Abstract
Background
The treatment effects and safety of ear acupressure (EAP) for patients with allergic rhinitis (AR) have yet to be clarified.
Objective
To evaluate the effects and safety of EAP in AR patients.
Design
Systematic review of published studies.
Methods
A total of 24 English and Chinese databases (PubMed, EMBASE (Excerpta Medical Database), Cochrane Central Register of Controlled Trials, CINAHL, Informit, ScienceDirect, LILACS (Latin American and Caribbean Health Sciences), ProQuest, AMED, Blackwell Synergy, PsycINFO, Panteleimon, AcuBriefs, KoreaMed, IndMed, Ingenta, mRCT, ISI Web of Knowledge, ERIC, VIP Information (http://www.cqvip.com), China National Knowledge Infrastructure (http://www.cnki.net), Cochrane Library, Chinese Cochrane Centre Controlled Trials Register Platform, and Wanfang Chinese Digital Periodical and Conference Database) were searched from their respective inceptions to August 2020 to collect randomized controlled trials of ear acupressure for allergic rhinitis. We performed literature inclusion, data extraction, and trial quality evaluations. Methodological quality was assessed according to the Cochrane Handbook. Revman5.3 was used for all analyses.
Results
A total of 203 trials were identified and eleven studies involved 1094 participants aged 3–70 years. EAP was better than control group interventions in terms of effectiveness (risk ratio (RR): 0.51; 95% confidence interval (CI): 0.36–0.70; P < 0.0001). EAP was superior to sham EAP in terms of improvement of the total nasal symptom score (RR: −0.50; 95% CI: −0.96–0.05; P = 0.03), sneezing score (RR: −0.36; 95% CI: −0.59–0.12; P = 0.003), global QoL score (RR: 0.42; 95% CI: 0.04–0.08; P = 0.03), and eye symptom score (RR: −0.36; 95% CI: −0.67–0.05; P = 0.02).
Conclusions
Despite the positive results, it is premature to confirm the efficacy of EAP for treating AR. More high-quality studies are needed to confirm safety and efficacy.
1. Introduction
Allergic rhinitis (AR) is a global health problem. It is a common symptomatic, inflammatory, and immunological disorder of the nasal mucosa, characterised by four classic symptoms: sneezing, nasal itching, airflow obstruction, and clear nasal discharge caused by IgE-mediated reactions [1]. AR can be subdivided into intermittent (four symptoms for <4 days per week or for <4 weeks) and persistent disease (four symptoms for >4 days per week or for >4 weeks) [2].
A self-reported epidemiologic study suggested that 10–30% of adults have AR and no fewer than 40% of children have AR [3]. In other words, more than 60 million people suffer from AR in the United States annually. A European epidemiologic study reported a prevalence rate of 25% [4].
Due to the annoying symptoms, AR has significant adverse effects according to several trials; these include disturbing symptoms [5–9], alterations in quality of life (QOL) [5, 8, 10–15], hindrance of daily activities [16–20], emotional disturbances [9, 21], sleep [10, 22–26], and education disturbances [9, 16, 27]. These data suggest that the effect on adolescent life is negative and far reaching. AR has been shown to be associated with obstructive sleep apnoea [27].
Avoidance of exposure to specific allergens, patient education, pharmacological treatment, and immunotherapy form the current management approaches. Among these methods, medications are the most often selected strategy. A stepwise medical treatment protocol was proposed at the ARIA workshop report [28]. However, treatment based on guidelines is not effective in all patients [29]. Hence, many allergic rhinitis sufferers seek complementary and alternative medicine (CAM).
EAP is an alternative therapy in which magnetic bead or the seed of cowherb is attached to specifically stimulate points on the pinna. From the point of view of traditional Chinese medicine (TCM), all the major energy lines (meridians where acupuncture points are situated) are directly or indirectly connected to the ear. EAP was a shown to be effective for relief AR symptoms [30, 31]. However, a previous meta-analysis suggested that the benefit of ear acupressure for symptomatic relief of allergic rhinitis is unknown [32].
In this previously published meta-analysis, the authors summarized the evidence of EAP on AR. However, this study made a mistake in literature, including a duplicate publication of Rao et al. (2005) and Rao and Han et al. (2006). In their results section, the authors stated that “ear acupressure was more effective than herbal medicine, as effective as body acupuncture or antihistamine for the short-term effect, but it was more effective than antihistamine for the long-term effect.” This statement may have been exaggerated, and the quality of evidence was low. In the present systematic review and meta-analysis, we provide an updated summary of evidence to evaluate the safety and efficacy of EAP for patients with AR.
2. Methods
Methodologic issues were resolved with guidance from the Cochrane Handbook for Systematic Reviews of Interventions [33].
2.1. Search Strategy
A total of 24 English and Chinese databases were searched from their inceptions to August 18, 2020. These were PubMed, EMBASE (Excerpta Medical Database), Cochrane Central Register of Controlled Trials, CINAHL, Informit, Science Direct, LILACS (Latin American and Caribbean Health Sciences), ProQuest, AMED, Blackwell Synergy, PsycINFO, Panteleimon, AcuBriefs, KoreaMed, IndMed, Ingenta, mRCT, ISI Web of Knowledge, ERIC, VIP Information (http://www.cqvip.com), China National Knowledge Infrastructure (http://www.cnki.net), Cochrane Library, Chinese Cochrane Centre Controlled Trials Register Platform, and Wanfang Chinese Digital Periodical and Conference Database. The Chinese Clinical Trial Registry Centre was also retrieved for ongoing trials. References of related identified publications were checked for additional trials, and we contacted authors by e-mail or telephone for additional data where necessary.
Throughout the search process, the following key words were used: the combination of allergic, rhinitis, rhinallergosis, AR, allergy, rhinitis, hay fever, ear, acupressure, acupuncture, auricular, acupoint, sticking, randomized controlled trial, RCT, and their synonyms. Two authors (SQL and QXZ) screened all citations independently. Table 1 displays the search strategy of the Cochrane Library.
Table 1.
Search strategy of the Cochrane Library.
| Number | Search terms |
|---|---|
| 1 | Mesh descriptor: (ear acupressure) explode all trees |
| 2 | ((Ear∗) or (acupressure∗) or (acupuncture∗) or (auricular∗) or (acupoint∗) or (sticking ∗)): ti, ab, kw |
| 3 | Or 1-2 |
| 4 | Mesh descriptor: (allergic rhinitis) explode all trees |
| 5 | ((Allergic rhinitis∗) or (allergic∗) or (rhinitis, allergic∗) or (rhinallergosis∗) or (AR∗) or (hay fever∗)): ti, ab, kw |
| 6 | Or 4–5 |
| 7 | Mesh descriptor:(randomized controlled trials) explode all trees |
| 8 | (Random∗) or (randomly∗) or (allocation∗) or (random allocation∗) or (placebo∗) or (double blind∗) or (clinical trials∗) or (randomized control trial∗) or (RCT∗) or (controlled clinical trials∗)): ti, ab, kw |
| 9 | Or: 7-8 |
| 10 | 3 and 6 and 9 |
2.2. Study Selection
2.2.1. Eligible Criteria
Randomised controlled trials of EAP for AR were taken into account regardless of language or publication year. Patients presenting with seasonal AR or perennial AR of any age or gender were all included. We compared EAP with conventional therapy or Chinese herbal medicine formula or acupuncture or electroacupuncture or surgical therapy or placebo regimens studies.
2.2.2. Ineligible Criteria
Observational studies, case reports, case series, letter, qualitative studies, and uncontrolled studies were excluded. Quasi-RCTs are not truly RCT. Including quasi-RCTs in the review may be detrimental to the power of conclusion. Hence, quasi-RCTs were also excluded. Allergic rhinitis merged with allergic asthma or allergic conjunctivitis and other allergic diseases were excluded. This was performed because targeted drug combination methods in these studies could not be used to compare effects.
EAP as intervention in the control group was excluded. When EAP was compared with other types of CHMFs or some other alternative therapy such as moxibustion therapy, nose massage, plaster therapy, or acupoint injection as the intervention treatment group, these were excluded due to the idea that combination therapy would disturb the efficacy summary. EAP as intervention in two groups using different auricular points was also excluded because these studies can be identified as explorations for the stimulation effect of various auricular ear points. Diagnostic criteria were required because accurate diagnosis is a prerequisite for targeted treatment.
All titles and abstracts of identified studies were initially scanned independently by our two authors (JZ and SQL). The full-text articles were obtained for further screening for inclusion in this review by these two authors when needed. A determination was then made as to whether the studies met our inclusion criteria. Any conflicts or disagreement were resolved by discussion.
2.3. Outcome Measures
Trials were required to include as outcome measures either relief of symptoms of AR or evaluation of the efficacy of EAP in AR. The efficacy of EAP for AR was set as primary outcomes. Improvement in quality of life, improvement of symptom scoring and other scale, and adverse events were set as secondary outcomes.
2.4. Methodological Quality Assessment, Data Extraction, and Data Analysis
The risk of bias was assessed according to the Cochrane Handbook for Systematic Reviews of Interventions. The latest version of this tool was updated in March 2011, version 5.1.0 (http://www.handbook.cochrane.org/). Risk of bias items included the following: randomization sequence generation, allocation concealment, blinding of participants or healthcare providers, detection bias, incompleteness bias, reporting bias, and other biases. Raw data of all included studies containing the details of authors, the publication information, and design information of the original study were separately extracted by three authors (DL, TL, and QG).
