Abstract
Early childhood adversity can cause an imbalance in the autonomic function, which may in turn lead to the development of trauma-spectrum disorders and aggressive behavior later in life. In the present study, we investigated the complex associations between early adversity, heart rate variability (HRV), cluster B personality disorders, and self-reported aggressive behavior in a group of 50 male forensic inpatients (M age = 41.16; SD = 10.72). Structural Equation Modeling analysis revealed that patients with cluster B personality disorders were more likely to have adverse early childhood experiences and reduced sympathetic dominance in response to a threat than patients without cluster B personality disorders. In addition, HRV and cluster B personality disorders did not significantly mediate the association between early childhood adversity and self-reported aggressive behavior. These findings are important for clinical practice to facilitate specific treatment programs for those affected.
Keywords: forensic patients, aggression, early childhood adversity, cluster B personality disorders, heart rate variability, structural equation modeling
Aggressive behavior represents one of the most important issues when dealing with forensic psychiatric patients residing in high secure psychiatric centers. It is defined as any act intended to cause harm, pain, or injury to another individual (Zirpoli, 2008). Aggressive behavior can cause serious psychological, emotional, and physical consequences to the victim and may adversely affect the treatment progress and the living environment (Tuente et al., 2018). Aggression in forensic psychiatric inpatient units takes place regularly because many forensic psychiatric patients have an antisocial personality disorder, high levels of impulsivity, and/or a lack of empathy, which are all factors directly related to aggression (Jeandarme et al.,2019; Lobbestael et al., 2015).
Generally, the explanatory factors underpinning aggressive behavior comprise an interplay between biological (e.g., genetic, fetal, hormonal), psychological (e.g., personality), and social factors (e.g., upbringing; Citrome & Volavka, 2003). In association with biological factors, it has been shown that the Autonomic Nervous System (ANS) plays an important role in stress and aggression regulation (Stifter et al., 2011). The ANS consists of two divisions that often have opposing effects on target organs: the sympathetic division (Sympathetic Nervous System [SNS]) and the parasympathetic division (Parasympathetic Nervous System [PNS]). The SNS is responsible for activities related to the “fight-or-flight” response to a threat, while the PNS controls the “rest-and-digest” response that calms the body down once the threat is over (Andreassi, 2010). Research has shown that aggressive behavior is associated with reduced Heart Rate Variability (HRV; Haller et al., 2014; Vögele et al., 2010), reflecting reduced vagal system activity (Cherland, 2012), and impaired emotion regulation capacity (Appelhans & Luecken, 2006). It is thought that in response to a threat the “vagal brake” is released, which allows the SNS to dominate and prepare the human body for the “fight-or-flight” response (Vögele et al., 2010). However, being exposed to chronic stress can affect the functioning of the vagal system in the long run, diminishing capacity for adaptive reactions to distressing events (Thayer et al., 2012). A higher resting HRV indicates the ability of the body to effectively respond to environmental challenges (Vögele et al., 2010). Conversely, reduced resting HRV is thought to index psychophysiological rigidity and maladaptive reaction to stress (Appelhans et al., 2006). It has also been documented that different HRV variables are differently associated with aggressive behavior. For example, Low Frequency (LF) was associated with physical aggression (Zohar et al., 2013), while decreased High Frequency (HF) and increased LF/HF ratio were associated with increased trait aggression and in vivo aggression (Puhalla et al., 2020). In the abovementioned studies, the association between HRV and aggression was investigated in adolescents or healthy community samples. However, no study to date has investigated the association between HRV and aggression in a group of high-risk forensic inpatients.
Furthermore, a large number of studies on adults from colleges, prisons, and the general population have also linked reduced HRV to different conditions such as early childhood adversity (McLaughlin et al., 2015; Shaikh al arab et al., 2012), and a range of mental disorders, particularly cluster B personality disorders (Carr et al., 2018; Zhang et al., 2012). Cluster B includes antisocial, borderline, histrionic and narcissistic personality disorders, and is characterized by dramatic overly emotional or unpredictable thinking, feeling or behaviors (American Psychiatric Association [APA], 2000). Early childhood adversity indicates children’s exposure to multiple traumatic events like witnessing violence, physical neglect and abuse, emotional neglect and abuse, and sexual abuse (Sansone et al., 2012). Interestingly, both childhood traumatic experiences and cluster B personality disorders have been consistently associated with the development of aggression and antisocial behavior (Sarchiapone et al., 2009; Verrill, 2018). Such results could signify that the same underlying physiological processes are associated with early adversity, cluster B personality disorders and aggressive behavior.
According to the theory of biological sensitivity to context (BSC; Boyce & Ellis, 2005), developmental experience plays an important role, along with heritable polygenic variation, in calibrating the responses designed to prepare the organism for challenge or threat, with potentially negative health outcomes under conditions of adversity and positive outcomes under conditions of support and protection (Kunst et al., 2010). As such, the constant need of the heart to adapt to traumatic experiences in early life is thought to cause an imbalance in the autonomic function, leading to an alteration in the structure of HRV in adulthood (McLaughlin et al., 2015). Failure to inhibit the stress response system can cause wear and tear on the body due to chronic overactivity of allostatic systems (McEwen, 1998), and can lead to a number of pathophysiological consequences. High exposure to stress and frequent activation of the stress response system can also shift toward the use of rapid life-history strategies (e.g., impulsivity, competitive risk-taking, and antisocial behavior), especially in males, resulting in low responsiveness and basal activity across the ANS and hypothalamic–pituitary–adrenal axis (Del Giudice et al., 2011). According to the Adaptive Calibration Model (ACM; Del Giudice et al., 2011) to adopt this strategy, the individual needs to become unresponsive to dangers and threats, and impervious to social context (e.g., lacking feelings of shame and remorse). This pattern of low responsiveness (i.e., Unemotional pattern in the ACM) is often detected in individuals with a high level of psychopathic traits, while low arousal as reflected in heart rate or HRV is a concurrent marker and predictor of antisocial behavior (Susman, 2006). In sum, impaired emotion regulation capacity provoked by early life adversity could have devastating consequences in adulthood, favoring trauma-spectrum disorders and furthering later aggressive and criminal behavior.
