Abstract
Introduction
COVID-19 pandemic has affected the whole world, especially the frontline worriers. To get shielded through this war, the world is racing to reach and manufacture COVID-19 vaccines. Vaccination hesitancy is one of the significant obstacles to global health.
Objectives
This study aimed to assess the perception and attitude of healthcare workers in Egypt toward COVID-19 vaccines, acknowledge the determinants of their attitude, and the factors that could increase the acceptance of the vaccine.
Methods
an observational web-based anonymous survey was conducted on 385 Egyptian healthcare workers in different governorates. The questionnaire-based on Vaccine Hesitancy Survey Questions of the World Health Organization was available in Arabic and English languages and was tested for reliability.
Results
Regarding vaccination decision, 51% of the participants were undecided, 28% refused, and 21% accepted vaccination. Reasons for vaccine acceptance mainly were risks of COVID-19 (93%), safety (57.5%), and effectiveness (56.25%) of the vaccine. Simultaneously, the reasons for vaccine hesitancy were the absence of enough clinical trials (92.4%) and fear of side effects of the vaccine (91.4%). The leading factor that could increase vaccination acceptance among the participants was to get sufficient and accurate information about the available vaccines. The participants revealed a high mean level of concern for COVID-19 vaccines’ safety (3.8 of 5) that differs significantly among the different study groups (P-value .002).
Conclusion
Despite the COVID-19 pandemic, only approximately 21% of Egyptian healthcare workers in our study accepted the COVID-19 vaccination. Vaccine hesitancy represents a major barrier to implementing vaccination programs.
Keywords: COVID-19, vaccination hesitancy, vaccination attitude, pandemic, SARS-CoV-2
Introduction
COVID-19 is the unpredicted strike in which the whole world allied and armed with knowledge and discipline to battle. Over 104 million confirmed cases of COVID-19 and 2.29 million deaths until now (February 6, 2021), as reported by World Health Organization (WHO).1 Despite the global preventive efforts (physical distancing, facemask, travel constraints, and quarantine) to contain the infection, COVID-19 is continuing with its devastating consequences on health, life, and economics. The world’s hopes are attached to a successful preventive measure that is the vaccination which has proved its capability to stop infections and save lives over the years. Near the end of 2020, several vaccines started to arise; there are about 100 candidate vaccines.2 Several vaccines are in the clinical trial phases, and few have already gained Emergency Use Authorization (EUA) (3). The most distributed 6 candidate vaccines are currently in the 3rd phase trial. They differ in composition, storage requirements, and effectiveness (70.4%-95%). No serious adverse effects were reported from those vaccines.3
As a result of the variability in COVID-19 vaccines, there are different directions, perceptions, and attitudes toward the vaccine. Those differences symbolize challenges for governments and public health experts. WHO4 declared vaccination hesitancy as one of the top 10 obstacles for global health. The currently building literature sheds light on the COVID-19 vaccination hesitancy challenge. Several reports from the United States of America (USA), China, the United Kingdom, Ireland, and Congo revealed varied population and healthcare workers’ vaccination acceptance and hesitancy.5-9
In Egypt, there have been 169 640 confirmed cases of COVID-19, with 9651 deaths till now (February 8, 2021).1 The Egyptian government exerts great efforts to provide the COVID-19 vaccines and sort the vaccination as a priority for healthcare workers (HCWs) and older people, especially with chronic diseases. To overcome the expected upcoming challenge of vaccination hesitancy, we have to measure it and know the exact reasons behind it.
In this study, we are targeting the healthcare workers to measure their perception and attitude toward the COVID-19 vaccines. We selected the healthcare workers group as our study population because they are among the priority groups for COVID-19 vaccination. Also, healthcare workers represent the guidance and the trusted source of information of the vaccine for the general population. They can shield against misleading and confusing information. So, their attitude will impact their and others’ health. To our knowledge, this is the first study in Egypt aiming to determine the perception and attitude of healthcare workers, recognize the determinants of their attitude, and factors that could help to increase vaccine acceptance among healthcare workers. This study represents a guide for health authorities and public health experts in Egypt to highlight the expected challenges for COVID-19 vaccination.
Methods
We conducted an observational web-based anonymous survey. The questionnaire was designed using Google Forms and distributed electronically. Data were collected from December 2020 to January 2021 using the most popular online groups of healthcare workers on Facebook and WhatsApp in Egypt. Participants were recruited through different online providers for different governorates to avoid coverage bias and to be a representative sample.
Ethical considerations
This study was approved by the Research and Ethics Committee (REC) of Kasralainy faculty of medicine, Cairo University (ID: 2021-N-13). Participation was entirely voluntary. Anonymity and confidentiality were kept as the study was conducted through a web-based anonymous survey. Electronic informed consent was obtained from all participants through a required question at the beginning of the survey after explaining the objectives and aim.