2.5. Data Analysis
Review Manager software version 5.3 was used to pool our data to perform the meta-analysis. Risk ratio (RR) was chosen for dichotomous data (efficacy, recurrence rate, and adverse events). Confidence interval (CI) was set at 95%, and P < 0.05 was defined as statistically significant. Cochrane X2 and I2 tests were used to investigate the heterogeneity of data. The statistical heterogeneity was considered substantial when P < 0.05 and I2 > 50%, and then, a random effect model was used to calculate the effect size. If P > 0.05 and I2 < 50%, then the studies included were homogeneous, and a fixed effect model was applied. Sensitivity analysis was conducted to test whether the resulting war was robust by excluding the study one by one and comparing the rest of the studies' effects with all the studies' total effects. We pooled trials when the intervention forms of those studies were adequately similar. Specific subgroups were analysed according to similar intervention forms or similar design. Funnel plots were generated for more than ten studies.
3. Results
We initially identified a total of 157 trials using the specific search strategy. No unpublished or ongoing studies were found. Sixty-nine duplicated texts were excluded. After reviewing titles, abstracts, and keywords, 52 studies were excluded for failure to conform to inclusion criteria. Thirty-six studies had initially appeared to meet our inclusion criteria. After the full texts were read, 25 were excluded, and t studies finally met our inclusion criteria. The study selection process is outlined in Figure 1.
Figure 1.
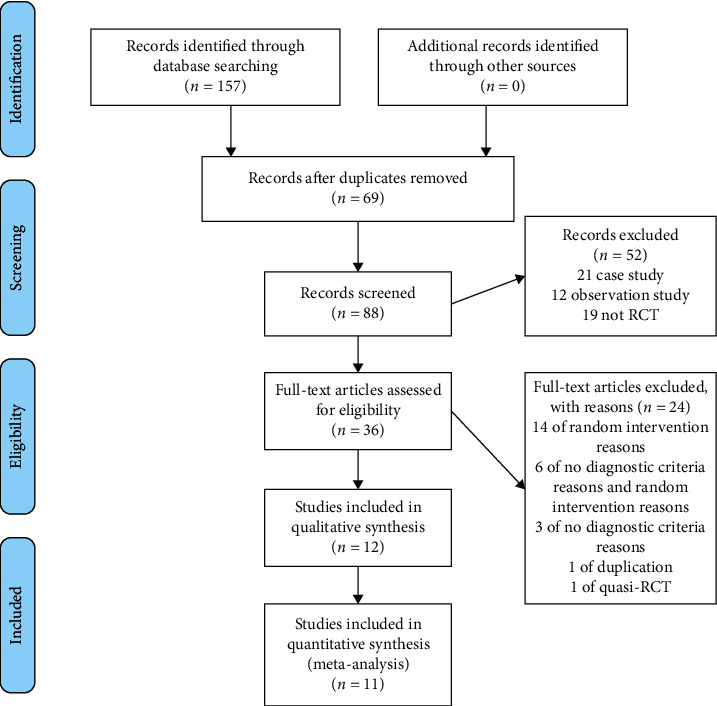
Flowchart of database searching and study identification.
3.1. Characteristics of Included Studies
There were eleven studies total. These included 10 Chinese language studies and one English language study [32], comprising 1094 participants aged 3–70 years [32, 34–43], published between 2005 and 2019. All Chinese studies come from the Chinese mainland.
Interventions in five Chinese studies [34, 35, 37, 38, 43] were EAP versus CT. Four studies [34, 35, 38, 43] compared EAP to CT, including levocabastine, beclomethasone propionate nasal spray, astemizole, and cetirizine [37]. One study compared EAP combined with cetirizine to cetirizine alone [37]. Among these studies, Rao et al. included three comparisons, that is, the experiment group (ear-acupressure) and two control groups (acupuncture and cetirizine). In order for the reader to accurately identify intervention data, we extracted cetirizine control group data from Rao et al. (2005a). There are 245 participants in Claire et al. (2014). This was an international, multicentre, randomized, single-blind, sham-controlled trial. The intervention was EAP vs. sham EAP. Acupuncture therapy was the intervention of the control group in three studies [34, 36, 40], and electroacupuncture was the intervention of the control group in one study [39]. In the remaining two studies, CHMF was the intervention in the control group; these were Xinqin granules [41] and Shetizhiqiu decoction [43].
In these studies, Semen vaccariae (cow soapwort seed or Wang Bu Liu Xing) were used in eleven studies [34, 38–43] to press the ear points, while stainless steel pellets were used by Claire et al [38].
All studies provided the details of points used for ear acupressure. Among the total 19 ear points used in these 11 studies, Nei Bi (TG4) was used in all the studies. The lung (CO14), kidney (CO10), spleen (CO13), and adrenal gland (TG2p) were applied 10, 8, 7, and 6 times, respectively. We presented the frequency of ear point use in a radar plot (Figure 2).
Figure 2.
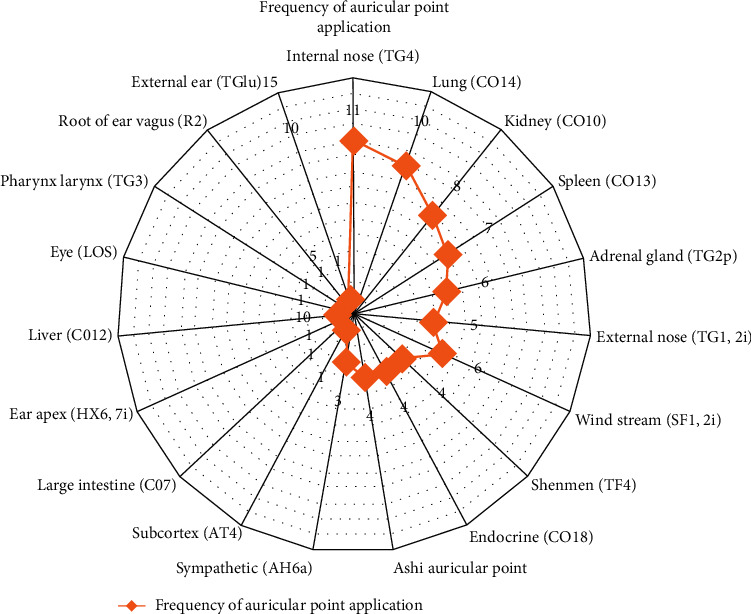
Frequency of auricular point application.
Referring to outcome measures, the effective rate indicator was regarded as the most important outcome measure in 10 trials [34–42]. Total nasal symptom score was calculated in two trials [37, 44]. The visual analogue scale was used in one trial [37]. The Quality Of Life Questionnaire is used only one study [39]. Of these 12 studies, five did not report details of adverse events [35, 36, 38–40], and six trials [32, 34, 37, 41, 42] recorded adverse events. In Claire et al., adverse events (AEs) were a secondary outcome. Characteristics of included studies are displayed in Table 2.
Table 2.
Characteristics of 11 included studies.
| Study ID | Sample size (E/C) | Male:female (E/C) | Age (E/C), year | Duration | Criteria of diagnose | Interventions | Period | Outcome measure | |
|---|---|---|---|---|---|---|---|---|---|
| Experimental group | Control group | ||||||||
| Yuan et al., 2013 [38] | 120 (60/60) | Not given | 3–14 | ≥1 year | Mentioned | Ear acupressure | Levocabastine | 30 days | Effective rate, IgE, PAF |
|
| |||||||||
| Li et al., 2018 [42] | 72 (36/36) | 19 : 17/16 : 20 | 18–65 | Not given | Mentioned | Ear acupressure | Beclomethasone propionate nasal spray | 3 weeks | Effective rate |
|
| |||||||||
| Han et al., 2006 [35] | 80 (40/40) | 24 : 16/21 : 19 | 10–50 | 1–15 years | Mentioned | Ear acupressure | Astemizole | 14 days/3 months | Effective rate |
|
| |||||||||
| Rao, 2005 [34] | 81 (39/42) | 24 : 25/26 : 21 | 13–65 | 1–40 years | Mentioned | Ear acupressure | Acupuncture | 1 month/follow-up | Effective rate, symptom score, IgE, TFN-γ |
|
| |||||||||
| Rao and Han, 2005a [45] | 80 (39/41) | 24 : 25/25 : 21 | 13–65 | 1–40 years | Mentioned | Ear acupressure | Cetirizine tablets | 1 month/follow-up | Effective rate, symptom score, IgE, TFN-γ |
|
| |||||||||
| Claire et al., 2014 [32] | 245 (124/121) | Not given | 18–70 | ≥2 years | Mentioned | Real ear acupressure | Sham ear acupressure | 8 weeks | Primary outcome measures: nasal and nonnasal symptom scores. Secondary outcomes:QoL score, change of relief medication usage, adverse events (AEs), and credibility of blinding |
|
| |||||||||
| Ou et al., 2012 [37] | 60 (30/30) | 15 : 15/13 : 17 | 18–51/18–52 | 4–60 weeks | Mentioned | Ear acupressure + conventional therapy | Conventional therapy (cetirizine) | 4 weeks | Effective rate, VAS |
|
| |||||||||
| Ye et al., 2008 [36] | 80 (40/40) | Not given | 10–61 | 0.5–5 years | Mentioned | Ear acupressure + acupuncture | Acupuncture | 4 weeks | Effective rate, symptom score |
|
| |||||||||
| Yuan et al., 2016 [40] | 120 (60/60) | 27 : 33/28 : 32 | 21–67/19–69 | 2–11 years | Mentioned | Ear acupressure + acupuncture | Acupuncture | 30 days | Effective rate |
|
| |||||||||
| Lu et al., 2015 [39] | 60 (30/30) | 19 : 11/21 : 9 | 10–70 | Not given | Mentioned | Ear acupressure + electroacupuncture | Electroacupuncture | 1 week | Effective rate, RQLQ |
|
| |||||||||
| Zhao, 2019 [43] | 58 (29/29) | 18 : 11/13 : 16 | 18–65 | 4.48 ± 1.9/4.24 ± 2.08 | Mentioned | Chinese medicine formula + ear acupressure | Chinese medicine formula (Shetizhiqiu decoction) | 4 weeks | Effective rate, symptom score |
|
| |||||||||
| Liao, 2016 [41] | 58 (30/28) | 11 : 19/12 : 16 | 18–60 | 2.7 ± 2.26/1.86 ± 1.04 | Mentioned | Chinese medicine formula + ear acupressure | Chinese medicine formula (Xinqin granule) | 20 days | Effective rate |
|
| |||||||||
| Li, 2017 [46] | 120 (60/60) | 62 : 58 | 15–74 | 1–18 years | Mentioned | Ear acupressure + microwave therapy under nasal endoscope | Microwave therapy under nasal endoscope | 30 days | Effective rate |
3.2. Reasons for Study Exclusion
After our two authors read full texts of all included studies, we excluded 25 trials. The reasons for exclusion of those studies were as follows:
If a trial did not mention “diagnostic criteria,” we excluded it on the basis of having “diagnostic criteria reason”
If a trial did not meet inclusion criteria for interventions, we excluded it on the basis of “intervention reason”
If a study was a repeated publication, we excluded it on the basis of being “duplication”
Overall, there were ten “diagnostic criteria reason” studies, 14 “intervention reason” trials, and six that had both. Those were excluded for incomparability of the interventions. One “duplication” was identified. Characteristics of the 25 excluded studies are displayed in Table 3.