However, little is known if childhood neglect and abuse and cluster B personality disorders in adulthood are directly or indirectly associated with low HRV and aggression in a sample of forensic psychiatric inpatients. The main goal of the present study was therefore to investigate these complex associations between early childhood adversity, HRV, cluster B personality disorders and self-reported aggressive behavior. Due to the fact that HRV decreases naturally with aging (De Meersman & Stein, 2007), controlling for age is necessary when examining the association between HRV and other psychological factors.
Based on the theory of BSC (Boyce & Ellis, 2005), the ACM (Del Giudice et al., 2011), the concept of allostatic load (McEwen, 1998), and previous empirical findings, it was hypothesized that HRV is a mediator of early adversity on cluster B personality disorders and self-reported aggressive behavior. Specifically, we expected that greater trauma exposure would lead to reduced vagally mediated and increased sympathetically mediated HRV, and consequently to the development of cluster B personality disorders and hence more pronounced aggressive behavior. It should be noted that due to the small sample size, only a composite score that captures all forms of early adversity was included in the model to preserve the statistical power. However, to the best of our knowledge, no studies have investigated how different forms of early childhood adversity are linked to HRV and whether various forms of early childhood adversity can contribute differentially to alterations in the functioning of the ANS. Therefore, a secondary aim of the current study was to investigate the association between three clinical forms of abuse and two aspects of neglect and HRV.
Methods
Participants
The sample consisted of 50 out of the 64 male patients who were selected to participate in a Randomized Controlled Trial on the effectiveness of Virtual Reality Aggression Prevention Training (VRAPT) to prevent and reduce aggression (Tuente et al., 2018). All 64 patients were assigned to VRAPT. The physiological data of 14 patients were not usable and these patients were therefore not included in the study. The study started in 2016 and lasted until the end of 2018. Patients varied in age from 25 to 67 (M = 41.16; SD = 10.72), and were staying in one of the four Dutch Forensic Psychiatric Centers (FPCs): FPC Dr. S. van Mesdag, located in Groningen; FPC Fivoor TBS, located in Poortugaal; FPC Pompestichting, located in Nijmegen; FPC de Rooyse Wissel, located in Oostrum. Forty-two percent of the patients were diagnosed with cluster B personality disorders. Among cluster B patients, the most common comorbid diagnoses were schizophrenia and other psychotic disorders (23.8%), autism (14.3%), and attention deficit hyperactivity disorder (ADHD; 14.3%) on Axis I, and cluster A personality disorder (4.8%) on Axis II. Among non-cluster B patients, the most common diagnoses were schizophrenia and other psychotic disorders (20.7%), autism (13.8%), and ADHD (6.9%) on Axis I, and personality disorder not otherwise specified (51.7%), and cluster C personality disorders (3.4%) on Axis II.
In the Netherlands, the FPC is the highest security institution for forensic psychiatric patients who have the highest chance of future violent recidivism. Patients in the FPC have committed one or more violent offenses caused by a severe psychiatric illness, with a minimum threat of 4 years imprisonment. All FPC patients have received a so-called “TBS” order imposed by the judge. This means that they are partially or completely irresponsible to their violent acts and they remain outside of society until the FPC deems it appropriate (TBS: in Dutch: terbeschikkingstelling: this translates as “detained under hospital order”; Klein Tuente et al., 2018).
Procedure
All patients who met predefined criteria were invited by their treatment supervisor and/or clinical team to participate in this study. Inclusion criteria were being a forensic psychiatric inpatient referred to the study by the clinician based on a history of aggression and/or problems with aggression during the stay in the FPC. Patients with an inability to speak and read Dutch, epilepsy, or intellectual disability (i.e., IQ below 70) were excluded. There were no restrictions when it comes to diagnoses based on the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; APA, 2000) and (history of) substance use disorders. If patients agreed to participate, they were asked to sign the consent form. After informed consent was obtained, the patients completed a set of validated psychosocial questionnaires and started with the VR training. The VR training consisted of 16-biweekly individual sessions that lasted between 30 and 60 minutes, with an average being 45 minutes. In the interactive three-dimensional virtual environment, participants can practice new desired behavior with virtual characters to learn how to cope with their own aggressive behavior in an adequate way. A VRAPT training protocol is based on the theory of Social Information Processing (SIP; Walther, 2008). Each step of the SIP model can be practiced separately. An example of an exercise is learning to recognize the facial emotions of others. The last part of the VRAPT training consists of role-plays in which the different SIP exercises are integrated into more challenging interactive virtual role-plays. For this, several interactive social scenarios were designed by software engineers, clinicians and researchers. During the VRAPT sessions, participants wear headphones while interacting with a virtual character. The training was controlled by the trainer who takes the role of the virtual character using a voice-distorted microphone. Trainers encourage participants to continue applying new behaviors that they have learned in the VR training. The trainer has control over the virtual environment at all times and can immediately change and/or stop the training if necessary. In general, the VRAPT program is standardized, but the stimulus given by the trainer is adapted to the specific learning goals of the participant. It is crucial that each participant is optimally triggered by the scenarios so that optimal stress responses are achieved that are at the same level for each patient. More details about the VRAPT protocol could be found in the Supplemental Appendix. The protocol of this study was approved by the medical ethical board of the University Medical Centre Groningen (number: NL52939.042.15).
