Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic is a public health emergency that has affected many world nations, including Ethiopia. Aside from its implications on the community as a whole, COVID-19 has also been associated with a variety of mental health problems among healthcare workers (HCWs). In this study, we aim to assess the prevalence of self-reported symptoms of depression, anxiety, and stress during the COVID-19 pandemic among HCWs in central Ethiopia.
Methods
An institutional-based cross-sectional study was conducted using an online survey from June 25, 2020, to July 25, 2020, in Ethiopia. Data were collected using a self-reported Depression, Anxiety, and Stress Scale (DASS-21). Data were cleaned, coded, and analysed using SPSS Version 23. A multivariable logistic regression analysis was done to identify the associated factors for mental health outcomes at a p-value of less than 0.05.
Results
A total of 816 HCWs completed the self-report questionnaire. The percentage of HCWs who had moderate to extremely severe symptoms of depression, anxiety, and stress were 60.3%, 78%, and 33.8%, respectively. Female participants, HCWs in the Oromiya Special Zone, medical laboratory professionals, and HCWs working in the COVID-19 treatment isolation centers were significantly more likely to have symptoms of depression, anxiety, and stress.
Conclusion
In this study, HCWs reported a high prevalence of depression, anxiety, and stress symptoms. Female participants, HCWs in the Oromiya Special Zone, medical laboratory professionals, and HCWs working in the COVID-19 treatment isolation centers were significantly more likely to have symptoms of depression, anxiety, and stress. It is imperative that the Ethiopian Federal Ministry of Health should develop psychological interventions to address the specific needs of HCWs who have been impacted by the COVID-19 pandemic.
Keywords: COVID-19, anxiety, depression, stress, health care workers, Ethiopia
Introduction
The COVID-19 pandemic is a public health emergency that has rapidly spread worldwide, starting in Wuhan city, China on December 31, 2019.1 By July 30, 2020, there were more than 10.2 million infections with 500,000 confirmed deaths reported by the World Health Organization globally. In Africa, a total of 97,508 infected cases and 3,020 deaths have been reported. In Ethiopia specifically, an alarming total of 9,589 cases and 263 deaths have occurred.2 The pandemic has not only impacted the economy and caused social isolation but has also been associated with several mental health problems among health care workers (HCWs).3 A high prevalence of stress, anxiety, and depression has been found among HCWs.4
The COVID-19 pandemic may lead to depression, anxiety, and stress among HCWs. Most HCWs are likely to experience symptoms of depression, anxiety, stress, fear of falling sick or dying themselves, feelings of helplessness, self-harm or suicide, and stigma as a result of the COVID-19 pandemic.5,6 A study conducted in China found that 73.4% of frontline HCWs in a hospital suffered from extreme stress levels, 50.7% had depressive symptoms, 44.7% had anxiety, and 36.1% had insomnia.7 Another study from China among HCWs treating patients exposed to COVID-19 found that 50.4% suffered from depression symptoms, 44.6% had anxiety, 34.0% had insomnia, and 71.5% had distress.8 A study done in Singapore and India among HCWs indicated that 8.7% had moderate to very severe anxiety, 5.3% had moderate to extremely severe depression, and 2.2% had moderate to extremely-severe stress.9 A web-based cross-sectional survey was conducted among HCWs during the COVID-19 pandemic indicated that 44.37% of HCWs had symptoms of depression, 46.04% had symptoms of anxiety, and 28.75% had experienced symptoms of insomnia, while another 56.59% report common overall psychological problems.10
As a consequence of the pandemic, HCWs are experiencing a number of stressors and emotional difficulties, including an extremely heavy workload, a shortage of personal protective equipment (PPE), a lack of specific drugs or vaccines, and the feeling of being inadequately supported.11–13 These stressors can contribute to the mental burden of HCWs, which could have long-term psychological implications and a lack of perceived psychological readiness.14–16
In order to minimize the risk of COVID-19 transmission in the community, many countries implemented a lockdown, travel restrictions, compulsory quarantine, working from home, and social/physical distancing measures. The Ethiopian government declared an emergency and mandated compulsory physical distancing, quarantine, frequent hand washing, and a reduction in public transportation capacity by half in efforts to reduce transmission of the virus. Despite all the efforts to contain the COVID-19 pandemic in low-resource countries, psychological distress among healthcare providers remains notably high in Sub-Saharan countries.17 A more inclusive evidence-based understanding of HCWs’ psychological burden during the COVID-19 is vital for providing psychological support, improving mental health services in low resource countries.18 The HCWs on the frontline who have been directly involved in the diagnosis, treatment, and care of patients with COVID-19 may be at significant risk of developing mental health problems. Therefore, we sought to assess the prevalence of self-reported symptoms of depression, anxiety, and stress among HCWs in central Ethiopia.