Table 3.
Characteristics of the 25 excluded studies.
| Study ID | Sample size (E/C) | Male:female (E/C) | Age (E/C), year | Duration | Criteria of diagnose | Interventions | Period | Outcome measure | Reasons of exclusion | |
|---|---|---|---|---|---|---|---|---|---|---|
| Experimental group | Control group | |||||||||
| Feng, 2020 | 70 (35/35) | 20 : 15/22 : 13 | 10–49 | 4–16 years | Not mentioned | EAP + traditional Chinese medicine sticking | Cetirizine tablets | 20 days | Effective rate | Diagnostic criteria reason and intervention reason |
|
| ||||||||||
| Zhou, 2015 [43] | 60 (30/30) | 14 : 16/13 : 17 | 18–60 | Not mentioned | Mentioned | EAP + Chinese herbal medicine formula | Ebastine hydrochloride tablets | 21 days | Effective rate | Intervention reason |
|
| ||||||||||
| Zeng, 2020 [30] | 100 (50/50) | 27 : 23/28 : 22 | 37–57 | 1–12 years | Not mentioned | EAP + Chinese medicine formula (Shenling Baizhu powder) | Cetirizine tablets | 30 days | Effective rate; SF-36 | Diagnostic criteria reason and intervention reason |
|
| ||||||||||
| Cai, 2019 | 36 (18/18) | 10 : 8/11 : 7 | 19–55 | Not mentioned | Mentioned | EAP + acupuncture + Chinese medicine formula (Wenyang Tongqiao formula) | Chinese medicine formula (Wenyang Tongqiao formula) | 21 days | Effective rate | Intervention reason |
|
| ||||||||||
| Chen, 2015 | 70 (35/35) | 20 : 15/18 : 17 | 15–70 | 1–22 years | Not mentioned | EAP + acupoint injection | Loratadine tablets + 1% ephedrine nasal drops | 30 days | Effective rate:Total nasal symtom score | Diagnostic criteria reason and intervention reason |
|
| ||||||||||
| Chen, 2016 | 96 (48/48) | 26 : 22/27 : 21 | 10–87 | Not mentioned | Not mentioned | EAP + traditional Chinese medicine sticking + sublingual immunotherapy | Sublingual immunotherapy | 30 days | Effective rate: total nasal symptom score | Diagnostic criteria reason and intervention reason |
|
| ||||||||||
| Cheng, 2011 | 60 (30/30) | 19 : 11/20 : 10 | 17–59 | 1–20 years | Mentioned | EAP + massage | Beclomethasone propionate nasal aerosol | 14 days | Effective rate: total nasal symptom score | Intervention reason |
|
| ||||||||||
| Lin, 2011 [8] | 60 (30/30) | 32 : 28 | 6–39 | 2–13 years | Mentioned | EAP + crude herb moxybustion | Acupuncture | Undefined | Effective rate | Intervention reason |
|
| ||||||||||
| Wang, 2012 | 80 (40/40) | 22 : 18/25 : 15 | 11–71 | 1–25 years | Mentioned | EAP + massage | Cetirizine tablets | 60 days | Effective rate: total nasal symptom score | Intervention reason |
|
| ||||||||||
| Wang, 2015 | 120 (60/60) | 24 : 36/22 : 38 | 16–60 | 1–7 years | Mentioned | EAP + catgut in acupoint | Acupuncture | 60 days | Effective rate | Intervention reason |
|
| ||||||||||
| Zhu, 2018 | 71 (48/29) | 27 : 21/15 : 14 | 16–58 | 1.5–21 years | Mentioned | EAP + crude herb moxibustion | Azotyn tablets | 2 weeks in the control group and 1 year on the treatment group | Effective rate; RQLQ | Intervention reason |
|
| ||||||||||
| Sun, 2019 | 60 (not mentioned) | 30 : 25 | 8–62 | 1 month–15 years | Mentioned | EAP + Chinese medicine formula (Guizhi decoction) | EAP | 20 days | Effective rate | Intervention reason |
|
| ||||||||||
| Xia, 2018 | 100 (50/50) | 22 : 28/20 : 30 | 18–46 | 5 weeks–13 years | Not mentioned | Ear acupuncture + blood-letting therapy | Ear acupuncture | 18 days | Effective rate | Diagnostic criteria reason and intervention reason |
|
| ||||||||||
| Li, 2013 | 100 (50/50) | 22 : 28/20 : 30 | 19–49 | 1–10 years | Mentioned | EAP + sweet chrysanthemum capsule | Loratadine tablets | 4 weeks | Effective rate: total nasal symptom score | Intervention reason |
|
| ||||||||||
| Xu, 2019 | 60 (30/30) | 17 : 13/15 : 15 | 26–63 | Not mentioned | Mentioned | EAP + Chinese medicine formula (Guizhi decoction) | Cetirizine tablets | Not mentioned | Effective rate: total nasal symptom score | Intervention reason |
|
| ||||||||||
| Huang, 2017 | 60 (30/30) | 13 : 17/13 : 17 | 5–70 | 3weeks-7 years | Mentioned | EAP + Chinese medicine formula (Wenbi Tongqiao decoction) | Not mentioned | Not mentioned | Effective rate | Intervention reason |
|
| ||||||||||
| Xue, 2016 | 60 (30/30) | 19 : 11/16 : 14 | 18–70 | 1–10 years | Mentioned | EAP + massage | Clarityne + Raynaud's nose spray | EAP: 1 days; massage: 6 months; Clarityne + Raynaud's nose spray: not mentioned | Effective rate: total nasal symptom score | Intervention reason |
|
| ||||||||||
| Fu, 2015 | 80 (40/40) | 18 : 22/19 : 21 | 9–49/11–56 | 1 month-20 years | Not mentioned | EAP + Chinese medicine formula (Yupingfeng granule) | Azelastine nasal spray | 2 weeks | VAS | Diagnostic criteria reason and intervention reason |
|
| ||||||||||
| Li, 2010 | 80 (47/33) | 28 : 19/20 : 13 | 4–55/8–57 | 2–17 years | Mentioned | EAP + Chinese medicine formula (Yupingfeng granule) | Cetirizine tablets | 20 days | Effective rate | Intervention reason |
|
| ||||||||||
| Lv, 2012 | 110 (60/50) | 26 : 34/21 : 29 | 13–56/11–60 | 3 months–12 years | Mentioned | EAP + Chinese medicine formula (Yupingfeng granule) | EAP | 3 months | Effective rate | Intervention reason |
|
| ||||||||||
| Wang, 2004 | 400 (300/100) | 241/159 | 5–59 | 3 months–5 years | Not mentioned | EAP | Chinese medicine formula (Biyankang tablets) | 1month | Effective rate | Diagnostic criteria reason |
|
| ||||||||||
| Kong, 2006 | 108 (54/54) | Not mentioned | 14–62 | Not mentioned | Not mentioned | EAP | Chinese medicine formula (Biyankang tablets) | Not mentioned | Effective rate | Diagnostic criteria reason |
|
| ||||||||||
| Huo, 2003 | 66 (30/36) | Not mentioned | 22–65/20–62 | Not mentioned | Not mentioned | EAP | Body acupuncture or antihistamine | Not mentioned | Effective rate | Diagnostic criteria reason |
|
| ||||||||||
| Rao, 2006 [45] | 141 (42/39/41) | 26 : 21/24 : 25/25 : 21 | 13–65 | 1–40 years | Mentioned | Ear acupressure | Acupuncture/cetirizine tablets | 1 month/follow-up | Effective rate, symptom score, IgE, TFN-γ | Duplication |
|
| ||||||||||
| Li, 2017 | 120 (60/60) | 62 : 58 | 15–74 | 1–18 years | Mentioned | Ear acupressure + microwave therapy under nasal endoscope | Microwave therapy under nasal endoscope | 30 days | Effective rate | |
A list of 25 excluded studies by reading full text is displayed in Table 4.
