Abstract
Background:
Surgical management of unstable distal clavicle fractures (DCFs) remains controversial. Traditional open techniques result in acceptable union rates but are fraught with complications. In response to these limitations, arthroscopic techniques have been developed; however, clinical outcome data are limited.
Purpose:
The primary purpose was to systematically evaluate the clinical and radiographic outcomes of arthroscopic fixation of unstable DCFs. The secondary purpose was to characterize the overall complication rate, focusing on major complications and subsequent reoperations.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review of the literature was performed following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and included a search of the PubMed, Web of Science, Cochrane Register of Controlled Trials, EMBASE, and Scopus databases. English-language studies between 2008 and 2019 that reported on outcomes of patients with DCFs who underwent operative fixation using an arthroscopic or arthroscopically assisted surgical technique were included. Data consisted of patient characteristics, fracture type, surgical technique, concomitant injuries, union rates, functional outcomes, and complications.
Results:
A total of 15 studies consisting of 226 DCFs treated using an arthroscopically based technique were included in the systematic review. The majority of fractures were classified as Neer type II. Most (97%) of the fractures underwent arthroscopic fixation using a cortical button coracoclavicular stabilization surgical technique. Bony union was reported in 94.1% of the fractures. Good to excellent outcomes were recorded in most patients at the final follow-up. The Constant-Murley score was the most widely used functional outcome score; the pooled mean Constant score was 93.06 (95% CI, 91.48-94.64). Complications were reported in 14 of the 15 studies, and the overall complication rate was 27.4%. However, only 12% of these were considered major complications, and only 6% required a reoperation for hardware-related complications.
Conclusion:
Arthroscopic fixation of DCFs resulted in good functional outcomes with union rates comparable to those of traditional open techniques. While the overall complication profile was similar to that of other described techniques, there was a much lower incidence of major complications, including hardware-related complications and reoperations.
Keywords: arthroscopic, distal clavicle fracture, coracoclavicular stabilization
Distal third clavicle fractures (DCFs) represent between 15% and 25% of all clavicle fractures.1,22,26 Approximately 25% of these fractures are unstable and demonstrate a high symptomatic nonunion rate when treated nonoperatively.1,20,21,25 Thegse unstable fractures, classified by Neer as type II or type V, present a unique challenge for surgical fixation because of the small size and comminution of the lateral fragment, the disruption of the coracoclavicular (CC) ligaments, and the large deforming forces on the fracture fragments.20 While numerous surgical techniques have been described to treat these fractures, most utilize plate osteosynthesis with either a hook or a locking plate. Despite excellent union rates,2 these techniques are associated with a high complication rate, and many require a second surgical procedure to remove prominent or painful hardware.
In response to these limitations, researchers have described newer techniques that are modeled conceptually after techniques used to treat acromioclavicular (AC) joint dislocations.18 These newer techniques achieve fracture union by reducing the medial fracture fragment to the lateral fragment using low-profile hardware that is fixed to the coracoid. While these CC stabilization techniques can be performed using an open approach, many authors advocate for an arthroscopic approach. The advantages of an arthroscopic approach include smaller incisions, less soft tissue stripping of the clavicle, and better visualization of the coracoid for implant positioning. Several studies utilizing this approach have demonstrated excellent radiographic and clinical results. Many authors have also reported low complication rates.7,34
The primary purpose of this study was to systematically review the literature, focusing on the clinical and radiographic results of arthroscopic fixation of unstable DCFs. The secondary purpose was to characterize the overall complication rate, focusing on major complications and subsequent reoperations. Our hypothesis was that arthroscopic fixation of unstable DCFs would result in acceptable radiographic and clinical results with fewer complications when compared with traditional fixation techniques.
Methods
Search Strategy
A systematic literature review was conducted on studies pertinent to arthroscopic fixation of DCFs. This was accomplished using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.29
An extensive literature search of the Medline (using PubMed), Web of Science, Cochrane Register of Controlled Trials, EMBASE, and Scopus databases was performed. Keywords employed for the search and selection were “distal AND clavicle AND fracture AND arthroscopic or arthroscopically assisted” or “Minimally Invasive Surgical Procedures” [Medical Subject Headings] AND “Clavicle” [Medical Subject Headings] AND (lateral OR distal). Furthermore, the reference sections of the included studies were screened for additional eligible papers.
Eligibility Criteria
This review included studies that reported the outcomes of patients with unstable DCFs who underwent operative fixation using an arthroscopic or arthroscopically assisted surgical technique. Studies with evidence levels 1 to 4 published in English between 2008 and 2019 were included. We excluded (1) studies that reported on patients with midshaft or medial clavicle fractures; (2) studies that included nonarthroscopic management of DCFs; (3) studies that reported on nonoperative treatment of DCFs; and (4) case reports, abstracts, reviews, letters to editors, and expert opinion.