Methods
Study Design, Period, Area, and Population
An institution-based cross-sectional study was conducted in central Ethiopia, particularly in Addis Ababa, and the Oromiya region (Oromiya Special Zone, North Shoa, East Shoa, and West Shoa) from June 25, 2020 to July 25, 2020. All HCWs who were working in the selected clustered departments were included. HCWs that were on annual leave, or critically ill were excluded from the study.
Sample Size and Sampling Technique
The sample size was determined using Epi-Info version 7.5.1, considering the power of 80% with a 95% confidence interval and a 5% margin of error. Due to the lack of previous studies, we assumed a prevalence of 50% depression or anxiety or stress, and a nonresponse rate of 10%. After using design effect 2, the total required sample size to achieve a power of 80% was deemed to be 846. Samples were regionally stratified by their geographic location (Addis Ababa city administration, and Oromiya regional state). More health care facilities (HCFs) in Addis Ababa were randomly sampled as it was more severely affected than other areas. A total of 12 HCFs were selected from Addis Ababa (eight COVID-19 isolation treatment centers, and four governmental hospitals). Twelve HCFs were selected from Oromia regional state (two hospitals, one COVID-19 treatment isolation center from each of North Shoa, West Shoa, and East Shoa Zone of the Oromiya region as well as three COVID-19 isolation treatment center from the Oromiya Special Zone of the Oromiya region). From each hospital, two department clusters were taken (20 clusters in total), and a total of 14 clusters were taken from COVID-19 treatment centers. A total of 24 HCFs (10 hospitals and 14 COVID-19 treatment centers) were involved. All HCWs working in clustered departments were invited to complete the online surveys through e-mail. The participants received a reminder two weeks after the initial survey distribution. To prevent duplicated responses, we made Google account Setting to allow only one response per user. Participation in the study was completely voluntarily.
Data Collection Tools and Procedure
The questionnaires were completed in the Afan Oromo and Amharic languages using Google Forms. The questionnaire was adapted from a different study9,19,20 that was originally written in the English language, translated to Afan Oromo and Amharic, and then back-translated to English by language experts to check its consistency. Both translated questionnaires were pre-tested before actual data collection and a few questions were modified after discussion with the study teams. The demographic data included age, sex, marital status, region/location, residence, educational level, profession, working unit, and years of experience. Participants were asked whether they had taken the online training course for COVID-19 infection prevention and control methods, which is provided on the Ethiopian Ministry of Health website.21 The participants were also asked about the availability of PPE at their institutions (see Underlying data).22
Mental health outcomes for all participants were measured using the Depression, Anxiety, and Stress Scale (DASS-21).23 It contains three subscales with response ranging from 0 to 3 (“0” did not apply to me at all; “1” applied to me to some degree, or some of the time; “2” applied to me to a considerable degree or a good part of the time, and “3” applied to me very much or most of the time). The depression subscale contained 7 items regarding past week depressive symptom (item 3, “I couldn’t seem to experience any positive feeling at all during COVID-19”; item 5, “I found it difficult to work up the initiative to do things during the pandemic”; item 10, “I felt that I had nothing to look forward to COVID-19”; item 13, “I felt down-hearted and blue as a result of COVID-19”; item 16, “I was unable to become enthusiastic about anything during COVID-19”; item 17, “I felt I wasn’t worth much as a person during COVID-19”; and item 21, “I felt that life was meaningless during COVID-19”) (see Underlying data).22 The total depression subscale score was categorised into normal (score of 0–9), mild depression (10–13), moderate depression (14–20), severe depression (21–27), and extremely severe depression (28 and above).
The anxiety subscale contained 7 items regarding past week anxiety symptoms (item 2, “I was aware of dryness of my mouth thinking about COVID-19”; item 4, “I experienced breathing difficulty when thinking COVID-19”; item 7, “I experienced trembling (eg in the hands) as a result of COVID-19”; item 9, “I was worried about COVID-19 in which I might panic and make a fool of myself”; item 15, “I felt I was close to panic as a result of COVID-19”; item 19, “I was aware of the action of my heart in the absence of physical exertion during COVID-19”; and item 20. “I felt scared without any good reason during COVID-19”) (see Underlying data).22 The total anxiety subscale score was categorised into normal (0–7), mild anxiety (8–9), moderate anxiety (10–14), severe anxiety (15–19), and extremely severe anxiety (20 and above).
