Current commercially available methods for reliably detecting antibodies against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remain expensive and inaccessible due to the need for whole-blood collection by highly trained phlebotomists using personal protective equipment (PPE). We have evaluated an antibody detection approach using the OraSure Technologies oral antibody collection device (OACD) and their proprietary SARS-CoV-2 total antibody detection enzyme-linked immunosorbent assay (ELISA).
KEYWORDS: ELISA, SARS-CoV-2, antibodies, oral fluid, rapid test, saliva, serology
ABSTRACT
Current commercially available methods for reliably detecting antibodies against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remain expensive and inaccessible due to the need for whole-blood collection by highly trained phlebotomists using personal protective equipment (PPE). We have evaluated an antibody detection approach using the OraSure Technologies oral antibody collection device (OACD) and their proprietary SARS-CoV-2 total antibody detection enzyme-linked immunosorbent assay (ELISA). We found that the OraSure test for total antibody detection in oral fluid had comparable sensitivity and specificity to commercially available serum-based ELISAs for SARS-CoV-2 antibody detection while allowing for a more accessible form of specimen collection with the potential for self-collection.
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has had a severe impact on populations and economies worldwide (1). While the relationship between antibodies and their protective role against reinfection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is under investigation, it has been shown that antibodies consistently develop as part of the immune response against the virus in some, if not most, infected individuals (2). Thus, reliable tests for detecting antibodies against SARS-CoV-2 are crucial to monitoring global COVID-19 disease spread, SARS-CoV-2 vaccine development and efficacy, and both the short- and long-term immune responses to SARS-CoV-2.
Antibodies are typically detected in patient serum. Serum is derived from whole blood, which must be collected by a trained phlebotomist (3). This process can be time-consuming and costly and can expose the phlebotomist to an infectious respiratory agent, which is a concern during the current COVID-19 pandemic. Phlebotomists must be protected with personal protective equipment (PPE), such as N95 masks, face shields, and gloves, and such equipment is of limited availability during the pandemic (4). Thus, a rapid noninvasive technology for self-collection is needed to improve access to antibody testing.
Numerous studies have successfully used patient saliva, instead of serum, to detect antibodies against SARS-CoV-2 (5–8), presenting a less-invasive medium in which antibodies can be detected. Some of these studies have relied on processes involving plasmonic gold substrates (5) and multiplexed magnetic microparticle based immunoassays (8) which do not scale up well due to time-consuming protocols and the need for expensive equipment. Alternatively, enzyme-linked immunosorbent assays (ELISAs) allow for high-throughput sample processing. We previously assessed the accuracy of the emergency use authorization (EUA)-approved EuroImmun SARS-CoV-2 ELISA (IgG) kit using saliva specimens collected with an in-house mouthwash formulation instead of serum, finding 84.2% sensitivity and 100% specificity (9). Similarly, Isho et al. profiled antibody responses by the use of antibody kits designed in-house in both serum and saliva specimens which were collected using Salivette saliva collection tubes, finding 89% sensitivity to spike (S) proteins and 85% sensitivity to receptor-binding domain (RBD) proteins (specificity not given) (7). Despite the successes of both of those studies, neither achieved the specifications recommended by guidance from the Food and Drug Administration (FDA), that is, greater than 90% sensitivity and 100% specificity.
The need for a noninvasive SARS-CoV-2 antibody test that could be mass-produced for widespread testing and maintain testing specifications recommended by the FDA led us to a collaboration with OraSure Technologies. OraSure Technologies has previously demonstrated the capacity of their oral specimen collection device (OSCD) to collect and store oral fluid antibodies against human immunodeficiency virus type 1 (HIV-1) (10). Their oral antibody collection device (OACD), adapted for improved antibody collection for antibodies against SARS-CoV-2, collects oral fluid between the gums and cheeks using an absorbent pad containing salts and citric acid. This region of the mouth contains an antibody-rich fluid known as gingival crevicular fluid (8). Thus, by collecting from this region, the OACD collects an oral fluid specimen richer in antibodies than saliva alone. In addition to adapting the use of their device for better collection of oral specimens, OraSure Technologies developed an ELISA kit for detection of total antibodies (IgG, IgM, IgA) against SARS-CoV-2 in specimens collected using the OACD (11, 12). At the time of submission of this article, OraSure Technologies was in the process of seeking FDA EUA approval for the ELISA. Here, we used OraSure Technologies OACDs and their ELISA kit to detect antibodies in oral fluids and compared the findings to results obtained with paired participant serum specimens evaluated on two serum-based SARS-CoV-2 antibody detection ELISAs.