Study design and population
This web-based survey was conducted on the healthcare workers in Egypt. Healthcare workers are “all people engaged in actions whose primary intent is to enhance health,” as defined by WHO. We included physicians, pharmacists, physiotherapists, dentists, and nursing staff. All healthcare workers of all Egyptian governorates were invited to participate in the study.
Sample size
We calculated the required sample size using Stata statistical software version 16. We assumed the population size (current healthcare workers in Egypt) to be 375 thousand as provided by the most recent report of The Central Agency for Public Mobilization and Statistics (CAPMAS).10 The proportion of the sample with the expected outcome (vaccination acceptance) is 50%, based on recently published literature.11 With a margin of error ±0.5% and a confidence level of 95%, the estimated required sample size is 384.
Study tool
The study tool was provided to the participants in 2 languages: Arabic and English versions. The questionnaire is based on Vaccine Hesitancy Survey Questions by the SAGE working group on vaccination hesitancy (WHO),12 and adapted to suit the current research objectives. Experts checked the consistency, objectivity, and language clarity of the Arabic and English versions. A pilot of 30 participants was invited for each version of the questionnaire, and then reliability testing was done. Cronbach alpha was 0.684 and 0.618 for perception and attitude sections of the Arabic version, respectively, and 0.638, 0.571 for perception and attitude sections of the English version, respectively.
Most of the questions were in the form of “yes and no” questions except for few questions with a third option of “I don’t know,” one five-point rating scale question, and few open-ended questions for participants to express their reasons openly. The questionnaire covered the following parts:
Firstly, it covered socio-demographic information, including age, sex, governorate, educational degree, and specialty. The participants were also asked if they were working in COVID-19 isolation hospital and if they were dealing directly with COVID-19 patients, also, the own previous history of COVID-19 diagnosis.
Secondly, it discussed COVID-19 vaccination perception and attitude (18 questions), asking about sufficiency, trust, sources of information of COVID-19 vaccines, also, their perception of the risks of COVID-19 disease. The pharmaceutical companies and vaccine producers’ primary interest, trust, and transparency in discussing the side effects were also asked questions. The level of the participants’ concern of vaccine safety was asked, and the response was recorded on a five-point rating scale (1 “Not concerned,” 2 “Mildly concerned,” 3 “Moderately concerned,” 4 “Considerably concerned,” 5 “Highly concerned”). The survey questioned the participants’ attitude toward non-obligatory vaccine in general if its cost could affect their decision, COVID-19 vaccine recommendations to others—finally, the decision to receive COVID-19 vaccine with 3 options either yes, no, or undecided. (NB. The term vaccine hesitancy refers to “delay in acceptance or refusal of vaccines despite availability of vaccination services” as defined by WHO. Still, it was used variably in various studies. In our study, we used the term hesitant for the undecided group).
Thirdly, the participants were asked for the reasons behind their vaccination decision.
Fourthly, the participants refusing and hesitant to take the COVID-19 vaccine were asked about the factors that could help to increase the vaccination acceptance from their point of view.
Statistical analysis
Categorical variables were described in numbers and percentages, while numerical variables in mean and standard deviation. Association of participants’ perception and attitude with their decision regarding COVID-19 vaccination were done using Chi-Square test. Significant variables were tested using univariate multinomial regression. Then we controlled for specific confounders (age, sex, governorate, job, degree, working in an isolation hospital, dealing directly with COVID-19 patients, own previous history of COVID-19 diagnosis), and multivariate multinomial regression was done. For testing the level of concern about COVID-19 vaccines’ safety difference among the 3 groups (accepting, refusing, and hesitant), we used one-way ANOVA.
Results
A total of 385 responses were received, representing a random sample of the healthcare workers from different governorates in Egypt.
The majority of the responses regarding COVID 19 vaccination decision reported undecided (51%), while 28% and 21% decided no and yes, respectively.
As listed in Table 1. The majority of our participants were females in the 17 to 35 age group, living in different governorates. Nearly half of the participants were physicians. About 60% of participants had post-graduate studies. More than 40% of the participants were working in COVID-19 isolation hospitals or dealing directly with COVID-19 patients. About 37.66% of the participants were previously diagnosed as COVID-19 cases.
Table 1.