The stress subscale contained 7 items regarding past week stress symptoms (item 1, “I felt scared without any good reason during COVID-19”; item 6, “I tended to over-react to situations of COVID-19”; item 8, “I felt that I was using a lot of nervous energy during COVID-19”; item 11, “I found myself getting agitated due to COVID-19”; item 12, “I found it difficult to relax during COVID-19”; item 14, “I was intolerant of anything that kept me from getting COVID-19 with what I was doing”; and item 18, “I felt that I was rather touchy during COVID-19”) (see Underlying data).22 The total stress subscale score was categorised into normal (0–14), mild stress (15–18), moderate stress (19–25), severe stress (26–33), and extremely severe stress (34 and above). The final score was calculated by multiplying the crude score by 2.24
This questionnaire has been validated in African countries; the subscales of depression, anxiety, and stress have Cronbach’s alpha values of 0.81, 0.89, and 0.78, respectively.24 In this study again the tools subscale reliability was with Cronbach’s alpha 0.78 for depression, 86 for anxiety, and 83 for stress in a pre-tested questionnaire.
Data Processing and Analysis
Data were transferred from Google Forms using spreadsheet, and coded, edited, cleaned, and analysed using SPSS version 23. Descriptive data analysis was performed as well as bivariate and multivariable logistic regression. The outcome cut-off points for the binary logistic regression were above 9, 7, and 14 for depression, anxiety, and stress, respectively. The odds ratio with a 95% confidence interval (CI) and a two-tailed P-value was calculated to identify the associated factors. Variables with P-value ≤ 0.2 in the bivariate logistic regression analysis were included in the multivariable logistic regression analysis to control for the confounding variables.25 Statistical significance was declared if P-value < 0.05.
Ethical Consideration
This study was conducted in accordance with the Declaration of Helsinki. The study protocol and methodology were approved by Salale University Ethical Review Committee on June 15, 2020, with approval number SLUERC/046/2020. At the beginning of the questionnaire, the participants were informed about the study aims and how their data would be used, and that they would be consenting to take part by default if they completed the survey. The respondents were told that their inclusion in the study was voluntary, and they were free to withdraw from the study at any time. The respondents’ confidentiality was ensured by excluding their names from the questionnaire and by keeping their data in a password-locked computer.
Results
In this study, 846 HCWs were asked to participate, of which (816; 96.5%) completed the online survey. The majority (376; 46.1%) of respondents were from the Addis Ababa region. All participants resided in urban areas. A total of 244 (29.9%) participants were frontline HCWs that were directly involved in diagnosing COVID-19, caring for patients, or treating patients with confirmed or suspected COVID-19. The majority of participants were male (540; 66.2%), aged 26 to 30 years (308; 37.7%), married (476; 58.3%), and had an educational level of first degree or an undergraduate degree (332; 40.7%). Nurses (236; 28.9%) comprised the majority of HCWs. A total of 340 (41.7%) participants had 5 to 10 years of working experience in their field. More than two-thirds of study participants had completed training on COVID-19 infection prevention, and a total of 580 (71.1%) HCWs reported a shortage of personal protective equipment (Table 1).
Table 1.
Socio-Demographic Characteristics of Healthcare Workers in Central Ethiopia, from June 25, 2020 to July 25, 2020 (n=816)