MATERIALS AND METHODS
Human serum and oral fluid specimen collection. (i) Post-COVID-19 serum and oral fluid specimens.
Clinical specimens were collected under University of California, Los Angeles (UCLA), Institutional Review Board (IRB)-approved study protocol IRB no. 20-000703. The UCLA IRB determined that the protocol was of minimal risk and that verbal informed consent was sufficient for the research under 45 CFR 46.117(c). The study team complied with all UCLA policies and procedures, as well as with all applicable federal, state, and local laws regarding the protection of human subjects in research as stated in the approved IRB. For this study, we obtained three specimens: oral fluid obtained for viral PCR testing, blood obtained via venipuncture, and one oral fluid specimen obtained through OraSure Technologies’ OACD for antibody testing.
(ii) Oral fluid swab for viral RNA.
This was obtained according to the reported guidelines for Curative’s FDA EUA-approved oral fluid COVID-19 test (13). Briefly, participants coughed hard three times while shielding their cough via mask and/or coughing into the crook of their elbow. They then self-swabbed the inner side of their cheeks, along the top and bottom gums, under the tongue, and, finally, on the top of the tongue, to gather a sufficient amount of oral fluid on the swab. Swabs were placed in a tube containing RNA Shield and transported at room temperature to the High-Complexity Clinical Laboratory Improvement Amendments (CLIA)-certified laboratory in San Dimas, CA, for processing by real-time quantitative PCR (RT-qPCR). Samples were manually plated onto 96-well deep-well plates, and then RNA was manually extracted. The samples were then transferred to master mix and run on a Bio-Rad CFX Thermocycler. A positive result for viral RNA was determined as a cycle threshold (CT) value below 35.
(iii) Blood sampling.
Participants underwent a standard venipuncture procedure. Briefly, licensed phlebotomists collected a maximum of 15 ml whole blood into 3 red-top SST tubes (Becton, Dickinson, catalog no. 367988). Once collected, the specimen was left at ambient temperature for 30 to 60 min to coagulate and then was centrifuged at 2,200 to 2,500 rpm for 15 min at room temperature. Specimens were then placed on ice for no more than 6 h until they were delivered to the laboratory site, where the serum was aliquoted to appropriate volumes for storage at −80°C until use.
(iv) OraSure oral fluid specimen collection.
OraSure oral antibody collection devices (OACD) (item number 3001-3442-70; OraSure, USA) were used as instructed (11, 14). Each pad was brushed 5 times on each side of the lower and upper gums (lower left, lower right, upper left, and upper right gums for a total of 20 times) and then held between the lower gum on one side and the cheek for 2 to 5 min. The pad was then placed into the storage tube, with the provided storage solution. Specimens were kept on ice until they reached the lab. The specimens were processed as recommended by the manufacturer before being aliquoted and stored at −80°C until use (15).
Serum ELISAs.
EuroImmun’s FDA EUA-approved SARS-CoV-2 IgG ELISA for serum (catalog no. EI 2606–9620, EuroImmun, NJ, USA) targeting spike (S) protein was run according to the manufacturer-provided protocol on a Thunderbolt (Gold Standard Diagnostics, Davis, CA) automated instrument (16). Briefly, serum was diluted 1:101 in each well with the provided sample buffer and then incubated at 37°C for 1 h. Sample wells were washed three times with a provided wash buffer (10× dilution with double-distilled water [ddH2O] [0.35 ml per well) before the provided conjugate solution was added (0.1 ml per well) and were then incubated at 37°C for 30 min. After a second wash step, the provided substrate solution was added (0.1 ml per well) and incubated at ambient temperature for 30 min. The provided stop solution was then added (0.1 ml per well) and absorbance of sample wells measured immediately at 450 nm and 630 nm, with output reports generated with the optical density (OD) at 630 nm subtracted from the OD at 450 nm.
Data were then analyzed as recommended by the manufacturer and results reported as a ratio (equation 1). Specimens whose ratio exceeded or was equal to 1.1 were considered positive, while specimens with a ratio greater than 0.8 and less than 1.1 were considered equivocal and specimens with a ratio less than or equal to 0.8 were considered negative. Specimens with ratios in the equivocal range were recommended to be rerun, but this did not apply to any specimens in this study.