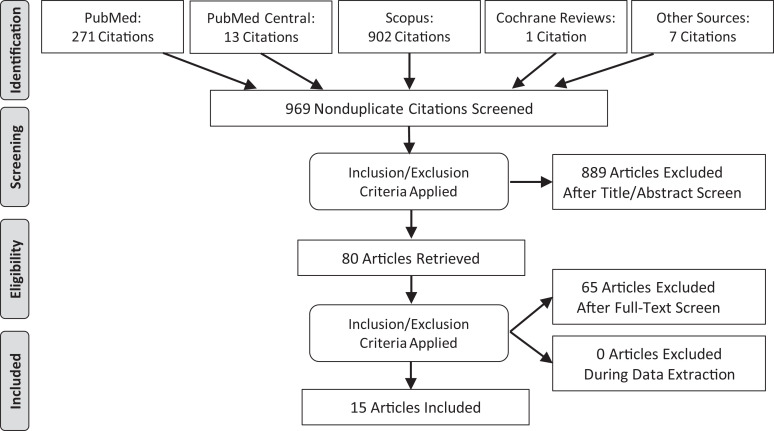
A total of 80 articles were obtained after the initial screening. After application of the inclusion and exclusion criteria, 15 articles were included in the final analysis. Figure 1 summarizes the process for study selection.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart for study selection.
Evaluation of Study Quality
Each study’s methodology, including quality and bias, were evaluated using a 10-item Coleman Methodology Score. The subsections that make up the Coleman Methodology Score are based on the subsections of the CONSORT (Consolidated Standards of Reporting Trials) statement for randomized controlled trials but are modified to allow for other trial designs.33 This scoring system ranks studies as excellent (85-100), good (70-84), fair (55-69), and poor (<55).
Data Abstraction and Synthesis
Two reviewers (R.I.N. and R.H.) independently performed data extraction using standardized data extraction forms from the included studies. Included studies were checked for unit of analysis errors. Where possible, the authors of the included studies were contacted to obtain any missing information. Study characteristics, patient characteristics, fracture type, surgical technique, follow-up intervals, and concomitant injuries from each study were included. Radiographic outcomes and union rates were documented, as were clinical outcomes as assessed using a variety of functional outcome tools. Dichotomous outcomes and cross-tabulated frequencies among surgical methods were also gathered.
Complications were extracted from all studies and were categorized as major or minor. Major complications included nonunion, construct failure or loss of reduction, infection requiring reoperation, and coracoid cortical breach requiring conversion of technique. Minor complications included CC ossification, symptomatic hardware, adhesive capsulitis, cortical button migration (without fixation failure), superficial infection, suture abscess/wound complication, and coracoid cortical breach not requiring conversion of technique.
Statistical Analysis
A descriptive analysis was used to describe the characteristics of included studies, and summary data were presented as mean and SD. We used the I 2 statistic to estimate the heterogeneity among different studies. If I 2 was >50%, significant heterogeneity was considered, and a random-effects model was used. Otherwise, a fixed-effects model was used. Furthermore, we also conducted multivariate meta-regression analyses to explore the effect of mean age, percentage male, total patients, and year of publication. The Egger linear regression test and funnel plots were used to examine the possibility of publication bias if >10 studies were included. P < .05 denoted a statistically significant difference. Statistical analysis was conducted using Stata Version 14 (StataCorp).
Results
Study Selection
The 15 included articles consisted of 8 retrospective cases series reporting on a single fixation technique,7,13–17,27,32 5 prospective case series that reported on a single fixation technique,4,12,19,24,31 and 2 retrospective comparative studies.9,34 All but 1 study14 provided data on union rates and functional outcome scores, and this study was excluded when deriving a mean. Additionally, 2 studies15,17 denoted concomitant injuries as an exclusion criterion in their data-gathering process, which was considered when evaluating concomitant injuries.
With respect to the 2 comparative studies, the first compared arthroscopic cortical button fracture stabilization with hooked plating,9 while the second compared 3 techniques (arthroscopic cortical button stabilization, hooked plating, and locked plating).34 During the data abstraction process, only data pertinent to the arthroscopic cases in these studies were incorporated when calculating means and SDs.
Characteristics and Quality of Included Studies
Table 1 summarizes the characteristics of the studies reviewed. A total of 226 fractures were treated using arthroscopically assisted techniques. Of these, 14 were Neer type IIa, 96 were type IIb, 106 were type II (subtype unspecified), 6 were type V, and 4 did not specify any fracture classification apart from “distal clavicle fracture.” Among studies, the mean ± SD age of patients who underwent arthroscopically assisted fixation ranged from 32 ± 5.8 to 51.6 ± 19.8 years; the pooled mean age was 39.21 years (95% CI, 36.66-41.75 years). The mean follow-up time ranged from 3 ± 29 to 62 ± 21 months, and the pooled mean follow-up time was 15.61 months (95% CI, 11.09-20.14 months). Among studies that reported the sex of their patients, the percentage of men ranged from 20% to 100% (Table 1).
Table 1.