| Variables | N (%) | Depression | Anxiety | Stress |
|---|---|---|---|---|
| X2, P-value | X2, P-value | X2, P-value | ||
| Age | ||||
| 20–25 | 140 (17.2) | 35.70, 0.001 | 23.86, 0.061 | 47.21, 0.001 |
| 26–30 | 308 (37.7) | |||
| 31–35 | 196 (24.0) | |||
| 36–40 | 100 (12.3) | |||
| >40 | 72 (8.8) | |||
| Sex | ||||
| Male | 540 (66.2) | 31.00, 0.001 | 25.23, 0.001 | 44.17, 0.001 |
| Female | 276 (33.8) | |||
| Marital status | ||||
| Single | 340 (41.7) | 56.72, 0.001 | 0.32, 0.569 | 34.19, 0.001 |
| Married | 476 (58.3) | |||
| Region/location | ||||
| Addis Ababa | 376 (46.1) | 86.19, 0.001 | 43.53, 0.001 | 76.79, 0.001 |
| Oromiya Special Zone | 112 (13.7) | |||
| East Shoa | 156 (19.1) | |||
| North Shoa | 96 (11.8) | |||
| West Shoa | 76 (9.3) | |||
| Educational status | ||||
| Diploma | 296 (36.3) | 6.52, 0.038 | 8.34, 0.015 | 31.07, 0.051 |
| BSc/MD | 332 (40.7) | |||
| MSc/specialty | 188 (23.0) | |||
| Profession | ||||
| Nurse | 236 (28.9) | 98.88, 0.001 | 11.64, 0.040 | 34.57, 0.001 |
| Physician | 136 (16.7) | |||
| Midwife | 192 (23.5) | |||
| Medical laboratory professionals | 68 (8.3) | |||
| Health officer | 96 (11.8) | |||
| Pharmacist | 88 (10.8) | |||
| Work department | ||||
| COVID-19 isolation center | 244 (29.9) | 37.30, 0.001 | 47.65, 0.001 | 42.98, 0.001 |
| Emergency | 88 (10.8) | |||
| Surgical | 116 (14.2) | |||
| Medical | 128 (15.7) | |||
| Outpatient department | 104 (12.7) | |||
| Laboratory | 62 (7.6) | |||
| Pharmacy | 74 (9.1) | |||
| Years of professional experience | ||||
| <5 Year | 268 (32.8) | 39.79, 0.001 | 22.97, 0.001 | 2.14, 0.343 |
| 5–10 years | 340 (41.7) | |||
| >10 years | 208 (25.5) | |||
| Taking online training about COVID-19 | ||||
| No | 268 (32.8) | 3.02, 0.082 | 7.32, 0.007 | 5.14, 0.023 |
| Yes | 548 (67.2) | |||
| PPE availability | ||||
| No | 580 (71.1) | 10.21, 0.001 | 0.54, 0.445 | 0.30, 0.585 |
| Yes | 236 (28.9) |
The Prevalence of Depression, Anxiety, and Stress
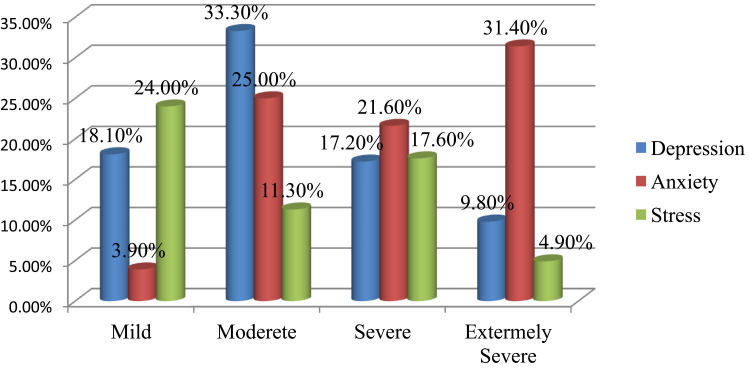
Among the 640 HCWs who screened positive for depression (scores >9), 60.3% (492) fell into the moderate to extremely severe depression subgroup. Of the 668 HCWs who screened positive for anxiety (scores >7), 78% (636) fell into the moderate to extremely severe anxiety subgroup. Of the 472 HCWs who screened positive for stress (scores >14), 33.8% (276) met the criteria for moderate to extremely severe stress (Figure 1).
Figure 1.
Prevalence of depression, anxiety, and stress among health care workers in central Ethiopia, from June 25, 2020 to July 25, 2020 (n=816).
Factors Associated with Depression, Anxiety, and Stress
The results of the bivariable and multivariable logistic regressions are documented in Table 2. In a multivariable logistic regression analysis, female HCWs who worked in the Oromiya Special Zone, medical laboratory professionals, and HCWs at the COVID-19 treatment isolation centers were significantly more likely to self-report symptoms of depression, anxiety, and distress.
Table 2.
Factors Associated with Depression, Anxiety, and Stress Among HCWs in Central Ethiopia, from June 25, 2020 to July 25, 2020 (n=816; Crude and Adjusted Odds Ratios, 95% Confidence Intervals)
| Variables | Depression | Anxiety | Stress | |||
|---|---|---|---|---|---|---|
| COR (95% CI) | AOR (95% CI) | COR (95% CI) | AOR (95% CI) | COR (95% CI) | AOR (95% CI) | |
| Age | ||||||
| 18–25 | 1 | 1 | 1 | 1 | 1 | 1 |
| 26–30 | 0.35 (0.23,0.54) | 0.32 (0.18,0.57)* | 0.51 (0.34,0.77) | 0.45 (0.39,1.07) | 0.24 (0.14,0.39) | 0.24 (0.13,0.43)* |
| 31–35 | 0.77 (0.50,1.21) | 0.60 (0.83,3.08) | 0.70 (0.44,1.09) | 0.65 (0.77,2.38) | 0.25 (0.15,0.43) | 0.20 (0.10,0.38)* |