Measures
Physiological measures
Lead II electrocardiogram (ECG) was recorded continuously during VRAPT sessions 5 to 16 by using a Nexus-10 amplifier and recording system (Nexus-10, TMS International BV, The Netherlands). The first four sessions were dedicated to getting participants familiar with the protocol (e.g., how to use the device) and checking if the procedure worked as planned (e.g., if the participant understands the instructions, if there are problems to be solved etc.). The signals were sampled at a rate of 1,024 Hz (Mesdag, Pompe, Rooyse Wissel) or 2,048 Hz (Kijvelanden), therefore precision with which the R-peaks were located was ~1 ms or ~0.5 ms (Kijvelanden). For each session in each participant, we started out by selecting the middle 5 minutes from the data. We then visually inspected the raw ECG data in order to determine whether this segment was relatively artifact-free. If it was, then this segment was used for further processing. If not, we selected another interval near to the middle based on visual inspection. Then, we attempted to score the R-peaks within those intervals by means of two well-known scoring methods (Afonso et al., 1999; Pan & Tompkins, 1985) in custom-made software developed in R (R Core Team, 2016). The idea was that different methods would be able to cope with different types of artifacts in the ECG. We then combined the results of the two methods. If they resulted in the same peak, then that peak was flagged as the correct peak. If not, we used a practical estimate and flagged it as a candidate peak. Subsequently, all correct and candidate peaks, for all participants in all sessions, were visually checked against the original ECG record in that period, and the true ECG peaks were determined. The R-peak locations were used to calculate cardiotachograms. Any remaining errors in determining the location of the R-peaks are immediately visible in the cardiotachogram, either by a sharp peak upwards (missed beat) or downwards (extra beat) in an otherwise fairly regular signal. These artifacts were detected by a mean ± SD procedure fitted over the data. The number of SDs was different for every participant and was based on visual inspection of the corrected cardiotachogram (range: 1.8–4 SDs). Peaks in the cardiotachograms outside of this range were deleted from the series and interpolated back in by cubic spline interpolation. Then, the cardiotachogram was visually inspected once more. The consequence of this elaborate procedure was that no data needed to be excluded once we selected a 5-minute interval.
Heart rate (HR), inter-beat intervals (IBI) and HRV measures were extracted from the cleaned electrocardiogram (ECG) using custom-made software developed in R (R Core Team, 2016). HR refers to the number of beats per minute. It is controlled by two branches of the ANS—the SNS accelerates, while the PNS slows the HR. The IBI represents the time between two individual beats in the cardiac cycle (Andreassi, 2010), while HRV refers to the variation in the time between successive heartbeats. The time-domain measures of HRV (i.e., mean, the root mean square differences of successive R-R intervals [RMSSD], and the standard deviation of normal to normal R-R intervals, [SDNN]) were computed on the raw IBI (Malik, 1996). The frequency-domain measures were based on IBIs transformed into the frequency domain by the Lomb-Scargle periodogram, which can handle the unevenly spaced time base that is characteristic of the heart period so that no interpolation is needed. Based on previous studies, the following frequency bands were analyzed: LF (0.04–0.15 Hz), HF (0.15–0.4 Hz), and the LF/HF ratio (von Rosenberg et al., 2017). The HF component indicates the activity of the PNS and the vagus nerve, whereas the LF is an indicator of the sympathetic activity, although this has been much debated in the literature, and others have argued that it is more a reflection of baroreflex function (e.g., Goldstein et al., 2011). The LF/HF ratio refers to the sympathovagal balance of the ANS, although it has been argued more recently that this measure is not an accurate indicator of sympathovagal balance given that LF does not only reflect sympathetic activity (Billman, 2013; von Rosenberg et al., 2017). Despite the current debate, LF and LF/HF ratio are still widely used in research and therefore, we kept them in the analysis to be comparable to other studies (e.g., Puhalla et al., 2020; Zohar et al., 2013). Lastly, average HRV measured over 12 VR training sessions was computed for each participant from the aggregated HRV data, in order to create one measure of each HRV parameter. The average HRV was chosen because HRV is significantly correlated with an average HR, and this association is both physiologically and mathematically determined (Sacha, 2013).
Self-reported measures
The level of aggressive behavior was assessed by the Dutch Reactive and Proactive Questionnaire (RPQ; Domburgh & Popma, 2003). The RPQ is a reliable and valid self-report questionnaire that comprises 11 items to assess reactive aggression (RA; e.g., “Reacted angrily when provoked by others”), and 12 items to assess proactive aggression (PA; e.g., “Had fights with others to show who was on top”). All items are scored on a 3-point Likert scale from 0 = never to 2 = often. Higher scores indicate higher levels of aggression. In this study, only the total score of the RPQ was used. The internal consistency of the RPQ was very good (Cronbach’s α = .91).
Early childhood adversity was measured by the Child Trauma Questionnaire-Short Form (CTQ-SF; Bernstein et al., 2003). The CTQ-SF consists of 25 items assessing three clinical forms of abuse: physical, sexual and emotional, and two aspects of neglect: physical and emotional, with each maltreatment being represented by five questions. All items are scored on a 5-point Likert scale from 1 = never true to 5 = very often true. Higher scores indicate more early adversity. The internal consistency of the CTQ-SF in the present study was α = .78.
Cluster B personality disorders
Diagnosis of cluster B personality disorders was based on the DSM-IV-TR (APA, 2000) and determined by a psychiatrist in consultation with a clinical psychologist considering all available file information. The diagnosis was discussed in the team and stored in electronic patient records. Cluster B personality disorders were coded as follows: 0 = no diagnosis and 1 = diagnosis.
Statistical Analysis
All analyses were conducted using R (R Core Team, 2016) and SPSS v.24.0 (IBM Corp., Armonk, NY, USA). To explore whether cluster B personality disorders and HRV adjusted for age, exert a mediating effect on the association between early childhood adversity and self-reported aggressive behavior, Structural Equation Modeling (SEM) analyses with the bootstrapping procedure were conducted, using the lavaan package in R (Rosseel, 2012). Bootstrapping involves repeatedly taking random samples with the replacement of the original data, to obtain estimates of the model test statistics and parameter standard errors (Nevitt & Hancock, 2001). The model was estimated with the Maximum Likelihood estimation, which looks for parameter estimates that make the likelihood for observed data maximal (Raykov & Marcoulides, 2012). Model evaluation was based on the statistical test for global model fit (i.e., the model Chi-Square), and the following fit indices: Comparative Fit Index (CFI) and Standardized Root Mean Square Residual (SRMR). The model Chi-Square “assesses the magnitude of discrepancy between the sample and fitted covariances matrices” (Hu & Bentler, 1999: 2). An insignificant result at a 0.05 threshold indicates a good model fit (Barrett, 2007). The CFI compares the fit of a target model against that of the independence (null) model. Values of at least 0.90 indicate a good model fit (Hooper et al., 2008). The SRMR refers to the square-root of the difference between the residuals of the sample covariance matrix and the hypothesized model. A value of less than 0.08 is considered a good fit (Hooper et al., 2008). The minimum sample size for conducting SEM is at least five observations per estimated parameter whereby 50 respondents generate sufficient power (Bentler & Chou, 1987).