Characteristics of the Included Studiesa
| Lead Author (Year) | No. of AA-DCF | Age, y, mean ± SD | Male, % | Neer Type | Surgical Construct | Union Rate, % | Complications | Reoperations |
|---|---|---|---|---|---|---|---|---|
| Blake (2017)4 | 17 | 41.0 ± 19.0 | 35 | II | Arthrex TightRope CC fixation with modified fracture site cerclage | 82 | 3 nonunions, 1 deep infection, 1 adhesive capsulitis, 1 symptomatic cerclage suture | 1 I&D, 1 suture debridement/ROH |
| Checchia (2008)7 | 7 | 46.3 ± 10.8 | 57 | II (n = 3), V (n = 4) | Double Arthrex No. 5 FiberWire clavicular subcoracoid cerclage | 100 | 1 superficial infection, 1 adhesive capsulitis | |
| Flinkkilä (2015)9 | 21 | 39.0 ± 14.0 | 95 | II | Arthrex TightRope CC fixation vs hooked plate | 95 | 1 nonunion, 1 hardware failure, 1 infection, 1 sinus formation | 1 revision fixation, 1 I&D, 1 excision of sinus tract |
| Kraus (2015)12 | 20 | 38.3 ± 7.3 | 65 | II | Arthrex TightRope CC fixation with fracture site cerclage | 95 | 1 nonunion, 1 hardware failure, 1 symptomatic implant, 6 CC ossifications | 1 revision fixation, 1 ROH |
| Kuner (2019)13 | 20 | 45.0 ± 12.0 | 70 | II | Arthrex TightRope or DogBone CC fixation | 70 | 6 nonunions, 1 wound complication, 2 adhesive capsulitis, 2 symptomatic implants | 2 nonunion revisions, 1 scar revision, 2 ROH |
| Lim (2019)14 | 5 | 51.6 ± 19.8 | 20 | IIb | Arthrex DogBone CC fixation | NR | 5 CCBRCCT, 1 superficial infection, 2 hardware failures, 1 button migration, 1 CC ossification | 2 revision fixations, 1 I&D |
| Loriaut (2015)15 | 21 | 33.0 ± 12.3 | 67 | IIb | Arthrex TightRope CC fixation | 95 | 1 hardware failure with nonunion, 1 symptomatic implant, 1 adhesive capsulitis, 2 CC ossifications | None |
| Lu (2010)16 | 7 | 51.0 ± 17.0 | 57 | IIb | Arthrex TightRope CC fixation with modified fracture site cerclage fixation | 100 | None | None |
| Mochizuki (2019)17 | 23 | 34.3 ± 9.5 | NR | IIb | Zimmer ZipTight + K-wire | 100 | NR | None |
| Motta (2014)19 | 14 | 32.0 ± 5.8 | 100 | IIa (n = 2), IIb (n = 10), V (n = 2) | Arthrex TightRope CC fixation | 100 | 1 superficial infection, 3 SCCB, 2 button migrations, 2 CC ossifications | None |
| Pujol (2008)24 | 4 | 35.0 ± 5.0 | 75 | NR | Arthrex TightRope CC fixation | 100 | None | None |
| Sautet (2018)27 | 14 | 34.6 ± 6.8 | 71 | IIb | Subcoracoid suture, Arthrex DogBone clavicular cortical button | 100 | 4 symptomatic implants | 2 ROH |
| Takase (2012)31 | 7 | 41.9 ± 0.50 | 100 | II | Smith & Nephew Endobutton (coracoid side) with spike washer and screw (clavicle side) fixation with Dacron (Smith & Nephew) artificial ligament | 100 | None | None |
| Takase (2019)32 | 18 | 43.5 ± 6.8 | 90 | II | Smith & Nephew Endobutton (coracoid side) with spike washer and screw (clavicle side) fixation with Dacron artificial ligament | 100 | None | None |
| Xiong (2018)34 | 28 | 41.9 ± 13.5 | 59 | IIa (n = 12), IIb (n = 16) | Arthroscopic Smith & Nephew double Endobutton vs hook plate vs LCP | 96 | 1 nonunion | 1 nonunion revision |
aAA-DCF, arthroscopically assisted distal clavicle fractures; CC, coracoclavicular; CCBRCCT, cortical coracoid breach requiring conversion of construct or technique; I&D, irrigation and debridement; K-wire, Kirschner wire; LCP, locking compression plate; NR, not reported; ROH, removal of hardware; SCCB, salvageable cortical coracoid breach.
According to the Coleman Methodology Score rankings, all of the included studies were considered poor (<55), and the overall mean Coleman score was 41.9 (Table 2).
Table 2.
Coleman Methodology Score (CMS) of the Included Studiesa
| Lead Author (Year) | Design | Mean Follow-up, mo | Total CMSb |
|---|---|---|---|
| Blake (2017)4 | Prospective | 12 | 42 |
| Checchia (2008)7 | Prospective | 15.86 | 42 |
| Flinkkilä (2015)9 | Retrospective | 32 | 32 |
| Kraus (2015)12 | Prospective | 23 | 46 |
| Kuner (2019)13 | Retrospective | 17.5 | 44 |
| Lim (2019)14 | Retrospective | 15.26 | 30 |
| Loriaut (2015)15 | Retrospective | 35 | 49 |
| Lu (2010)16 | Retrospective | 3 | 32 |
| Mochizuki (2019)17 | Retrospective | 4.5 | 51 |
| Motta (2014)19 | Prospective | 4.5 | 53 |
| Pujol (2008)24 | Prospective | 6 | 50 |
| Sautet (2018)27 | Retrospective | 20 | 30 |
| Takase (2012)31 | Prospective | 3 | 52 |
| Takase (2019)32 | Retrospective | 19 | 33 |
| Xiong (2018)34 | Retrospective | 35.6 | 42 |
aAll studies were level 4 evidence.
bScored on a scale from 0 to 100: 85-100, excellent; 70-84, good; 55-69, fair; <55, poor.