Table 4.
A list of excluded studies by reading full text.
| Reason | Reference |
|---|---|
| Duplication (n = 1) | Rao Y.Q. and Han N.Y. (2006): therapeutic effect of acupuncture on allergic rhinitis and its effects on immunologic function (in Chinese). Zhongguo Zhen Jiu 26, 557–560 |
|
| |
| Diagnostic criteria (n = 4) | Wang W.H. (2004): 300 cases of allergic rhinitis treated by ear acupressure (in Chinese). Shanghai zhen jiu za zhi 23, 35 |
| Kong X.B., Ren H.Y., and Lu M.L. (2006): 108 cases of allergic rhinitis tested by ear acupressure (in Chinese). World Health Digest3, 34 | |
| Huo Z.J. (2003): comparison of therapeutic effects of auricular acupuncture and body acupuncture on allergic rhinitis (in Chinese). Zhong Guo Zhen Jiu 23, 253–254 | |
|
| |
| Intervention reason (n = 13) | Changqing L.: clinical observation of 60 cases of allergic F-inflammation treated by acupoint pressing with traditional Chinese medicine according to syndrome differentiation. Chinese community doctors 2012, 17 : 228–229. DOI: l0.3969/j.issn. l007 -6l4x.20l2.l7.2l7. |
| Bofeng L.: observation on the curative effect of auricular point sticking and pressing plus yufeng powder on 47 cases of allergic rhinitis. Inner Mongolia traditional Chinese medicine 2010, 3 : 28–29. DOI: 10. 16040/j. cnki. cn15 -1101. 2010. 10. 045 | |
| Haiyan X.: evaluation of the therapeutic efficiency of the comprehensive care combining auricular acupoint magnetic therapy and nasal acupoint massage on the prevention and treatment for the allergic rhinitis. Int J Nurs, June 2016, 35(11): 1569–1573. | |
| Huangjiali: auricular point pressing bean therapy was used to treat 60 cases of allergic rhinitis. Int J Nurs, June 2017, 3 : 259. Ying X.: efficacy of the Guizhi decoction plus auricular point on clinical symptoms in patients with allergic rhinitis. Clinical Journal of Chinese Medicine 2019, 32 (11):28–30. | |
| Xun L., LiXin T., Yali Z., and Jianhua L.: clinical observation of Xiangju capsule combined with auricular point pressing bean in the treatment of allergic rhinitis. Chinese Journal of Otolaryngology 2013, 12(1):23–25. | |
| LiSun: observation on the effect of guizhi decoction combined with allergic decoction and auricular point pressing therapy on allergic rhinitis. Contemporary Medical Symposium 2019, 17(2):187–188. | |
| Zhuhua: Crude herb moxibustion therapy combined with auricular point sticking therapy for allergic rhinitis. IMHGN, September 2018, 24(18):2751–2753. DOI: 10.3760/cma.j.issn.1007–1245.2018.18.007 | |
| Quanquan W., Huimin H., Fang Z., Hailin C., and Maosen Z: observation of 40 cases of perennial allergic rhinitis treated by ear pressure combined with massage. Hebei J TCM 2012, 34(3):403–404. | |
| Yanxia L., Lihong D., and Liying F: observation on the curative effect of tian moxibustion plus auricular acupoint on allergic rhinitis. Journal of Medical Forum 2011, 32(2):183–184. | |
| Ling Z. and Wo Y.: clinical observation of the treatment of rhinitis 1 combined with auricular point platen press on allergic rhinitis. Heilongjiang Medical Journal 2015, 39(3):297–298. | |
| Hualei W. and Rong Y.: clinical observation of acupoint embedding line combined with ear pressure in the treatment of 60 cases of allergic rhinitis. Yunnan Journal of Traditional Chinese Medicine 2015, 36(12):57–58. | |
| Guolin C., Qiuhong Y., and Deyao C.: clinical observation on the treatment of allergic rhinitis by self-imitating five acupuncture points and four points combined with the warming yang tongqiao supplement-benefit method. Heilongjiang Medicine Journal 2019, 32(1):15–17. | |
| Zhipeng C., Li F., Jinming W., Lijun L., and Xiuxi T.: clinical observation of 30 cases of allergic rhinitis treated by massage and auricular point sticking. Journal of Community Medicine 2011, 9(1):49–50. | |
| Diagnostic criteria reason and intervention reason (n = 6) | Shuyan F.: study on the value of auricular point pressing pill plus Chinese medicine sticking point in the treatment of allergic rhinitis. Broad vision of health 2020, 13 : 191. |
| Jing C.: clinical observation on the treatment of allergic rhinitis by sublingual immunity combined with auricular point pricking and Chinese medicine application. Shenzhen Journal of Integrated Traditional Chinese and Western Medicine, 2016, 26(6):25–26. | |
| Zheng X.: to explore the clinical effect of ear acupuncture combined with blood-letting puncture in the treatment of allergic rhinitis. Feet and health care 2018, 12(194):177–178. DOI: 10.19589/j.cnki.issn 1004–6569.2018.12.17.7 | |
| Fujixiong.: efficacy evaluation of auricular point sticking pressure combined with yufeng granules in treating allergic rhinitis. Journal of new medicine 2015, 47(2):189–190. | |
| Koufen C. and Xiuhua X.: observation on the effect of acupoint injection combined with auricular press in the treatment of perennial allergic rhinitis. Contemporary Medicine Forum 2015, 13(22):19–20. | |
| Huiyan Z.: clinical effect of Shenling Baizhu powder combined with ear acupressure pills on allergic rhinitis. China Modern Medicine 2020, 27(16):186–189. | |
|
| |
| Quasi-RCT (n = 1) | Lixia: effect of auricular point sticking combined with microwave under nasal endoscope in the treatment of allergic rhinitis. Journal of Chinese Rural Medicine 2017,24(20): 62–63. |
3.3. Methodological Quality of Included Studies
3.3.1. Allocation (Selection Bias)
In 11 included studies, there were all designed as randomized controlled trials [32, 34–43].
In six RCTs [35–38, 40, 42], the method of randomization and allocation was not mentioned. Because of the lack of allocation concealment and the details of the randomization procedure, there might be a high risk of selection bias in these trials.
In the study by Lu et al. (2015) [39], randomization and the random allocation sequence concealment were reported. Hence, a low risk of bias could be defined in these trials.
Three studies conducted by Li et al. (2018) [42], Rao et al. (2005) [34], and Liao et al. (2016) [41] mentioned that a random number table tool was used for the allocation of participants. However, in the original texts, the authors failed to clearly describe the details regarding how the participants were allocated and concealed. Therefore, there was a high risk of selection bias in these studies.
3.3.2. Blinding (Performance and Detection Biases)
Of the 11 studies, only Claire et al. (2014) [32] and Lu et al. (2015) [39] presented blinding information. In Claire et al. (2014), randomization numbers were reported as generated by an independent statistician using a computer system and sealed in individual opaque envelopes. In the study Lu et al. (2015) [39], to blind the outcome assessor, researchers who knew the whole course of treatment were not involved. In this way, the risk of performance and detection bias were be classified as low.
The remaining 9 trials failed to mention their blinding [34–38, 40–42]. Perhaps blinding was difficult because the materials and manipulations used in the treatment were totally different in the test and control groups. However, at least the outcome assessors should have been blinded. Because there was no blinding in these studies, there might be high risk of performance and detection biases.
3.3.3. Incomplete Outcome Data (Attrition Bias)
In the study by Claire et al. (2014) [32], the sample size was determined based on previous reported results. Intention-to-treat analysis and dropout information were offered in this study also. Therefore, there might be a low risk of attrition bias.
Information regarding patient withdrawal was provided in Rao et al. (2005) [34], Liao et al. (2016) [41], and Zhao et al. (2019) [43]. Zhao et al. [43] reported one participant dropout into both groups. Liao et al. [41] reported two dropouts in the control group; however, the reason why those two patients were dropped out was not noted. Rao et al. [34] reported that three in the acupuncture therapy group (fear of pain), one in the ear-acupressure group (refused to continue treatment because of pain in the pinna), and four in the control group (severe headache, drowsiness and other adverse reactions occurred during taking the medicine could not continue to receive treatment) were dropped out. Therefore, those three studies were at a low risk for incomplete outcome reporting bias. However, a crucial limitation was that intention-to-treat and per-protocol analyses were not conducted in these three trials.
There were some limitations in seven studies (Ouyang et al. (2012), Yuan et al. (2013), Li et al. (2018), Ye et al. (2008), Yuan et al. (2016), Han et al. (2006), and Lu et al. (2015)) [35–40, 42] in terms of incompleteness bias because there were no sample size calculations, and no cases were reported to have been lost to follow-up or withdrawn from the trials. The incompleteness bias might be unclear in these trials due to failure to report dropouts.