| 36–40 | 0.42 (0.34,0.74) | 0.30 (0.23,1.13) | 0.29 (0.17,0.50) | 0.20 (0.27,1.07) | 0.16 (0.09,0.29) | 0.10 (0.05,0.22)* |
| >40 | 1.07 (0.60,1.89) | 0.97 (0.53,3.01) | 0.65 (0.37,1.17) | 0.51 (0.44,1.90) | 0.26 (0.14,0.49) | 0.16 (0.07,0.36)* |
| Sex | ||||||
| Male | 1 | 1 | 1 | 1 | 1 | 1 |
| Female | 2.38 (1.75,3.24) | 2.01 (1.25,3.23)* | 2.14 (1.59,2.89) | 1.91 (1.27,2.86)* | 2.88 (2.09,3.95) | 2.08 (1.33,3.24)* |
| Marital status | ||||||
| Single | 1 | 1 | 1 | 1 | 1 | 1 |
| Married | 3.55 (2.53,4.99) | 3.53 (2.15,5.80)* | 1.08 (0.82,1.43) | 0.83 (0.57,1.21) | 3.33 (1.75,3.10) | 3.15 (2.25,5.05)* |
| Location | ||||||
| Addis Ababa | 4.72 (2.07,10.66) | 3.83 (1.35,7.49)* | 1.67 (1.15,2.40) | 0.78 (0.38,1.60) | 3.66 (2.50,5.36) | 1.65 (0.78,3.58) |
| Oromiya Special Zone | 4.20 (2.76,12.87) | 3 94 (1.94,8.09)* | 2.57 (1.73,3.81) | 1.85 (1.14,2.99)* | 3.96 (2.64,5.95) | 2.14 (1.28,3.59)* |
| Central Oromiya | 1 | 1 | 1 | 1 | 1 | |
| Educational status | ||||||
| Diploma | 1.57 (1.04,2.38) | 0.51 (0.24,1.09) | 1.38 (0.96,1.99) | 1.23 (0.90,2.62)* | 1.46 (1.01,2.10) | 1.12 (0.62,2.02) |
| BSC/MD | 1.67 (1.11,2.50) | 0.36 (0.17,0.74)* | 1.70 (1.18,2.44) | 1.34 (0.80,2.24) | 2.71 (1.88,3.93) | 1.48 (0.83,2.63) |
| MSC/MPH/Specialty | 1 | 1 | 1 | 1 | ||
| Profession | ||||||
| Nurse | 3.31 (1.82,6.03) | 3.28 (1.90,8.33)* | 1.42 (0.87,2.33) | 1.40 (0.97,3.32) | 1.22 (0.74,1.99) | 0.87 (0.46,1.64) |
| Physician | 1.86 (0.97,3.61) | 2.22 (0.99,5.00) | 1.35 (0.79,2.31) | 1.29 (0.86,3.29) | 0.94 (0.55,1.61) | 0.76 (0.38,1.53) |
| Midwife | 0.90 (0.46,1.74) | 0.87 (0.36,2.10) | 1.20 (0.72,1.99) | 1.11 (0.66,2.60) | 0.71 (0.43,1.17) | 0.64 (0.32,1.29) |
| Medical laboratory professional | 5.80 (3.09,14.91) | 4.69 (2.81,9.17)* | 2.88 (1.48,5.63) | 2.75 (1.78,4.79)* | 2.71 (1.35,5.45) | 1.63 (1.27,2.47)* |
| Health officer | 0.90 (0.42,1.93) | 0.78 (0.46,2.99) | 1.20 (0.67,2.14) | 1.15 (0.62,2.49) | 2.50 (1.34,4.67) | 2.31 (0.21,5.65) |
| Pharmacist | 1 | 1 | 1 | 1 | 1 | |
| Work department | ||||||
| COVID-19 isolation centers | 2.77 (1.44,5.36) | 2.14 (1.05,4.39)* | 4.55 (2.33,9.93) | 3.49 (2.24,6.97)* | 3.52 (1.65,5.94) | 2.38 (1.18,4.79)* |
| Emergency | 1.44 (0.76,0.75) | 0.29 (0.10,0.87)* | 1.49 (0.79,2.79) | 1.19 (0.49,2.87) | 2.53 (1.31,3.86) | 1.08 (0.43,2.73) |
| Surgical | 0.38 (0.19,0.77) | 0.07 (0.02,0.21)* | 0.60 (0.33,1.08) | 0.43 (0.22,0.85)* | 0.77 (0.43,1.38) | 0.43 (0.21,1.89) |
| Medical | 0.95 (0.51,1.75) | 0.47 (0.21,1.06) | 1.42 (0.79,2.53) | 1.13 (0.60,2.13) | 1.39 (0.78,2.46) | 0.80 (0.41,1.54) |
| OPD | 2.08 (1.12,3.87) | 0.33 (0.11,0.97)* | 1.61 (0.87,2.96) | 1.19 (0.51,2.79) | 3.16 (1.66,4.02) | 1.48 (0.59,3.69) |
| Laboratory | 0.73 (0.34,0.53) | 0.27 (0.09,0.79)* | 2.08 (1.02,4.24) | 1.43 (0.65,3.16) | 1.99 (0.99,4.01) | 1.15 (0.49,2.69) |
| Pharmacy | 1 | 1 | 1 | 1 | 1 | 1 |
| Years of professional experience | ||||||
| <5 Year | 3.41 (2.26,5.19) | 2.45 (1.37,4.36)* | 1.33 (0.92,1.93) | 0.93 (0.59,1.46) | 1.16 (0.80,1.67) | 0.69 (0.42,1.12) |
| 5 −10 years | 2.56 (1.02,2.37) | 2.49 (1.40,4.41)* | 0.61 (0.43,0.87) | 0.54 (0.42,0.98)* | 0.91 (0.64,1.29) | 0.82 (0.26,2.12) |
| >10 years | 1 | 1 | 1 | 1 | 1 | 1 |
| Online training for COVID-19 | ||||||
| No | 0.75 (0.54,1.04) | 0.64 (0.36,3.69) | 1.57 (1.12,2.02) | 1.50 (1.74,3.79)* | 0.71 (0.53,0.96) | 0.53 (0.56,1.24) |
| Yes | 1 | 1 | 1 | 1 | 1 | 1 |
| PPE available | ||||||
| No | 0.60 (0.43,0.82) | 0.55 (0.34,0.90)* | 1.13 (0.83,1.52) | 0.60 (0.39,0.92) | 0.92 (0.68,1.25) | 0.69 (0.81,1.95) |
| Yes | 1 | 1 | 1 | 1 | 1 | |
Notes: 1=reference, and *statistically significant at p-value< 0.05 in bivariable and multivariable logistic regression.
