Abstract
Background
The effect of parathyroid autotransplantation on hypoparathyroidism is not fully understood. The purpose of the study was to determine the effect of autotransplantation of a parathyroid gland on the incidence of hypoparathyroidism and recovery of parathyroid function at 6 months after total thyroidectomy with central neck dissection for papillary thyroid carcinoma.
Methods
All patients with autotransplantation of a parathyroid gland (no inadvertent parathyroidectomy) (group A), in situ preservation of all parathyroid glands (no autotransplantation and inadvertent parathyroidectomy) (group B) or inadvertent removal of a parathyroid gland (no autotransplantation) (group C) who underwent first-time total thyroidectomy with central neck dissection for papillary thyroid carcinoma between January 2013 and June 2016 were included retrospectively.
Results
Of the 702 patients, 383, 297 and 22 were respectively included in the groups A, B and C. The overall rates of transient and permanent hypoparathyroidism were 37.6% and 1.0%. The incidence of transient hypoparathyroidism was 43.9, 29.0 and 45.5% (A vs B, P = 0.000; A vs C, P = 1.000), and the incidence of permanent hypoparathyroidism was 1.0, 0.7 and 4.5% (P > 0.05). The recovery rates of serum parathyroid hormone levels were 71.4, 72.2 and 66.0% at 6-month follow-up (P > 0.05).
Conclusion
Autotransplantation of a parathyroid gland does not affect the incidence of permanent hypoparathyroidism, but increases the risk of transient hypoparathyroidism when the rest of parathyroid glands are preserved in situ. At least 2 parathyroid glands should be preserved during total thyroidectomy with central neck dissection to prevent permanent hypoparathyroidism.
Keywords: autotransplantation, hypoparathyroidism, parathyroid gland
Introduction
Total thyroidectomy with central neck dissection has been adopted in many specialized endocrine surgery units for the treatment of papillary thyroid carcinoma (PTC) (1, 2, 3). However, central neck dissection, especially bilateral central neck dissection, always increases the risk of postoperative hypoparathyroidism (3). The reported incidence in the literature varies from 14 to 51.9% for transient hypoparathyroidism and 0–43% for permanent hypoparathyroidism (3, 4, 5, 6). Although transient hypoparathyroidism will recover within few months, it occasionally prolongs hospitalization or leads to readmission (4). Permanent hypoparathyroidism is a severe and potentially lethal complication. It not only increases the overall costs of thyroid surgery, but also accounts for the main category of thyroidectomy-related claims (7, 8).
Hypoparathyroidism is caused by injury to the parathyroid glands from ligation of the blood supply, inadvertent or deliberate removal, improper use of electrocauterization or destruction due to hematoma formation (9, 10). Meticulous dissection is a preferred method to preserve parathyroid glands with their blood supply in situ and to prevent inadvertent parathyroidectomy. However, parathyroid glands are still devascularized or occasionally found in the surgical specimens because of the anatomic location. Autotransplantation of devascularized or unintentionally removed parathyroid glands is generally recommended to prevent postoperative hypoparathyroidism (10, 11). Some endocrine surgeons even adopted routine autotransplantation of at least 1 parathyroid gland or all identifiable parathyroid glands to minimize the incidence of permanent hypoparathyriodism (12, 13, 14, 15). However, several studies demonstrated that parathyroid autotransplantation increased the risk of transient and permanent hypoparathyroidism (16, 17, 18). In addition, a recent study found similar incidence of permanent hypoparathyriodism whether a parathyroid gland was autotransplanted or inadvertently excised (19). Inadvertent parathyroidectomy is commonly regarded as one of the risk factors of postoperative hypoparathyroidism (20, 21). Interestingly, some studies reported that it had no relationship to the complication (22, 23, 24), suggesting that rather than removal of one or more parathyroid glands, autotransplantation renders them dysfunctional and causes postoperative hypoparathyroidism.