3.3.4. Selective Reporting (Reporting Bias)
To reduce reporting bias, all analyses with and without statistically significant differences should be reported. One of the ways to assess reporting bias is to compare the results in the final reports with those in the protocol. However, 10 in 11 studies protocol could not be found in these studies, and only Claire et al. (2014) [32] declared a clinical trial registration number (ACTRN12608000149369). It was difficult to determine whether the other 10 outcomes were included in the published reports. Hence, the risk of reporting bias in these 10 studies was classified as “unclear,” while the risk of reporting bias in Claire et al. (2014) [32] was low.
3.3.5. Other Potential Sources of Bias
We set “support from pharmaceutical manufacturers” as other potential source of bias. Support in the form of free medical supplies, research funding support, and medical supplies marketing cooperation coming from pharmaceutical manufacturers could bias results. Nevertheless, no other potential sources of bias were found in these studies. There was publication bias by Rao et al. (2005). The risk of bias graph and summary of authors' judgements concerning included studies are shown in Figures 3 and 4, respectively.
Figure 3.
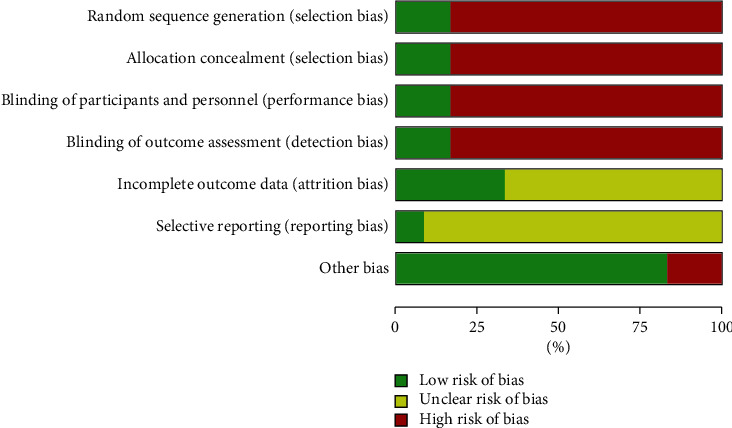
The risk of bias graph of authors' judgements concerning included studies.
Figure 4.
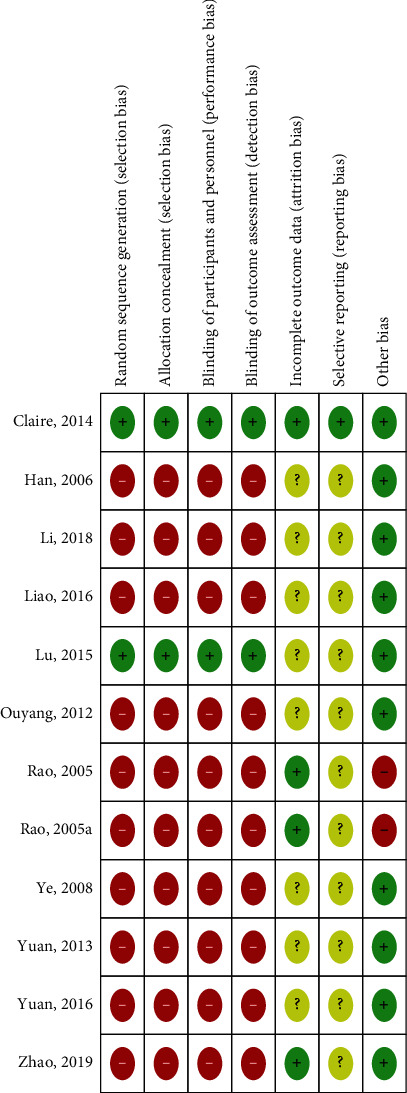
The risk of bias summary of authors' judgements concerning included studies.
4. Outcomes
4.1. Clinical Effectiveness
According to raw data extracted from 11 original texts, primary outcomes including effective rate, total nasal symptom score, runny nasal score, sneezing score, global QoL score, and eye symptoms were presented. Adverse events were presented as secondary outcomes.
4.2. Primary Outcomes
4.2.1. Total Effective Rate of EAP for AR
The effective rate is a composite endpoint composed of improvement of clinical symptoms. The results can be divided into three categories: significantly effective, effective, and ineffective. Four versions of the Chinese AR Clinical Handbook Indicator recommend AR therapies [46–49]. They were slightly different. In Haikou, 1997 criteria [46], “according to the sum of symptoms and signs scores before and after treatment, the efficacy of perennial allergic rhinitis was evaluated by the following formula: ≥51% was considered effective, 50%–21% was considered effective, and ≤20% was considered ineffective.” In other reports, “according to the symptoms and signs score, the efficacy was evaluated by the following scoring methods: ≥66% was marked as effective, 65%–26% as effective, and ≤25% as ineffective.”
In our review, there are 10 trials reporting effectiveness rates [34–43]. Han et al. 2006 and Rao et al. 2005 applied 1997 criteria, different from the others. We divided these studies into six subgroups according to intervention comparison forms into two groups: (1) four studies (Han et al., 2006; Li et al., 2008; Rao et al., 2005a; and Yuan et al., 2013) were EAP vs. CMT (conventional medicine therapy) comparisons; (2) Rao et al. (2005) used EAP vs. acupuncture; (3) two trials (Ye et al., 2008 and Yuan et al., 2016) used EAP plus acupuncture vs. acupuncture alone; (4) Lu et al. studied EPA plus electroacupuncture vs. electroacupuncture alone; (5) EPA plus Chinese medicine formula (CMF) vs. Chinese medicine formula alone was used in two articles (Liao et al. 2016; Zhao et al. 2019); and (6) one trial (Ouyang et al. 2012) studied EAP plus conventional therapy (CT) vs. CT alone.
We pooled these trials using RevMan 5.3. A total of 869 participants were pooled, 433 in the treatment group and 436 in the control group. We used a random-effects model because of the significant heterogeneity (I2 = 56%, P = 0.01). Meta-analysis revealed that the total effective rate in the treatment group was greater than that in the control group (pooled risk ratio = 0.51, 95% CI (0.36–0.70), P < 0.0001; Figure 5). Sensitivity analysis indicated that their result was robust (Figure 6).
Figure 5.
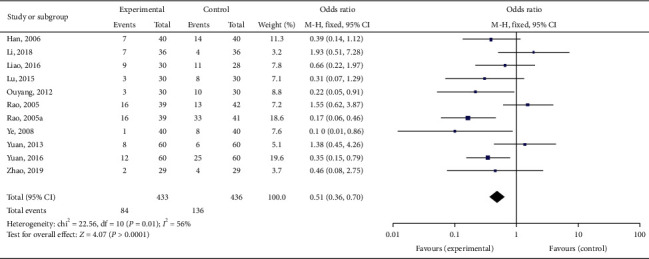
Forest plot for total effective rate.
Figure 6.
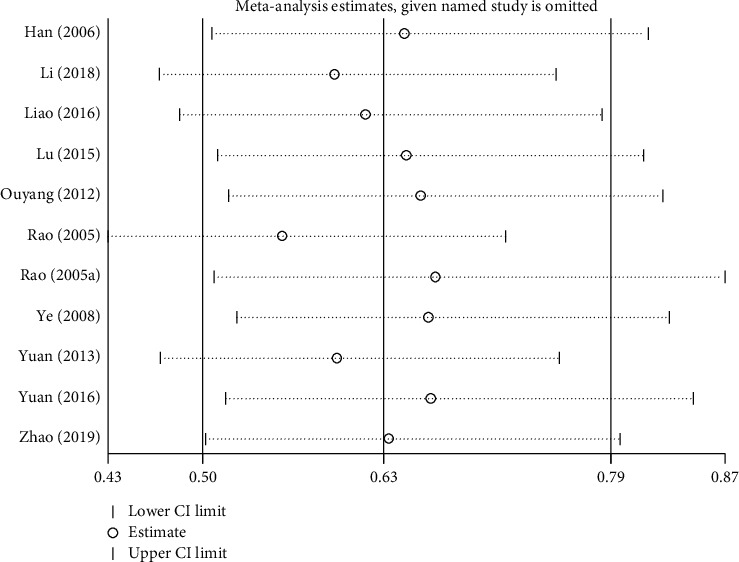
Sensitivity analysis for total effective rate.
Subgroup analysis showed that EAP was superior to control group treatments (RR: 0.63; 95% CI: 0.50–0.79; P=0.005; Figure 7).
Figure 7.
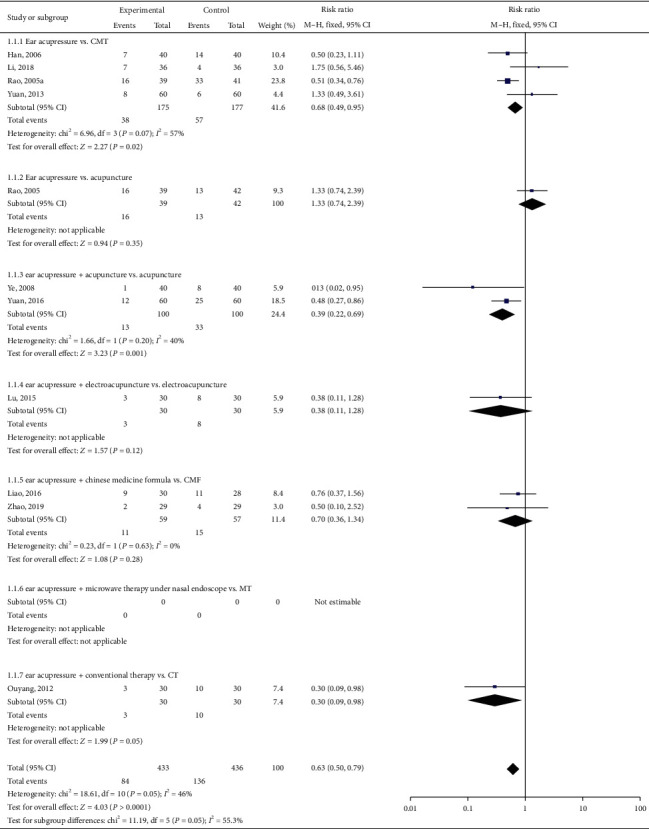
Forest plot for subgroup of total effective rate.