Additionally, female participants were two times more likely to have depression than male participants [AOR=2.01; 95% CI, (1.25, 3.23)]. HCWs in the Oromiya Special Zone were four times more likely to have depression than HCWs working in central Oromiya [AOR=3.94; 95% CI, (1.94, 8.09)]. Medical laboratory professionals were 4.69 times more likely to have depression when compared with pharmacy professionals [AOR=4.69; 95% CI, (2.81, 9.17)]. HCWs working in the COVID-19 isolation treatment center were twice more likely to have depression than those in the pharmacy department [AOR=2.14; 95% CI, (1.05, 4.39)] (Table 2).
HCWs working in the Oromiya Special Zone were 1.85 times more likely to have anxiety than those working in central Oromiya [AOR=1.85; 95% CI, (1.14, 2.99)]. Female participants were twice more likely to have anxiety than male participants [AOR=1.91; 95% CI, (1.27, 2.86)]. Medical laboratory professionals were three times more likely to develop anxiety when compared to pharmacy professionals [AOR=2.75; 95% CI, (1.78, 4.79)]. HCWs working in the COVID-19 treatment isolation center were 3.49 times more likely to have anxiety than workers in the pharmacy department [AOR=3.49; 95% CI, (2.24, 6.97)] (Table 2).
Female participants [AOR=2.08; 95% CI, (1.33, 3.24)], HCWs working in the Oromiya Special Zone [AOR=2.14; 95% CI, (1.28, 3.59)], medical laboratory professionals [AOR=1.63; 95% CI, (1.27, 2.47)] and HCWs working in the COVID-19 isolation treatment center [AOR=2.38; 95% CI, (1.18, 4.79)] had higher odds of having stress compared to those working in the pharmacy department. Married participants were also significantly more likely to have depression, anxiety, and stress (Table 2).
Discussion
This cross-sectional study revealed a high prevalence of mental health symptoms among HCWs in central Ethiopia amid the COVID-19 pandemic. Of the total cohort of participants, 60.3%, 78%, and 33.8% self-reported symptoms of depression, anxiety, and stress, respectively. These rates were higher than those reported in a study conducted among HCWs in China, which demonstrated a prevalence of 50.7%, 44.7%, and 73.4% for depression, anxiety, and stress, respectively.7 Similarly, our findings were higher than those reported by a study in Iraq, which found a prevalence of 45%, 47%, and 18% for depression, anxiety, and stress, respectively.20 This difference may be due to the high fear of COVID-19 and/or due to the scarcity of PPE in central Ethiopia. Indeed, 71.1% of our respondents reported that there is a limited amount of PPE. In resourced countries, this is not as much of a concern as in low resourced counties.26
Most age categories have a risk of developing stress symptoms; nonetheless, participants aged 26 to 30 years had significantly higher rates of depression symptoms compared to those aged 18 to 25. This result was in line with the study done in China.26 Also, symptoms of anxiety, depression, and stress were reported among younger age HCWs in a systematic review results.27 With increasing age, individuals are more likely to worry about their families, which subsequently may impact their mental health status.28
Married HCWS also had a higher odds ratio of depression and stress, which similarly may be due to added anxiety of spreading the virus to other members of the household. This finding is similar with a narrative review among HCWs.16 Additionally, this study in line with the study results in Singapore,29 conversely, contradicts with findings in Beijing, China,30 and a rapid literature review27 revealed that being single is a risk of higher symptoms of depression, anxiety, and psychological distress.