Determination of specimen-to-cutoff ratio (S/CO ratio) as defined by the manufacturer by dividing specimen OD by the average OD of the calibrators was performed using equation 1 as follows:
| (1) |
Gold Standard Diagnostics (GSD) SARS-CoV-2 IgG ELISA for serum (catalog no. GSD01-1028 IgG; Gold Standard Diagnostics, Davis, USA) targeting nucleocapsid (N) protein was run according to the manufacturer-provided protocol on a Thunderbolt (Gold Standard Diagnostics, Davis, CA) automated instrument. Briefly, serum was diluted 1:100 in each well with the provided sample buffer and then incubated at room temperature for 30 min. Sample wells were washed three times with a provided wash buffer (20× dilution with ddH2O, 0.3 ml per well) before the provided conjugate solution was added (0.1 ml per well) and were then incubated at ambient temperature for 30 min. After a second wash step, the provided substrate solution was added (0.1 ml per well) and incubated at ambient temperature for 30 min. The provided stop solution was then added (0.05 ml per well) and absorbance of sample wells measured immediately at 450 nm and 630 nm, with output reports generated with optical density (OD) at 630 nm subtracted from OD at 450 nm. Data were then analyzed as recommended based on a correction factor (specific to each kit) and a mathematical formula provided by the manufacturer (equations 2 and 3). Specimens whose ratio exceeded or was equal to 11 were considered positive, while specimens with a ratio greater than 8 and less than 11 were considered equivocal and specimens with a ratio less than or equal to 8 were considered negative. Specimens with ratios in the equivocal range were recommended to be rerun. Specimens producing equivocal ratios on the GSD SARS-CoV-2 IgG ELISA in this study were rerun on the EuroImmun SARS-CoV-2 IgG ELISA.
Determination of specimen positivity cutoff value as an average of the calibrator values multiplied by a lot-specific correction factor was performed using equation 2 as follows:
| (2) |
Determination of the specimen-to-cutoff (S/CO) ratio as defined by the manufacturer was performed using equation 3 by dividing specimen OD by the positivity cutoff value and multiplying by 10 as follows:
| (3) |
Oral fluid ELISA.
OraSure Technologies SARS-CoV-2 Total Antibody ELISA for oral fluid specimen (item number 3001-3317-70, catalog no. 1125SB) targeting coronavirus spike protein antigens S1 and S2 was run manually according to the manufacturer-provided protocol (12). A 25-μl volume of provided sample diluent buffer was added to the chosen wells of the plate followed by 100 μl of each specimen. Specimens were incubated at ambient temperature for 1 h. Sample wells were washed six times with a provided wash buffer (20× dilution with ddH2O, 0.35 ml per well), before the provided conjugate solution was added (0.1 ml per well) and incubated at ambient temperature for 1 h. After a second wash step, the provided substrate solution was added (0.1 ml per well) and incubated at ambient temperature for 30 min. The provided stop solution was then added (0.1 ml per well) and absorbance of sample wells measured immediately at 450 nm and 630 nm, with output reports generated with OD at 630 nm subtracted from OD at 450 nm.
Data were analyzed as recommended by the manufacturer and results reported as a specimen-to-cutoff (S/CO) ratio (equation 4). Specimens whose ratio was equal to or exceeded 1.0 were considered positive, while specimens with a ratio greater than 0.8 and less than 1.0 were considered equivocal and specimens with a ratio less than or equal to 0.8 were considered negative. Specimens with ratios in the equivocal range were recommended to be rerun, but this did not apply to any specimens in this study.
Determination of specimen-to-cutoff (S/CO) ratio was performed using equation 4 based on specimen OD divided by the averaged OD of the cutoff calibrators as follows:
| (4) |
ELISA automation.
Using an automated Dynex DSX 4-plate ELISA processing system, we developed a quick two-step automated method for SARS-CoV-2 antibody detection involving (i) centrifugation of the OACDs in a secondary tube to transfer oral fluid from the device and (ii) processing of the collected saliva specimens with OraSure Technologies SARS-CoV-2 total antibody ELISA plates on the DSX system.
Drive-through site data collection.
As a part of normal drive-through site operation for sample collection for the FDA EUA-approved SARS-CoV-2 RNA diagnostic test (Curative Inc.), the number of individuals who pass through the site and perform self-collection of oral fluid for RT-qPCR SARS-CoV-2 viral detection under health care worker supervision are recorded. These numbers are distributed internally to allow optimization of site staff procedures and to improve the consumer’s experience, and the data on the number of cars and the number of individuals in them who are tested are made available to all interested Curative Inc. employees. Using these data, we have estimated the number of individuals who could perform self-collection of oral fluid for antibody analysis under health care worker supervision using the OACD in a similar time frame.
Statistical analysis.