Therefore, the effect of parathyroid autotransplantation on postoperative hypoparathyroidism is not fully understood. In this study, we compared the patients with autotransplantation of a parathyroid gland to those with all the parathyroid glands preserved in situ and those with inadvertent removal of a parathyroid gland. The purpose of the study was to determine whether autotransplantation of a parathyroid gland affected the incidence of postoperative hypoparathyroidism and recovery of parathyroid function at 6 months after total thyroidectomy with central neck dissection for papillary thyroid carcinoma.
Methods
Patients
We retrospectively searched for all PTC patients who underwent first-time total thyroidectomy with central neck dissection (including lateral neck dissection) in the Department of Thyroid Surgery, West China Hospital of Sichuan University between January 2013 and June 2016. Those patients with autotransplantation of a parathyroid gland (no inadvertent parathyroidectomy) (group A), in situ preservation of all the parathyroid glands (no autotransplantation and inadvertent parathyroidectomy) (group B) or inadvertent removal of a parathyroid gland (no autotransplantation) (group C) were included for analyses. The patients with preoperative parathyroid dysfunction, resurgery, completion thyroidectomy, endoscopic thyroidectomy or loss of 6-month follow-up were excluded. Informed consent of at least 6-month follow-up was obtained from each patient. The study was approved by the Medical Ethics Committee of West China Hospital, Sichuan University.
Indications and surgical procedures of total thyroidectomy with lymph node dissection
In our department, the indications and surgical procedures of total thyroidectomy with lymph node dissection for PTC treatment have been described in detail previously (25, 26). Unilateral central neck dissection is performed routinely. All patients underwent therapeutic lateral neck dissection (preoperative fine-needle aspiration cytology). All surgical procedures were performed by an experienced surgeon (Zhu). Each parathyroid gland was tried to be preserved in situ intraoperatively. Thymectomy was avoided except for tumor invasion. Surgical specimens (thyroid gland and central lymphadenectomy specimen) were examined routinely for any unintentionally removed parathyroid glands. If a parathyroid gland was nonviable or resected unintentionally, it was autotransplanted into the contralateral sternocleidomastoid muscle after the confirmation by intraoperative frozen biopsy. Precise information on the number of parathyroid glands identified and autotransplanted was recorded in operative notes. A same group of experienced pathologists analyzed all surgical specimens. The presence of a whole parathyroid gland or parathyroid tissue fragments (≤1 mm) in the perithyroidal area and/or the central lymphadenectomy specimen reported by pathologists was defined as inadvertent parathyroidectomy (2).
Perioperative management
Each patient accepted preoperative assessment including serum calcium, parathyroid hormone (PTH), thyroid function, neck ultrasound and laryngoscopy. The levels of serum calcium and PTH were routinely obtained on the first postoperative day and 1 month and 6 months after surgery. Intravenous calcium supplementation (calcium gluconate 10%, 40 mL) was routinely applied at the end of surgery. A standard dose of calcium carbonate (600–2400 mg/day) was orally administered on the first postoperative day if the serum PTH level was below the normal range. Calcitriol at 0.25–0.5 μg/day was simultaneously taken to promote absorption and reabsorption of calcium. Patients with normal PTH levels were not treated with oral calcium. Intravenous calcium was supplemented for the treatment of symptomatic hypocalcemia regardless of oral calcium and calcitriol administration. Oral calcium and calcitriol were ceased within 1 month after hospital discharge if possible. Hypoparathyroidism was defined as serum PTH level <1.6 pmol/L after surgery (normal range, 1.6–6.9 pmol/L). If serum PTH level returned to normal within 6 months postoperatively, hypoparathyroidism was classified as transient. On the contrary, it was classified as permanent if it persisted more than 6 months (27).
Data collection
The demographic characteristics, preoperative assessment, details of surgical extent (unilateral or bilateral central neck dissection), number of parathyroid glands identified, autotransplanted and inadvertently removed, final pathology, incidence of postoperative hypoparathyroidism and serum PTH levels at 6-month follow-up of all included patients were collected. Operative notes and pathology reports were reviewed independently by two authors (Su A and Gong Y) to determine the detail of parathyroid glands. PTC was staged by the system of American Joint Committee on Cancer (AJCC) (the 7th edition) (28). The primary endpoints were the number of parathyroid glands identified, autotransplanted and inadvertently removed, incidence of postoperative hypoparathyroidism and serum PTH levels at 6-month follow-up.