In this study, our results demonstrated that symptoms of depression, anxiety, and stress were significantly higher among female participants compared to males. This is in line with the studies reported in Turkey,31 and China that also confirmed that females had a higher prevalence of mental health issues during the COVID-19 pandemic.32 A study from China found that women had three-fold higher anxiety, depression, and stress than men during the COVID-19 pandemic.33
In this study, we found that working in the Addis Ababa and Oromiya Special Zone was significantly associated with symptoms of depression, anxiety, and stress compared to Central Oromiya. This may be because the Addis Ababa and Oromiya Special Zone have a higher incidence of COVID-19 infections compared to other central Oromiya zones. Regarding professional attributes, compared to pharmacists, medical laboratory professionals were significantly associated with symptoms of depression, anxiety, and stress, whereas nurses were significantly associated with depression symptoms. This may be due to the fact that medical laboratory technologists/technicians and nurses have a higher exposure to blood and blood products, higher workload, and longer times in the wards, as well as more direct patient interaction than other HCWs. This finding was also reported in the studies done in China.34,35 This suggests that the working environment may influence the HCW’s mental health status.
The study results show that HCWs working in the COVID-19 treatment center were more significantly associated with the symptoms of depression, anxiety, and stress compared to HCWs in the pharmacy department. This is congruent with the results of the study conducted in China.8 Similarly, HCWs working in the emergency department, surgical department, outpatient department, and the laboratory department had significantly higher rates of self-reported symptoms of depression. This was also observed in studies conducted in China,26,35 and London, UK.6 These findings can be explained by the particularly high psychological burden of working in a high-risk exposure area.
In this study, HCWs who had less than ten years of working experience were significantly more likely to have symptoms of depression and anxiety compared to HCWs with longer work experience. A systematic review and meta-analysis identified HCWs who have less working experience had higher symptoms of depression, anxiety, and stress.27 This could be because HCWs with less experience might have a higher fear of contagion and hence, a higher level of depression, and anxiety during a disease outbreak.35 Additionally, the study participants who had not done the COVID-19 infection prevention and control training had higher anxiety. During a disease outbreak, it is vital that HCWs receive training and education on prevention and control mechanisms, personal protection methods, the severity of the disease, transmission methods, and the importance of timely psychological intervention for HCWs.35,36
In this study, we found that 71.1% of HCWs reported a shortage of PPE, a finding that was significantly associated with symptoms of depression. Ensuring staff protection against COVID-19 is essential to reduce disease transmission and minimize fear of the pandemic, which may in turn improve mental health outcomes.36 A systematic review and meta-analysis demonstrated that having PPE in the workplace, following preventive actions, and timely reporting of COVID-19 exposure are protective factors for mental health.34
Limitations of the Study
This study has a couple of limitations; first, it does not show a causal relationship due to its cross-sectional nature; and second, the study has been conducted at healthcare facilities located only in central Ethiopia, hence, our findings are not generalizable to the other regions of Ethiopia. Third, all healthcare workers working in clustered departments were invited to complete the online surveys, which may have a selection bias. Finally, this study is not ruled out the previous history of mental health problems.
Conclusion
In this study, HCWs in central Ethiopia reported a high prevalence of depression, anxiety, and stress symptoms. Female participants, HCWs in the Oromiya Special Zone, medical laboratory professionals, and HCWs working in COVID-19 treatment isolation centers were more likely to have depression, anxiety, and stress. Ensuring the mental well-being of HCWs should be a significant element of public health actions for controlling the COVID-19 pandemic. It is imperative that the Ethiopian Federal Ministry of Health should develop psychological interventions to address the specific needs of HCWs who have been impacted by the COVID-19 pandemic.
Acknowledgments
The authors acknowledge the Salale University, all health facilities from where the data were collected, and study participants for their cooperation.
Funding Statement
The authors declared that no grants were involved in supporting this work.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COVID-19, coronavirus disease 2019; DASS-21, Depression, Anxiety, and Stress Scale; HCWs, health care workers.
Data Sharing Statement
The datasets used and analyzed during the current study are available at
Figshare: Self-reported symptoms of depression, anxiety, and stress among healthcare workers in Ethiopia during the COVID-19 pandemic: https://doi.org/10.6084/m9.figshare.13378646.v1.22
Data are available under the terms of the Creative Commons Zero “No rights reserved” data waiver (CC0 1.0 Public domain dedication).
Ethics Approval and Informed Consent
This study was conducted in accordance with the Declaration of Helsinki. The study protocol and methodology were approved by Salale University Ethical Review Committee on June 15, 2020, with approval number SLUERC/046/2020. At the beginning of the questionnaire, the participants were informed about the study aims and how their data would be used, and that they would be consenting to take part by default if they completed the survey. The respondents were told that their inclusion in the study was voluntary, and they were free to withdraw from the study at any time. The respondents’ confidentiality was ensured by excluding their names from the questionnaire and by keeping their data in a password-locked computer.