Fixation Techniques
Fixation techniques are detailed in Table 1. Most (97%; 219/226) of constructs used a cortical button–based CC stabilization technique. In all cases, a diagnostic arthroscopy was performed, and the arthroscope was used to expose and visualize the undersurface of coracoid in order to pass sutures through or around the coracoid. There were 113 fractures stabilized using a double cortical suture button technique (cortical suture button on the cephalad side of clavicle and undersurface of the coracoid, spanned by nonabsorbable suture). Another 44 were also stabilized with this double cortical suture button technique, with the additional use of the nonabsorbable suture for direct reduction and fixation of the fracture fragments—either with bony or capsular cerclage. Twenty-three were fixated using the double cortical suture button technique and a supplementary Kirschner wire. Twenty-five fractures were treated using a Smith & Nephew Dacron “artificial ligament” fixated using a single cortical suture button on the undersurface of the coracoid and a screw with a spike washer on the cephalad surface of the clavicle. A single clavicular cortical suture button and a subcoracoid suture were employed in the treatment of 14 fractures. Last, a double-suture cerclage technique of both the clavicle and the coracoid was used to fixate the remaining 7 fractures.
Union Rates
Union rates were reported in 221 arthroscopically treated fractures and included in 14 of the 15 studies (Table 1). A definition of union was provided by 3 of 15 authors.4,13,19 Most authors reported that union was achieved at the end of the follow-up period, while some described the date of earliest radiographic union.4,9,12,13,24,31 Bony union was reported in 208 of the 221 (94.1%) fractures. Of the 13 reported nonunions, only 4 (30.8%) were symptomatic and required revision surgery. In total, 216 of the 221 (97.7%) fractures were successfully treated and went on to either bony union or asymptomatic nonunion.
Functional Outcomes
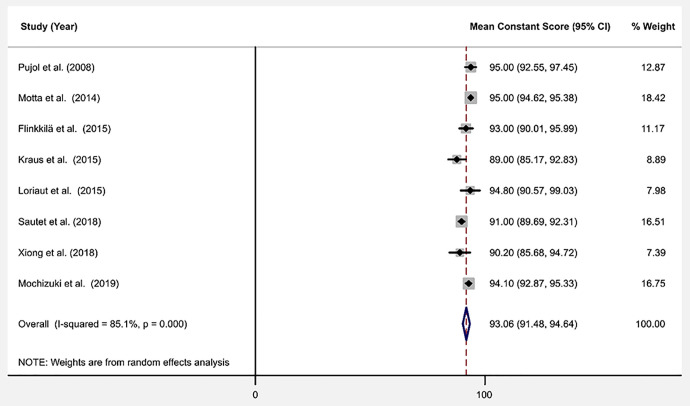
Of the 15 papers, 14 included data on functional outcomes.∥ A wide variety of functional outcome tools were utilized and included the American Shoulder and Elbow Surgeons Subjective Shoulder Scale; Constant-Murley score (Constant score); Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH); the shortened version of the DASH (QuickDASH); Penn Shoulder Score; Simple Shoulder Test; Subjective Shoulder Value (SSV); University of California Los Angeles Shoulder Score; and visual analog scale for pain. In each of these studies, the average functional outcome score qualified as good to excellent. The Constant score was the most widely used functional outcome score, appearing in 9 of the 15 studies.¶ The pooled mean Constant score was 93.06 (95% CI, 91.48-94.64) (Figure 2).
Figure 2.
Forest plot of mean Constant score.
Meta-regression analysis showed that year of publication (coefficient, –0.49; SE, 0.22; P > .15) and mean age of patients (coefficient, –0.37; SE, 0.27; P > .30) were negatively associated, while the proportion of men in the study (coefficient, 0.04; SE, 0.04; P > .47) and total number of patients in the study (coefficient, 0.11; SE, 0.15; P > .52) were positively associated with the mean Constant score, respectively. The I 2 statistic was 85.1%, indicating high heterogeneity between studies. The Egger test and funnel plots did not indicate any bias due to small-study effects (bias, –2.12; SE, 1.04; P =.08) (Figure 3).
Figure 3.
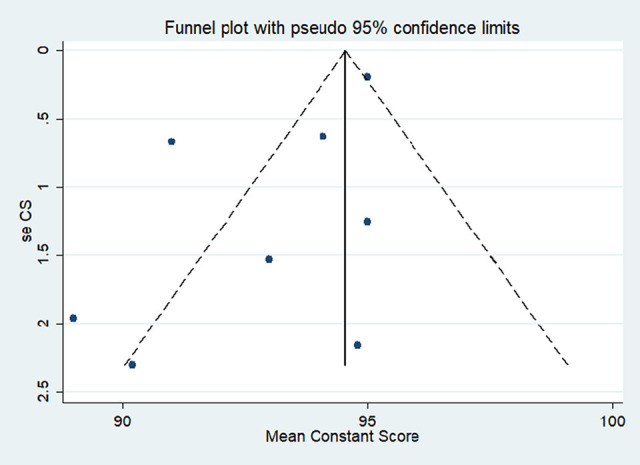
Funnel plot of mean Constant score. seCS, standard error of the mean Constant score.
