuresed in the earlier part of the day if used only once daily. Focusing on the eGFR levels given on laboratory reports to determine kidney function will enable the physician to prescribe the appropriate diuretic. (Currently, GFR is mandated to be reported on laboratory slips in only 11 states.)
In many cases, however, appropriate use of 3 antihypertensive agents is not enough to achieve BP goal. It is not uncommon to add agents such as β‐blockers and vasodilators (eg, hydralazine and minoxidil) and still not achieve BP goal in a small subset of patients who could benefit from other antihypertensive therapy.
Neutral endopeptidases/ACE inhibitors have shown promise but were found to have serious adverse effects. 51 Another class of agents under investigation are the selective endothelin (ET)‐A receptor antagonists. Increasing evidence indicates that the ET system contributes to the development of hypertension secondary to its role in kidney disease development and receptor changes that occur in hypertriglyceridemic conditions and with aging. 52 , 53
Inhibition of ET‐1 54 through blockade of selective ET‐A receptors or improvement in insulin resistance is associated with changes in ET receptor binding 53 , 55 and contributes to BP reduction. This class of agents is currently under investigation in resistant hypertension in patients already receiving 4 maximally dosed drugs. Initial data support the notion that this class of agents has an antihypertensive effect.
THE FUTURE OF BP MANAGEMENT
Confluence of Risk Factors
The future perspectives of BP management should be examined in the context of confluence of all the aforementioned factors associated with resistant hypertension. The prevalence of obesity has been steadily increasing over the past decades in the industrialized world. Among US adults, 19.8% had a body mass index (BMI) ≥30 kg/m2 in 2000 and 20.9% did in 2001, an annual increase of 5.6%. 7 In a recent survey, >50% of patients with hypertension had a BMI >30 kg/m2. 15 Increasing rates of obesity are associated with increased prevalence of diabetes, high BP, and elevated cholesterol levels. 7 The worldwide burden of type 2 diabetes is estimated to rise from 124 million persons in 1997 to 221 million in 2010, 56 with an increased prevalence of the metabolic syndrome in developed societies on both sides of the Atlantic. 57 , 58
In addition, the prevalence of kidney disease is also high and is rapidly increasing. Data from NHANES III suggested that the prevalence of chronic kidney disease in the United States was roughly 11%, with more than 20 million adults estimated to suffer from the disease. 8 , 59 The United States Renal Data System estimates that by the year 2030, >2.2 million persons in the United States will require treatment for end‐stage renal disease. 60
Because the frequency of all of these conditions increases with advancing age, 4 , 7 , 8 , 9 , 58 continuous aging of the US population 61 will be a major factor driving the future rise in prevalence of hypertension. Further, it can be anticipated that if the state of hypertension management remains the same, these trends in associated risk factors will result in even lower control rates and higher rates of resistant hypertension.
Role of the Physician in Improving Hypertension Treatment and Control
Improving hypertension awareness in the general population seems a task that requires a multilevel approach and involvement of various agencies, from federal and state health agencies to professional and public organizations. As evident from the discussion above, however, physicians are the most crucial players in improving hypertension treatment and control. The familiarity of the average primary care physician with JNC guidelines should be improved, given that increased familiarity with guidelines or research methods has been shown to be associated with lower treatment thresholds and greater use of diuretics or β‐blockers as first‐line agents. 44 In addition to adhering to these guidelines, physicians should transfer their knowledge to their patients as effectively as possible (Table III). Recently developed tools are believed to provide more accurate and objective evaluations of adherence to guidelines, enabling organizations to identify specific problematic areas in treatment practice. 62 In communications with patients, the physician has to ensure that they are educated about the risks of uncontrolled hypertension, the value of lifestyle modifications, and the benefits of treatment and are motivated toward an appropriate BP goal. A recent survey suggests that this may be occurring. 15 Then, an appropriate regimen with optimal doses of antihypertensive medications should be prescribed based on patient characteristics, aggressively to currently recommended goals.
Table III.