Receiver operating characteristic (ROC) curves were generated in GraphPad Prism (GraphPad Prism Version 8.4.3; San Diego, USA), with a 95% confidence interval. Area under the curves was also calculated.
Data availability.
The data that support the findings of this study are available from us upon reasonable request.
RESULTS
To determine whether we could adequately detect antibodies against SARS-CoV-2 in oral fluid self-collected under observation by a health care worker using the OraSure OACD (see the schematic in Text S1 in the supplemental material), we evaluated paired serum and oral fluid samples from individuals who had undergone SARS-CoV-2 oral fluid molecular RNA testing (Fig. 1). Participant specimens were collected with informed consent from a diverse population of participants (Table 1). Note that the antibody detection kits described here do not claim to quantify antibody in the sample but instead aim to provide a binary indicator of antibody presence. Thus, we cannot derive any correlations here between antibody signal and any other factor but can use the results to determine the presence or absence of an antibody response.
FIG 1.
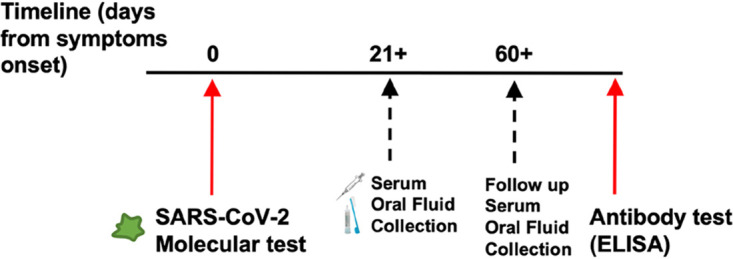
Timeline of sample collection, methods, and sample metrics from clinical trial participants.
TABLE 1.
Demographics of our cohort of clinical samples and days post-symptom onset of our positive participant samples
| Parameter | No. (%) of samples |
|---|---|
| Gender (n = 147) | |
| Female | 88 (59.9) |
| Male | 59 (40.1) |
| Age (yr) (n = 147) | |
| 20–29 | 51 (34.7) |
| 30–39 | 29 (19.7) |
| 40–49 | 19 (12.9) |
| 50–59 | 13 (8.8) |
| 60–69 | 23 (15.7) |
| 70+ | 12 (8.2) |
| Original PCR status (n = 147) | |
| Negative | 81 (55.1) |
| Positive | 66 (44.9) |
| No. of days post-symptom onset (n = 66) | |
| 21–40 | 36 (54.5) |
| 41–60 | 17 (25.8) |
| 60+ | 13 (19.7) |
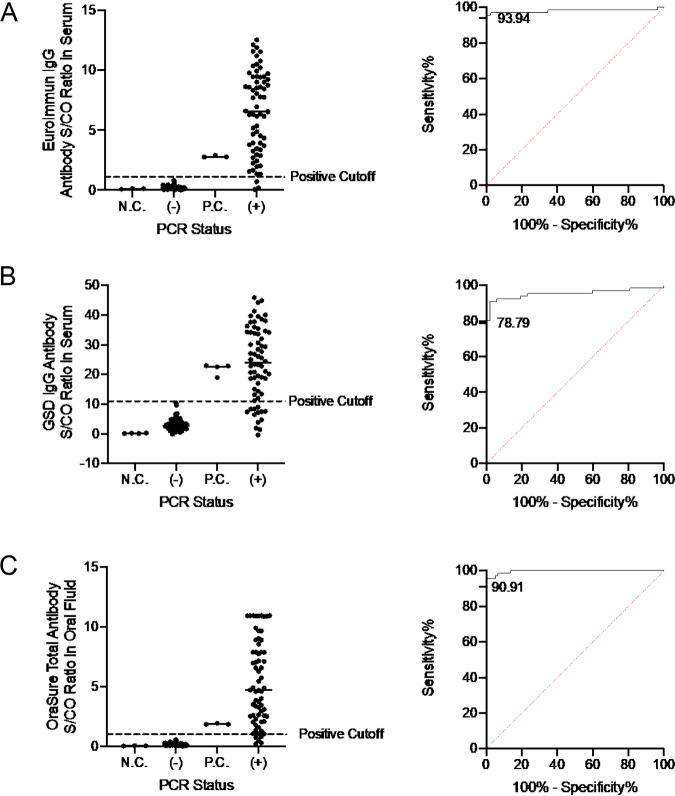
Participants were tested for SARS-CoV-2 RNA using Curative’s FDA EUA-approved RT-PCR SARS-CoV-2 RNA diagnostic test and received either a positive or negative diagnosis (13). For symptomatic participants who received a positive SARS-CoV-2 RNA diagnosis, serum and oral fluid samples were collected at least 21 but not more than 100 days after the date of reported symptom onset to ensure adequate time for antibody seroconversion (2). We tested participant serum specimens by the use of the EuroImmun SARS-CoV-2 IgG ELISA kit (16) and the Gold Standard Diagnostic (GSD) SARS-CoV-2 ELISA for IgG (https://www.goldstandarddiagnostics.com/home/products/covid-19-elisa-assays/gsd-sars-cov-2-elisa/gsd-sars-cov-2-elisa-igg/), which detect antibodies against the spike (S) and nucleocapsid (N) protein, respectively, to determine whether the participants expressed IgG antibodies in serum against SARS-CoV-2 by the use of