In addition to the Constant score, 4 studies each utilized the University of California Los Angeles Shoulder Score,7,14,31,32 and the SSV.9,12,13,27 The visual analog scale for pain score,13,14,34 the American Shoulder and Elbow Surgeons Subjective Shoulder Scale4,14,17 and the DASH score4,9,13 were used in 3 papers each. The Simple Shoulder Test was used in 2 papers,19,34 and the Penn Shoulder Score4 and the QuickDASH17 were each used in 1 study.
Complications
Complications were reported in 14 of the 15 included studies (Table 1). A total number of 62 complications occurred in 226 arthroscopically treated DCFs for an overall complication rate of 27.4%. Eighteen of these complications resulted in a second surgical procedure, for a reoperation rate of 8%. Thirteen of the 18 complications (6% of the treated fractures) underwent a second surgical procedure specifically for hardware-related issues.
Major complications occurred in 27 of the 226 (11.9%) cases and included nonunion, construct failure or loss of reduction, infection requiring reoperation, and coracoid cortical breach requiring conversion of technique (Table 3).
Table 3.
Major and Minor Complications
| Complication Type | No. of Cases |
|---|---|
| Major | |
| Nonunion | 13 |
| Construct failure or loss of reduction | 5 |
| Infection requiring reoperation | 4 |
| Coracoid cortical breach requiring conversion of technique or construct | 5 |
| Total major complications (% of total cases) | 27 (11.9) |
| Minor | |
| Coracoclavicular ossification | 11 |
| Symptomatic hardware | 9 |
| Adhesive capsulitis | 5 |
| Button migration (without fixation failure) | 3 |
| Superficial infection | 2 |
| Suture abscess/wound complication | 2 |
| Coracoid cortical breach not requiring conversion of technique | 3 |
| Total minor complications (% of total cases) | 35 (15.5) |
| Total complications (% of total cases) | 62 (27.4) |
Of the 27 major complications, 10 required a second surgical procedure and included 4 revisions for construct failure, 3 revisions for nonunions, and 3 cases of irrigation and debridement for infection.
Minor complications occurred in 35 of the 226 (15.5%) treated fractures (Table 3). Of these, 8 of the 35 required a second surgical procedure, including 6 hardware removals, 1 excision of the sinus tract, and 1 scar revision. Reported minor complications included 11 instances of CC ligament ossification, 9 cases of symptomatic hardware, 5 cases of adhesive capsulitis, 3 cases of button migration without construct failure, 2 superficial infections, 2 suture abscesses/wound complications requiring local debridement, and 3 stable inadvertent cortical breaches of the coracoid that did not require a revision or conversion of technique.
Concomitant Injuries
Concomitant injuries were reported in 312,16,34 of the 15 studies reviewed (Table 4). Ten of the 28 reported injuries involved the ipsilateral shoulder joint and included 5 labral injury variants, 3 rotator cuff tears, 1 glenoid fracture, and 1 scapular body fracture. The remaining injuries included 7 head or face injuries, 4 elbow, wrist or hand injuries, 2 pneumothoraxes, 1 brachial plexus injury, 1 rib fracture, 1 pubis fracture, 1 anterior cruciate ligament injury, and 1 contralateral AC joint injury. According to our study, 44% of the concomittant injuries could have been addressed arthroscopically during the index procedure, potentially reducing the need for secondary procedures.
Table 4.
Concomitant Injuries
| Lead Author (Year) | No. of Patients | Mean Age, y | Concomitant Injuries | |
|---|---|---|---|---|
| Injury type | n | |||
| Kraus (2015)12 | 20 | 41 | Head and facial trauma | 7 |
| Elbow, wrist, and hand injury | 4 | |||
| Chest trauma | 3 | |||
| Subscapularis tear | 2 | |||
| Pelvis and lower extremity injury | 2 | |||
| Contralateral acromioclavicular injury | 1 | |||
| Lu (2010)16 | 7 | 51 | Labral tear | 3 |
| Glenoid fracture | 1 | |||
| Scapular fracture | 1 | |||
| Brachial plexopathy | 1 | |||
| Xiong (2018)34 | 28 | 43.5 | Bankart lesion | 1 |
| Rotator cuff injury | 1 | |||
| Glenolabral articular disruption | 1 | |||
Comparative Studies
Two of the included studies were comparative papers.9,34 Xiong et al34 compared 3 methods of fixation of Neer type II fractures and included patients treated with hook plating, anatomic plating, and arthroscopic cortical suture button. They reported comparable union rates with a 100% union rate in the hook and locking plate groups and a 95% union rate in the arthroscopic cortical suture button group. They did note, however, smaller incision length and less blood loss in the anatomic plating and arthroscopic cortical suture button groups when compared with the hook plate group.
Flinkkilä et al9 compared arthroscopic cortical suture button CC stabilization of type II DCFs with hook plating. They found a similar union rate between the 2 treatment techniques, with 1 nonunion (5%) in the hook plate group and 1 nonunion and 1 construct failure (10%) in the arthroscopic cortical suture button group. While the overall complication rate was similar, all of the patients with hook plating underwent a second surgical procedure for hardware removal at an average of 4.8 months after surgery. Additionally, the arthroscopic cortical suture button group performed marginally better with respect to the Constant score, DASH score, and SSV; however, this did not reach a level of statistical significance.