The direct and indirect paths among key constructs (i.e., early adversity and self-reported aggressive behavior) were based on the theory of BSC (Boyce & Ellis, 2005), the ACM (Del Giudice et al., 2011), and findings from existing literature (Shaikh al arab et al., 2012; Verrill, 2018). A visual representation of the hypothesized model is presented in Figure 1. Finally, multiple regression analyses were performed to test the unique associations between various forms of early adversity, and HRV whilst controlling for age.
Figure 1.
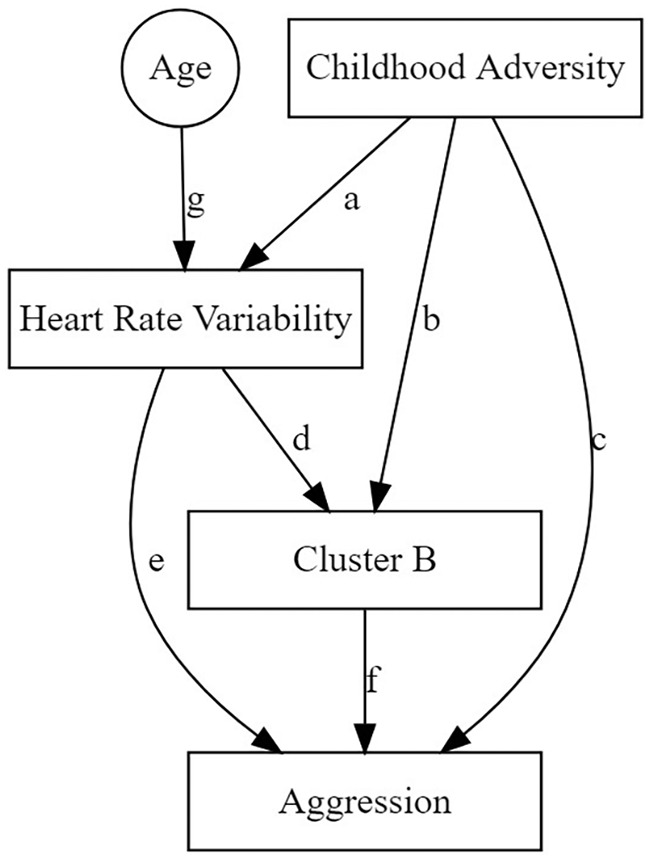
Diagram of structural equation modeling predicting aggressive behavior.
Results
Descriptive Statistics
Descriptive statistics and correlations for study variables are displayed in Table 1.
Table 1.
Descriptive Statistics and Correlations for Study Variables.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Emotional abuse | 10.91 | 5.12 | – | |||||||||||||
| 2. Emotional neglect | 16.36 | 5.60 | −0.64** | – | ||||||||||||
| 3. Physical neglect | 10.88 | 6.24 | 0.76** | −0.58** | – | |||||||||||
| 4. Physical abuse | 11.68 | 2.50 | 0.08 | 0.15 | 0.03 | – | ||||||||||
| 5. Sexual abuse | 7.95 | 5.54 | 0.50** | −0.30* | 0.40** | −0.07 | – | |||||||||
| 6. Adversity total score | 57.78 | 12.16 | 0.76** | −0.21 | 0.76** | 0.29* | 0.72** | – | ||||||||
| 7. IBI | 0.76 | 0.13 | 0.14 | −0.14 | 0.16 | −0.23 | 0.04 | 0.05 | – | |||||||
| 8. SDNN | 0.04 | 0.02 | 0.06 | −0.08 | 0.15 | −0.33* | −0.04 | −0.03 | 0.71** | – | ||||||
| 9. RMSDD | 0.02 | 0.01 | 0.07 | −0.24 | 0.16 | −0.30* | −0.09 | −0.10 | 0.63** | 0.80** | – | |||||
| 10. LF | 63.86 | 28.43 | 0.15 | −0.15 | 0.24 | 0.10 | 0.01 | 0.14 | −0.48** | −0.19 | −0.19 | – | ||||
| 11. HF | 19.29 | 15.36 | −0.06 | −0.11 | −0.02 | −0.06 | −0.08 | −0.14 | 0.14 | 0.01 | 0.48** | −0.25 | – | |||
| 12. LF/HF | 6.08 | 4.56 | 0.05 | 0.04 | 0.00 | 0.16 | −0.09 | 0.03 | −0.41** | −0.18 | −0.38** | 0.67** | −0.59** | – | ||
| 13. Age | 41.16 | 10.72 | −0.18 | 0.26 | −0.18 | −0.13 | −0.05 | −0.09 | 0.13 | −0.29* | −0.23 | −0.33* | 0.13 | −0.14 | – | |
| 14. Aggression | 15.63 | 8.49 | 0.18 | −0.09 | 0.25 | −0.01 | 0.15 | 0.22 | −0.13 | −0.03 | −0.10 | 0.19 | −0.08 | −0.3 | −0.25 | – |
Note. IBI = Inter-beat Interval; RMSSD = Root Mean Square of the Successive Differences; SDNN = Standard Deviation of Normal to Normal R-R intervals; LF = Low Frequency Power of Heart Rate Variability, HF = High Frequency Power of Heart Rate Variability; LF/HF = Ratio between Low and High Frequency Components of Heart Rate Variability.
p < .05. **p < .01.