previously described methods (9) (Fig. 2A and B). Based on manufacturer-provided cutoff values, the data obtained with this sample set were found to be 93.94% sensitive and 100% specific on the EuroImmun kit and 78.79% sensitive and 100% specific on the GSD kit. Participants whose serum had detectable antibodies on either the EuroImmun or the GSD kit were selected for oral fluid analysis. Paired oral fluid samples collected using the OraSure OACD from 66 SARS-CoV-2 RNA-positive and antibody-positive participants and 81 SARS-CoV-2 RNA-negative and antibody-negative participants was evaluated by the use of the OraSure total antibody ELISA. The OraSure total antibody ELISA detects antibodies against the SARS-CoV-2 S1 and S2 antigens of the S protein of SARS-CoV-2. Antibodies were detected in 60 (90.9% sensitivity) of 66 serum antibody-positive participant specimens and zero (100% specificity) of 81 serum-antibody-negative participant specimens (Fig. 2C).
FIG 2.
Detection of IgG antibodies against SARS-CoV-2 in participant-derived serum and oral fluid samples collected from participants who previously tested negative or positive for COVID-19 by an oral-fluid PCR test. Receiver operating characteristic (ROC) curves represent sensitivity and specificity of each test. Manufacturer-provided cutoff values are represented by a horizontal dashed line. N.C. = negative control; P.C. = positive control. (A) With an S/CO ratio cutoff of 1.1, the EuroImmun COVID-19 antibody detection kit was 93.94% sensitive and 100% specific with an area under the ROC curve (AUC) of 0.9798. (B) The Gold Standard Diagnostics COVID-19 antibody detection kit was 78.79% sensitive and 100% specific with an AUC of 0.9543. (C) With an S/CO ratio cutoff of 1.0, the OraSure Technologies COVID-19 ELISA kit was 90.91% sensitive and 100% specific with an AUC of 0.9962.
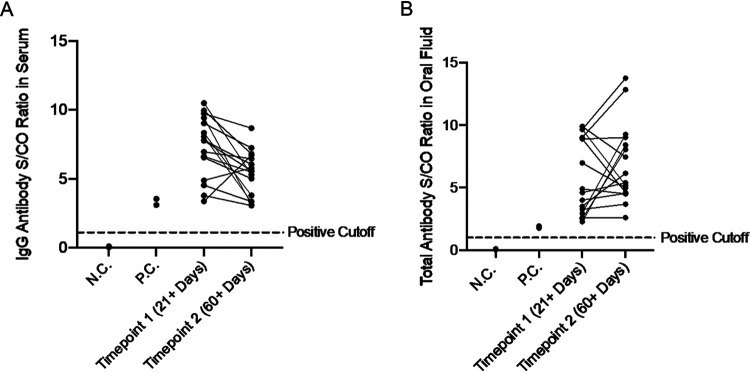
We further investigated how well the OACD and OraSure total antibody ELISA performed in monitoring paired specimens collected from the same participants at later time points postinfection. To evaluate this, we followed up with the 66 participants with positive results and collected paired oral fluid and serum specimens from 16 of them at least 60 days after the original collection date. We found that the performance of the oral fluid-based total antibody ELISA from OraSure Technologies was statistically equivalent to that seen with the serum-based IgG antibody ELISA from EuroImmun, with all positive specimens passing the antibody detection cutoff after both 21+ days and 60+ days (Fig. 3). Only the FDA EUA-approved SARS-CoV-2 antibody detection kit from EuroImmun was used for comparison in this study because it shares common antigens from the S protein to capture antibodies with the OraSure total antibody ELISA plates.
FIG 3.
