Abstract
Background:
Although Bankart repair with remplissage is commonly performed to treat anterior shoulder instability, there is limited information on specific outcomes or patients’ fears regarding return to sports (RTS).
Purpose:
To study recurrence rates, pain, shoulder function, active range of motion (ROM), RTS rate, and patients’ fears and expectations for RTS after arthroscopic Bankart repair with remplissage for anterior shoulder instability. We compared these outcomes with those after Bankart repair alone.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective cohort study was carried out between 2007 and 2017 among patients who underwent arthroscopic Bankart repair with remplissage (group BR) and Bankart repair alone (group B). At the final follow-up, outcomes including recurrence, pain, shoulder function, active ROM, RTS rate, and fear toward RTS were assessed. The specific outcomes for RTS were evaluated based on 3 levels: return to normal life, RTS at any level (RTSA), and RTS at previous level (RTSP).
Results:
A total of 70 patients were included (29 in group BR and 41 in group B) with a mean 67.2 months of follow-up. Group BR demonstrated a significantly lower recurrence rate than did group B (0 vs 22.0%, respectively; P = .007) as well as higher postoperative Rowe score (92.8 ± 7.1 vs 83.3 ± 16.2, respectively; P = .005). There were no differences between the groups in postoperative visual analog scale for pain score, American Shoulder and Elbow Surgeons score, Oxford Shoulder Instability Score, or active ROM. The rates of RTSA (100% vs 84.2%; P = .03) and RTSP (77.8% vs 50.0%; P = .02) were higher in group BR than in group B, respectively, and significantly fewer patients in group BR reported fear of RTS (40.7% vs 63.2%; P = .04).
Conclusion:
In this study, recurrence rate, pain, shoulder function, active ROM, and RTS rate were satisfactory after arthroscopic Bankart repair with remplissage. Patients who underwent this procedure reported less fear toward RTS and higher rates of RTSA and RTSP than did those who undergo Bankart repair alone.
Keywords: anterior shoulder instability, arthroscopy, remplissage, Bankart repair, return to sport
Patients who experience recurrent anterior shoulder instability usually have difficulty in daily activities and avoid sports participation. To date, arthroscopic Bankart repair has been adopted as a major surgical procedure to treat the “essential lesion” of the anteroinferior glenoid labrum for shoulder stabilization.5 In addition, an extra procedure called remplissage (“to fill” in French)29 can be conducted when the patient has a Hill-Sachs lesion, which is a risk factor for recurrent shoulder instability.3,31,36
Previous studies have reported excellent clinical outcomes for arthroscopic Bankart repair with remplissage, revealing low recurrence rates (0%-5%) and high postoperative functional scores.6–8,16,23,27,35,37 However, concerns remain regarding loss of range of motion (ROM), poor healing of tissues, and possible negative effects upon return to sports (RTS), especially among overhead athletes.11,17 Several studies have shown significant loss of external rotation after remplissage,11,17 whereas others have not found a significant difference.8,15,16
Notably, increasing importance has been attached to whether patients are capable of returning to sports at their preinjury level after a relatively short recovery period.22,34 Although high rates of RTS after arthroscopic Bankart repair with remplissage have been reported,1,10,16 a control group is needed with midterm to long-term follow-up was expected to be further included. Furthermore, most studies have demonstrated only the rate and time of RTS in general, without detailed analysis according to specific sports.1,6,11,16 Therefore, it is important to carry out a study assessing sports type, level, and intensity as well as patients’ fears and expectations after arthroscopic stabilization in order to achieve an overall evaluation of RTS.
The purpose of this study was to investigate the outcomes after arthroscopic Bankart repair with remplissage, with a focus on RTS outcomes and patients’ fears and expectations. We compared the outcomes of these patients with those of a parallel control group, endeavoring to optimize the treatment of anterior shoulder instability. It was hypothesized that pain, outcome measures, active ROM, RTS rate, and ability to overcome fears would be satisfactory after arthroscopic Bankart repair with remplissage and would be similar to outcomes after Bankart repair alone.
Methods
Study Design
The retrospective and nonrandomized study was approved by the health sciences institutional review board of our hospital, and informed consent was obtained from all participants. Patients were included between September 2007 and November 2017 if they satisfied the following criteria: (1) experienced anterior shoulder instability with a Bankart lesion or an anterior labrum periosteal sleeve avulsion lesion in the affected shoulder, (2) underwent arthroscopic Bankart repair with or without the remplissage procedure, and (3) could be evaluated at least 2 years after surgery using postoperative assessments.