Participant’s Characteristics and Association with COVID-19 Vaccination Decision (n = 385).
| Total n (%) | Yes | Undecided | No | P-value* | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Age group | |||||
| 17-35 | 271 (70.39) | 57 (21.03) | 137 (50.55) | 77 (28.41) | .864 |
| 36-66 | 114 (29.61) | 23 (20.18) | 61 (53.51) | 30 (26.32) | |
| Gender | |||||
| Female | 313 (81.30) | 52 (16.61) | 171 (54.63) | 90 (28.75) | <.001 |
| Male | 72 (18.70) | 28 (38.89) | 27 (37.50) | 17 (23.61) | |
| Governorate | |||||
| Cairo | 102 (26.49) | 26 (25.49) | 52 (50.98) | 24 (23.53) | .602 |
| Dakahlia | 114 (29.61) | 19 (16.67) | 62 (54.39) | 33 (28.95) | |
| Giza | 47 (12.21) | 12 (25.53) | 25 (53.19) | 10 (21.28) | |
| Damietta | 46 (11.95) | 9 (19.57) | 21 (45.65) | 16 (34.78) | |
| Menofia | 10 (2.60) | 2 (20.00) | 3 (30.00) | 5 (50.00) | |
| Others | 66 (17.14) | 12 (18.18) | 35 (53.03) | 19 (28.79) | |
| Job | |||||
| Physician | 192 (49.87) | 47 (24.48) | 98 (51.04) | 47 (24.48) | .237 |
| Nursing Staff | 89 (23.12) | 10 (11.24) | 50 (56.18) | 29 (32.58) | |
| Pharmacist | 87 (22.60) | 21 (24.14) | 39 (44.83) | 27 (31.03) | |
| Dentist | 13 (3.38) | 2 (15.38) | 8 (61.54) | 3 (23.08) | |
| Physiotherapist | 4 (1.04) | 0 (00.00) | 3 (75.00) | 1 (25.00) | |
| Educational Degree | |||||
| Baccalaureate degree | 154 (40.00) | 28 (18.18) | 78 (50.65) | 48 (31.17) | .258 |
| Professional Diploma | 35 (9.09) | 7 (20.00) | 13 (37.14) | 15 (42.86) | |
| Master’s degree | 115 (29.87) | 24 (20.87) | 65 (56.52) | 26 (22.61) | |
| MD degree | 67 (17.40) | 18 (26.87) | 33 (49.25) | 16 (23.88) | |
| Working in the COVID-19 isolation hospital | |||||
| No | 227 (58.96) | 47 (20.70) | 121 (53.30) | 59 (25.99) | .599 |
| Yes | 158 (41.04) | 33 (20.89) | 77 (48.73) | 48 (30.38) | |
| Dealing directly with COVID-19 patients | |||||
| No | 227 (58.96) | 33 (14.54) | 131 (57.71) | 63 (27.75) | .001 |
| Yes | 158 (41.04) | 47 (29.75) | 67 (42.41) | 44 (27.85) | |
| Diagnosed as COVID-19 suspected or confirmed patient | |||||
| No | 240 (62.34) | 48 (20.00) | 131 (54.58) | 61 (25.42) | .258 |
| Yes | 145 (37.66) | 32 (22.07) | 67 (46.21) | 46 (31.72) | |
P-value is considered significant if <.05.
We found that gender and dealing directly with COVID-19 patients are notably significant factors with a P-value <.001. Surprisingly, age, governorates, job, educational degree, working in a COVID-19 isolation hospital, and being diagnosed as COVID-19 suspected or confirmed patients were not significant factors for COVID-19 vaccination decision with P-value .864, .602, .237, .258, .599, and .258, respectively.
As shown in Table 2, most responders (75.06%) did not get sufficient information about the COVID-19 vaccine, and 79% do not trust their information. Colleagues, social media, and published scientific articles were respectively the most common sources of information. Nearly 92% accepted that COVID-19 is a dangerous disease.
Table 2.
COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt (n = 385).
