Abstract
Instrumented fixation and fusion of the thoracic spine present distinct challenges and complications including pseudarthrosis and junctional kyphosis. When complications arise, morbidity to the patient can be significant, involving neurologic injury, failure of instrumentation constructs, as well as iatrogenic spinal deformity. Causes of fusion failure are multifactorial, and incompletely understood. Most likely, a diverse set of biomechanical and biologic factors are at the heart of failures. Revision surgery for thoracic fusion failures is complex and often requires revision or extension of instrumentation, and frequently necessitates complex soft tissue manipulation to manage index level injury or to augment the changes of fusion.
Keywords: thoracic spinal fusion, pedicle screw fixation, proximal junctional kyphosis, proximal junctional failure, pseudarthrosis
The thoracic spine is comprised of the 12 rib bearing vertebrae between the cervical and lumbar spine. Biomechanically, the thoracic spine can be further subdivided into semirigid and mobile segments, the former spanning T1 to 7, and the latter spanning T8 to 12 based on biomechanical stability provided by the adjacent attached structures. The rigid upper thoracic spine owes ∼78% of its rigidity to the presence of the ribs and their associated connections to the sternum, which act as an additional scaffold, limiting the segmental range of motion. 1 In contrast, the ribs associated with the T8 to 12 vertebrae are not rigidly bound to the sternum and thus confer greater flexibility and segmental movement to the lower thoracic spine comparably. Taken as a whole, the thoracic spine in general has a higher degree of stiffness and lower range of motion when compared with the cervical and lumbar spine. 2 Nevertheless, despite the inherent increased stability of the thoracic spine, critical mechanical disruptions requiring arthrodesis and instrumentation are often indicated in cases of trauma, deformity, infection, malignancy, and other pathologies ( Fig. 1A–B ). In most contemporary practices, surgical intervention involves segmental fixation with pedicle screw and rod constructs concurrent with boney arthrodesis and fusion ( Fig. 1C ). 3
Fig. 1.
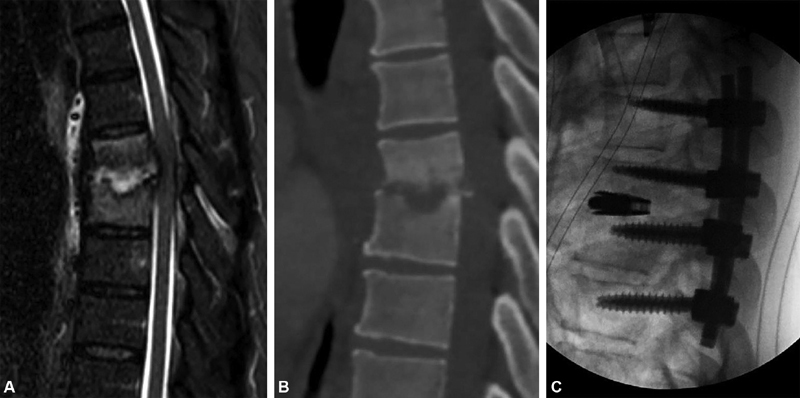
Thoracic fusion for osteomyelitis discitis. ( A ) Sagittal T2-weighted magnetic resonance imaging of a 53-year-old man presenting with back pain shows a midthoracic osteomyelitis/discitis complex causing spinal cord compression and a focal kyphotic deformity. ( B ) A sagittal computed tomography image reveals significant bony destruction and the kyphotic deformity. ( C ) Postoperative lateral radiograph after segmental fixation with pedicle screws and interbody cage with reduction in kyphosis. Posterolateral arthrodesis across the vertebral joints and in the disc space will proceed with immediate stability provided by the spinal hardware.