Author Contributions
All authors made a significant contribution to the conception, study design, execution, and acquisition of data, analysis, and interpretation. All authors involved in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
- 1.Chinazzi M, Davis JT, Ajelli M, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. doi: 10.1126/science.aba9757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease (COVID-19) outbreak situation. Coronavirus Dis. COVID-19 Pandemic; 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed March29, 2020.
- 3.Pathan A, Thakur S Economic analysis of legislative process of parliament in the light of pandemic of covid-19 and india: revisiting existing physical infrastructure from the prism of evolving Information and Communication Technology (ICT). Available at SSRN 3587590; 2020.
- 4.Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mamun MA, Griffiths MD. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J Psychiatr. 2020;51:102073. doi: 10.1016/j.ajp.2020.102073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:368. doi: 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- 7.Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–e8. doi: 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976–e. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chew NW, Lee GK, Tan BY, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Que J, Le Shi JD, Liu J, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatry. 2020;33(3):e100259. doi: 10.1136/gpsych-2020-100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J Psychiatry. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e83. doi: 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balasubramanian S, Rao NM, Goenka A, Roderick M, Ramanan AV. Coronavirus disease 2019 (COVID-19) in children-What we know so far and what we do not. Indian Pediatr. 2020;57(5):435–442. doi: 10.1007/s13312-020-1819-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kowalski LP, Sanabria A, Ridge JA, et al. COVID‐19 pandemic: effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020;42(6):1259–1267. doi: 10.1002/hed.26164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ng QX, De Deyn MLZQ, Lim DY, Chan HW, Yeo WS. The wounded healer: a narrative review of the mental health effects of the COVID-19 pandemic on healthcare workers. Asian J Psychiatr. 2020;54:102258. doi: 10.1016/j.ajp.2020.102258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ochillo M, Elsie I. Mental health implications of COVID-19 in Kenya. Europasian J Med Sci. 2020;2(2):36–38. doi: 10.46405/ejms.v2i2.111 [DOI] [Google Scholar]
- 18.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e8. doi: 10.1016/S0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verma S, Mishra A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int J Social Psychiatry. 2020;66(8):756–762. doi: 10.1177/0020764020934508 [DOI] [PubMed] [Google Scholar]
- 20.Othman N. Depression, anxiety, and stress in the time of COVID-19 pandemic in Kurdistan region, Iraq. Kurdistan J Appl Res. 2020;37–44. [Google Scholar]
- 21.Ministry of Health-Ethiopian. Ethiopian Ministry of Health online COVID-19 training; 2020.Available from: http://www.moh.gov.et/covid19-courses/2020. Accessed April21, 2021.
- 22.Jemal K, Deriba BS, Geleta TA, et al. Self-reported symptoms of depression, anxiety, and stress among healthcare workers in Ethiopia during the COVID-19 pandemic. Figshare Software. 2020. doi: 10.6084/m9.figshare.13378646.v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (dass) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- 24.Coker A, Coker O, Sanni D. Psychometric properties of the 21-item depression anxiety stress scale (DASS-21). Afr Res Rev. 2018;12(2):135–142. doi: 10.4314/afrrev.v12i2.13 [DOI] [Google Scholar]
- 25.Sperandei S. Understanding logistic regression analysis. Biochem Med. 2014;24(1):12–18. doi: 10.11613/BM.2014.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vyas KJ, Delaney EM, Webb-Murphy JA, Johnston SL. Psychological impact of deploying in support of the US response to Ebola: a systematic review and meta-analysis of past outbreaks. Mil Med. 2016;181(11):e1515–e31. doi: 10.7205/MILMED-D-15-00473 [DOI] [PubMed] [Google Scholar]
- 28.Ennis E, Bunting BP. Family burden, family health, and personal mental health. BMC Public Health. 2013;13(1):1–9. doi: 10.1186/1471-2458-13-255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sim K, Chong PN, Chan YH, Soon WSW. Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. J Clin Psychiatry. 2004;65(8):1120–1127. doi: 10.4088/JCP.v65n0815 [DOI] [PubMed] [Google Scholar]
- 30.Liua X, Kakadeb M, Fullerb CJ, et al. Depression after exposure to stressful events: lessons learned from the SARS epidemic. Compr Psychiatry. 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Özdin S, Bayrak özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Social Psychiatry. 2020;66(5):504–511. doi: 10.1177/0020764020927051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2021;26(1):13–22. doi: 10.1080/13548506.2020.1746817 [DOI] [PubMed] [Google Scholar]
- 34.Luo M, Guo L, Yu M, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. doi: 10.1016/j.psychres.2020.113190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. World Health Organization; 2020.