| Total n (%) | Yes | Undecided | No | P-value* | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Getting sufficient information about the COVID-19 vaccine | |||||
| No | 298 (75.06) | 50 (17.30) | 159 (55.02) | 80 (27.68) | .008 |
| Yes | 96 (24.94) | 30 (31.25) | 39 (40.63) | 27 (28.13) | |
| Trusting the information about the COVID-19 vaccine | |||||
| No | 305 (79.22) | 40 (13.11) | 173 (56.72) | 92 (30.16) | <.001 |
| Yes | 80 (20.78) | 40 (50.00) | 25 (31.25) | 15 (18.75) | |
| The sources of information about the COVID-19 vaccine | |||||
| Published scientific articles | 239 (62.08) | 57 (23.85) | 118 (49.37) | 64 (26.78) | .164 |
| Social media | 299 (77.66) | 56 (18.73) | 153 (51.17) | 90 (30.10) | .071 |
| Mass media | 206 (53.51) | 45 (21.84) | 110 (53.40) | 51 (24.76) | .360 |
| Colleagues | 304 (78.96) | 62 (20.39) | 161 (52.96) | 81 (26.64) | .485 |
| Others | 80 (20.78) | 17 (21.25) | 42 (52.50) | 21 (26.25) | .942 |
| COVID-19 is a dangerous disease | |||||
| No | 29 (7.53) | 7 (24.14) | 15 (51.72) | 7 (24.14) | .852 |
| Yes | 356 (92.47) | 73 (20.51) | 183 (51.40) | 100 (28.09) | |
| Needing the vaccine to build your immunity | |||||
| No | 186 (48.31) | 10 (5.38) | 85 (45.70) | 91 (48.92) | <.001 |
| Yes | 199 (51.69) | 70 (35.18) | 113 (56.78) | 16 (8.04) | |
| It is a community responsibility to get vaccinated. | |||||
| No | 160 (41.56) | 8 (5.00) | 67 (41.88) | 85 (53.13) | <.001 |
| Yes | 225 (58.44) | 72 (32.00) | 131 (58.22) | 22 (9.78) | |
| Celebrities’ or leaders’ advocation of COVID-19 vaccination could affect your decision. | |||||
| No | 267 (69.35) | 35 (13.11) | 134 (50.19) | 98 (36.70) | <.001 |
| Yes | 118 (30.65) | 45 (38.14) | 64 (54.24) | 9 (7.63) | |
| Recommending COVID-19 vaccination for family, friends, or patients | |||||
| No | 223 (57.92) | 7 (3.14) | 119 (53.36) | 97 (43.50) | <.001 |
| Yes | 162 (42.08) | 73 (45.06) | 79 (48.77) | 10 (6.17) | |
| Getting non-obligatory vaccinations | |||||
| No | 188 (48.83) | 24 (12.77) | 100 (53.19) | 64 (34.04) | <.001 |
| Yes | 197 (51.17) | 56 (28.43) | 98 (49.75) | 43 (21.83) | |
| The vaccination cost could affect your decision of vaccination. | |||||
| No | 276 (71.69) | 51 (18.48) | 139 (50.36) | 86 (31.16) | .035 |
| Yes | 109 (28.31) | 29 (26.61) | 59 (54.13) | 21 (19.27) | |
| Hearing of anyone with a bad reaction related to COVID-19 vaccination | |||||
| No | 196 (50.91) | 46 (23.47) | 111 (56.63) | 39 (19.90) | .002 |
| Yes | 189 (49.09) | 34 (17.99) | 87 (46.03) | 68 (35.98) | |
| This situation affected your decision for the COVID-19 vaccination. | |||||
| No | 148 (47.28) | 38 (25.68) | 68 (45.95) | 42 (28.38) | .104 |
| Yes | 165 (52.72) | 28 (16.97) | 93 (56.36) | 44 (26.67) | |
| Your hospital or medical center advice to get the vaccine | |||||
| No | 176 (45.71) | 24 (13.64) | 92 (52.27) | 60 (34.09) | .002 |
| Yes | 209 (54.29) | 56 (26.79) | 106 (50.72) | 47 (22.49) | |
| The vaccine producers are interested primarily in your health. | |||||
| I do not know | 192 (49.87) | 18 (9.38) | 110 (57.29) | 64 (33.33) | <.001 |
| No | 70 (18.18) | 7 (10.00) | 35 (50.00) | 28 (40.00) | |
| Yes | 123 (31.95) | 55 (44.72) | 53 (43.09) | 15 (12.20) | |
| Trusting the pharmaceutical companies for producing a safe and effective vaccine | |||||
| I do not know | 159 (41.30) | 19 (11.95) | 93 (58.49) | 47 (29.56) | <.001 |
| No | 132 (34.29) | 11 (8.33) | 66 (50.00) | 55 (41.67) | |
| Yes | 94 (24.42) | 50 (53.19) | 39 (41.49) | 5 (5.32) | |
| Information about side effects is discussed openly by authorities. | |||||
| I do not know | 97 (25.19) | 12 (12.37) | 66 (68.04) | 19 (19.59) | <.001 |
| No | 240 (62.34) | 36 (15.00) | 123 (51.25) | 81 (33.75) | |
| Yes | 48 (12.47) | 32 (66.67) | 9 (18.75) | 7 (14.58) | |
P-value is considered significant if <.05.