SEM Analysis
To explore whether cluster B personality disorders and HRV adjusted for age (i.e., mean IBI, SDNN, RMSSD, LF, HF, and LF/HF ratio), play an intermediary role linking early childhood adversity and self-reported aggressive behavior, SEM analyses were conducted. The results showed that there was a consistent and positive association between early adversity and cluster B personality disorders across all tested models, with a standardized beta coefficient ranging in value from β = .351 to β = .382, p < .001. In addition, a significant negative association was also found between cluster B personality disorders and the LF/HF ratio adjusted for age, β = −.295, p = .007. Direct paths between other HRV parameters and key constructs were insignificant. Lastly, the indirect paths were insignificant as well in all models tested, indicating that cluster B personality disorders and HRV adjusted for age do not mediate the association between early childhood adversity and aggression (Tables A1 and A2 in the Supplemental Appendix).
Further, as can be seen from Table 2, the Chi-square for global model fit, as well as the SRMR, an absolute measure of fit, were very good for all HRV parameters, while the CFI was good only for the LF HRV parameter. However, given the small sample size in this study, it could be said that the measurement models yielded acceptable fit indices.
Table 2.
SEM Summary Table for Fit Statistics.
| Variables | Chi-Square | df | P | CFI | SRMR |
|---|---|---|---|---|---|
| IBI | 3.047 | 2 | .218 | 0.870 | 0.064 |
| SDNN | 4.616 | 2 | .099 | 0.770 | 0.077 |
| RMSSD | 4.432 | 2 | .109 | 0.752 | 0.077 |
| LF | 2.952 | 2 | .229 | 0.924 | 0.062 |
| HF | 3.850 | 2 | .146 | 0.808 | 0.074 |
| LF/HF | 4.538 | 2 | .012 | 0.792 | 0.078 |
Note. SD = Standard Deviation; IBI = Inter-beat Interval; RMSSD = Root Mean Square of the Successive Differences; SDNN = Standard Deviation of Normal to Normal R-R intervals; LF = Low Frequency Power of Heart Rate Variability; HF = High Frequency Power of Heart Rate Variability; LF/HF = Ratio between Low and High Frequency Components of Heart Rate Variability; df = degrees of freedom, CFI = Comparative Fit Index; SRMR = Standardized Root Mean Square Residual.
Multiple Regression Analyses
Associations between various forms of early adversity including three clinical forms of abuse (i.e., physical, sexual and emotional), and two aspects of neglect (i.e., physical and emotional), and HRV variables adjusted for age (i.e., mean IBI, SDNN, RMSSD, LF, HF, and LF/HF ratio) were examined with multiple regression analyses. Results revealed that physical neglect was negatively associated with SDNN, β = −.429, t = −3.007, p = .004, and RMSSD, β = −.326, t = −2.253, p = .030, whilst controlled for age (β = −.363, t = −2.624, p = .012; β = −.230, t = −1.607, p = .115), respectively (Tables A3 and A4 in the Supplemental Appendix). There were no other significant associations between HRV variables and different types of early adversity.
Discussion
This was the first study aimed at exploring the complex associations between early childhood adversity, HRV, cluster B personality disorders, and self-reported aggressive behavior, in a sample of 50 male psychiatric forensic patients. The SEM analysis revealed that the empirical model fits well with the proposed theoretical model. The results showed that cluster B personality disorders were positively associated with early childhood adversity and negatively associated with the LF/HF ratio adjusted for age. Further, we also conducted multiple regression analyses to investigate the unique associations between various forms of early childhood adversity including physical, sexual and emotional abuse, and physical and emotional neglect and HRV variables adjusted for age. The results showed that physical neglect was negatively associated with SDNN and RMSSD, respectively, supporting our hypothesis that there is a link between early childhood adversity and diminished parasympathetic activity.
Consistent with the concept of allostatic load (McEwen, 1998), the theory of BSC (Boyce & Ellis, 2005) and the ACM (Del Giudice et al., 2011), early childhood adversity can cause an imbalance in the function of the ANS, leading to the structural alterations of HRV in adulthood. Such alterations could further cause the impaired emotion regulation capacity and maladaptive emotional response to both stressful and social situations, which in turn may enforce the emotional and impulsive symptoms to emerge. These symptoms could subsequently progress in dramatic overly emotional or unpredictable thinking, feeling or behavior, furthering later development of cluster B personality disorders and aggression.
Furthermore, the SEM analyses revealed that forensic psychiatric patients who experienced early childhood adversity were more likely to develop cluster B personality disorders in adulthood. This result supports a large number of previous studies demonstrating a positive association between early adversity and cluster B personality disorders (e.g., Bogaerts et al., 2005; Zhang et al., 2012). However, contrary to our expectations, a significant negative path between cluster B personality disorders and the LF/HF ratio was found. This finding showed that forensic psychiatric patients with cluster B personality disorders had reduced SNS dominance in response to a threat, indicating a system under reduced stress, which cannot be supported by previous research. An alternative indirect explanation could be that when the “fight-or-flight” responses (i.e., state sympathetic arousal) fail, the freeze state (i.e., immobility state) may occur as an expression of a defensive strategy. Brain processes suppress the SNS response to escape the danger (Niermann et al., 2017). Defensive stress-responses were frequently detected in traumatized patients and patients with anxiety disorders (Kozlowska et al., 2015), while aggression was associated with the absence of avoidance behavior to social threats (von Borries et al., 2012). Given that cluster B personality disorders have been consistently associated with the development of aggression and antisocial behavior (Sarchiapone et al., 2009), this result is the opposite of what would be expected. However, it is important to note that the functional interpretation of the LF/HF ratio is currently under debate (Billman, 2013; von Rosenberg et al., 2017), and therefore the interpretation of this result should be done with care. Moreover, we did not find significant paths between other HRV parameters (i.e., IBI, SDNN, RMSSD, LF, and HF) and early adversity, cluster B personality disorders and aggression. This result differs from previous findings in adolescents and community samples, linking aggressive behavior, early adversity and cluster B personality disorders to reduced HRV (Carr et al., 2018; Haller et al., 2014; Shaikh al arab et al., 2012; Vögele et al., 2010). It might be that the associations among these constructs in a sample of forensic psychiatric patients indeed differ from those found in community samples or samples of adolescents. More studies are needed that would incorporate a healthy control group. Lastly, cluster B personality disorders and HRV adjusted for age, did not significantly mediate the association between early childhood adversity and aggression. However, this result may provide some support to the previous research showing that low HR, but not HRV, mediates the relationship between social adversity (e.g., poor parenting, poverty, segregation) and antisocial behavior (Choy et al., 2015; Fagan et al., 2017). This may signify that neither the SNS nor PNS activity alone is responsible for the unique way in which early childhood adversity influences aggressive behavior (Fagan et al., 2017). Alternatively, we may not have had enough statistical power to find significant mediating effects due to the small sample size.