Actions to Be Taken by Physicians to Improve Hypertension Treatment and Control
| Become familiar with and adhere to the most recent hypertension guidelines. |
| Educate the patient on the risks of uncontrolled hypertension, the value of lifestyle modifications, and the benefits of drug treatment. |
| Motivate the patient toward an appropriate BP goal. |
| Treat aggressively with optimal doses of antihypertensive medications according to patient characteristics and recommended goals. |
| Follow up with the patient effectively to evaluate BP control. |
| Monitor the patient's adherence to the treatment regimens. |
| Perform appropriate adjustments and/or changes of the antihypertensive medication. |
| Carefully evaluate the possibility of resistant hypertension; identify and correct remediable causes. |
| Refer recalcitrant cases to a hypertension specialist. |
If the patient appears to have resistant hypertension, 2 a careful evaluation should be done. Home or ambulatory BP measurement may be an important step. 33 When BP remains elevated, 2 primary factors should be considered, physician inertia with medications and doses and patient adherence to therapy. Given that a recent survey found that 31% of patients whose BP levels were not at goal were still continued on the same antihypertensive regimen, 15 physicians should pay attention to their own behavior as well as that of their patients. If the patient's poor adherence to therapy is the cause, the physician should discuss adverse effects and cost with the patient because these are the most common factors involved. 31 The physician must also ensure that the patient does not have an inordinately high sodium intake (>4 g/d). Drug interactions must also be evaluated and corrected, and a careful search for identifiable causes of hypertension should be conducted, including an assessment of kidney function by measuring eGFR. If, after all these procedures, BP still cannot be controlled or if GFR is <40–50 mL/min/1.73 m2, the patient should be referred to a hypertension specialist.
CONCLUSIONS
The unadjusted and age‐adjusted prevalence of hypertension and conditions associated with the development of hypertension are increasing in the United States. Current treatment practices are only partially achieving acceptable rates of BP control. Because of demographic and disease trends, resistant hypertension is likely to become more prevalent; physicians will need to be particularly vigilant with this specific patient population. Adherence to current guidelines, aggressive therapy toward BP goals, and close cooperation with patients as well as the development of newer medical therapies may help to ensure future success and higher goal attainment rates.
References
- 1. Kaplan NM. Primary hypertension: pathogenesis. In: Kaplan NM, ed. Clinical Hypertension. 8th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2002:56–135. [Google Scholar]
- 2. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High BP: the JNC 7 report. JAMA. 2003;289(19):2560–2572. [DOI] [PubMed] [Google Scholar]
- 3. Burt VL, Cutler JA, Higgins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26(1):60–69. [DOI] [PubMed] [Google Scholar]
- 4. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(2):199–206. [DOI] [PubMed] [Google Scholar]
- 5. Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75. [DOI] [PubMed] [Google Scholar]
- 6. Smith NL, Chen L, Au DH, et al. Cardiovascular risk factor control among veterans with diabetes: the ambulatory care quality improvement project. Diabetes Care. 2004;27(suppl 2):B33–B38. [DOI] [PubMed] [Google Scholar]
- 7. Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity‐related health risk factors, 2001. JAMA. 2003;289(1):76–79. [DOI] [PubMed] [Google Scholar]
- 8. Coresh J, Astor BC, Greene T, et al. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41(1):1–12. [DOI] [PubMed] [Google Scholar]
- 9. Fields LE, Burt VL, Cutler JA, et al. The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension. 2004;44(4):398–404. [DOI] [PubMed] [Google Scholar]
- 10. Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–e171. [DOI] [PubMed] [Google Scholar]
- 11. Whyte JL, Lapuerta P, L'Italien GJ, et al. The challenge of controlling systolic BP: data from the National Health and Nutrition Examination Survey (NHANES III), 1988–1994. J Clin Hypertens (Greenwich). 2001;3(4):211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Colhoun HM, Dong W, Poulter NR. BP screening, management and control in England: results from the health survey for England 1994. J Hypertens. 1998;16(6):747–752. [DOI] [PubMed] [Google Scholar]