The funnel plot (Figure 8) suggested that publication bias may exist; however, other factors could also be present in Rao et al. (2005). This may due to poor design, in particular, the poorly allocated concealment method (the allocation concealment method was not mentioned in this study), leading to exaggerated treatment effects.
Figure 8.
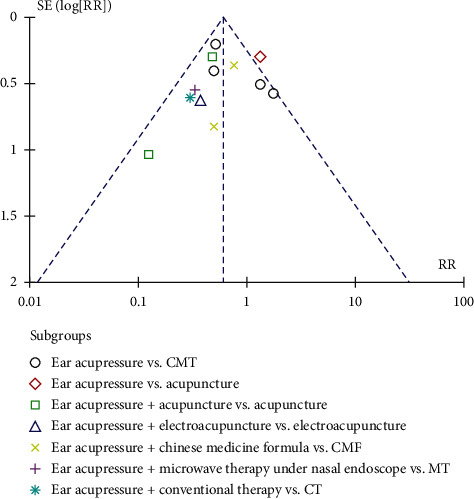
Funnel plot of total effective rate.
4.3. Secondary Outcomes
4.3.1. Total Nasal Symptom Score
Three studies reported the total nasal symptom score [32, 34, 45]. We pooled these data. We found that EAP was better than control group interventions (RR: −0.50; 95% CI: −0.96–0.05, P=0.03; Figure 9), including sham EAP, acupuncture, Western medicine cetirizine, and Shetizhiqiu decoction. There was significant heterogeneity among studies (I2 = 75%, P=0.008). Sensitivity analysis indicated that their result was robust (Figure 10).
Figure 9.
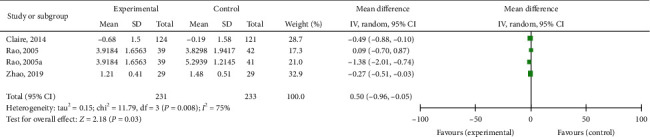
Forest plot for the total nasal symptom score.
Figure 10.
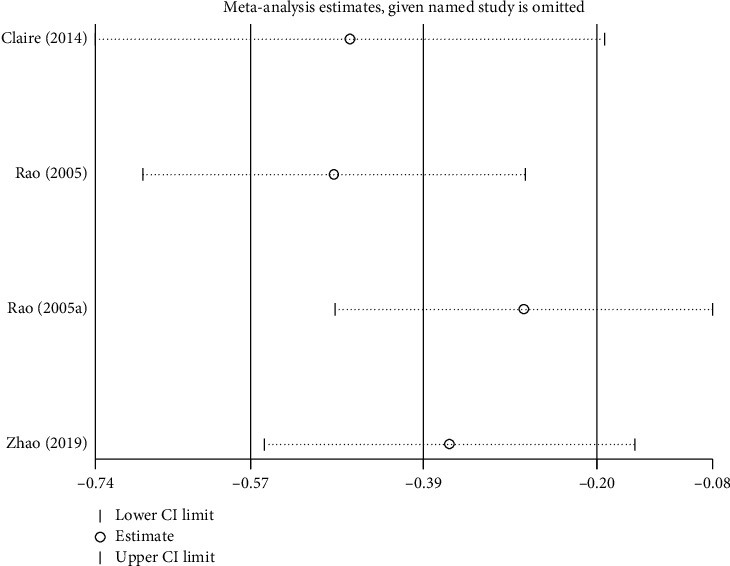
Sensitivity analysis for the total nasal symptom score.
4.3.2. Runny Nose Score
There were two trials noting the runny nose score [32, 45]. When EAP was compared with sham EAP or Shetizhiqiu decoction, the results were not statistically significant (RR: -0.23; 95% CI: -0.81–0.35; P=0.44; Figure 11). Sensitivity analysis indicated that this result was robust (Figure 12).
Figure 11.
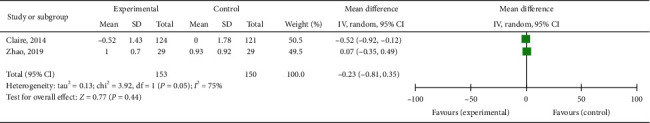
Forest plot for the runny nose score.
Figure 12.
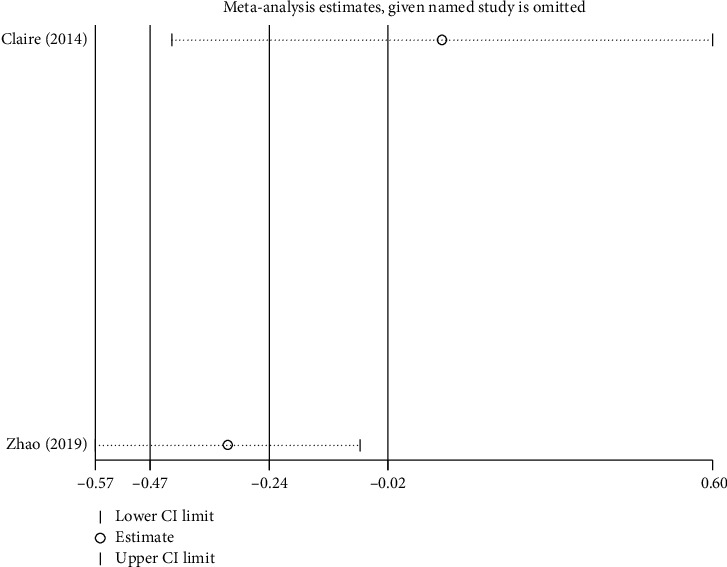
Sensitivity analysis for the runny nose score.
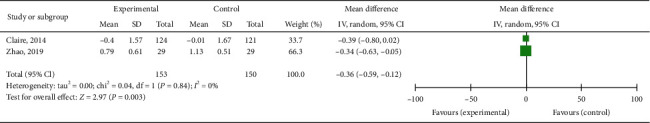
4.3.3. Sneezing Score
Two studies presented the sneezing score as outcome [39, 44]. Patients treated by EAP are superior to the patients in the control group (RR: −0.36; 95% CI: −0.59–0.12; P=0.003; Figure 13).
Figure 13.
Forest plot for Sneezing score.
4.3.4. Global QOL Score and Eye Symptom Score
Only Claire et al., 2014, used the eye symptom score and global QoL score. EAP was better than sham EAP in terms of the global QOl score improvement (RR: 0.42; 95% CI: 0.04–0.08; P=0.03) and eye symptom score (RR: −0.36; 95% CI: −0.67–0.05; P=0.02).
4.3.5. EAP Related Adverse Events (AEs)
In these 12 studies, five did not mention adverse events information [35, 36, 38–40], and six trials [32, 34, 37, 41–43] recorded adverse events. Of these, three studies [37, 41, 45] reported adverse events in two groups. Li et al. reported that five participants in the control group had nasal mucosa drying and bloody nasal mucus [42]. In the study by Rao et al. [33], the incidence of adverse reactions was reported as follows: no adverse reactions occurred in the acupuncture group (2.17% ear pressure group) or the control group (13.04%). Statistical analysis showed that there was a significant difference between the control group and the ear pressure group (P=0.05). In the acupuncture group, a patient had dizziness and nausea during the process of acupuncture. After the needle was released quickly, it was completely relieved after resting for half an hour. There were six cases of mild or transient adverse reactions, including two cases of mild headache and drowsiness, four cases of dry mouth, and three cases of gastrointestinal discomfort. However, how these effects were resolved was not noted.
In the study by Claire et al. [32], details of safety were noted specifically. There were eight participants in the real group who reported 17 AEs and nine participants in the sham group who reported 20 AEs (x2 = 0.01; P=0.76). Some EAP-related AEs such as pellets irritating skin (one and two in real/sham groups) and ear acupoint inflammation (two and one events in real/sham groups) were reported during the 1st week. These events were effectively managed by refining the pressing techniques by the participants, without any medical assistance required. On the other hand, they reported that some participants reported headache or dizziness (11 and 14 events in the real/sham group) and insomnia (two events in the sham group).
Another study presented safety information; they reported that, after microwave therapy under nasal endoscope [32], there were seven complications in the control group (11.7%), including three cases of haemorrhage, two cases of nasal stenosis, and two cases of infection. Complications occurred in five cases (8.3%) in the group, including two cases of bleeding and infection each, and one case of nasal cavity stenosis. There was no significant difference in the incidence of complications between the two groups. They also noted that the treatment group had no obvious adverse reactions after auricular point pressing.
