Abstract
Pseudarthrosis is a feared complication of spinal fusion procedures. Currently, the gold standard in prevention or treatment of pseudarthrosis is placement of nonvascularized iliac crest bone autograft. While rates of fusion are significantly higher in patients with use of nonvascularized bone autografts than with allografts, patients who have previously failed lumbar arthrodesis or those at a high risk for pseudarthrosis may benefit from a more robust, vascularized bone graft with enhanced osteogenicity. In this article, we discuss the use of iliac crest vascularized bone grafts as an adjunct for high-risk patients undergoing lumbosacral spine arthrodesis.
Keywords: vascularized bone graft, spinoplastic reconstruction, iliac crest, autograft, spinal fusion, pseudoarthrosis
Background
Lumbar arthrodesis is a commonly performed method to treat tumors, trauma, deformity, and degenerative diseases of the lumbar spine. Pseudarthrosis, or failed bony fusion, is a feared and well-studied complication of spinal fusion procedures, with reported rates of up to 35% in single-level lumbar arthrodeses and a higher incidence in multilevel fusions. 1 2 3 4 These patients often present with a recurrence of pain and/or neurological symptoms or a loss of anatomic alignment on examination after primary lumbar arthrodesis. 1
Currently, prevention/treatment of pseudarthrosis during repeat fusion operation involves augmentation with various orthobiologic materials. The ideal biologic material has osteoconductive, osteoinductive, and osteogenic properties that enhance bony fusion. 1 Osteoconductive materials, such as allograft, passively allow bony ingrowth and migration of osteogenic cells along their surface. 5 6 Osteoinductive materials, such as bone morphogenic protein (BMP) and demineralized bone matrix (DBM), induce differentiation of osteoprogenitor cells to allow osteogenesis. 3 5 7 8 9 Materials with osteogenic properties, such as autologous bone grafts, bring osteoprogenitor cells to the tissue bed to enhance bone growth. 5 6
The current gold standard in pseudarthrosis management is nonvascularized iliac crest autograft. Use of nonvascularized bone graft (N-VBG) is associated with significantly higher fusion rates that with allograft alone (79 vs. 52%). 1 10 11 While most patients have successful fusion with N-VBG alone, patients with significant risk factors for pseudarthrosis, including severe deformity, multisegment involvement, prior radiation, active infection, malnutrition, smoking, or poor bone quality secondary to metabolic (e.g., osteoporosis), neoplastic, or social risk factors may benefit from a more robust autograft material with enhanced osteogenic potential. 6
Vascularized bone grafts (VBGs) are superior autografts that allow delivery of stem cells and antibiotics to the fusion bed via a microvascularly transferred or pedicled vascular supply. They also maintain osteocyte viability, allowing primary bone healing rather than healing by creeping substitution, and display more rapid incorporation, more robust fusion, and increased resistance to infection compared with N-VBGs. 6 10 12
Free-transfer vascularized bone flaps (e.g., free fibular and free rib flaps) have not gained popularity as they are associated with a significantly increased operative time, increased blood loss, significant donor site morbidity, increased blood loss, technically challenging microvascular anastomosis, and difficulty in finding donor vessels. 12 13 Pedicled VBGs provide the benefits of free-transfer bone flaps but effectively bypass the aforementioned difficulties, allowing harvest of vascularized bone from a local donor site without disruption of the graft's vascular pedicle with minimally increased operative time. 4 In this review, we discuss the use of pedicled iliac crest vascularized bone grafts (IC-VBGs) in posterior spinal fusion procedures for prevention or treatment of pseudarthrosis.
Indications
Use of an IC-VBG is not a first-line option for all patients undergoing spinal fusion procedures and should only be considered in patients with complex spinal pathologies who have failed/are likely to fail standard reconstruction. 4 14 Those who benefit most are patients with a history of bone disorders (e.g., osteoporosis) or previous pseudarthrosis, those requiring revision surgery, and those at a high risk of nonunion due to a previously irradiated surgical field or actively infected wound. 15
The pedicled posterior IC-VBG is capable of reaching spinal levels L1 (range T12–L1) through S1 (range S1–S3) and is able to cover up to 3 vertebral levels. 12 Therefore, patients undergoing posterior unilateral spinal fusion procedures with defects in the lower thoracic, lumbar, or upper sacral vertebrae are potential candidates. IC-VBGs also have the potential to reach contralaterally to the mid and upper lumbar vertebrae, allowing bilateral graft support from a unilateral donor site. Patients undergoing posterior bilateral lumbosacral spinal fusion are considered potential candidates; however, the size of the graft taken for any fusion requiring bilateral support must be balanced with potential defect in the pelvis and loss of quadrates lumborum (QL) support. In a patient requiring bilateral graft support, Bohl et al recommend bilateral IC-VBGs as the operation is technically easier than a unilateral approach and decreases donor-site morbidity. 12
Anatomy and Surgical Technique
IC-VBGs have been described based on a variety of nutrient pedicles, including the deep circumflex scapular artery, tensor fascia lata (TFL) muscle, internal oblique muscle, external oblique muscle, and QL muscle. 15 In this article, we describe the relevant anatomy and operative technique for harvest of a segment of the posterior iliac crest, pedicled on its periosteal attachments to the QL muscle, as a VBG for patients undergoing posterior lumbosacral spinal fusion.