Discussion
This systematic review provides significant insights into the clinical outcomes of arthroscopic fixation of unstable DCFs. Of the fractures in this study, 97% were fixed using a cortical button CC stabilization–based technique and resulted in bony union in 94.1% of the fractures. Despite the heterogeneity of the patient-reported outcome tools utilized in the studies, good to excellent functional outcomes were achieved at the final follow-up in the majority of patients. Major complications occurred in 12% of the patients; however, only 8% of the patients required a second surgical procedure for infection, nonunion, failed fixation, or hardware-related complications.
Operative treatment of unstable DCFs remains challenging. Traditional techniques include locked or hook plates, Kirschner wires, CC screws, suture anchors, or suture tension band wiring.2,3,5,6,20,21,25 Despite satisfactory union rates, various complications have been associated with these techniques, including loss of reduction, hardware migration, AC joint arthritis, coracoid fracture, and hardware irritation.3,5,23,30 Many of these techniques require a second surgical procedure for hardware removal. A systematic review by Oh et al23 demonstrated a 41% complication rate with hook plate fixation, which has been considered the gold standard in the treatment of unstable DCFs.
In response to these complications, newer arthroscopic techniques have been described that incorporate lower-profile hardware and CC stabilization in an attempt to treat these fractures with less overall morbidity.23,35–37 There are several advantages to these techniques when compared with plating. The main advantage is that they can be used in most DCF patterns, including fractures with small or comminuted lateral fragments. The low-profile hardware also requires less soft tissue stripping of the clavicle and results in fewer postoperative hardware-related complications. Finally, diagnostic arthroscopy performed as part of the index procedure allows for visualization and treatment of concomitant shoulder pathology.
The strength of this study is that it is the first systematic review to examine the results of only arthroscopic fixation of unstable DCFs. While most of the included studies consisted of small case series, the majority utilized a similar arthroscopic cortical button CC stabilization–based technique, which enabled us to systematically summarize and analyze the data. Our study demonstrated a union rate of 94.1%, which is comparable with those reported in other published systematic reviews that have examined the operative results of DCF repair.5,23,28 The systematic review by Oh et al23 demonstrated a 98% union rate in 365 patients with unstable DCFs treated utilizing a variety of open surgical techniques, including plate osteosynthesis, tension band fixation, intramedullary fixation, and CC ligament stabilization. In a meta-analysis by Stegeman et al,30 the authors reported a 98% union rate in 350 surgically managed DCFs, again using a variety of surgical techniques.
Although union rates are comparable, most DCF fixation techniques demonstrate an unacceptably high complication rate. The majority of these are hardware-related complications and are due to failed or prominent hardware. Stegeman et al30 found no difference in the overall risk for minor complications among various fixation techniques; however, they reported that hook plate fixation was associated with an 11-fold increase in major complications compared with intramedullary fixation and a 24-fold increase when compared with coracoid-based fixation techniques. Our study demonstrated that only 12% of the patients who underwent arthroscopic fixation experienced a major complication, which is lower than reported complication rates for plate osteosynthesis.8,10,28 Most importantly only 6% of the patients in this review underwent a subsequent reoperation for hardware-related complications. This is in stark contrast to hook plate fixation, in which a large number of the patients undergo a second procedure to remove the plate. A recent systematic review demonstrated a 92.5% mean probability for hook plate removal versus only a 1.3% mean probability for suture button removal.11 This is an important consideration when choosing a technique, as a second surgical procedure increases the overall morbidity and cost. Additionally, a second procedure not only subjects patients to the inherent risks of an additional anesthetic but also increases the risks of postoperative infections, wound complications, or possible refracture through vacated screw holes in the clavicle.
Although we noted a high degree of heterogeneity in functional outcome reporting, the included studies demonstrated good to excellent functional outcomes in the majority of patients at the time of final follow-up. According to our analysis, the pooled mean Constant score in this study was 93, which is generally considered a good to excellent functional outcome score. These results are in concordance with those reported in other similar systematic reviews examining the results of DCF repair. Stegeman et al30 found good to excellent functional outcomes in 350 surgically treated DCFs regardless of surgical technique. Our meta-regression analysis also demonstrated that year of the study and mean age of patients were negatively associated with functional outcomes. Interestingly, nonunions did not appear to be correlated with poor functional outcomes; however, larger studies would be needed to identify true risk factors for poor functional outcomes.
Despite these encouraging results, there are some disadvantages to the arthroscopic techniques described in these studies. Arthroscopic techniques may not be applicable to all fracture types, including highly comminuted or long oblique fractures. These procedures can also be technically challenging and lead to increased operative time and cost. Most of these techniques relied on coracoid fixation, which carries inherent risk. Coracoid complications or construct failure occurred in 5.7% of the fractures treated in this study, highlighting the risks of coracoid-based fixation techniques. Additionally, coracoid exposure and instrumentation carry a potential risk of serious neurovascular complication despite the fact that no neurovascular complications were reported in any of the included studies.