Being vaccinated would help build immunity, and if it is a community responsibility to get vaccinated were significantly associated with the vaccination decision (P-value <.001 and <.001, respectively). Celebrities and leaders’ advocation of the COVID-19 vaccine would not affect the participants’ decision to get the vaccine (69.3%). Furthermore, for recommending the COVID-19 vaccine for family, friends, or patients, the responses went to no (57.9%) and yes (42.08%), which was also a significantly associated factor with the vaccination decision.
Hearing about bad reactions of COVID-19 vaccine (P = .002) was significantly important in the decision. Also, 52.7% of participants agreed that this reaction affected their vaccination decision.
Regarding authorities’ and vaccine producers’ attitude, trusting that vaccine producers are interested primarily in patient’s health or that pharmaceutical companies could produce safe and effective vaccines were most answered by “I don’t know.” When asking if information about the side effects is discussed openly by authorities, the majority went to “no” (62.3%), then “I do not know” (25.1%). Their hospitals or centers advised about 54.2 % of participants to accept the vaccine.
Table 3 shows the multinomial regression analysis results for the decision determinants for COVID-19 vaccination in the accepting (Yes) and refusing (No) groups compared to the hesitant group.
Table 3.
Multinomial Logistic Regression for COVID-19 Vaccination Decision Determinants.
| Yes | No | |||
|---|---|---|---|---|
| Adjusted OR* (95% CI) | P# | Adjusted OR (95% CI) | P | |
| Gender (Male) | 3.11 (1.59-6.10) | .001 | 1.19 (0.59-2.39) | .632 |
| Dealing directly with COVID-19 patients (Yes) | 2.28 (1.28-4.08) | .005 | 1.43 (0.85-2.42) | .181 |
| Getting sufficient information about COVID-19 vaccine (Yes) | 2.78 (1.45-5.30) | .002 | 1.44 (0.79-2.63) | .235 |
| Trusting the information about COVID-19 vaccine (Yes) | 9.18 (4.54-18.53) | <.001 | 1.20 (0.57-2.49) | .631 |
| Needing the vaccine to build your immunity (Yes) | 4.99 (2.29-10.86) | <.001 | 0.10 (0.05-0.19) | <.001 |
| It is a community responsibility to get vaccinated (Yes) | 3.69 (1.62-8.40) | .002 | 0.10 (0.06-0.19) | <.001 |
| Leaders’ advocation of COVID-19 vaccination could affect your decision (Yes) | 4.54 (2.38-8.64) | <.001 | 0.15 (0.07-0.35) | <.001 |
| Recommending COVID-19 vaccination for others (Yes) | 16.55 (6.92-39.59) | <.001 | 0.12 (0.06-0.27) | <.001 |
| Getting non-obligatory vaccinations (Yes) | 2.55 (1.38-4.70) | .003 | 0.66 (0.39-1.10) | .112 |
| The vaccination cost could affect your decision of vaccination (Yes) | 0.95 (0.52-1.74) | .867 | 0.43 (0.23-0.79) | .007 |
| Heard of bad reaction related to COVID-19 vaccination (Yes) | 0.84 (0.48-1.49) | .554 | 2.19 (1.31-3.64) | .003 |
| Your hospital or medical center advice to get the vaccine (Yes) | 2.45 (1.33-4.51) | .004 | 0.62 (0.37-1.04) | .069 |
| The vaccine producers are interested primarily in health. | ||||
| No | 1.17 (0.41-3.32) | .774 | 1.83 (0.95-3.54) | .071 |
| Yes | 10.79 (5.02-23.18) | <.001 | 0.42 (0.20-0.87) | .019 |
| Trusting the pharmaceuticals for a safe and effective vaccine | ||||
| No | 0.80 (0.33-1.92) | .612 | 1.94 (1.13-3.35) | .017 |
| Yes | 8.83 (4.09-19.07) | <.001 | 0.23 (0.08-0.64) | .005 |
| Information about side effects is discussed openly by authorities. | ||||
| No | 1.80 (0.82-3.96) | .141 | 3.19 (1.68-6.04) | <.001 |
| Yes | 22.50 (7.78-65.07) | <.001 | 3.03 (0.94-9.70) | .062 |
OR: odds ratio.
95% CI: 95% confidence interval.
#P value is considered significant if ≤.05.
For the accepting group, being male and dealing directly with COVID-19 patients showed nearly 3 times higher odds of accepting the vaccination compared to females and those who are not dealing directly (OR 3.11 and 2.28, 95% CI 1.59-6.10 and 1.28-4.08, 0.001 and 0.005, respectively). Participants who took non-compulsory vaccines and those who recommended COVID-19 vaccination to others were 3 and 17 times more likely to accept COVID-19 vaccination (OR 2.55 and 16.55, 95% CI 1.38-4.70 and 6.92-39.59, 0.003 and <0.001, respectively). Participants who received advice from their hospitals to get the vaccine had 2.5 higher odds to accept the vaccine (OR 2.45, 95% CI 1.33-4.51, 0.004). Participants showed trust in vaccine producers, pharmaceutical companies, and authorities had higher odds for vaccination acceptance (OR 10.79, 8.83, and 22.50, 95% CI 5.02-23.18, 4.09-19.07, and 7.78-65.07, <0.001, <0.001, and <0.001, respectively).