The biomechanical properties and unique anatomic aspects of the thoracic spine are implicated in many postsurgical complications including pseudarthrosis, junctional kyphosis, and junctional failure. Pseudoarthrosis is the broadest term used to describe a failure of spinal fusion and describes a failure of boney arthrodesis to occur across a spinal segment. The goal of spinal arthrodesis is to permanently immobilize and align pathologically mobile or unstable segments of the vertebral column. According to a large meta-analysis by Hofler et al, the incidence of pseudarthrosis in thoracic fusion is ∼1.8%. 4 Factors contributing to pseudarthrosis are multiple and include both biologic and biomechanical factors. Patient risk factors include smoking, long-term steroid use, and osteoporosis, as well as malignancy and infection, which may be local or systemic. 4 In contrast, surgical risk factors to pseudarthrosis include bone graft materials, increasing length of fixation construct, the quality of fixation achieved, and the use of high-dose intravenous nonsteroidal anti-inflammatory drugs such as ketorolac following surgical fixation or fusion. 5
In select patients, nonoperative management of pseudoarthrosis is reasonable if the associated pain symptoms are not overburdensome. A recent series of patients with pseudarthrosis following pedicle subtraction osteotomies in the lumbar spine, a highly destabilizing operative technique, found that patients managed nonoperatively did well at long-term follow-up, as long as focal instability did not alter the patient's global alignment and an appropriate sagittal vertical axis (SVA) was maintained. 6 Additionally, revision surgery for pseudoarthrosis carries significant intrinsic risk, and is reported to have a failure rate of 40 to 70%. 7 Nevertheless, in the correct clinical scenario, where the patient experiences increasing pain or decline in neurologic or functional status, revision surgery may be appropriate. Such revisions generally involve reattempting fusion either by the same or different surgical approach and utilizing biologic augmentation such as different autograft bone products or bone morphogenic protein. Specific risk factors for failure of revision arthrodesis are generally congruent with those of the index surgery. 7
Junctional kyphosis refers to a deformity of at least 10 degrees of kyphosis that occurs either proximal (cranial) or distal (caudal) to an instrumented spinal construct. It is a relatively common complication, occurring in more than 30% of long construct thoracic fusions. 8 In the thoracic spine, it is relatively common since long constructs typically end at T2 to 4 for cervicothoracic fusions and T9 to 11 for thoracolumbar fusions due to the large pedicle sizes at those vertebra, and their relative neutral biomechanical alignment. Risk factors can be divided into surgical factors, patient factors, and radiographic factors. Surgical factors include disruption of the spinal posterior column tension band, use of combined anterior–posterior approaches, and extension of the fusion construct to the sacrum or pelvis. 9 Additionally, a greater degree of deformity correction has also been suggested to contribute to proximal junctional kyphosis (PJK), perhaps because of compensatory biomechanical forces resulting from this correction ( Fig. 2A–B ). 10 Patient risk factors for junctional kyphosis include poor bone quality (osteopenia or osteoporosis, malignancy, infection) and neuromuscular disorders. 11 Radiographic factors that may contribute to junctional kyphosis include a greater degree of preoperative junctional kyphosis as well as a high degree of sagittal malalignment as measured by SVA.
Fig. 2.

Proximal junctional kyphosis. ( A ) Lateral radiographs showing a 60-year-old woman with degenerative scoliosis and sagittal lumbar hypolordosis undergo correction by distal thoracolumbar instrumented fixation and fusion. ( B ) The construct was focally overcorrected at the proximal junctional level resulting in significant proximal junctional kyphosis.
Junctional failure does not have a clearly accepted definition, but generally refers to severe junctional kyphosis that results in biomechanical instability or neurologic sequalae ( Fig. 3A–B ). Some frequently used definitions include cases that satisfy one of the following features: fracture of the most proximal or distal instrumented level or the level above, disruption of the posterior osteoligamentous complex, or pullout of the screws at the most cranial instrumented level. 9 12 Patients with junctional failure frequently have a very prominent focal kyphosis, which significantly may result in protrusion of instrumentation or erosion of adjacent bone through the skin ( Fig. 4A–B ).
Fig. 3.