Moreover, the multiple regression analyses revealed that physical neglect was negatively associated with SDNN and RMSSD, respectively, indicating that patients who were physically neglected in early childhood had reduced parasympathetic activity in adulthood. These results signify that, in a forensic psychiatric sample, a specific form of early adversity, rather than the overall adverse childhood experiences, might play a more important role in the development of aggressive behavior.
Apart from contributing to the understandings of the development of aggressive behavior, the present study could be of practical value, as well. As mentioned previously, forensic psychiatric inpatients residing in FPCs have the highest chance of future violent recidivism. Hence, for each patient, a structured violence risk assessment must be performed at least once a year, using validated risk assessment tools such as the Historical Clinical Future [Historisch Klinisch Toekomst] Revised (Bogaerts et al., 2018; Spreen et al., 2014). These assessments are performed to investigate the treatment progress and to estimate the likelihood of future inpatient violence. Depending on the disorder and individual risk management plan, the FPC provides patients with different treatment programs and modules (Puri & Treasaden, 2017). However, when dealing with forensic patients, aggressive behavior could represent a major obstacle to the implementation of the planned treatment. The current study showed that screening for early physical neglect could give us more insight into those patients at higher risk for the development of aggressive behavior toward staff and other forensic patients. This knowledge could help clinicians design timely interventions aimed at reducing aggression in closed forensic psychiatric settings, subsequently providing offenders with more protection from the occurrence of reoffending.
This study is not without limitations. First, the study was limited by a small sample size, which could potentially lower statistical power to find significant effects between main constructs. Also, to maintain sufficient statistical power, we did not control for autism, schizophrenia, and ADHD, although the prevalence of these comorbid diagnoses was not negligible in cluster B patients. In addition, we did not control for smoking status and medication use that have been shown to influence HRV (Murgia et al., 2019). Another issue is that we included the LF/HF ratio in the analysis, despite the recent debate that the LF/HF ratio may not accurately quantify cardiac “sympathovagal balance.” However, to resolve the ambiguities in the standard LF/HF-ratio analyses, von Rosenberg et al. (2017) proposed a joint treatment of the LF and HF powers in HRV within a two-dimensional representation framework, which could be the key component in future attempts to overcome the limitations of the present study. The study was also limited by the fact that baseline HRV data were not available and therefore we were not able to examine session-related physiological changes nor how resting HRV parameters are associated with key constructs. Finally, we did not distinguish between reactive (i.e., impulsive, anger oriented and in response to a threat) and proactive aggression (i.e., goal driven, intentional and manipulative; Kunst et al., 2010) although there is some evidence that these two forms of aggression are differently associated with HRV variables (Scarpa et al., 2010). Future studies should aim to replicate our findings by considering both forms of aggressive behavior. It would also be beneficial for future studies to include the various forms of early childhood adversity in the model rather than the total early adversity score, as our study showed that HRV is differently associated with different forms of early adversity. Last but not least, researchers may also consider selecting periods of HRV related to specific events in the VRAPT training. This will likely make the results more consistent over participants and sessions.
In conclusion, the findings of the present study add to the understanding of the origins of the aggressive behavior of psychiatric forensic patients. Even though there were some limitations of the current study and certain deviations from predicted models, this work certainly opens up new avenues of future research on determinants of aggressive behavior from multiple perspectives.
Supplemental Material
Supplemental material, sj-pdf-1-ijo-10.1177_0306624X20986537 for The Complex Associations Between Early Childhood Adversity, Heart Rate Variability, Cluster B Personality Disorders, and Aggression by Marija Jankovic, Stefan Bogaerts, Stéphanie Klein Tuente, Carlo Garofalo, Wim Veling and Geert van Boxtel in International Journal of Offender Therapy and Comparative Criminology
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study is funded by the Netherlands Organization for Scientific Research, as part of the research program “Geweld tegen psychatrisch patienten” (Violence against psychiatric patients; NWO grant number 432–13-802).
ORCID iDs: Marija Jankovic  https://orcid.org/0000-0002-7385-8169
https://orcid.org/0000-0002-7385-8169
Carlo Garofalo  https://orcid.org/0000-0003-2306-6961
https://orcid.org/0000-0003-2306-6961
Supplemental Material: Supplemental material for this article is available online.