The exclusion criteria were as follows: (1) posterior or multidirectional shoulder instability; (2) previous stabilization surgery of the affected shoulder; (3) open surgery, arthroscopic bone block transplant, or acromioplasty; (4) rotator cuff tear, frozen shoulder, glenoid bone defect >25% in size, rupture of the long head of biceps tendon; and (5) age <13 or >50 years at the time of surgery. Subsequently, the patients were allocated to 2 groups according to the surgical technique: group BR for arthroscopic Bankart repair with remplissage and group B for arthroscopic Bankart repair alone.
Surgical Technique
All arthroscopic shoulder stabilization procedures were performed by a senior surgeon (S.C.) with assistants, using previously established surgical methods; patients were under general anesthesia and were placed in the lateral decubitus position.13,27 A dynamic evaluation of the Hill-Sachs lesion was performed during arthroscopic surgery with the affected arm positioned at 90° of abduction and 90° of external rotation. When the Hill-Sachs lesion engaged with the anterior glenoid rim or had a tendency to become engaging, it was treated using an additional remplissage procedure.9 No bone grafting was needed when the glenoid bone loss was <25% in size (calculated on preoperative magnetic resonance imaging or 3-dimensional computed tomography scan and confirmed during arthroscopic surgery). In addition, any superior labral anterior posterior lesion was assessed and repaired if needed.
Postoperative Rehabilitation
Using the same protocol, all patients were instructed to place the operated arm in a sling (10° of external rotation and 15° of abduction) for 6 weeks. No arm rise was allowed for at least 4 weeks. Passive shoulder flexion, external rotation, and isometric strengthening exercises were gradually assigned. After discharge, patients were required to visit the clinic and rehabilitation center for follow-up at 2 weeks, 4 weeks, and 8 weeks after surgery. Wall slides, internal rotation stretching, and abduction-external rotation stretching were initiated within 3 months. After 6 months, preinjury activities were permitted.
Data Collection
The preoperative evaluation was performed on admission, and the operation-related information was reviewed from medical records. The collected data were double confirmed with the patients during follow-up. Preoperative assessments included visual analog scale (VAS) for pain; Rowe score32; and active ROM including forward flexion, abduction, external rotation at 90° of abduction, and internal rotation of both shoulders. Postoperative outcomes included VAS, Rowe score, American Shoulder and Elbow Surgeons (ASES) score,24 Oxford Shoulder Instability Score (OSIS),12 active ROM, and RTS.
Postoperative Outcome Evaluations
At the final follow-up, patients were assessed in detail through patient-reported outcome surveys (functional scoring and RTS questionnaires) as well as clinical examination of active ROM. Recurrence was defined as postoperative shoulder dislocations, with number, time, and causes of dislocation events reported by the patients. Subjective pain was scored by VAS and ranged from 0 (no pain) to 10 (extreme pain). Active shoulder ROM was measured by blinded assistance (M.C.) using standard criteria. General postoperative complications such as infection, neurovascular injury, and anchor displacement were also evaluated. In the RTS questionnaire, the patients were asked to respond yes or no to (1) whether they had a sense of fear about returning to sports after the stabilization surgery and (2) whether their expectations for RTS were fulfilled by the stabilization surgery. The number of positive responses was recorded.
The outcomes for RTS were evaluated based on 3 levels: (1) return to normal life (RTL; defined as resumption of daily activities using the operated arm); (2) RTS at any level (RTSA; defined as RTS at lower, average, or previous intensity); (3) RTS at previous level (RTSP; defined as RTS at preoperative or preinjury level). The patients who did not participate in sports preoperatively were assessed for only RTL. Time to RTS was counted from the day of surgery to the day when the patient resumed sports. Sports were classified into 3 types20: (1) minimal shoulder demands (eg, cycling, jogging, fishing), (2) moderate shoulder demands (eg, skiing, swimming, fitness exercise, soccer), and (3) high shoulder demands (eg, martial arts, tennis, badminton, volleyball, basketball).
Statistical Analysis
A sample size estimation was performed before patient involvement, and the RTSA rate was selected as the endpoint using an established formula using data from 2 previously published studies.11,28 The ratio (7:8) of patient number between groups was based on the proportion of patients who underwent the 2 procedures during the study period. As calculated, the minimum number of patients was 29 in group BR and 33 in group B for the difference to reach a level of statistical significance (P < .05) under a statistical power of 0.9 and an α level of .05. Statistical analyses were performed using SPSS Statistical Software (Version 23; IBM Corp) and Excel Office 365 (Microsoft Corp), with a 95% confidence level. Continuous variables were compared using 2-tailed t tests and are reported as means and SDs. Categorical variables were compared using χ2 tests and are reported as counts and frequencies. P < .05 was regarded as statistically significant.