Relevant Anatomy
The iliac crest is the superior border of the wing of the ilium and the superolateral margin of the greater pelvis. It receives its dominant blood supply from the inferiorly based deep circumflex iliac vessels, which are often utilized in free iliac crest bone flaps, and its secondary blood supply from segmental lumbar vessels and various periosteal muscular attachments. 16 Muscular attachments include those of the gluteus medius and TFL (anterior lateral surface), gluteus maximus (posterior lateral surface), iliacus (medial surface), internal and external oblique (anterior superior border), and QL (posterior superior border) muscles. 17
The QL is a robust muscle of the posterior abdominal wall, lying just dorsal to the paraspinous muscles, that extends from the inner lip of the iliac crest and the iliolumbar ligament to the internal surface of the 12th rib and transverse processes of the lumbar vertebrae. 18 It is supplied by the lumbar arteries and the lumbar branch of the iliolumbar artery. Positioned posteriorly and superiorly to the iliac crest, the QL is an optimal pedicle for augmentation of posterior lower thoracic, lumbar, and sacral spinal fusions.
IC-VBGs based on the anteriorly attaching internal and external oblique muscles or inferiorly based deep circumflex artery and TFL muscle do not provide a sufficient reach or arc of rotation to augment a posterior spinal fusion. 15
Operative Technique
Supplementary Video 1 Animation of posterior iliac crest vascularized bone graft being rotated on its quadrates lumborum muscle pedicle, tunneled under the paraspinous muscles, and rotated into a spine defect.
A pedicled, vascularized iliac crest bone graft based on the QL muscle may be harvested from the same standard midline incision used in spinal fusion procedures. 4 10 Alternatively, the iliac crest may be exposed through a separate horizontal incision overlying the iliac wing; however, this places patients at higher risk of superior cluneal nerve injury and subsequent postoperative donor site pain. 12 14 After identification of the superior-dorsal aspect of the iliac crest by palpation, dissection begins lateral to the paraspinal muscles and is carried down to the iliac crest. The surgeon should be cognizant of the retroperitoneal structures, including the iliac vessels and ureters, lying just dorsal to the iliac wing and QL. 4 Blunt dissection minimizes the risk of retroperitoneal injury. Care is taken to preserve the iliac crest's QL attachments to ensure adequate vascularity of the VBG. 12
After adequate exposure of the bone and release of the laterally situated superior gluteal attachments, the spinal defect should be measured, and markings transposed on the posterior aspect of the iliac crest. 4 After marking, a 6- to 10-cm segment of cortical-cancellous bone may be harvested using an osteotome or reciprocating bone scalpel. Three bicortical osteotomies are made medially, laterally, and inferiorly, with caution not to dive with the blade after the second cortex is violated. 4 Following VBG harvest, additional cancellous bone is readily available should additional grafting be required to increase stability of the construct. 4 10
The bone segment is grasped with a clamp and dissected free from the iliacus, gluteus maximus, and paraspinous muscles. During elevation of the pedicled graft to approximately the 12th rib, care should be taken to leave a posterior layer of fascia in place to prevent a postoperative lumbar hernia. 12 Steady oozing of blood should be seen from the exposed medullary bone on the vascularized graft, indicating adequately maintained vascularization. 12
The VBG may then be tunneled under the lumbar paraspinal muscles ( Fig. 1 ) and rotated into the defect ( Supplementary Video 1 ; online only). The graft should lay posterolateral to the spine, without tension on the pedicle or the bone segment. The graft is then secured in place with titanium cables or miniplates and screws, and additional iliac crest N-VBG may be packed adjacent to the VBG and hardware, if indicated. After graft fixation, the wound is closed in multiple layers, with drains left both deep and superficial to the paraspinous muscles to prevent postoperative seroma formation.
Fig. 1.