For the refusing group, the participants who heard of anyone with a bad reaction related to COVID-19 vaccination were 2 times more likely to refuse the vaccine (OR 2.19, 95% CI 1.31-3.64, 0.003) compared to those who did not hear of it. Participants who did not trust pharmaceutical companies to produce a safe and effective vaccine and who did not believe that the side effects are discussed openly were 2 and 3 times more likely to refuse COVID-19 vaccination (OR 1.94 and 3.19, 95% CI 1.13-3.35 and 1.68-6.04, 0.017 and <0.001, respectively).
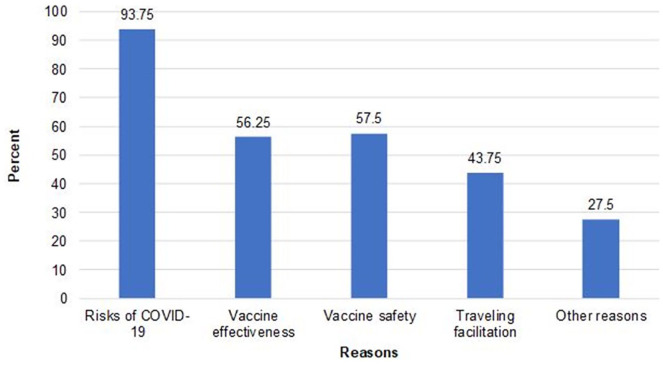
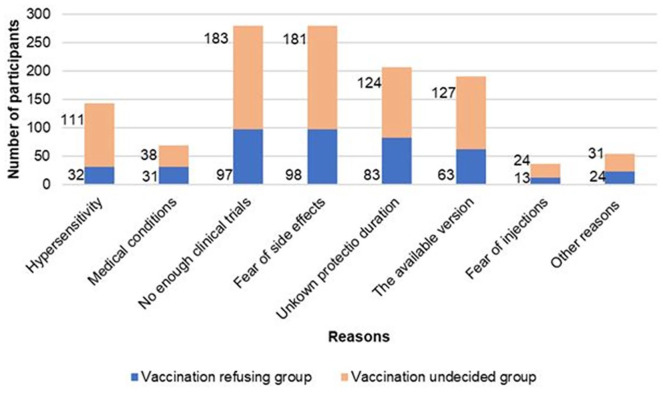
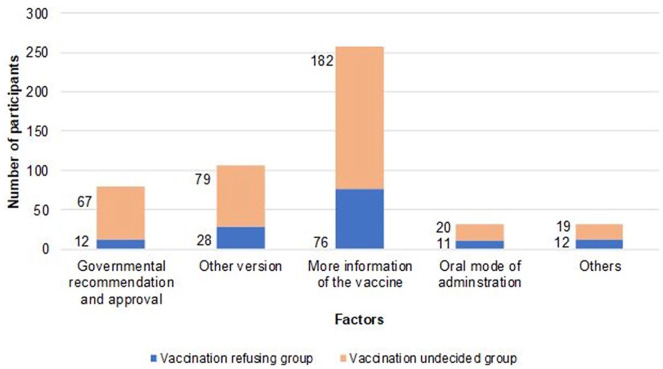
As shown in Figure 1, reasons for vaccine acceptance were found to be basically due to risks of COVID-19 (93%), followed by the safety of the vaccine (57.5%), the effectiveness of the vaccine (56.25%), traveling facilitation (43.75%). While the reasons for vaccine hesitancy and refusing were lack of enough clinical trials (92.4%) and fear of vaccine’s side effects (91.4%), as shown in Figure 2. The unknown protection and immunity duration and the rumors about the vaccine’s available version in Egypt were also substantial hindering factors for vaccination acceptance. The leading factor that could increase vaccination acceptance among our study participants was to get sufficient and accurate information about the available vaccines, as revealed in Figure 3.
Figure 1.
Reasons of COVID-19 vaccination acceptance among healthcare workers.
Figure 2.
Reasons of vaccination refusal and vaccination hesitancy among healthcare workers.
Figure 3.
Factors helping in vaccination acceptance.