Results
Patient Characteristics
A total of 92 patients met the inclusion criteria, and 70 patients were available for the final follow-up (29 in group BR and 41 in group B), with a 24% loss to follow-up. The mean age at surgery of all patients was 26.3 years, and the mean follow-up time was 67.2 months. No general complications were found at the final follow-up. Patient characteristics are shown in Table 1.
Table 1.
Patient Characteristicsa
| Group BR (n = 29) | Group B (n = 41) | P | |
|---|---|---|---|
| Age at surgery, y | 27.3 ± 6.6 | 25.5 ± 6.6 | .28 |
| Follow-up time, mo | 58.6 ± 26.6 | 73.3 ± 39.3 | .09 |
| Sex, male/female, n | 23/6 | 35/6 | .51 |
| Body mass index | 24.0 ± 3.2 | 24.2 ± 3.3 | .79 |
| Arm dominance, n (%) | 15 (51.7) | 29 (70.7) | .10 |
| No. of preoperative dislocations | 7.2 ± 3.0 | 6.6 ± 5.1 | .61 |
| Age at initial instability, y | 22.2 ± 5.6 | 21.3 ± 6.4 | .54 |
| Duration of symptoms, mo | 60.4 ± 49.5 | 49.2 ± 57.6 | .47 |
| Reason for initial instability, n (%) | |||
| Competitive sports | 16 (55.2) | 18 (43.9) | .35 |
| Noncompetitive sports | 4 (13.8) | 5 (12.2) | .84 |
| Falling | 3 (10.3) | 8 (19.5) | .30 |
| Other causes | 6 (20.7) | 10 (24.4) | .72 |
| No. of anchors for Bankart repair | 3.3 ± 0.4 | 3.3 ± 0.7 | .78 |
| Operative time, min | 104.0 ± 36.6 | 94.8 ± 30.6 | .28 |
aData are presented as mean ± SD unless otherwise indicated. B, Bankart repair alone; BR, Bankart repair with remplissage.
Intraoperative Findings
During arthroscopic surgery, Hill-Sachs lesions were found in 29 patients in group BR and 16 patients in group B. In group BR, 2 patients had glenoid bony defects, although they were <25% in size. A total of 2 to 5 suture anchors were used for Bankart repair according to the size of Bankart lesion. Furthermore, 1 or 2 additional suture anchors were implanted for the remplissage procedure, in which 2 anchors were used in 13 patients and 1 anchor was used in 16 patients, based on the size and degree of Hill-Sachs lesion.
Clinical Outcomes
Comparison of clinical outcomes including recurrence, functional scores, and active ROM between groups is shown in Table 2.
Table 2.
Preoperative and Postoperative Comparisons Between the 2 Groupsa
| Group BR | Group B | ||||||
|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | P | Preoperative | Postoperative | P | P (Postoperative, BR vs B) | |
| Recurrence, n (%) | — | 0 | — | — | 9 (22.0) | — | .007 |
| VAS for pain score | 1.3 ± 2.4 | 0.6 ± 0.9 | .10 | 1.3 ± 2.4 | 0.7 ± 1.3 | .09 | .54 |
| Rowe score | 60.5 ± 15.7 | 92.8 ± 7.1 | <.001 | 56.6 ± 17.7 | 83.3 ± 16.2 | <.001 | .005 |
| ASES score | — | 94.1 ± 5.6 | — | — | 93.2 ± 8.1 | — | .58 |
| OSIS | — | 39.9 ± 6.8 | — | — | 39.6 ± 8.1 | — | .89 |
| Forward flexion, deg | |||||||
| Symp | 170.3 ± 16.5 | 179.7 ± 1.8 | .004 | 170.7 ± 17.6 | 179.3 ± 4.6 | .004 | .67 |
| Diffcont | –9.7 ± 16.5 | –0.3 ± 1.8 | .004 | –9.3 ± 17.6 | –0.7 ± 4.6 | .004 | .67 |
| Abduction, deg | |||||||
| Symp | 164.1 ± 24.1 | 179.7 ± 1.8 | .001 | 164.6 ± 29.0 | 179.0 ± 4.8 | .003 | .51 |
| Diffcont | 15.9 ± 24.1 | –0.3 ± 1.8 | .001 | 15.4 ± 29.0 | –1.0 ± 4.8 | .003 | .51 |
| External rotation, deg | |||||||
| Symp | 74.1 ± 24.5 | 83.3 ± 12.3 | .08 | 74.3 ± 20.5 | 81.7 ± 11.8 | .05 | .60 |
| Diffcont | –13.6 ± 26.7 | –4.5 ± 7.4 | .09 | –14.8 ± 20.4 | –7.3 ± 10.5 | .04 | .22 |
| Internal rotation, median | |||||||
| Symp | T9 | T9 | .52 | T8 | T10 | .08 | .52 |
| Diffcont | –2T | –2T | .88 | –1T | –3T | .07 | .27 |
aData are presented as mean ± SD unless otherwise indicated. Dashes indicate not reported for preoperative ASES score/OSIS and not applicable for recurrence. Bolded P values indicate statistically significant difference between groups (P < .05). ASES, American Shoulder and Elbow Surgeons; B, Bankart repair alone; BR, Bankart repair with remplissage; Diffcont, difference between symptomatic and contralateral shoulder; OSIS, Oxford Shoulder Instability Score; Symp, symptomatic shoulder; T, thoracic vertebra; VAS, visual analog scale.