References
- Afonso V. X., Tompkins W. J., Nguyen T. Q., Luo S. (1999). ECG beat detection using filter banks. IEEE Transactions on Biomedical Engineering, 46(2), 192–202. 10.1109/10.740882 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Author. [Google Scholar]
- Andreassi J. L. (2010). Psychophysiology: Human behavior and physiological response. Psychology Press. [Google Scholar]
- Appelhans B. M., Luecken L. J. (2006). Heart rate variability as an index of regulated emotional responding. Review of General Psychology, 10(3), 229. 10.1037/1089-2680.10.3.229 [DOI] [Google Scholar]
- Barrett P. (2007). Structural equation modelling: Adjudging model fit. Personality and Individual Differences, 42(5), 815–824. 10.1016/j.paid.2006.09.018 [DOI] [Google Scholar]
- Bernstein D. P., Stein J. A., Newcomb M. D., Walker E., Pogge D., Ahluvalia T., Stokes J., Handelsman L., Medrano M., Desmond D., Zule W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Bentler P. M., Chou C. P. (1987). Practical issues in structural modeling. Sociological Methods & Research, 16(1), 78–117. 10.1177/0049124187016001004 [DOI] [Google Scholar]
- Billman G. E. (2013). The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Frontiers in Physiology, 4, 26. 10.3389/fphys.2013.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogaerts S., Spreen M., Ter Horst P, Gerlsma C. (2018). Predictive validity of the HKT-R Risk Assessment for two and five-year recidivism in a cohort of Dutch Forensic Psychiatric Patients. International Journal of Offender Therapy and Comparative Criminology, 62, 2259–2270. 10.1177/0306624X17717128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogaerts S., Vanheule S., Declercq F. (2005). Recalled parental bonding, adult attachment style, and personality disorders in child molesters: A comparative study. Journal of Forensic Psychiatry & Psychology, 16(3), 445–458. 10.1080/14789940500094524 [DOI] [Google Scholar]
- Boyce W. T., Ellis B. J. (2005). Biological sensitivity to context: I. An evolutionary developmental theory of the origins and functions of stress reactivity. Development and Psychopathology, 17(2), 271–301. 10.1017/S0954579405050145 [DOI] [PubMed] [Google Scholar]
- Carr O., de Vos M., Saunders K. E. (2018). Heart rate variability in bipolar disorder and borderline personality disorder: A clinical review. Evidence-Based Mental Health, 21(1), 23–30. 10.1136/eb-2017-102760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherland E. (2012). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, self-regulation. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 21(4), 313. [Google Scholar]
- Choy O., Raine A., Portnoy J., Rudo-Hutt A., Gao Y., Soyfer L. (2015). The mediating role of heart rate on the social adversity-antisocial behavior relationship: A social neurocriminology perspective. Journal of Research in Crime and Delinquency, 52(3), 303–341. 10.1177/0022427814565905 [DOI] [Google Scholar]
- Citrome L., Volavka J. (2003). Treatment of violent behavior. In Tasman A., Lieberman J., Kay J. (Eds.), Psychiatry (2nd ed.). John Wiley & Sons, Ltd. [Google Scholar]
- De Meersman R. E., Stein P. K. (2007). Vagal modulation and aging. Biological Psychology, 74(2), 165–173. 10.1016/j.biopsycho.2006.04.008 [DOI] [PubMed] [Google Scholar]
- Del Giudice M., Ellis B. J., Shirtcliff E. A. (2011). The adaptive calibration model of stress responsivity. Neuroscience & Biobehavioral Reviews, 35(7), 1562–1592. 10.1016/j.neubiorev.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domburgh L., Popma A. (2003). Reactive and proactive questionnaire; [Dutch translation]. Duivendrecht, The Netherlands. [Google Scholar]
- Fagan S. E., Zhang W., Gao Y. (2017). Social adversity and antisocial behavior: Mediating effects of autonomic nervous system activity. Journal of Abnormal Child Psychology, 45(8), 1553–1564. 10.1007/s10802-017-0262-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein D. S., Bentho O., Park M. Y., Sharabi Y. (2011). Low-frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Experimental Physiology, 96(12), 1255–1261. 10.1113/expphysiol.2010.056259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller J., Raczkevy-Deak G., Gyimesine K. P., Szakmary A., Farkas I., Vegh J. (2014). Cardiac autonomic functions and the emergence of violence in a highly realistic model of social conflict in humans. Frontiers in Behavioral Neuroscience, 8, 364. 10.3389/fnbeh.2014.00364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper D., Coughlan J., Mullen M. R. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60. 10.21427/D79B73 [DOI] [Google Scholar]
- Hu L. T., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jeandarme I., Wittouck C., Vander Laenen F., Pouls C., Oei T. I., Bogaerts S. (2019). Risk factors associated with inpatient violence during medium security treatment. Journal of Interpersonal Violence, 34(17), 3711–3736. 10.1177/0886260516670884 [DOI] [PubMed] [Google Scholar]
- Kozlowska K., Walker P., McLean L., Carrive P. (2015). Fear and the defense cascade: Clinical implications and management. Harvard Review of Psychiatry, 23(4), 263. 10.1097/HRP.0000000000000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunst M., Winkel F. W., Bogaerts S. (2010). Prevalence and predictors of posttraumatic stress disorder among victims of violence applying for state compensation. Journal of Interpersonal Violence, 25(9), 1631–1654. 10.1177/0886260509354591 [DOI] [PubMed] [Google Scholar]
- Lobbestael J., Cima M., Lemmens A. (2015). The relationship between personality disorder traits and reactive versus proactive motivation for aggression. Psychiatry Research, 229(1–2), 155–160. 10.1016/j.psychres.2015.07.052 [DOI] [PubMed] [Google Scholar]
- Malik M. (1996). Heart rate variability: Standards of measurement, physiological interpretation, and clinical use: Task force of the European Society of Cardiology and the North American Society for Pacing and Electrophysiology. Annals of Noninvasive Electrocardiology, 1(2), 151–181. [Google Scholar]
- McLaughlin K. A., Sheridan M. A., Tibu F., Fox N. A., Zeanah C. H., Nelson C. A. (2015). Causal effects of the early caregiving environment on development of stress response systems in children. Proceedings of the National Academy of Sciences, 112(18), 5637–5642. 10.1073/pnas.1423363112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840(1), 33–44. 10.1111/j.1749-6632.1998.tb09546.x [DOI] [PubMed] [Google Scholar]