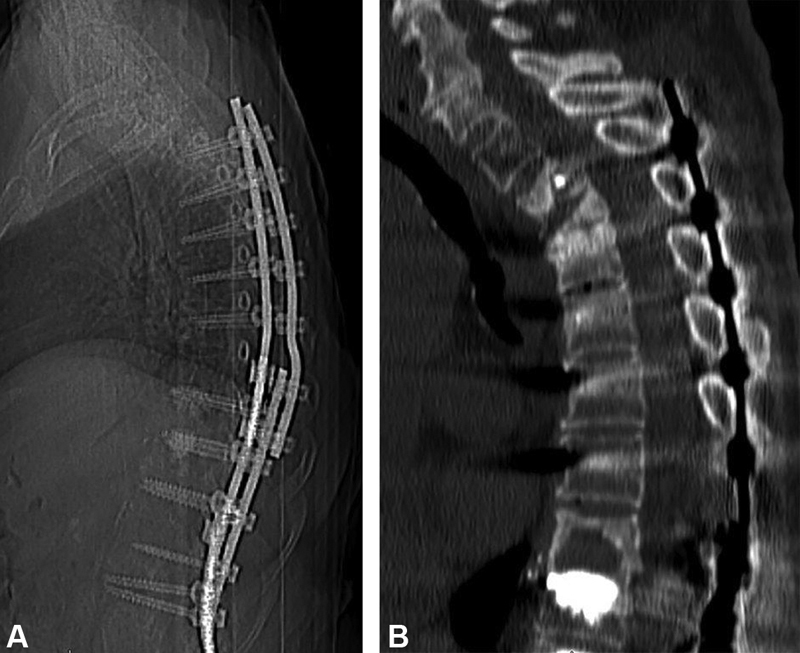
Proximal junctional failure with neurologic injury. ( A ) Lateral radiograph and ( B ) sagittal computed tomographic image of a 73-year-old woman who previously underwent a T3 to pelvis spinal fusion for deformity correction presented several months later with subacute paraplegia due to proximal junctional failure. Sequential compression fractures occurred at T2 and T3 causing focal kyphosis and subacute spinal cord compression.
Fig. 4.
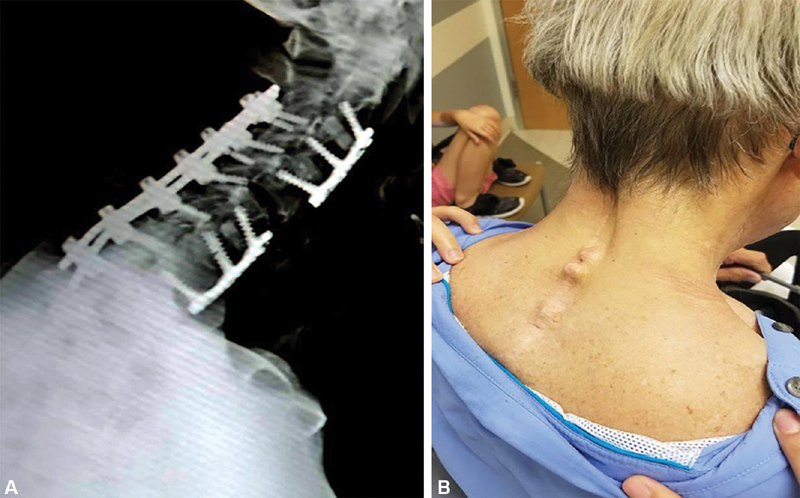
Distal junctional kyphosis and wound healing issues. ( A ) Lateral radiograph of a 65-year-old man with a previous C2 to C7 posterior cervical fusion showing distal junctional kyphosis at the cervicothoracic junction. ( B ) Pictures of the patient show dehiscence of the underlying fascia and muscle planes by the patient's hardware and spinous processes.
Meaningful prevention strategies for PJK and failure (PJF) are not well established, and preventative strategies are poorly examined in the literature. 9 In general, the discussion of preoperative patient-specific risk factors should be optimized, especially in the case of osteoporosis, as poor bone quality may contribute strongly to the risk of fractures and screw pullout at the upper instrumented level. Other strategies include extending the fusion construct to neutral levels or with less than 5 degrees of segmental kyphosis, greater preservation of the posterior soft tissues such as the paraspinal muscles and fascia at the junctional during dissection, and avoidance of over correction of global sagittal alignment. In one series, correction of sagittal alignment was the only predictive factor of recurrent PJK. 13 Additional surgical procedures such as ligament augmentation, which involves the wire or Mersiline tape stabilization of the posterior elements at upper vertebral levels, have also been described. 14 15
When PJK and PJF occur, patients frequently undergo revision surgery, with some series reporting up to 57% of patients with PJK or PJF undergoing revision. 12 Additionally, revision of PJK is the most common indication for fixation spanning the cervical spine through the pelvis. 16 Goals of surgery for correction of junctional failure include further correction of deformity and spinal instability, as well as decompression of neural elements and restoration of physiologic alignment that may limit the ability to perform activities of daily living. This is generally accomplished by correcting the secondary proximal deformity and extending the fusion construct to include higher vertebral levels. 13
In addition to new spinal deformity, patients with PJK may have wound complications that require complex closures or reconstructions with plastic surgery. Vascularized muscle flaps using trapezius, latissimus, gluteal, or other muscle flaps are frequently used during reconstruction due to their ability to provide increased vascularity to the surgery site and eliminate dead space. 17 Furthermore, muscle flaps may also be utilized to construct wounds complicated by wound erosion at the junctional level as well as in the setting of cerebrospinal fluid leak making them versatile options for closure.