Recurrence
At the final follow-up, the recurrence rate in group B was significantly higher than that in group BR (22.0% vs 0, respectively; P = .007). A total of 9 patients experienced postoperative shoulder dislocation, all in group B. Among the 9 cases of dislocation, 7 were caused by trauma (5 in sports and 2 in accidents), and 2 occurred without traumatic events. The average duration from surgery to the first postoperative dislocation event was 2 years (range, 0.25-4 years).
Functional Scores
A significant pre- to postoperative improvement in Rowe scores was found for both groups (group BR: 60.5 ± 15.7 vs 92.8 ± 7.1, P < .001; group B: 56.6 ± 17.7 vs 83.3 ± 16.2, P < .001). The postoperative Rowe score in group BR was significantly higher than that in group B (P = .005). There were no significant differences in VAS for pain score, ASES score, or OSIS within or between groups.
Active ROM
Significant improvements were noted in both groups regarding pre- to postoperative forward flexion and abduction; in addition, the difference between the symptomatic and contralateral shoulders was significantly reduced for these directions. For external rotation, a significant reduction was seen in the difference between the symptomatic and contralateral shoulder in group B. No significant differences between the 2 groups were found in postoperative ROM in any direction.
Return to Sports
The outcomes for RTS regarding sports type, level, rate, and time were evaluated. Furthermore, correlation analysis of possible factors that might affect RTS was conducted.
Sports Type and Level
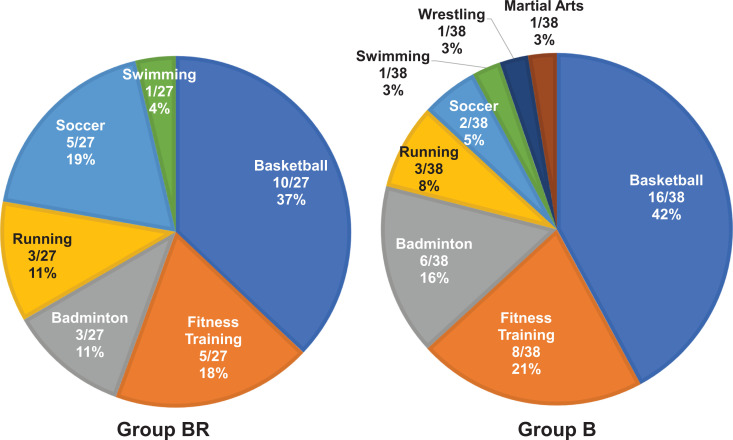
Figure 1 shows the types of sports played preoperatively by participants in the 2 study groups. No significant differences in specific sports were found between the 2 groups. However, the number of patients involved in competitive, overhead, and high shoulder demands sports postoperatively was reduced in both groups (Table 3).
Figure 1.
Sports played preoperatively by study group. B, Bankart repair alone; BR, Bankart repair with remplissage.
Table 3.