- 13. Sarafidis PA, Lasaridis A, Gousopoulos S, et al. Prevalence, awareness, treatment and control of hypertension in employees of factories of Northern Greece: the Naoussa study. J Hum Hypertens. 2004;18(9):623–629. [DOI] [PubMed] [Google Scholar]
- 14. Wolf‐Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43(1):10–17. [DOI] [PubMed] [Google Scholar]
- 15. Moser M, Franklin SS. Hypertension management: results of a new national survey for the hypertension education foundation: Harris interactive. J Clin Hypertens (Greenwich). 2007;9(5):316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dahlof B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995–1003. [DOI] [PubMed] [Google Scholar]
- 17. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group . Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288(23):2981–2997. [DOI] [PubMed] [Google Scholar]
- 18. Pepine CJ, Handberg EM, Cooper‐DeHoff RM, et al. A calcium antagonist vs a non‐calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil‐Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290(21):2805–2816. [DOI] [PubMed] [Google Scholar]
- 19. Jamerson K, Bakris GL, Dahlof B, et al. Exceptional early BP control rates: the ACCOMPLISH trial. Blood Press. 2007;16(2):80–86. [DOI] [PubMed] [Google Scholar]
- 20. Malik S, Lopez V, Chen R, et al. Undertreatment of cardiovascular risk factors among persons with diabetes in the United States. Diabetes Res Clin Pract. 2007;77(1):126–133. [DOI] [PubMed] [Google Scholar]
- 21. Wong ND, Lopez V, Tang S, et al. Prevalence, treatment, and control of combined hypertension and hypercholesterolemia in the United States. Am J Cardiol. 2006;98(2):204–208. [DOI] [PubMed] [Google Scholar]
- 22. Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291(3):335–342. [DOI] [PubMed] [Google Scholar]
- 23. Parikh NI, Hwang SJ, Larson MG, et al. Cardiovascular disease risk factors in chronic kidney disease: overall burden and rates of treatment and control. Arch Intern Med. 2006;166(17):1884–1891. [DOI] [PubMed] [Google Scholar]
- 24. Chua DY, Bakris GL. Diabetes and chronic kidney disease: tragedy and challenge. Blood Purif. 2004;22(1):130–135. [DOI] [PubMed] [Google Scholar]
- 25. KEEP Annual Data Report. Am J Kidney Dis. 2007;49(3 suppl 2):1–232. 17185139 [Google Scholar]
- 26. Bakris GL, Weir MR. Achieving goal BP in patients with type 2 diabetes: conventional versus fixed‐dose combination approaches. J Clin Hypertens (Greenwich). 2003;5(3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kaplan NM. Resistant hypertension. J Hypertens. 2005;23(8):1441–1444. [DOI] [PubMed] [Google Scholar]
- 28. Taler SJ. Treatment of resistant hypertension. Curr Hypertens Rep. 2005;7(5):323–329. [DOI] [PubMed] [Google Scholar]
- 29. Moser M, Setaro JF. Clinical practice. Resistant or difficult‐to‐control hypertension. N Engl J Med. 2006;355(4):385–392. [DOI] [PubMed] [Google Scholar]
- 30. Calhoun DA, Zaman MA, Nishizaka MK. Resistant hypertension. Curr Hypertens Rep. 2002;4(3):221–228. [DOI] [PubMed] [Google Scholar]
- 31. Hall WD. Resistant hypertension, secondary hypertension, and hypertensive crises. Cardiol Clin. 2002;20(2):281–289. [DOI] [PubMed] [Google Scholar]
- 32. Oster JR, Materson BJ. Pseudohypertension: a diagnostic dilemma. J Clin Hypertens. 1986;2(4):307–313. [PubMed] [Google Scholar]
- 33. Brown MA, Buddle ML, Martin A. Is resistant hypertension really resistant? Am J Hypertens. 2001;14(12):1263–1269. [DOI] [PubMed] [Google Scholar]
- 34. Yakovlevitch M, Black HR. Resistant hypertension in a tertiary care clinic. Arch Intern Med. 1991;151(9):1786–1792. [PubMed] [Google Scholar]
- 35. Nilsson PM, Gudbjornsdottir S, Eliasson B, et al. Hypertension in diabetes: trends in clinical control in repeated large‐scale national surveys from Sweden. J Hum Hypertens. 2003;17(1):37–44. [DOI] [PubMed] [Google Scholar]
- 36. Wright JT Jr, Bakris G, Greene T, et al. Effect of BP lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288(19):2421–2431. [DOI] [PubMed] [Google Scholar]
- 37. Pepine CJ, Handberg EM, Cooper‐DeHoff RM, et al. A calcium antagonist vs a non‐calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil‐Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290(21):2805–2816. [DOI] [PubMed] [Google Scholar]
- 38. Bakris GL, Weir MR, Shanifar S, et al. Effects of BP level on progression of diabetic nephropathy: results from the RENAAL study. Arch Intern Med. 2003;163(13):1555–1565. [DOI] [PubMed] [Google Scholar]