5. Discussion
5.1. Overview of Findings
To the best of our knowledge, there was only one previous systematic review published in 2010 on this topic [32]. Five studies were included in the previous review. Three of those were excluded by us because diagnostic criteria were absent in the original texts (Tables 3 and 4). By detailed comparison, we discovered that Rao and Han (2006) [50] in their review was Rao et al. (2005) [34] in our review. These two studies illustrate the same experiment, with the same data and same author, however, in different publication years. In other words, this was a repeated publication. We chose Rao et al. (2005) instead of Rao and Han et al. (2006) because of the more detailed test records including laboratory instrument details, dropout details, and adverse reactions details. Hence, we have two studies identical to those of the previous review [34, 36]. In the present review, we tried to update the topic based on the findings of the previous review.
We included 12 studies. The control group intervention can be classified in six categories: sham ear acupressure, conventional medicine therapy, acupuncture, electroacupuncture, Chinese medicine formula, and microwave therapy under nasal endoscope. EAP was not inferior to control group interventions (conventional medicine therapy, acupuncture, electroacupuncture, Chinese medicine formula, and microwave therapy under nasal endoscope) in terms of improving effective rate of allergic patients, symptom. However, the data extracted from 11 Chinese trials had small sample sizes and poor quality measures, according to the methodology measurement. The real EAP group was significantly greater than the sham group in terms of changes of global QoL score, scores for total nasal symptom, runny nose, and eye symptoms.
Validated questionnaire and scales such as the Quality Of Life Questionnaire are tools used to evaluate the quality of life of AR patients. The visual analogue scale is used to assess the severity of symptoms of AR. However, each has an application in included studies. Others such as quality of life score and nasal symptom scores evaluation methods can measure melioration of AR severity or disability; however, they are not widely used, despite the fact that these scales are recommended by the 2015 Clinical Guidelines.
5.2. Potential Biases in the Review Process
No ongoing trials were found. The conclusion of this review was drawn from the 12 trials, comprising a limited number of participants. More studies and high-quality trials should be included in future reviews. In addition, 3 key points that may cause potential heterogeneity may be summarized as follows:
As a noninvasive alternative, small seeds (Wang Bu Liu Xing and Vaccariae Semen) come from a plant or metal pellets on auricular points. Both are commonly used materials in EAP treatment and are effective. However, the differences between them remain unknown. In our review, Vaccariae Semen seeds applied in eleven China mainland publication trials [34–43, 45] and stainless steel pellets (1.2 mm in diameter; PELSST S/Steel Tan; Acuneeds Co., Camberwell, Victoria, Australia) were used in a two centres (Royal Melbourne Institute of Technology University (Melbourne, Australia) and Clinical Trial Clinic and Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, China) (Claire et al.) [32]. This situation might make a subtle difference in terms of efficacy. More in-depth studies on the two raw materials may be needed.
Commonly used auricular points were summarized in our review: Nei Bi (TG4), lung (CO14), kidney (CO10), spleen (CO13), adrenal gland (TG2p), external nose (TG1, 2i), wind stream (SF1, 2i), and Shenmen (TF4). Therefore, these can be regarded as commonly used EAR for AR ear points. However, in Lu et al. (2015) [39], three ear acupoints including internal nose (TG4), sympathetic (AH6a), and root of ear tragus (R2) were selected. This is very different from other studies, which may be the source of heterogeneity, because EAP is based on the meridians theory of TCM. In meridians theory, each acupoint serves a different purpose. The specificity of acupoints in morphological structure, biophysical characters, pathological reactions, acupuncture stimulation-induced responses in different brain regions, and therapeutic effects were supported by scholars [44].
Despite our use of validated effectiveness assessment criteria documents supporting trials in this review, the nonuniform standard of efficacy evaluation might influence outcomes and results (especially effectiveness rate). It might be challenging to employ the same diagnosis and effectiveness assessment criteria for each trial, as these criteria vary with each update.
6. Conclusion
Despite the positive results of some outcomes, it is premature to confirm the efficacy of EAP for treating AR. More high-quality studies are needed to validate its efficacy. There are insufficient data to state that EAP is safe and reliable due to the small number of trials reporting adverse events. Therefore, studies with larger sample sizes and rigorously designed studies are necessary to determine conclusively a definitive association between EAP and AR.
Acknowledgments
The authors thank Shuqin Liu for methodologic guidance. The funding have come from the National Natural Science Foundation of China (81473523) and National Science and Technology Pillar Program during the Twelfth Five-year Plan Period of China (2015BAI04B00) and are external supports to their organization. The URL is http://isisn.nsfc.gov.cn/egrantindex/funcindex/prjsearch-list.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
J.Z., Q.Z., and S.L. designed the study. P.L. and Q.G. conducted the literature search and identified and selected the studies. B.F. resolved any disagreements. D.L. and T.L. assessed methodologic quality and extracted data. S.L. and J.Z. performed data synthesis and analysis and drafted the manuscript. Y.S. and J.Z. revised the manuscript. All authors reviewed and approved the final version of the article.
References
- 1.Zhong J., Lai D., Zheng Y., Li G. Ma-huang-fu-zi-xi-xin decoction for allergic rhinitis: a systematic review. Evidence-Based Complementary and Alternative Medicine. 2018;2018:6. doi: 10.1155/2018/8132798.8132798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bousquet J., Van Cauwenberge P., Khaltaev N. allergic rhinitis and its impact on asthma. Journal of Allergy and Clinical Immunology. 2001;108(5 Suppl):S147–S334. doi: 10.1067/mai.2001.118891. [DOI] [PubMed] [Google Scholar]
- 3.Meltzer E. O. Allergic rhinitis. Immunology and Allergy Clinics of North America. 2016;36(2):235–248. doi: 10.1016/j.iac.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 4.Bauchau V., Durham S. R. Prevalence and rate of diagnosis of allergic rhinitis in europe. European Respiratory Journal. 2004;24(5):758–764. doi: 10.1183/09031936.04.00013904. [DOI] [PubMed] [Google Scholar]
- 5.Amizadeh M., Safizadeh H., Bazargan N., Farrokhdoost Z. Survey on the prevalence of allergic rhinitis and its effect on the quality of high school students’ life. Iranian Journal of Otorhinolaryngology. 2013;25(71):79–84. [PMC free article] [PubMed] [Google Scholar]
- 6.Danell C. S., Bergström A., Wahlgren C.-F., Hallner E., Böhme M., Kull I. Parents and school children reported symptoms and treatment of allergic disease differently. Journal of Clinical Epidemiology. 2013;66(7):783–789. doi: 10.1016/j.jclinepi.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Devillier P., Bousquet P.-J., Grassin-Delyle S., et al. Comparison of outcome measures in allergic rhinitis in children, adolescents and adults. Pediatric Allergy and Immunology. 2016;27(4):375–381. doi: 10.1111/pai.12561. [DOI] [PubMed] [Google Scholar]
- 8.Lin L., Li T., Sun M., et al. Effect of particulate matter exposure on the prevalence of allergic rhinitis in children: a systematic review and meta-analysis. Chemosphere. 2021;268 doi: 10.1016/j.chemosphere.2020.128841.128841 [DOI] [PubMed] [Google Scholar]
- 9.Meltzer E. O., Farrar J. R., Sennett C. Findings from an online survey assessing the burden and management of seasonal allergic rhinoconjunctivitis in us patients. The Journal of Allergy and Clinical Immunology: In Practice. 2017;5(3):779–789. doi: 10.1016/j.jaip.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 10.La Grutta S., Landi M., Braido F., et al. Rhinasthma-adolescents: a new quality of life tool for patients with respiratory allergy. Pediatric Allergy and Immunology. 2014;25(5):450–455. doi: 10.1111/pai.12242. [DOI] [PubMed] [Google Scholar]
- 11.Matterne U., Schmitt J., Diepgen T. L., Apfelbacher C. Children and adolescents’ health-related quality of life in relation to eczema, asthma and hay fever: results from a population-based cross-sectional study. Quality of Life Research. 2011;20(8):1295–1305. doi: 10.1007/s11136-011-9868-9. [DOI] [PubMed] [Google Scholar]
- 12.Matterne U., Apfelbacher C. Is the impact of atopic disease on children and adolescents’ health related quality of life modified by mental health? Results from a population-based cross-sectional study. Health Qual Life Outcomes. 2013;11:p. 115. doi: 10.1186/1477-7525-11-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bemanin M. H., Fallahpour M., Arshi S., Nabavi M., Yousofi T., Shariatifar A. First report of asthma prevalence in Afghanistan using international standardized methods. Eastern Mediterranean Health Journal. 2015;21(3):194–198. doi: 10.26719/2015.21.3.194. [DOI] [PubMed] [Google Scholar]