Another disadvantage of this technique is that in many of these procedures, the fracture site was not fully exposed, and an indirect reduction of the fracture was instead obtained. This may have resulted in residual interposed soft tissue at the fracture site, possibly explaining the slightly higher nonunion rates found in this review when compared with those of direct plating. This was highlighted by the study from Kuner et al,13 in which the authors employed an indirect reduction technique resulting in a 30% nonunion rate, the highest of the included studies. Exposure of the fracture site and removal of any interposed soft tissue should therefore be considered when employing an arthroscopic approach to these fractures.
A number of limitations should be considered when interpreting the results of this systematic review. The level of evidence of the included studies was low, and all studies were either prospective or retrospective case series. The majority of the studies lacked a control group of either nonoperatively treated fractures or fractures fixed using a different surgical technique. However, the 2 comparative studies included in the analysis did demonstrate union rates, functional outcomes, and complication rates similar to the pooled data. Additionally, while the majority of techniques were conceptually equivalent, there were subtle differences among the techniques that may have made pooling these data less reliable. The criteria for nonunion were defined in only 3 of the studies, which may have influenced the overall union rates.4,10,13 Another limitation was the heterogeneity in the outcome tools used to assess functional outcomes. Finally, while complications were reported in all of the studies, they were often poorly described, leading to possible underreporting of both major and minor complications. Larger, prospective randomized clinical studies comparing arthroscopic techniques with traditional methods of DCF fixation are needed to determine the optimal management for these fractures.
Conclusion
The results of this systematic review support arthroscopic fixation of DCFs as a viable treatment option with union rates and functional outcomes comparable with those of traditional open techniques. While the overall complication profile is similar to other described techniques, there is a much lower incidence of major complications, including hardware-related complications and reoperations.
Footnotes
Final revision submitted November 5, 2020; accepted December 8, 2020
One or more of the authors has declared the following potential conflict of interest or source of funding: G.P.Y. has received consulting fees from Arthrex, nonconsulting fees from Arthrex, and educational fees from Southern Edge Orthopedics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Albrecht HU, Bamert P. Die Klavikulafraktur: Therapie und Komplikationen. Helv Chir Acta. 1982;48(5):571–583. [PubMed] [Google Scholar]
- 2. Asadollahi S, Bucknill A. Hook plate fixation for acute unstable distal clavicle fracture: a systematic review and meta-analysis. J Orthop Trauma. 2019;33(8):417–422. [DOI] [PubMed] [Google Scholar]
- 3. Basamania CJ, Craig EV, Rockwood CA. Fractures of the clavicle. In: Rockwood CA, Matsen FA, Wirth MA, Lippitt SB, eds. The Shoulder. Vol 1. 3rd ed. Saunders; 2004:508. [Google Scholar]
- 4. Blake MH, Lu MT, Shulman BS, Glaser DL, Huffman GR. Arthroscopic cortical button stabilization of isolated acute Neer type II fractures of the distal clavicle. Orthopedics. 2017;40(6):e1050–e1054. [DOI] [PubMed] [Google Scholar]
- 5. Boonard M, Sumanont S, Arirachakaran A, et al. Fixation method for treatment of unstable distal clavicle fracture: systematic review and network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28(6):1065–1078. [DOI] [PubMed] [Google Scholar]
- 6. Bosworth MB. Acromioclavicular separation: new method of repair. Surg Gynecol Obstet. 1941;73:866. [Google Scholar]
- 7. Checchia SL, Doneux PS, Miyazaki AN, Fregoneze M, Silva LA. Treatment of distal clavicle fractures using an arthroscopic technique. J Shoulder Elbow Surg. 2008;17(3):395. [DOI] [PubMed] [Google Scholar]
- 8. Ding M, Ni J, Hu J, Song D. Rare complication of clavicular hook plate: clavicle fracture at the medial end of the plate. J Shoulder Elbow Surg. 2011;20(7):e18–e20. [DOI] [PubMed] [Google Scholar]
- 9. Flinkkilä T, Heikkilä A, Sirniö K, Pakarinen H. TightRope versus clavicular hook plate fixation for unstable distal clavicular fractures. Eur J Orthop Surg Traumatol. 2015;25(3):465–469. [DOI] [PubMed] [Google Scholar]
- 10. Flinkkilä T, Ristiniemi J, Lakovaara M, Hyvonen P, Leppilahti J. Hook plate fixation of unstable lateral clavicle fractures: a report on 63 patients. Acta Orthop. 2006;77(4):644–649. [DOI] [PubMed] [Google Scholar]
- 11. Fox HM, Ramsey DC, Thompson AR, Hoekstra CJ, Mirarchi AJ, Nazir OF. Neer type-II distal clavicle fractures: a cost-effectiveness analysis of fixation techniques. J Bone Joint Surg Am. 2020;102(3):254-261. [DOI] [PubMed] [Google Scholar]
- 12. Kraus N, Stein V, Gerhardt C, Scheibel M. Arthroscopically assisted stabilization of displaced lateral clavicle fractures with coracoclavicular instability. Arch Orthop Trauma Surg. 2015;135(9):1283–1290. [DOI] [PubMed] [Google Scholar]