The participants showed a high level of concerns for COVID-19 vaccines safety (on a scale from 1 to 5) as 34.8% were highly concerned while only 4.6% revealed no concerns. The mean level of concern differs significantly among the different groups, where it was 2.9 in the accepting group, 3.9 in the hesitant group, and 4.3 in the refusing group (P-value .002).
Discussion
Healthcare workers’ perception and attitude to COVID 19 vaccines play an essential role in the general population’s vaccination behavior through their consultation. The diversity of representation from both genders, age groups, categories in healthcare, and proximity in dealing with COVID-19 patients represents strength in this study. This study represents a guide for health authorities and public health experts in Egypt to enable them to maximize acceptance of COVID-19 vaccination.
In this study, only 21% of the participants agreed to get a vaccine against COVID-19, 28% disagreed, while nearly half of the participants were in the undecided group. This low acceptance agreed with the Congo study that found the acceptance of COVID-19 vaccination among healthcare workers to be only 28%.9 It also agreed with the study conducted in the USA with 36% acceptance and 56% hesitancy.13 Meanwhile, our findings were against the study conducted in France, where 77.6% of participants “probably agreed” to get vaccinated.14 Also, this disagreed with Barry et al,15 who carried out a study to assess COVID-19 vaccine confidence in a MERS-CoV experienced nation and found that two-thirds of HCWs expressed willingness to receive a potential COVID-19 vaccine.
Regarding gender, the results agreed with other studies where the odds of acceptance of vaccination among males were significantly higher compared to females.14 This could be explained by that nearly 60% of the males in the current study were physicians and dealing directly with COVID-19 patients, which led to the high probability of vaccination acceptance. Dealing directly with COVID-19 patients led to 3 times higher odds of acceptance. This agreed with the study in the USA where HCWs who had not taken care of COVID-19 patients had higher rates of vaccine refusal.13
Regarding the age, it was insignificantly associated with the decision of vaccination. This was incompatible with Grech et al,11 where higher uptake of a COVID-19 vaccine was in the oldest age group as they are the more vulnerable group and therefore more likely to accept the vaccine. In this study, hesitancy related to the COVID-19 vaccine was indifferent among categories of HCWs (P-value .237), disagreeing with the study revealing that hesitancy was greater among nurses than physicians.6
In the current study, most of the respondents (75.06%) believed that they did not get sufficient information about COVID-19 vaccines, and 79% of them did not trust the information they got. This was following the study in the USA where a high percentage of HCWs did not trust information about COVID-19 and its severity, also by the regulatory authorities and pharmaceutical companies for vaccine development and safety.13 Like other studies, colleagues, social media, and published scientific articles were respectively the most common sources of information in this study.13
As a reflection of participants’ expected attitude toward COVID-19 vaccines, the researchers asked the participants the non-obligatory vaccines and its cost. Participants who got non-obligatory vaccines were 3 times more likely to accept the COVID-19 vaccination, agreeing with other studies.11,13 The current study participants agreed with HCWs in the USA who were worried about the out-of-pocket cost of the COVID-19 vaccine.13
The participants who recommended COVID-19 vaccination for others were 17 times more likely to accept COVID-19 vaccination and 88% less likely to refuse vaccination. This agreed with the study carried by Shekhar et al,13 whose study showed that HCWs who are vaccinated are more likely to recommend vaccines to others.
Regarding reasons of acceptance among those who decided to receive the vaccine once it becomes available, the risk associated with COVID-19 disease was the most prevalent reason. While, for reasons of vaccination refusing and hesitancy, the commonest reason was insufficient knowledge about its safety and absence of enough clinical trials. This was compatible with almost all studies done for the assessment of COVID 19 vaccination hesitancy.6,11,14
In the current study, the participants showed a high level of concern for COVID-19 vaccine safety that differed significantly among the different groups. This agreed with Dodd et al16 study in Australia, where concern about the vaccine’s safety was 36% among the hesitancy group and 11% among those who were willing to get the vaccination. Concerns for vaccination safety, effectiveness, and duration of trials and testing were common findings in many studies.5,13
The leading factor that could increase vaccination acceptance among this study participants was to get sufficient and accurate information about the available vaccines. This finding which revealed the major obstacle for vaccination acceptance, actually represented the solution that could be quickly adopted and provided by the authorities to maximize vaccination acceptance and coverage.
The governmental approval and recommendation of the vaccine was the third factor. This was in contrast with the results of Qiao et al,17 where the hesitant college students had greater scores on authoritative advice factors such as school/college, government, and doctors. This contrast may be referred to the different study population.