- 14.Sritipsukho P., Satdhabudha A., Nanthapisal S. Effect of allergic rhinitis and asthma on the quality of life in young Thai adolescents. Asian Pacific Journal of Allergy and Immunology. 2015;33(3):222–226. doi: 10.12932/AP0548.33.3.2015. [DOI] [PubMed] [Google Scholar]
- 15.Valls-Mateus M., Marino-Sanchez F., Ruiz-Echevarría K., et al. Nasal obstructive disorders impair health-related quality of life in adolescents with persistent allergic rhinitis: a real-life study. Pediatric Allergy and Immunology. 2017;28(5):438–445. doi: 10.1111/pai.12724. [DOI] [PubMed] [Google Scholar]
- 16.Batlles-Garrido J., Torres-Borrego J., Rubí-Ruiz T., et al. Prevalence and factors linked to allergic rhinitis in 10 and 11-year-old children in Almería. Isaac Phase II, Spain. Allergologia et Immunopathologia. 2010;38(3):135–141. doi: 10.1016/j.aller.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 17.Devillier P., Bousquet J., Salvator H., Naline E., Grassin-Delyle S., de Beaumont O. In allergic rhinitis, work, classroom and activity impairments are weakly related to other outcome measures. Clinical and Experimental Allergy. 2016;46(11):1456–1464. doi: 10.1111/cea.12801. [DOI] [PubMed] [Google Scholar]
- 18.Montefort S., Ellul P., Montefort M., Caruana S., Agius Muscat H. A decrease in the prevalence and improved control of allergic conditions in 13- to 15-yr-old Maltese children (isaac) Pediatric Allergy and Immunology. 2011;22(1pt2):e107–e111. doi: 10.1111/j.1399-3038.2010.01058.x. [DOI] [PubMed] [Google Scholar]
- 19.Kakaje A., Alhalabi M. M., Alyousbashi A., Hamid A., Hosam Aldeen O. Allergic rhinitis and its epidemiological distribution in Syria: a high prevalence and additional risks in war time. BioMed Research International. 2020;2020:9. doi: 10.1155/2020/7212037.7212037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zar H. J., Ehrlich R. I., Workman L., Weinberg E. G. The changing prevalence of asthma, allergic rhinitis and atopic eczema in african adolescents from 1995 to 2002. Pediatric Allergy and Immunology. 2007;18(7):560–565. doi: 10.1111/j.1399-3038.2007.00554.x. [DOI] [PubMed] [Google Scholar]
- 21.Adamia N., Jorjoliani L., Manjavidze N., Ubiria I., Saginadze L. Psycho-emotional Characteristics of the adolescents with allergic rhinitis. Georgian Med News. 2015;243:38–42. [PubMed] [Google Scholar]
- 22.Kwon J. A., Lee M., Yoo K. B., Park E. C. Does the duration and time of sleep increase the risk of allergic rhinitis? Results of the 6-year nationwide korea youth risk behavior web-based survey. PLoS One. 2013;8(8) doi: 10.1371/journal.pone.0072507.e72507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim M.-S., Lee C. H., Sim S., Hong S. K., Choi H. G. Physical activity, sedentary habits, sleep, and obesity are associated with asthma, allergic rhinitis, and atopic dermatitis in Korean adolescents. Yonsei Medical Journal. 2017;58(5):1040–1046. doi: 10.3349/ymj.2017.58.5.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ng D. K., Chan C.-h., Ng E. P. Natural history of snoring in Hong Kong adolescents. Journal of Paediatrics and Child Health. 2014;50(8):596–604. doi: 10.1111/jpc.12607. [DOI] [PubMed] [Google Scholar]
- 25.Sogut A., Yilmaz O., Dinc G., Yuksel H. Prevalence of habitual snoring and symptoms of sleep-disordered breathing in adolescents. International Journal of Pediatric Otorhinolaryngology. 2009;73(12):1769–1773. doi: 10.1016/j.ijporl.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 26.Song Y., Wang M., Xie J., et al. Prevalence of allergic rhinitis among elementary and middle school students in changsha city and its impact on quality of life. The Journal of Laryngology and Otology. 2015;129(11):1108–1114. doi: 10.1017/s0022215115002492. [DOI] [PubMed] [Google Scholar]
- 27.Chirakalwasan N., Ruxrungtham K. The linkage of allergic rhinitis and obstructive sleep apnea. Asian Pacific Journal of Allergy and Immunology. 2014;32(4):276–286. [PubMed] [Google Scholar]
- 28.Bousquet J., Khaltaev N., Cruz A. A., et al. Allergic rhinitis and its impact on asthma (aria) 2008 update (in collaboration with the world health organization, Ga(2)Len and allergen) Allergy. 2008;63(Suppl 86):8–160. doi: 10.1111/j.1398-9995.2007.01620.x. [DOI] [PubMed] [Google Scholar]
- 29.Li X.-R., Zhang Q.-X., Liu M., et al. Catgut implantation at acupoints for allergic rhinitis: a systematic review. Chinese Journal of Integrative Medicine. 2014;20(3):235–240. doi: 10.1007/s11655-014-1748-z. [DOI] [PubMed] [Google Scholar]
- 30.Zeng H. Y. Clinical effect of shenling baizhu powder combined with ear acupressure pills on allergic rhinitis. Journal of Contemporary Chinese Medicine. 2020;27(16):186–189. [Google Scholar]
- 31.Ying X. Efficacy of the Guizhi decoction plus auricular point on clinical symptoms in patients with allergic rhinitis. Clinical Journal of Chinese Medicine. 2019;11(32):28–32. [Google Scholar]
- 32.Zhang C. S., Xia J., Zhang A. L., et al. Ear acupressure for perennial allergic rhinitis: a multicenter randomized controlled trial. American Journal of Rhinology and Allergy. 2014;28(4):E152–e157. doi: 10.2500/ajra.2014.28.4081. In English. [DOI] [PubMed] [Google Scholar]
- 33.McInnes M. D. F., Moher D., Thombs B. D. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the prisma-dta statement (vol 319, pg 388, 2018) Jama-Journal of the American Medical Association. 2019;322(20):p. 2026. doi: 10.1001/jama.2017.19163. In English. [DOI] [PubMed] [Google Scholar]
- 34.Rao Y. Q. Contrast of the Observation of the Acupuncture and Auricular Point Pression’s Curative Effect on Perennial Allergre Rhinitis and Their Effect on Serum Ig-E, IFN-γFNIL-4. Shandong, China: Shandong University of TCM; 2005. [Google Scholar]
- 35.Han M., Wang L. M., Du L., Liu F. F. Observation on effect of ear point pressing beans in the treatment of weak lung and cold biqiu. Journal of Jilin TCM. 2006;26(2):p. 53. [Google Scholar]
- 36.Ye Q. Q., Luo T., Xia W. Observation of 40 cases of allergic rhinitis treated by acupuncture and auricular point pressing. Journal of Practical Traditional Chinese Medicine. 2008;24(2):p. 115. [Google Scholar]
- 37.Ou Y., Yu L. Clinical observation of ear pressure combined with oral cetirizine in the treatment of 30 cases of moderate to severe allergic rhinitis. Jiangsu Traditional Chinese Medicine. 2012;44(9):59–60. [Google Scholar]
- 38.Yuan K., Tang J. Q., Jiang Z. X., Du H., Peng L. Y. Clinical study on auricular point sticking combined with Lifuting to treat allergic rhinitis in children. Hubei Journal of TCM. 2013;35(2):67–68. [Google Scholar]
- 39.Lu D. The Clinical Study on the Effect of Allergic Rhinitis by Electroacupuncture Fitted with Ear Acupoint Pressing. Guangzhou, China: Guangzhou University of TCM; 2015. [Google Scholar]
- 40.Yuan N., Zhang N., Liu C., Zhang C., Che X. H. Professor JI Qingshan in treatment of allergic rhinitis with auricular needle acupuncture. Journal of Changchun University of Chinese Medicine. 32(2):231–233. Mar-2016) [Google Scholar]
- 41.Liao C. The Clinical Observation and Syndrome Type Analysis of Allergic Rhinitis by Pressing Auricular Points with Bean Combined with Xinqin Particles. Chengdu, China: Chengdu University of TCM; 2016. [Google Scholar]
- 42.Li L., Zhang L., Yang H. Z. Clinical observation of auricular point sticking pressure in the treatment of allergic rhinitis with lung spleen qi deficiency syndrome. Journal of Basic Chinese Medicine. 2018;24(6):815–817. [Google Scholar]
- 43.Zhao Y. Clinical Observation on the Treatment of Allergic Rhinitis of Lung and Kidney Deficiency with Sheti Zhiqiu and Auricular Points. Chengdu, China: Chengdu University of TCM; 2019. [Google Scholar]
- 44.Li C. H., Xu D. Z., Liu Y. Q., et al. [Progress of researches on specificity of acupoints in China in recent 10 Years] Zhen Ci Yan Jiu. 2013;38(4):324–329. [PubMed] [Google Scholar]
- 45.Rao Y. Q., Han N. Y. [Therapeutic effect of acupuncture on allergic rhinitis and its effects on immunologic function] Zhongguo Zhen Jiu. 2006;26(8):557–560. [PubMed] [Google Scholar]
- 46.Lei C., Zhen D., Wei K., et al. Guidelines for the diagnosis and treatment of allergic rhinitis (2015,Tianjin) International Journal of Otolaryngology - Head and Neck Surgery. 2015;51(1):6–24. [Google Scholar]
- 47.Zhi G., Zhen D. Diagnosis and treatment of allergic rhinitis and recommended protocol (2004,Lanzhou) Chinese Journal of Otolaryngology - Head and Neck Surgery’s. 2004;3:8–9. [Google Scholar]
- 48.Diagnostic criteria and therapeutic evaluation criteria of allergic rhinitis (1997, modified, Haikou) Chinese Journal of Otolaryngology - Head and Neck Surgery’s. 1997;3:3–5. [Google Scholar]
- 49.Higgins J. P., Thompson S. G. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 50.Guidelines for the diagnosis and treatment of allergic rhinitis (2009, Wuyishan) Chinese Journal of Otolaryngology - Head and Neck Surgery’s. 2009;12:977–978. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