In summary, despite the inherently greater stability of the thoracic spine in comparison to other components of the axial skeleton, fusion failures can occur due to a variety of biological and biomechanical. Fusion constructs of the thoracic spine also involve a set of particular complications including pseudarthrosis and proximal distal kyphosis and failure. Each of these complications has certain management strategies that may involve both spinal revision/reconstruction and plastic surgery assistance with soft tissue or bony reconstruction.
Case Illustration
A 74-year-old man presents to clinic with several months of worsening chin on chest deformity. He had a history of lung cancer, oral cancer, both in remission after lengthy treatments with chemotherapy and radiation. At the time of presentation, he had been abstinent from smoking for the past year, as well as abstinent from all nicotine products for the past 6 months.
The patient initially underwent a three-stage procedure for deformity correction. Stage 1 involved posterior osteotomies from C3 to 6, followed by Stage 2 C3 to 6 anterior cervical discectomy and fusion with placement of a cervical plate anteriorly. Stage 3 entailed posterior spinal instrumented fusion from C2 to T3 ( Fig. 5A–B ).
Fig. 5.

Case illustration index surgery. ( A ) Lateral standing radiographs show a 74-year-old man with chin on chest deformity. ( B ) Postoperative lateral radiographs showing excellent correction.
Although the patient achieved excellent radiographic correction of his initial deformity, the patient presented to the emergency room 5 weeks postoperatively with upper extremity weakness and worsening dysphagia resulting in weight loss of ∼20 pounds. Radiographs revealed distal junctional failure at T3 with a 90 degrees focal kyphotic deformity with the distal ends of the instrumentation eroding through the skin ( Fig. 6A–B ). The patient underwent percutaneous gastrostomy placement for nutritional supplementation and was placed on a high-calorie diet for 2 weeks. Following supplementation, the patient underwent T3 corpectomy for anterior column reconstruction, as well as extension of the posterior fusion construct to L2 with bilateral trapezius and latissimus muscle flaps ( Fig. 6C–D ). He was transferred to an acute rehabilitation center for postsurgical physical therapy.
Fig. 6.

Case illustration first revision. ( A ) Lateral radiograph showing distal junctional failure at the upper thoracic spin with a T3 compression fracture causing 90 degrees of focal kyphosis. The instrumentation on the radiograph can be seen protruding through the patient's soft tissue. Pictures ( B ) before and ( C ) after surgical correction showing the reduction in kyphotic deformity and excellent closure with trapezius and latissimus dorsi muscle flaps. ( D ) Lateral radiographs after surgery showing good correction at the upper thoracic spine.
Unfortunately, the patient was transferred back to the emergency room for wound breakdown about 4 weeks ago following revision surgery. On presentation, the patient was noted to have lost over 40 pounds since the time of previous discharge and on radiographs exhibited repeat distal junctional kyphosis with pullout of his hardware that was now eroding through the skin again, this time in the lumbar spine ( Fig. 7A ). The patient's lumbar wound was noted to be open, requiring multiple stage debridement and bilateral paraspinal muscle flaps for definitive closure following extension of the fusion to the pelvis ( Fig. 7B ). The patient was again transferred to an acute rehab facility where he recovered enough to be discharged home. At his most recent clinical follow-up 18 months after his last revision, he remained clinically and radiographically stable.
Fig. 7.

Case illustration of second revision. Lateral radiographs showing ( A ) recurrent distal junctional failure with multiple distal thoracic compression fractures and pullout of the patient's pedicle screws at T10 as well a focal kyphotic deformity. ( B ) Surgical correction with extension to the pelvis and paraspinal muscle flaps enabled safe coverage of the extended hardware.
Footnotes
Conflicts of Interest Dr. Ropper receives consulting fees from Globus Medical and Stryker, but have no conflict with this article.