Public health authorities and the government in Egypt have a heavy mission for implementing successful vaccination programs with high coverage. WHO recommended prior planning for any vaccination program to ensure high acceptance.18 A successful plan should adopt 2 main approaches; the first is prioritizing population categories in need of vaccination that was already designed and declared by Egyptian authorities; the other highly impactful approach is to alleviate any concerns related to vaccination and increase the awareness and demand of vaccination.19 The current study provides the authorities with deep insights into the expected obstacles, concerns, and approaches for solutions to reach the desirable vaccination coverage.
There are some limitations of the current study. Firstly, the use of an online survey may result in sampling bias, but this was the available way in the current situations. Notably, females and adults between 17 and 35 were over-represented in this study. It is also noteworthy that the assessment of intention to vaccinate in this study did not account for the other possible factors affecting vaccination decision, such as duration of protection of the vaccine and the need for booster doses, which could influence participants’ decision.
Conclusion
Despite the COVID-19 pandemic, only approximately 21% of Egyptian healthcare workers in the current study accepted to get COVID-19 vaccines. In the context of a pandemic, vaccine hesitancy represents a major barrier to implementing vaccination programs. In this study, we concluded that the absence of enough clinical trials and the fear of the vaccine’s side effects were the significant reasons for vaccine hesitancy and refusal. The leading factor that could increase vaccination acceptance was to get sufficient and accurate information about the available vaccines. The current study provides the authorities with deep insights into the expected obstacles, concerns, and approaches for solutions.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors declare absence of conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Samar Fares  https://orcid.org/0000-0002-3438-1329
https://orcid.org/0000-0002-3438-1329
Radwa Elsayed  https://orcid.org/0000-0002-3219-3703
https://orcid.org/0000-0002-3219-3703
References
- 1. World Health Organization. COVID-19 dashboard. who.int. Update February 2021. Accessed February 6, 2021. https://covid19.who.int/
- 2. World Health Organization. DRAFT landscape and tracker of COVID-19 candidate vaccines. who.int. Update February 2021. Accessed February 12, 2021. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
- 3. Ferbeyre G, Santiago Vispo N. The race for a coronavirus vaccine. Bionatura. 2020;5:1290-1292. doi: 10.21931/rb/2020.05.04.1 [DOI] [Google Scholar]
- 4. World Health Organization. Ten threats to global health in 2019. Who.int. Update February 2021. Accessed February 12, 2021. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- 5. Pogue K, Jensen J, Stancil C, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines (Basel). 2020;8:582. doi: 10.3390/vaccines8040582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gadoth A, Halbrook M, Martin-Blais R, et al. Cross-sectional assessment of COVID-19 vaccine acceptance among health care workers in Los Angeles. Ann Intern Med. Published online February 9, 2021. doi: 10.7326/m20-7580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong L. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020;14:e0008961. doi: 10.1371/journal.pntd.0008961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Murphy J, Vallières F, Bentall R, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12:29. doi: 10.1038/s41467-020-20226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res. 2020;11:103-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. CAPMAS, Egypt. Statistical yearbook. capmas.gov.eg. Update 2019. Accessed January 2021. https://www.capmas.gov.eg/Pages/Publications.aspx?page_id=5104&Year=23479
- 11. Grech V, Gauci C, Agius S. Withdrawn: vaccine hesitancy among Maltese Healthcare workers toward influenza and novel COVID-19 vaccination. Early Hum Dev. Published online October 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization. Vaccine hesitancy survey questions related to SAGE vaccine hesitancy matrix. who.int. Update 2014. Accessed January 2021 https://www.who.int/immunization/programmes_systems/Survey_Questions_Hesitancy.pdf
- 13. Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines (Basel). 2021;9:119. doi: 10.3390/vaccines9020119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002-7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barry M, Temsah M-H, Alhuzaimi A, et al. COVID-19 vaccine confidence and hesitancy among healthcare workers: a cross-sectional survey from a MERS-CoV experienced nation. bioRxiv. Published online 2020. doi: 10.1101/2020.12.09.20246447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dodd RH, Pickles K, Nickel B, et al. Concerns and motivations about COVID-19 vaccination. Lancet Infect Dis. 2021;21:161-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Qiao S, Friedman DB, Tam CC, Zeng C, Li X. Vaccine acceptance among college students in South Carolina: do information sources and trust in information make a difference? medRxiv. Published online 2020. doi: 10.1101/2020.12.02.20242982 [DOI] [PubMed] [Google Scholar]
- 18. World Health Organization. Tailoring immunization programmes. who.int. Update May 2018. Accessed February 17, 2021. https://www.who.int/immunization/programmes_systems/Global_TIP_overview_July2018.pdf?ua=1
- 19. French J, Deshpande S, Evans W, Obregon R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int J Environ Res Public Health. 2020;17:5893. [DOI] [PMC free article] [PubMed] [Google Scholar]