- 39. Bakris GL, Fonseca V, Katholi RE, et al. Differential effects of beta‐blockers on albuminuria in patients with type 2 diabetes. Hypertension. 2005;46(6):1309–1315. [DOI] [PubMed] [Google Scholar]
- 40. Logan AG, Perlikowski SM, Mente A, et al. High prevalence of unrecognized sleep apnoea in drug‐resistant hypertension. J Hypertens. 2001;19(12):2271–2277. [DOI] [PubMed] [Google Scholar]
- 41. Dickinson BD, Havas S. Reducing the population burden of cardiovascular disease by reducing sodium intake: a report of the Council on Science and Public Health. Arch Intern Med. 2007;167(14):1460–1468. [DOI] [PubMed] [Google Scholar]
- 42. Hypertension in America: a national reading. Am J Manag Care. 2005;11(suppl 13):S383–S385. [PubMed] [Google Scholar]
- 43. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157(21):2413–2446. [DOI] [PubMed] [Google Scholar]
- 44. Hyman DJ, Pavlik VN. Self‐reported hypertension treatment practices among primary care physicians: BP thresholds, drug choices, and the role of guidelines and evidence‐based medicine. Arch Intern Med. 2000;160(15):2281–2286. [DOI] [PubMed] [Google Scholar]
- 45. Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician‐related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162(4):413–420. [DOI] [PubMed] [Google Scholar]
- 46. Hajjar I, Miller K, Hirth V. Age‐related bias in the management of hypertension: a national survey of physicians' opinions on hypertension in elderly adults. J Gerontol A Biol Sci Med Sci. 2002;57(8):M487–M491. [DOI] [PubMed] [Google Scholar]
- 47. Phillips CL, Cistulli PA. Obstructive sleep apnea and hypertension: epidemiology, mechanisms and treatment effects. Minerva Med. 2006;97(4):299–312. [PubMed] [Google Scholar]
- 48. Pratt‐Ubunama MN, Nishizaka MK, Boedefeld RL, et al. Plasma aldosterone is related to severity of obstructive sleep apnea in subjects with resistant hypertension. Chest. 2007;131(2):453–459. [DOI] [PubMed] [Google Scholar]
- 49. Calhoun DA. Low‐dose aldosterone blockade as a new treatment paradigm for controlling resistant hypertension. J Clin Hypertens (Greenwich). 2007;9(1 suppl 1):19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Douketis JD, Sharma AM. The management of hypertension in the overweight and obese patient: is weight reduction sufficient? Drugs. 2004;64(8):795–803. [DOI] [PubMed] [Google Scholar]
- 51. Ferdinand KC. Advances in antihypertensive combination therapy: benefits of low‐dose thiazide diuretics in conjunction with omapatrilat, a vasopeptidase inhibitor. J Clin Hypertens (Greenwich). 2001;3(5):307–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Neuhofer W, Pittrow D. Role of endothelin and endothelin receptor antagonists in renal disease. Eur J Clin Invest. 2006;36(suppl 3):78–88. [DOI] [PubMed] [Google Scholar]
- 53. Rubio ME, Banos G, Diaz E, et al. Effect of age on insulin‐induced endothelin release and vasoreactivity in hypertriglyceridemic and hypertensive rats. Exp Gerontol. 2006;41(3):282–288. [DOI] [PubMed] [Google Scholar]
- 54. Schiffrin EL. Vascular endothelin in hypertension. Vascul Pharmacol. 2005;43(1):19–29. [DOI] [PubMed] [Google Scholar]
- 55. Sarafidis PA, Bakris GL. Protection of the kidney by thiazolidinediones: an assessment from bench to bedside. Kidney Int. 2006;70(7):1223–1233. [DOI] [PubMed] [Google Scholar]
- 56. Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med. 1997;14(suppl 5):S1–S85. [PubMed] [Google Scholar]
- 57. Beck‐Nielsen H. General characteristics of the insulin resistance syndrome: prevalence and heritability. European Group for the study of Insulin Resistance (EGIR). Drugs. 1999;58(suppl 1):7–10. [DOI] [PubMed] [Google Scholar]
- 58. Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among US Adults. Diabetes Care. 2004;27(10):2444–2449. [DOI] [PubMed] [Google Scholar]
- 59. National Kidney Foundation . K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Kidney Disease Outcome Quality Initiative. Am J Kidney Dis. 2002;39(2 suppl 1):S1–S266. [PubMed] [Google Scholar]
- 60. U.S. Renal Data System. USRDS 2004 Annual Data Report: Atlas of End‐Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2004. [Google Scholar]
- 61. Sonnenschein E, Brody JA. Effect of population aging on proportionate mortality from heart disease and cancer, U.S. 2000–2050. J Gerontol B Psychol Sci Soc Sci. 2005;60(2):S110–S112. [DOI] [PubMed] [Google Scholar]
- 62. Milchak JL, Carter BL, Ardery G, et al. Development of explicit criteria to measure adherence to hypertension guidelines. J Hum Hypertens. 2006;20(6):426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]