- Murgia F., Melotti R., Foco L., Gögele M., Meraviglia V., Motta B., Steger A., Toifl M., Sinnecker D., Müller A., Merati G. (2019). Effects of smoking status, history and intensity on heart rate variability in the general population: The CHRIS study. Plos One, 14(4), e0215053. 10.1371/journal.pone.0215053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nevitt J., Hancock G. R. (2001). Performance of bootstrapping approaches to model test statistics and parameter standard error estimation in structural equation modeling. Structural Equation Modeling, 8(3), 353–377. 10.1207/S15328007SEM0803_2 [DOI] [Google Scholar]
- Niermann H. C., Figner B., Roelofs K. (2017). Individual differences in defensive stress-responses: The potential relevance for psychopathology. Current Opinion in Behavioral Sciences, 14, 94–101. 10.1016/j.cobeha.2017.01.002 [DOI] [Google Scholar]
- Puri B., Treasaden I. H. (Eds.). (2017). Forensic psychiatry: Fundamentals and clinical practice. CRC Press. [Google Scholar]
- Puhalla A. A., Kulper D. A., Fahlgren M. K., McCloskey M. S. (2020). The relationship between resting heart rate variability, hostility, and in vivo aggression among young adults. Journal of Aggression, Maltreatment & Trauma, 29(2), 206–222. 10.1080/10926771.2018.1558324 [DOI] [Google Scholar]
- Raykov T., Marcoulides G. A. (2012). A first course in structural equation modeling. Routledge. [Google Scholar]
- Rosseel Y. (2012). Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). Journal of Statistical Software, 48(2), 1–36. [Google Scholar]
- Sacha J. (2013). Why should one normalize heart rate variability with respect to average heart rate. Frontiers in Physiology, 4, 306. 10.3389/fphys.2013.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone R. A., Leung J. S., Wiederman M. W. (2012). Five forms of childhood trauma: Relationships with aggressive behavior in adulthood. The Primary Care Companion for CNS Disorders, 14(5), PCC.12m01353. 10.4088/PCC.12m01353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarchiapone M., Carli V., Cuomo C., Marchetti M., Roy A. (2009). Association between childhood trauma and aggression in male prisoners. Psychiatry Research, 165(1–2), 187–192. 10.1016/j.psychres.2008.04.026 [DOI] [PubMed] [Google Scholar]
- Scarpa A., Haden S. C., Tanaka A. (2010). Being hot-tempered: Autonomic, emotional, and behavioral distinctions between childhood reactive and proactive aggression. Biological Psychology, 84(3), 488–496. 10.1016/j.biopsycho.2009.11.006 [DOI] [PubMed] [Google Scholar]
- Shaikh al arab A., Guédon-Moreau L., Ducrocq F., Molenda S., Duhem S., Salleron J., Chaudieu I., Bert D., Libersa C., Vaiva G. (2012). Temporal analysis of heart rate variability as a predictor of post traumatic stress disorder in road traffic accidents survivors. Journal of Psychiatric Research, 46(6), 790–796. 10.1016/j.jpsychires.2012.02.006 [DOI] [PubMed] [Google Scholar]
- Spreen M., Brand E., Ter Horst P., Bogaerts S. (2014). Handleiding en Methodologische Verantwoording HKT-R, Historisch, Klinische en Toekomstige-Revisie. Tilburg University Research. [Google Scholar]
- Stifter C. A., Dollar J. M., Cipriano E. A. (2011). Temperament and emotion regulation: The role of autonomic nervous system reactivity. Developmental Psychobiology, 53(3), 266–279. 10.1002/dev.20519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susman E. J. (2006). Psychobiology of persistent antisocial behavior: Stress, early vulnerabilities and the attenuation hypothesis. Neuroscience & Biobehavioral Reviews, 30(3), 376–389. 10.1016/j.neubiorev.2005.08.002 [DOI] [PubMed] [Google Scholar]
- Thayer J. F., Åhs F., Fredrikson M., Sollers J. J.,, III, Wager T. D. (2012). A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neuroscience & Biobehavioral Reviews, 36(2), 747–756. 10.1016/j.neubiorev.2011.11.009 [DOI] [PubMed] [Google Scholar]
- Team R. C. (2016). R: A language and environment for statistical computing. R Foundation for Statistical Computing. [Google Scholar]
- Tuente S. K., Bogaerts S., van IJzendoorn S., Veling W. (2018). Effect of virtual reality aggression prevention training for forensic psychiatric patients (VRAPT): Study protocol of a multi-center RCT. BMC Psychiatry, 18(1), 251. 10.1186/s12888-018-1830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verrill A. (2018). The relationship between childhood abuse and aggressive behavior in adulthood. Journal of Interdisciplinary Undergraduate Research, 10(1), 2. 10.1016/j.biopsycho.2010.09.010 [DOI] [Google Scholar]
- Vögele C., Sorg S., Studtmann M., Weber H. (2010). Cardiac autonomic regulation and anger coping in adolescents. Biological Psychology, 85(3), 465–471. 10.1016/j.biopsycho.2010.09.010 [DOI] [PubMed] [Google Scholar]
- von Borries A. K. L., Volman I., de Bruijn E. R. A., Bulten B. H., Verkes R. J., Roelofs K. (2012). Psychopaths lack the automatic avoidance of social threat: Relation to instrumental aggression. Psychiatry Research, 200(2–3), 761–766. 10.1016/j.psychres.2012.06.026 [DOI] [PubMed] [Google Scholar]
- von Rosenberg W., Chanwimalueang T., Adjei T., Jaffer U., Goverdovsky V., Mandic D. P. (2017). Resolving ambiguities in the LF/HF ratio: LF-HF scatter plots for the categorization of mental and physical stress from HRV. Frontiers in Physiology, 8, 360. 10.3389/fphys.2017.00360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walther J. B. (2008). Social information processing theory. Engaging Theories in Interpersonal Communication: Multiple Perspectives, 391–404. [Google Scholar]
- Zhang T., Chow A., Wang L., Dai Y., Xiao Z. (2012). Role of childhood traumatic experience in personality disorders in China. Comprehensive Psychiatry, 53(6), 829–836. 10.1016/j.comppsych.2011.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zirpoli T. J. (2008). Behavior management: Applications for teachers. Prentice Hall. [Google Scholar]
- Zohar A. H., Cloninger C. R., McCraty R. (2013). Personality and heart rate variability: Exploring pathways from personality to cardiac coherence and health. Open Journal of Social Sciences, 1(06), 32. 10.4236/jss.2013.16007 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ijo-10.1177_0306624X20986537 for The Complex Associations Between Early Childhood Adversity, Heart Rate Variability, Cluster B Personality Disorders, and Aggression by Marija Jankovic, Stefan Bogaerts, Stéphanie Klein Tuente, Carlo Garofalo, Wim Veling and Geert van Boxtel in International Journal of Offender Therapy and Comparative Criminology