Changes in Sports Level From Preoperative to Postoperativea
| Group BR | Group B | |||
|---|---|---|---|---|
| Pre (n = 27) | Post (n = 27) | Pre (n = 38) | Post (n = 32) | |
| Competitive sports | 18 (66.7) | 9 (33.3) | 26 (68.4) | 13 (40.6) |
| Overhead sports | 13 (48.1) | 6 (22.2) | 22 (57.9) | 10 (31.3) |
| Minimal shoulder demands sports | 3 (11.1) | 8 (29.6) | 3 (7.9) | 5 (15.6) |
| Moderate shoulder demands sports | 11 (40.7) | 13 (48.1) | 11 (28.9) | 16 (50.0) |
| High shoulder demands sports | 13 (48.1) | 6 (22.2) | 24 (63.2) | 11 (34.3) |
aData are presented as n (%). B, Bankart repair alone; BR, Bankart repair with remplissage; Post, postoperative; Pre, preoperative.
Rate and Time of RTS
In total, 92.9% of the included patients (n = 65) were involved in different types and levels of sports preoperatively. As shown in Table 4, 90.8% of the patients (n = 59) RTSA postoperatively (100% in group BR vs 84.2% in group B; P = .03). In group BR, 77.8% of the patients RTSP compared with 50.0% in group B (P = .02). Notably, 40.7% of the patients in group BR showed a sense of fear postoperatively, significantly less than that (63.2%) in group B (P = .04). No significant differences were found regarding time to RTL, time to RTSA, rate of RTSP in competitive and overhead sports, or rate of expectation fulfillment between the 2 groups.
Table 4.
Rate and Time of RTSa
| Group BR | Group B | P Value | |
|---|---|---|---|
| RTL, n (%) | 29/29 (100) | 41/41 (100) | — |
| Time to RTL, mo | 2.0 ± 1.5 | 1.7 ± 1.6 | .50 |
| RTSA, n (%) | 27/27 (100) | 32/38 (84.2) | .03 |
| Time to RTSA (lower level), mo | 4.2 ± 4.1 | 3.3 ± 2.0 | .26 |
| Time to RTSA (average level), mo | 9.1 ± 14.6 | 8.3 ± 7.8 | .84 |
| RTSP, n (%) | 21/27 (77.8) | 19/38 (50.0) | .02 |
| RTSP of competitive sports, n (%) | 14/18 (77.8) | 13/26 (50) | .06 |
| RTSP of overhead sports, n (%) | 10/13 (76.9) | 12/22 (54.5) | .19 |
| Sense of fear, n (%) | 11/27 (40.7) | 24/38 (63.2) | .04 |
| Expectation fulfillment, n (%) | 20/27 (74.1) | 19/38 (50.0) | .05 |
aData are presented as mean ± SD unless otherwise indicated. Dash indicates not applicable. Bolded P values indicate statistically significant difference between groups (P < .05). B, Bankart repair alone; BR, Bankart repair with remplissage; RTL, return to normal life; RTS, return to sports; RTSA, return to sports at any level; RTSP, return to sports at previous level.
Correlation Analysis
Significantly negative correlations were found between sense of fear and the rates of RTSA, RTSP, and expectation fulfillment in both groups. For the listed outcomes for RTS, no significant associations were found regarding age at surgery, age at initial instability, symptom duration, and number of preoperative dislocations (Table 5).
Table 5.
P Values for Correlation Between Factors and RTS Outcomesa
| RTSA | RTSP | Time to RTSA (lower level) | Time to RTSA (average level) | Expectation Fulfillment | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BR | B | BR | B | BR | B | BR | B | BR | B | |
| Age at surgery | — | .23 | .39 | >.99 | .34 | .06 | .63 | .69 | .98 | .38 |
| Age at initial instability | — | .23 | .69 | .59 | .26 | .13 | .74 | .78 | .61 | .94 |
| Symptom duration | — | .84 | .36 | .43 | .85 | .25 | .75 | .33 | .42 | .11 |
| No. of preoperative dislocations | — | .86 | .07 | .87 | .22 | .36 | .61 | .54 | .09 | .62 |
| Sense of fear | — | .04 | .006 | <.001 | .64 | .03 | .37 | .78 | .001 | <.001 |
aDashes indicate not applicable. Bolded P values indicate statistical significance (P < .05). B, Bankart repair alone; BR, Bankart repair with remplissage; RTS, return to sports; RTSA, return to sports at any level; RTSP, return to sports at previous level.
Discussion
The principal findings of this study were that arthroscopic Bankart repair with remplissage resulted in satisfactory outcomes for recurrence, pain, shoulder function, active ROM, RTS, and sense of fear in the treatment of anterior shoulder instability. Specifically, both RTSA and RTSP were better after Bankart repair with remplissage than after Bankart repair alone, with less sense of fear.