(A) Detection of antibodies against SARS-CoV-2 using the EuroImmun COVID-19 antibody detection kit in participant-derived serum samples collected from participants who previously tested positive for COVID-19 by an oral-fluid PCR test both 21+ days post-symptom onset and 60+ days post-symptom onset. All samples passed the positive cutoff value of 1.1 set by the manufacturer (represented by the horizontal dashed line). N.C. = negative control; P.C. = positive control. ROC analysis of this data set in serum resulted in 100% sensitivity and 100% specificity with an area under the ROC curve (AUC) of 1. (B) Detection of antibodies against SARS-CoV-2 in oral fluid samples collected using the OraSure Technologies oral fluid specimen collection device from the same participants whose serum was tested. The manufacturer-provided positive cutoff value of 1.0 is represented by the dotted line. N.C. = negative control; P.C. = positive control. ROC analysis of this data set in oral fluid revealed 100% sensitivity and 100% specificity with the manufacturer-provided cutoff value of 1.0 for total antibody units and an AUC of 1.
To evaluate the potential time and cost savings of using the OACD for antibody detection instead of traditional serum-based methods, we estimated that a trained phlebotomist operating at a full-capacity drive-through center can collect and process blood serum from only ∼40 patients in a 5-h period, resulting in collection of one patient specimen per 7.5 min. Because oral fluid can potentially be self-collected using the OACD, face-to-face specimen collection time can be eliminated. This dramatically reduces the amount of time needed for collection of each specimen, leading us to estimate that we can collect devices from ∼1,000 patients in a similar drive-through setting over the same 5-h period, resulting in collection of one specimen in approximately 0.3 min. Note that this time does not include the actual time for collection of the sample, which we are assuming individuals would perform under health care worker supervision while they are waiting in the drive-through line, thus highlighting the dramatic benefit of self-collected oral samples. This represents an approximately 25-fold increase in sample collection throughput versus traditional blood serum sample collection in the same time frame (Fig. 4).
FIG 4.
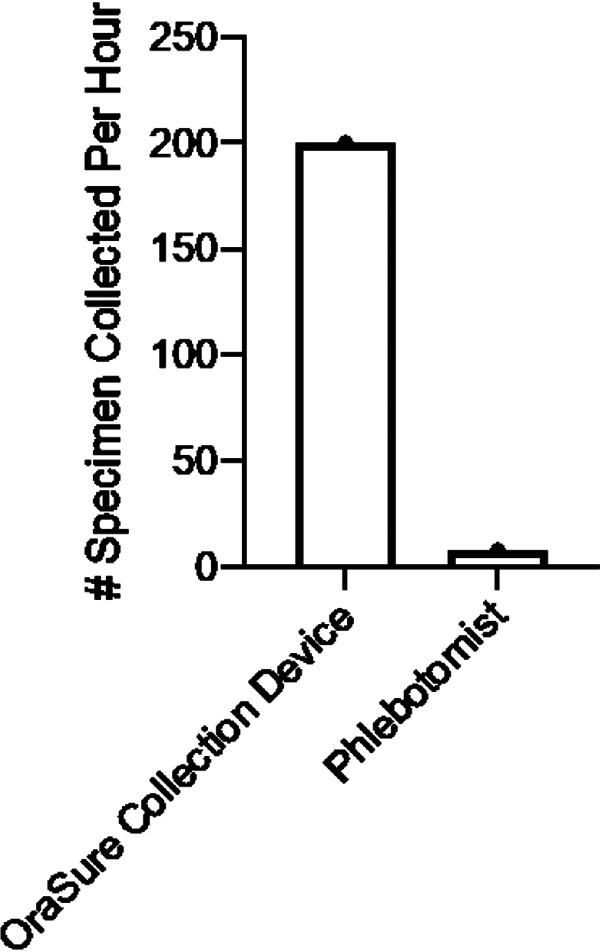
Number of antibody specimens which can be collected in a drive-through testing center per hour. Oral fluid specimens (200/h) are able to be observed after self-collection using the OraSure OACD and simply handed off to a test site employee, while blood serum specimens (8/h) must be collected through direct contact with a phlebotomist, thus highlighting the benefit of testing by self-collection.
DISCUSSION
While antibody testing has previously been limited by the requirement of trained personnel for specimen collection, we have evaluated here a technology for noninvasive self-collection which is able to be produced at scale appropriate for widespread SARS-CoV-2 antibody testing. By allowing patients to self-collect their samples, the OACD eliminates the need for trained phlebotomists to collect serum specimens, reducing requirements of time, money, and personnel. On the basis of the test efficacy and savings afforded by this method of antibody detection, OraSure Technologies has developed a testing process that is more accessible and affordable than what is currently available through serum-based testing.