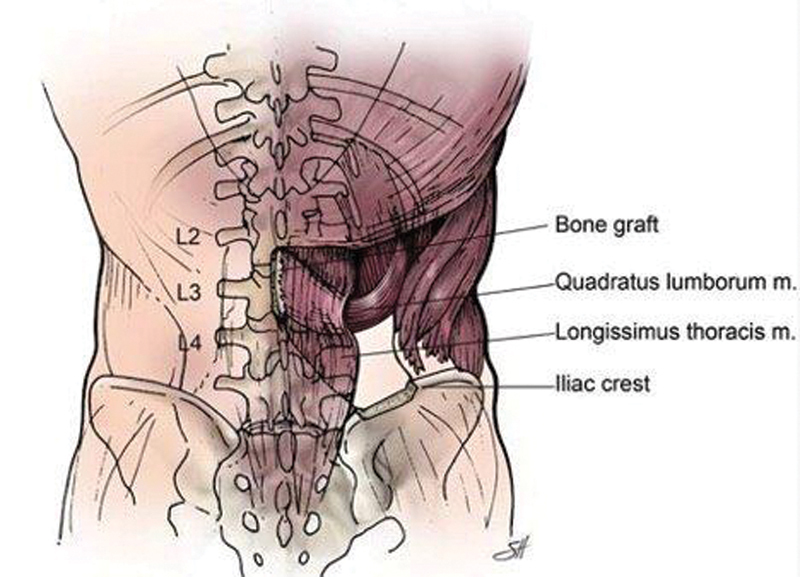
Illustration of a pedicled iliac crest vascularized bone graft after elevation and inset. A segment of the iliac crest has been elevated on a quadrates lumborum muscle pedicle, tunneled under the paraspinous muscles, and rotated into a defect in the lumbar spine.
Clinical Outcomes
Vascularized bone transfers have been shown to maintain radiologic density 1.5 to 2 times better than N-VBGs. They rapidly incorporate, demonstrating callus formation within 1 week; maintain long-term stability under compressive and rotary forces; and have the ability to treat active infections in situ. 4 10 While the use of pedicled IC-VBGs is a novel tool in facilitation of lumbar spinal fusion in high-risk patients, and there is limited data on long-term outcomes, this technique has shown promise in small cohorts.
Of 14 patients who underwent lumbar spinal fusion procedures augmented by pedicled vascularized iliac bone flap, Reece et al reported no spigelian hernias or significant donor-site pain, likely due to the submuscular plane of dissection. 14 Recent case reports by Bohl et al and Reece et al demonstrate successful incorporation of IC-VBGs into high-risk fusion beds. These included patients with an extensive lumbar osteomyelitis and discitis, and a history of three previously failed spinal fusions, with postoperative imaging at 3 months and 1 year showing continued IC-VBG hyperdensity and successful graft incorporation, respectively. 4 12
Alternatives
Alternatives to the pedicled IC-VBGs as a tool in prevention or treatment of lumbar pseudarthrosis include N-VBGs and free-transfer bone flaps, as previously discussed, as well as pedicled posterior element VBGs (PE-VBGs) and the addition of bone morphogenic proteins (BMPs) or demineralized bone matrix (DBM) to the fusion site.
The lumbar PE-VBG is based on a lumbar paraspinal pedicle and provides the same osteoconductive, osteoinductive, and osteogenic properties as the IC-VBG. One major limitation of this VBG is that it cannot be mobilized to the contralateral intertransverse process space due its segmental vascular pedicle and is, therefore, only useful in unilateral fusion augmentation. In addition, previous lumbar decompression or fusion procedures effectively remove the posterior elements and/or disrupt their blood supply, making this graft a nonviable option for patients undergoing revision surgery. 12
BMPs are naturally occurring, osteoinductive proteins that stimulate bone healing by inducing differentiation of primitive mesenchymal cells into osteoblasts. Use of these proteins in spinal fusion procedures has been associated with a reduction in reoperation rates and an increase in solid fusion rates (up to 94%) when compared with iliac crest N-VBGs 1 ; however, BMPs have demonstrated nonsignificant differences in patients satisfaction and postoperative work status. 8 DBM is an allograft material composed of collagens, BMPs, and other growth factors, allowing much greater osteoinductive properties that other allografts. Use of DBM has resulted in reported fusion rates comparable to those reported with use of autogenous iliac crest N-VBG (80–89%). 1 3 While use of DBM may avoid the donor-site morbidity, postoperative pain, or increased operative time associated with N-VBGs, they have variable lot-to-lot osteoinductive properties due to variability in concentration of BMPs. Both BMPs and DBM are incapable of providing antibiotics to the wound bed. The surgeon should also take into account the significant financial expense of these two products in comparison to autologous bone graft prior to utilizing these methods as an augment in spinal fusion procedures.
Conclusion
Patients at high risk of nonunion after lumbar spine arthrodesis include those with active infection, severe deformity, multilevel involvement, prior radiation, and various social or medical risk factors. These patients, particularly those who have previously failed standard spinal fusion procedures, may benefit from the use of IC-VBGs. The IC-VBG may be easily accessed from the same incision utilized in standard spinal fusion procedures; requires minimal additional operative time; and, in the small number of postoperative studies available to date, demonstrates a high rate of successful graft incorporation, making it an effective and relatively uncomplicated salvage strategy for patients with complex spinal pathology.