- 13. Kuner E, Beeres FJP, Babst R, Schoeniger R. Which lateral clavicle fractures can be treated by an arthroscopic-assisted Endobutton procedure? An analysis of risk factors. Arch Orthop Trauma Surg. 2019;139(3):331–337. [DOI] [PubMed] [Google Scholar]
- 14. Lim TK, Oh WK. Intraoperative and postoperative complications after arthroscopic coracoclavicular stabilization. Clin Orthop Surg. 2019;11(1):103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Loriaut P, Moreau PE, Dallaudière B, et al. Outcome of arthroscopic treatment for displaced lateral clavicle fractures using a double button device. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1429–1433. [DOI] [PubMed] [Google Scholar]
- 16. Lu MT, Glaser DL, Huffman GR. Arthroscopically assisted fixation of unstable distal third clavicle fractures. U Penn Orthop J. 2010;21:36–40. [Google Scholar]
- 17. Mochizuki Y, Kaneko T, Kawahara K, Toyoda S, Ikegami H, Musha Y. Outcome of arthroscopy-assisted treatment for distal clavicle fractures. Arch Orthop Trauma Surg. 2019;139(10):1393–1398. [DOI] [PubMed] [Google Scholar]
- 18. Modi CS, Beazley J, Zywiel MG, Lawrence TM, Veillette CJ. Controversies relating to the management of acromioclavicular joint dislocations. Bone Joint J. 2013;95(12):1595–1602. [DOI] [PubMed] [Google Scholar]
- 19. Motta P, Bruno L, Maderni A, Tosco P, Mariotti U. Acute lateral dislocated clavicular fractures: arthroscopic stabilization with TightRope. J Shoulder Elbow Surg. 2014;23(3):e47–e52. [DOI] [PubMed] [Google Scholar]
- 20. Neer CS. Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963;3:99–110. [DOI] [PubMed] [Google Scholar]
- 21. Neer CS II. Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 22. Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. [PubMed] [Google Scholar]
- 23. Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131(4):525–533. [DOI] [PubMed] [Google Scholar]
- 24. Pujol N, Philippeau JM, Richou J, Lespagnol F, Graveleau N, Hardy P. Arthroscopic treatment of distal clavicle fractures: a technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):884–886. [DOI] [PubMed] [Google Scholar]
- 25. Ring D, Jupiter JB. Injuries to the shoulder girdle. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, Krettek C, eds. Skeletal Trauma. Vol 2. 4th ed. Saunders; 2009:1770–1771. [Google Scholar]
- 26. Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am. 2004;86(4):778–782. [DOI] [PubMed] [Google Scholar]
- 27. Sautet P, Galland A, Airaudi S, Argenson JN, Gravier R. Arthroscopy-assisted fixation of fracture of the distal part of the clavicle by subcoracoid suture and clavicle button. Orthop Traumatol Surg Res. 2018;104(8):1237–1240. [DOI] [PubMed] [Google Scholar]
- 28. Seyhan M, Kocaoglu B, Kiyak G, Gereli A, Turkmen M. Anatomic locking plate and coracoclavicular stabilization with suture Endobutton technique is superior in the treatment of Neer type II distal clavicle fractures. Eur J Orthop Surg Traumatol. 2015;25(5):827–832. [DOI] [PubMed] [Google Scholar]
- 29. Shamseer L, Moher D, Clarke M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:G7647. [DOI] [PubMed] [Google Scholar]
- 30. Stegeman SA, Nacak H, Huvenaars KH, Stijnen T, Krijnen P, Schipper IB. Surgical treatment of Neer type-II fractures of the distal clavicle: a meta-analysis. Acta Orthop. 2013;84(2):184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Takase K, Kono R, Yamamoto K. Arthroscopic stabilization for Neer type 2 fracture of the distal clavicle fracture. Arch Orthop Trauma Surg. 2012;132(3):399–403. [DOI] [PubMed] [Google Scholar]
- 32. Takase K, Yamamoto K. Outcomes and function of conoid ligament on the basis of postoperative radiographic findings of arthroscopic stabilization for the distal clavicle fractures. Orthop Traumatol Surg Res. 2019;105(2):281–286. [DOI] [PubMed] [Google Scholar]
- 33. Watsend AME, Osestad TMO, Jakobsen RB, Engebretsen L. Clinical studies on posterior cruciate ligament tears have weak design. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):140–149. [DOI] [PubMed] [Google Scholar]
- 34. Xiong J, Chen JH, Dang Y, Zhang DY, Fu ZG, Zhang PX. Treatment of unstable distal clavicle fractures (Neer type II): a comparison of three internal fixation methods. J Int Med Res. 2018;46(11):4678–4683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yagnik GP, Brady PC, Zimmerman JP, Jordan CJ, Porter DA. A biomechanical comparison of new techniques for distal clavicular fracture repair versus locked plating. J Shoulder Elbow Surg. 2019;28(5):982–988. [DOI] [PubMed] [Google Scholar]
- 36. Yagnik GP, Jordan CJ, Narvel RR, Hassan RJ, Porter DA. Distal clavicle fracture repair: clinical outcomes of a surgical technique utilizing a combination of cortical button fixation and coracoclavicular ligament reconstruction. Orthop J Sports Med. 2019;7(9):2325967119867920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yagnik GP, Porter DA, Jordan CJ. Distal clavicle fracture repair using cortical button fixation with coracoclavicular ligament reconstruction. Arthrosc Tech. 2018;7(4):e41. [DOI] [PMC free article] [PubMed] [Google Scholar]