Oral fluid and mucosal antibodies comprise the first line of defense against a respiratory virus, and such antibodies are known to typically contribute to sterilizing immunity by neutralizing the virus prior to infection (17). This neutralization results in reductions in both viral load and impact of subsequent infection, further highlighting the importance of antibody detection and monitoring in oral fluid specimens. Although the results of this study have demonstrated the persistence of antibodies against SARS-CoV-2 in oral fluid of convalescent humans, there are limitations to consider and further improvements that could be made to optimize oral fluid-based antibody detection.
Human error must always be considered as a factor when allowing test specimens to be self-collected as we have suggested. We acknowledge that there is a chance that an individual would be unable to collect an accurately representative oral fluid sample through self-collection, potentially leading to false-negative results, but this possibility is mitigated in part by having a trained health care worker observe the collection.
Additionally, it must also be considered that although the antigens used by OraSure Technologies and those used by EuroImmun are taken from the same component of the SARS-CoV-2 protein structure, each is proprietary and the two may have differences which could lead to variations in test efficacy. Both serum-based kits are also advertised as IgG detection kits, while that of OraSure Technologies is advertised as a total antibody kit (IgA, IgG, and IgM), which may result in a test that is more sensitive at earlier time points in the trajectory of antibody development. Thus, the comparison of this oral fluid-based test to those serum-based tests is not perfect but does provide a good sense of how the oral fluid-based test compares to commercially available and FDA EUA-approved serum-based tests. Further testing to evaluate how the OraSure Technologies COVID-19 total antibody ELISA performs with paired serum samples compared to serum-based tests might illuminate the impact of some of these differences.
Despite these limitations, the OACD, when used with the SARS-CoV-2 total antibody ELISA kit developed by OraSure Technologies, achieved sensitivity and specificity which were statistically equivalent to those achieved with the commercially available serum-based ELISAs tested (9). This represents a unique and highly successful advancement in antibody detection technology. As we move closer to the development and implementation of a successful vaccine against SARS-CoV-2, there may be a greater need for reliable methods for monitoring antibody production on a large scale and over time. This antibody detection system allows us to overcome the limitations presented by currently administered serum antibody tests, increasing accessibility to antibody testing and enabling a better understanding of the trends of temporal immune response against this virus.
Supplementary Material
ACKNOWLEDGMENTS
We thank Joseph Kapcia III, Cedie Bagos, Aaron Angel, Marilisa Santa-Cruz, and Matthew Geluz from Curative Inc. as well as Kerry Phillips, Toral Zaveri, and Matthew Sullivan from OraSure Technologies.
M.A.M. designed and ran experiments, analyzed and interpreted data, and drafted the manuscript; P.C. automated the experimental system and drafted the manuscript; A.M. and S.D. analyzed and interpreted data; F.T. and V.I.S. conceptualized the project; A.I. designed experiments, oversaw data collection and analysis, edited the manuscript, and maintained correspondence with OraSure Technologies for the duration of these experiments.
All of us are, or were at the time of research, employed by Curative Inc., a COVID-19 diagnostics company. F.T. and V.I.S. have partial ownership of Curative Inc. Curative Inc. does not have conflicts of interest with OraSure Technologies to disclose.
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.McKibbin W, Fernando R. 2020. The economic impact of COVID-19, p 45–53. In Economics in the time of COVID-19. CEPR Press, London, United Kingdom. [Google Scholar]
- 2.Long QX, Liu BZ, Deng HJ, Wu GC, Deng K, Chen YK, Liao P, Qiu JF, Lin Y, Cai XF, Wang DQ, Hu Y, Ren JH, Tang N, Xu YY, Yu LH, Mo Z, Gong F, Zhang XL, Tian WG, Hu L, Zhang XX, Xiang JL, Du HX, Liu HW, Lang CH, Luo XH, Wu SB, Cui XP, Zhou Z, Zhu MM, Wang J, Xue CJ, Li XF, Wang L, Li ZJ, Wang K, Niu CC, Yang QJ, Tang XJ, Zhang Y, Liu XM, Li JJ, Zhang DC, Zhang F, Liu P, Yuan J, Li Q, Hu JL, Chen J, Huang AL. 2020. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med 26:845–848. doi: 10.1038/s41591-020-0897-1. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 2020. Interim guidelines for COVID-19 antibody testing: current status of antibody testing in the United States: antigenic targets. CDC. https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antibody-tests-guidelines.html#anchor_1590280385631.