Footnotes
Conflict of Interest Dr. Ropper receives consulting fees from Globus Medical and Stryker, but they have no conflict with this report.
References
- 1.Chun D S, Baker K C, Hsu W K. Lumbar pseudarthrosis: a review of current diagnosis and treatment. Neurosurg Focus. 2015;39(04):E10. doi: 10.3171/2015.7.FOCUS15292. [DOI] [PubMed] [Google Scholar]
- 2.Hibbs R A. An operation for progressive spinal deformities: a preliminary report of three cases from the service of the orthopaedic hospital. 1911. Clin Orthop Relat Res. 2007;460(460):17–20. doi: 10.1097/BLO.0b013e3180686b30. [DOI] [PubMed] [Google Scholar]
- 3.Fu T S, Wang I C, Lu M L, Hsieh M K, Chen L H, Chen W J. The fusion rate of demineralized bone matrix compared with autogenous iliac bone graft for long multi-segment posterolateral spinal fusion. BMC Musculoskelet Disord. 2016;17:3. doi: 10.1186/s12891-015-0861-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reece E M, Raghuram A C, Bartlett E L. Vascularized iliac bone graft for complex closure during spinal deformity surgery. Plast Reconstr Surg Glob Open. 2019;7(07):e2345. doi: 10.1097/GOX.0000000000002345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Genitiempo M. 2nd ed. New Delhi, India: Woodhead Publishing; 2019. Biomaterial in spinal surgery; pp. 341–359. [Google Scholar]
- 6.Roberts T T, Rosenbaum A J. Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012;8(04):114–124. doi: 10.4161/org.23306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burkus J K, Gornet M F, Dickman C A, Zdeblick T A. Anterior lumbar interbody fusion using rhBMP-2 with tapered interbody cages. J Spinal Disord Tech. 2002;15(05):337–349. doi: 10.1097/00024720-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H, Wang F, Ding L. A meta analysis of lumbar spinal fusion surgery using bone morphogenetic proteins and autologous iliac crest bone graft. PLoS One. 2014;9(06):e97049. doi: 10.1371/journal.pone.0097049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vaccaro A R, Lawrence J P, Patel T. The safety and efficacy of OP-1 (rhBMP-7) as a replacement for iliac crest autograft in posterolateral lumbar arthrodesis: a long-term (>4 years) pivotal study. Spine. 2008;33(26):2850–2862. doi: 10.1097/BRS.0b013e31818a314d. [DOI] [PubMed] [Google Scholar]
- 10.Yelizarov V G, Minachenko V K, Gerasimov O R, Pshenisnov K P. Vascularized bone flaps for thoracolumbar spinal fusion. Ann Plast Surg. 1993;31(06):532–538. doi: 10.1097/00000637-199312000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Tuchman A, Brodke D S, Youssef J A. Iliac crest bone graft versus local autograft or allograft for lumbar spinal fusion: a systematic review. Global Spine J. 2016;6(06):592–606. doi: 10.1055/s-0035-1570749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bohl M A, Mooney M A, Catapano J S. Pedicled vascularized bone grafts for posterior lumbosacral fusion: a cadaveric feasibility study and case report. Spine Deform. 2018;6(05):498–506. doi: 10.1016/j.jspd.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Cervenansky J, Skrovina B, Maar D. Use of fibular bone grafts in reconstructive surgery [in Polish] Pol Orthop Traumatol. 1962;27:297–307. [PubMed] [Google Scholar]
- 14.Reece E M, Davis M J, Wagner R D.Vascularized Bone Grafts for Spinal Fusion-Part 1: The Iliac CrestOper Neurosurg 2021 (e pub ahead of print).Doi;10.1093/ons/opab037 [DOI] [PubMed]
- 15.Hayashi A, Maruyama Y, Okajima Y, Motegi M. Vascularized iliac bone graft based on a pedicle of upper lumbar vessels for anterior fusion of the thoraco-lumbar spine. Br J Plast Surg. 1994;47(06):425–430. doi: 10.1016/0007-1226(94)90072-8. [DOI] [PubMed] [Google Scholar]
- 16.Ghassemi A, Furkert R, Prescher A. Variants of the supplying vessels of the vascularized iliac bone graft and their relationship to important surgical landmarks. Clin Anat. 2013;26(04):509–521. doi: 10.1002/ca.22199. [DOI] [PubMed] [Google Scholar]
- 17.Beahm E, Hanasono M, Shenaq S. Edinburgh: Saunders; 2009. Iliac flap; pp. 339–357. [Google Scholar]
- 18.Bordoni B, Varacallo M. Treasure Island, FL: StatPearls Publishing; 2018. Anatomy, Abdomen and Pelvis, Quadratus Lumborum. [PubMed] [Google Scholar]