The recurrence rate of arthroscopic Bankart repair with or without remplissage ranges from 0 to about 20%.4,6,8,10,16,21,29,30,37 In the current study, the patients who underwent remplissage maintained shoulder stability with no postoperative recurrence, whereas patients who had Bankart repair alone had a significantly higher recurrence rate of 22%. The result could be ascribed to the remplissage procedure not only treating the Hill-Sachs lesion, preventing further engagement, but also restoring stability and mobility via a well-healed Bankart lesion.6 Moreover, significant improvements were seen in overall shoulder function in terms of the Rowe score and active ROM.
Previous studies have raised concerns about restriction of postoperative shoulder ROM, particularly the loss of external rotation due to excessive tension on the posterior capsule from the remplissage procedure.2,6,15,25,37 The average postoperative external rotation deficit at 90° of abduction in previous studies has ranged from 2° to 9°.6–8,10,15,16,25,26,37 Although most of the reported deficits were not statistically significant, negative effects on patients’ shoulder function during daily activities and sports have been reported.14,23 In the current study, an average deficit of 5° in external rotation in the symptomatic shoulder compared with the contralateral shoulder was found in patients who underwent Bankart repair with remplissage, which was not significantly different from that in patients with Bankart repair alone. Furthermore, desirable outcomes for RTS also indicated a functional recovery of shoulder ROM. Therefore, worries about possible failure to RTS because of loss of shoulder ROM are not warranted.
To our knowledge, this is the first study to report specific outcomes for RTS after arthroscopic Bankart repair with remplissage in comparison with Bankart repair alone. In this study, the general rate and time of RTS in patients who underwent additional remplissage procedure were comparable with findings of previous studies.6,11,16 Significantly higher rates of RTSA and RTSP indicated desirable outcomes of arthroscopic Bankart repair with remplissage. Furthermore, several studies revealed a negative effect of remplissage in patients who were involved in competitive sports, especially overhead and throwing sports.11,16 However, in the present study, no significant differences of RTSP rate were shown among the patients who played competitive and overhead sports after remplissage compared with Bankart repair alone. This might have been caused by different sports played by our population (eg, no patients played rugby in this cohort).
Interestingly, it has been suggested that patients who present a sense of fear have worse outcomes for RTS. Physiologic factors such as loss of ROM and postoperative pain have been blamed for unsatisfactory RTS outcomes.1,18 However, the present study revealed that fear might act as a crucial psychological barrier to RTS after shoulder stabilization surgery. At the final follow-up, half of the patients in group B did not RTS at their previous level, although there were no obvious abnormalities in their physical function regarding functional scores and active ROM.
Although sense of fear after shoulder stabilization surgery has not been formally defined, kinesiophobia, known as fear of movement due to a feeling of vulnerability to a painful injury or reinjury,19 might describe the situation to some extent. Similar to kinesiophobia, a sense of fear could possibly alter how patients move during sports in order to avoid shoulder dislocations. People with fear could overreact in response to actual or potential threats, developing avoidance behaviors that aim to reduce fear.33 These avoidance behaviors could gradually progress to physical inactivity in the long term, leading to undesirable outcomes for RTS. Even if some patients do RTS postoperatively, they might be unable to RTSP due to distorted movements. Furthermore, sense of fear might negatively affect therapeutic effectiveness of rehabilitation when exercise is prescribed, resulting in unsatisfactory sports level and intensity after surgery. In this study, patients with remplissage showed less sense of fear than did those with Bankart repair alone, which might explain the higher rates of RTSA and RTSP. Moreover, less sense of fear could be brought on by a feeling of security resulting from remplissage.
There are several limitations in the present study. First, the outcomes for RTS were reported by the patients, which could result in inaccuracy due to the retrospective nature of this study. Second, given the epidemiologic features of anterior shoulder instability in our region, a relatively small sample size was achieved, and the patients’ sports types in this cohort were slightly different from those reported in previous studies. Third, inability to measure an engaging Hill-Sachs lesion and the amount of glenoid bone loss may have impaired our understanding for indications. For example, we may have missed lesions that needed to be better addressed. Because the indications for Bankart repair with or without remplissage were different, any comparison of the outcomes should be interpreted with caution. Fourth, further quantitative evaluation of outcomes for RTS is needed because standard criteria for RTS after shoulder stabilization surgery are not widely established.
Conclusion
Recurrence, pain, shoulder function, active ROM, RTS, and sense of fear were satisfactory after arthroscopic Bankart repair with remplissage. Specifically, along with less sense of fear, the rates of RTSA and RTSP after remplissage were better than those after Bankart repair alone. Consideration should be given to the psychological state of patients who have a sense of fear, which might act as a risk factor for unsatisfactory outcomes for RTS.