- 4.Center for Health Security. 2020. Serology testing for COVID-19. Johns Hopkins, Baltimore, MD. [Google Scholar]
- 5.Liu T, Hsiung J, Zhao S, Kost J, Sreedhar D, Hanson CV, Olson K, Keare D, Chang ST, Bliden KP, Gurbel PA, Tantry US, Roche J, Press C, Boggs J, Rodriguez-Soto JP, Montoya JG, Tang M, Dai H. 29 October 2020, posting date. Quantification of antibody avidities and accurate detection of SARS-CoV-2 antibodies in serum and saliva on plasmonic substrates. Nat Biomed Eng doi: 10.1038/s41551-020-00642-4. [DOI] [PubMed] [Google Scholar]
- 6.Varadhachary A, Chatterjee D, Garza J, Garr RP, Foley C, Letkeman AF, Dean J, Haug D, Breeze J, Traylor R, Malek A, Nath R, Linbeck IIL. 2020. Salivary anti-SARS-CoV-2 IgA as an accessible biomarker of mucosal immunity against COVID-19. medRxiv 10.1101/2020.08.07.20170258. [DOI]
- 7.Isho B, Abe KT, Zuo M, Jamal AJ, Rathod B, Wang JH, Li Z, Chao G, Rojas OL, Bang YM, Pu A, Christie-Holmes N, Gervais C, Ceccarelli D, Samavarchi-Tehrani P, Guvenc F, Budylowski P, Li A, Paterson A, Yue FY, Marin LM, Caldwell L, Wrana JL, Colwill K, Sicheri F, Mubareka S, Gray-Owen SD, Drews SJ, Siqueira WL, Barrios-Rodiles M, Ostrowski M, Rini JM, Durocher Y, McGeer AJ, Gommerman JL, Gingras AC. 2020. Persistence of serum and saliva antibody responses to SARS-CoV-2 spike antigens in COVID-19 patients. Sci Immunol 5:eabe5511. doi: 10.1126/sciimmunol.abe5511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Randad PR, Pisanic N, Kruczynski K, Manabe YC, Thomas D, Pekosz A, Klein SL, Betenbaugh MJ, Clarke WA, Laeyendecker O, Caturegli PP, Larman HB, Detrick B, Fairley JK, Sherman AC, Rouphael N, Edupuganti S, Granger DA, Granger SW, Collins M, Heaney CD. 2020. COVID-19 serology at population scale: SARS-CoV-2 specific antibody responses in saliva. medRxiv doi: 10.1101/2020.05.24.20112300. [DOI] [PMC free article] [PubMed]
- 9.MacMullan MA, Ibrayeva A, Trettner K, Deming L, Das S, Tran F, Moreno JR, Casian JG, Chellamuthu P, Kraft J, Kozak K, Turner FE, Slepnev VI, Le Page LM. 2020. ELISA detection of SARS-CoV-2 antibodies in saliva. Sci Rep 10:20818. doi: 10.1038/s41598-020-77555-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.OraSure Technologies Inc. 2020. Oral specimen collection device. OraSure Technologies Inc, Bethlehem, PA. [Google Scholar]
- 11.OraSure Technologies Inc. 2020. Antibody collection device. OraSure Technologies Inc, Bethlehem, PA. [Google Scholar]
- 12.OraSure Technologies Inc. 2020. SARS-CoV-2 Antibody ELISA for use with OraSure Oral Specimens 1–7. OraSure Technologies Inc, Bethlehem, PA. [Google Scholar]
- 13.FDA. 2020. Curative-Korva SARS-Cov-2 Assay accelerated emergency use authorization (EUA) summary: Curative-Korva SARS-COV-2 assay (Curative-Korva, KorvaLabs Inc Clinical Laboratory). https://www.fda.gov/media/137089/download.
- 14.OraSure Technologies Inc. 2020. Collection procedure for use with antibody collection device. OraSure Technologies Inc, Bethlehem, PA. [Google Scholar]
- 15.OraSure Technologies Inc. 2020. Recommended laboratory preparation. OraSure Technologies Inc, Bethlehem, PA. [Google Scholar]
- 16.EuroImmun US. 2020. Anti-SARS-CoV-2 ELISA (IgG) instructions for use. EuroImmun US, Mountain Lakes, NJ. [Google Scholar]
- 17.McGhee JR, Mestecky J, Dertzbaugh MT, Eldridge JH, Hirasawa M, Kiyono H. 1992. The mucosal immune system: from fundamental concepts to vaccine development. Vaccine 10:75–88. doi: 10.1016/0264-410x(92)90021-b. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from us upon reasonable request.