References
- 1.Brasiliense L B, Lazaro B C, Reyes P M, Dogan S, Theodore N, Crawford N R. Biomechanical contribution of the rib cage to thoracic stability. Spine. 2011;36(26):E1686–E1693. doi: 10.1097/BRS.0b013e318219ce84. [DOI] [PubMed] [Google Scholar]
- 2.Bergmark A. Stability of the lumbar spine. A study in mechanical engineering. Acta Orthop Scand Suppl. 1989;230:1–54. doi: 10.3109/17453678909154177. [DOI] [PubMed] [Google Scholar]
- 3.Zindrick M R, Wiltse L L, Widell E H. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;(203):99–112. [PubMed] [Google Scholar]
- 4.Hofler R C, Swong K, Martin B, Wemhoff M, Jones G A. Risk of pseudoarthrosis after spinal fusion: analysis from the healthcare cost and utilization project. World Neurosurg. 2018;120:e194–e202. doi: 10.1016/j.wneu.2018.08.026. [DOI] [PubMed] [Google Scholar]
- 5.Li J, Ajiboye R M, Orden M H, Sharma A, Drysch A, Pourtaheri S. The effect of ketorolac on thoracolumbar posterolateral fusion: a systematic review and meta-analysis. Clin Spine Surg. 2018;31(02):65–72. doi: 10.1097/BSD.0000000000000613. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y C, Kim K T, Kim C K. Outcomes of non-operative management for pseudarthrosis after pedicle subtraction osteotomies at minimum 5 years follow-up. J Korean Neurosurg Soc. 2019;62(05):567–576. doi: 10.3340/jkns.2018.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee Y, Farhan S, Musa A, Bhatia N. Pseudarthrosis in spine surgery: diagnosis and treatment. Contemp Spine Surg. 2019;20(08):1–8. [Google Scholar]
- 8.Liu F Y, Wang T, Yang S D, Wang H, Yang D L, Ding W Y. Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J. 2016;25(08):2376–2383. doi: 10.1007/s00586-016-4534-0. [DOI] [PubMed] [Google Scholar]
- 9.Kim H J, Iyer S. Proximal junctional kyphosis. J Am Acad Orthop Surg. 2016;24(05):318–326. doi: 10.5435/JAAOS-D-14-00393. [DOI] [PubMed] [Google Scholar]
- 10.International Spine Study Group(ISSG) . Kim H J, York P J, Elysee J C. Cervical, thoracic, and spinopelvic compensation after proximal junctional kyphosis (PJK): does location of PJK matter? Global Spine J. 2020;10(01):6–12. doi: 10.1177/2192568219879085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glassman S D, Coseo M P, Carreon L Y. Sagittal balance is more than just alignment: why PJK remains an unresolved problem. Scoliosis Spinal Disord. 2016;11:1. doi: 10.1186/s13013-016-0064-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Spine Study Group . Hart R, McCarthy I, Oʼbrien M. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine. 2013;38(19):E1223–E1227. doi: 10.1097/BRS.0b013e31829fedde. [DOI] [PubMed] [Google Scholar]
- 13.International Spine Study Group . Kim H J, Wang S J, Lafage R. Recurrent proximal junctional kyphosis: incidence, risk factors, revision rates, and outcomes at 2-year minimum follow-up. Spine. 2020;45(01):E18–E24. doi: 10.1097/BRS.0000000000003202. [DOI] [PubMed] [Google Scholar]
- 14.Safaee M M, Deviren V, Dalle Ore C. Ligament augmentation for prevention of proximal junctional kyphosis and proximal junctional failure in adult spinal deformity. J Neurosurg Spine. 2018;28(05):512–519. doi: 10.3171/2017.9.SPINE1710. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez-Fontan F, Reeves B J, Noshchenko A.Strap stabilization for proximal junctional kyphosis prevention in instrumented posterior spinal fusionEur Spine J2020 [DOI] [PubMed]
- 16.Iyer S, Kim H J, Theologis A. Outcomes of fusions from the cervical spine to the pelvis. Global Spine J. 2019;9(01):6–13. doi: 10.1177/2192568217705655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen L E, Fullerton N, Mundy L R. Optimizing successful outcomes in complex spine reconstruction using local muscle flaps. Plast Reconstr Surg. 2016;137(01):295–301. doi: 10.1097/PRS.0000000000001875. [DOI] [PubMed] [Google Scholar]