Footnotes
Final revision submitted October 29, 2020; accepted January 5, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by the National Key R&D Program of China (2016YFC1100300), National Natural Science Foundation of China (grants 81772339, 81972129, 81911530136, 81811530750, and 82072521), Key Clinical Medicine Center of Shanghai (2017ZZ01006), Sanming Project of Medicine in Shenzhen (SZSM201612078), Shanghai Rising-Star Project (18QB1400500), Introduction Project of Clinical Medicine Expert Team for Suzhou (SZYJTD201714), Development Project of Shanghai Peak Disciplines–Integrative Medicine (20180101), Shanghai Talent Development Funding Scheme (2020080), and Shanghai Committee of Science and Technology (19441901600 and 19441902000). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the health sciences institutional review board of Huashan Hospital (No. KY2019-410).
References
- 1. Abdul-Rassoul H, Galvin JW, Curry EJ, Simon J, Li X. Return to sport after surgical treatment for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47(6):1507–1515. [DOI] [PubMed] [Google Scholar]
- 2. Argintar E, Heckmann N, Wang L, Tibone JE, Lee TQ. The biomechanical effect of shoulder remplissage combined with Bankart repair for the treatment of engaging Hill-Sachs lesions. Knee Surg Sports Traumatol Arthrosc. 2014;24(2):585–592. [DOI] [PubMed] [Google Scholar]
- 3. Baker CL, Uribe JW, Whitman C. Arthroscopic evaluation of acute initial anterior shoulder dislocations. Am J Sports Med. 1990;18(1):25–28. [DOI] [PubMed] [Google Scholar]
- 4. Balg F, Boileau P. The instability severity index score: a simple preoperative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89:1470–1477. [DOI] [PubMed] [Google Scholar]
- 5. Bankart ASB. Recurrent or habitual dislocation of the shoulder-joint. Br Med J. 1923;2:1132–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boileau P, O’Shea K, Vargas P, et al. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am. 2012;94(7):618–626. [DOI] [PubMed] [Google Scholar]
- 7. Brilakis E, Avramidis G, Malahias MA, et al. Long-term outcome of arthroscopic remplissage in addition to the classic Bankart repair for the management of recurrent anterior shoulder instability with engaging Hill-Sachs lesions. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):305–313. [DOI] [PubMed] [Google Scholar]
- 8. Brilakis E, Mataragas E, Deligeorgis A, Maniatis V, Antonogiannakis E. Midterm outcomes of arthroscopic remplissage for the management of recurrent anterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):593–600. [DOI] [PubMed] [Google Scholar]
- 9. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. [DOI] [PubMed] [Google Scholar]
- 10. Buza JAI, Iyengar JJ, Anakwenze OA, Ahmad CS, Levine WN. Arthroscopic Hill-Sachs remplissage: a systematic review. J Bone Joint Surg Am. 2014;96(7):549–555. [DOI] [PubMed] [Google Scholar]
- 11. Cho NS, Yoo JH, Rhee YG. Management of an engaging Hill-Sachs lesion: arthroscopic remplissage with Bankart repair versus Latarjet procedure. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3793–3800. [DOI] [PubMed] [Google Scholar]
- 12. Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability: the development and validation of a questionnaire. J Bone Joint Surg Br. 1999;81(3):420–426. [DOI] [PubMed] [Google Scholar]
- 13. DeFroda S, Bokshan S, Stern E, Sullivan K, Owens BD. Arthroscopic Bankart repair for the management of anterior shoulder instability: indications and outcomes. Curr Rev Musculoskelet Med. 2017;10(4):442–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Elkinson I, Giles JW, Faber KJ, et al. The effect of the remplissage procedure on shoulder stability and range of motion. J Bone Joint Surg Am. 2012;94(11):1003–1012. [DOI] [PubMed] [Google Scholar]
- 15. Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair—new frontiers in the prevention of recurrent shoulder instability: a 2-year follow-up comparative study. Am J Sports Med. 2012;40(11):2462–2469. [DOI] [PubMed] [Google Scholar]
- 16. Garcia GH, Wu HH, Liu JN, Huffman GR, Kelly JD. Outcomes of the remplissage procedure and its effects on return to sports: average 5-year follow-up. Am J Sports Med. 2016;44(5):1124–1130. [DOI] [PubMed] [Google Scholar]
- 17. Grimberg J, Diop A, Bou Ghosn R, et al. Bankart repair versus Bankart repair plus remplissage: an in vitro biomechanical comparative study. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):374–380. [DOI] [PubMed] [Google Scholar]
- 18. Jobe FW, Giangarra CE, Kvitne RS, Glousman RE. Anterior capsulolabral reconstruction of the shoulder in athletes in overhand sports. Am J Sports Med. 1991;19(5):428–434. [DOI] [PubMed] [Google Scholar]
- 19. Kori S, Miller R, Todd DD. Kinesiophobia: a new view of chronic pain behavior Pain Manag. 1990;3:35–43. [Google Scholar]
- 20. Kralinger FS, Golser K, Wischatta R, Wambacher M, Sperner G. Predicting recurrence after primary anterior shoulder dislocation. Am J Sports Med. 2002;30(1):116–120. [DOI] [PubMed] [Google Scholar]
- 21. Liu JN, Gowd AK, Garcia GH, et al. Recurrence rate of instability after remplissage for treatment of traumatic anterior shoulder instability: a systematic review in treatment of subcritical glenoid bone loss. Arthroscopy. 2018;34(10):2894–2907.e2892. [DOI] [PubMed] [Google Scholar]
- 22. Mancuso CA, Altchek DW, Craig EV, et al. Patients’ expectations of shoulder surgery. J Shoulder Elbow Surg. 2002;11(6):541–549. [DOI] [PubMed] [Google Scholar]
- 23. Merolla G, Paladini P, Di Napoli G, Campi F, Porcellini G. Outcomes of arthroscopic Hill-Sachs remplissage and anterior Bankart repair: a retrospective controlled study including ultrasound evaluation of posterior capsulotenodesis and infraspinatus strength assessment. Am J Sports Med. 2015;43(2):407–414. [DOI] [PubMed] [Google Scholar]
- 24. Michener L, McClure P, Sennett B. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–594. [DOI] [PubMed] [Google Scholar]
- 25. Nourissat G, Kilinc AS, Werther JR, Doursounian L. A prospective, comparative, radiological, and clinical study of the influence of the “remplissage” procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med. 2011;39(10):2147–2152. [DOI] [PubMed] [Google Scholar]
- 26. Park MJ, Garcia G, Malhotra A, et al. The evaluation of arthroscopic remplissage by high-resolution magnetic resonance imaging. Am J Sports Med. 2012;40(10):2331–2336. [DOI] [PubMed] [Google Scholar]
- 27. Park MJ, Tjoumakaris FP, Garcia G, Patel A, Kelly JD. Arthroscopic remplissage with Bankart repair for the treatment of glenohumeral instability with Hill-Sachs defects. Arthroscopy. 2011;27(9):1187–1194. [DOI] [PubMed] [Google Scholar]
- 28. Petrera M, Dwyer T, Tsuji MR, Theodoropoulos JS. Outcomes of arthroscopic Bankart repair in collision versus noncollision athletes. Orthopedics. 2013;36(5):e621–e626. [DOI] [PubMed] [Google Scholar]
- 29. Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs “remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2008;24(6):723–726. [DOI] [PubMed] [Google Scholar]
- 30. Rashid MS, Crichton J, Butt U, Akimau PI, Charalambous CP. Arthroscopic “remplissage” for shoulder instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):578–584. [DOI] [PubMed] [Google Scholar]
- 31. Robinson CM, Dobson RJ. Anterior instability of the shoulder after trauma. J Bone Joint Surg Br. 2004;86(4):469–479. [DOI] [PubMed] [Google Scholar]
- 32. Rowe C, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63(6):863–872. [PubMed] [Google Scholar]
- 33. Steimer T. The biology of fear- and anxiety-related behaviors. Dialogues Clin Neurosci. 2002;4(3):231–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Warth RJ, Briggs KK, Dornan GJ, Horan MP, Millett PJ. Patient expectations before arthroscopic shoulder surgery: correlation with patients’ reasons for seeking treatment. J Shoulder Elbow Surg. 2013;22(12):1676–1681. [DOI] [PubMed] [Google Scholar]
- 35. Wolf E, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg. 2014;23(6):814–820. [DOI] [PubMed] [Google Scholar]
- 36. Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy. 2007;23:985–990. [DOI] [PubMed] [Google Scholar]
- 37. Zhu YM, Lu Y, Zhang J, Shen JW, Jiang CY. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med. 2011;39(8):1640–1647. [DOI] [PubMed] [Google Scholar]