Statistical analysis
Continuous variables were expressed as mean ± s.d. The data were analyzed by SPSS software (version 19.0, SPSS, Inc., 1989–2010). Statistical comparison between groups A and B or groups A and C was calculated by the Fisher’s exact test or Student’s t-test. Multivariate analyses were performed to assess the independent risk factors of transient and permanent hypoparathyroidism. For multivariate analyses, the variables that were statistically significant in univariate analyses were included in logistic regression analyses. The results of the multivariate analyses were expressed as odds ratio (OR) and 95% confidence interval (CI). Statistical significance was set at P < 0.05.
Results
Patient characteristics
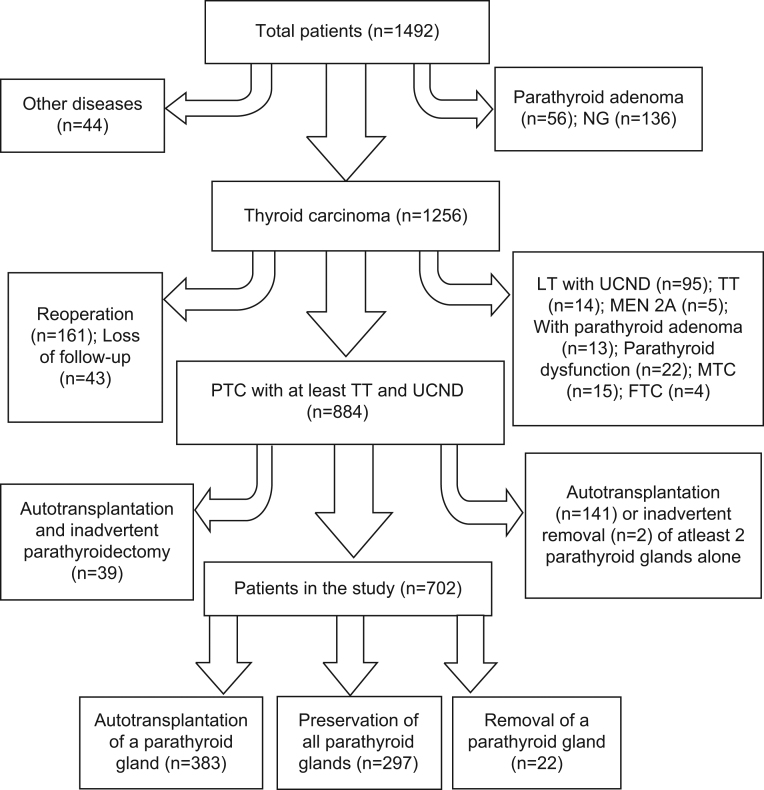
Of the 1492 patients whose medical records were reviewed, 702 met the study criteria and were included in the study (Fig. 1). There were 192 male and 510 female, with a mean age of 42.6 ± 12.9 years. Unilateral central neck dissection and bilateral central neck dissection were performed on 253 and 356 patients, respectively. Seventy-seven patients underwent bilateral central neck dissection with unilateral neck dissection, and 16 accepted bilateral central neck dissection with bilateral neck dissection. Groups A, B and C consisted of 383, 297 and 22 patients, respectively. Table 1 shows a comparison of baseline characteristics of the patients in the 3 groups. No significant differences were found between groups A and B or groups A and C in age, gender, body mass index (BMI), comorbidities (hypertension, diabetes, thyroiditis, Graves’ disease, hypothyroidism and nodular goiter) and preoperative levels of serum calcium and PTH. Patients with autotransplantation of a parathyroid gland underwent more bilateral central neck dissection than those with preservation of all the parathyroid glands in situ (67.4% vs 58.6%, P = 0.020).
Figure 1.
Flow chart of the patients investigated. FTC, follicular thyroid carcinoma; LT, lobectomy; MEN, multiple endocrine neoplasia; MTC, medullary thyroid carcinoma; NG, nodular goiter; PTC, papillary thyroid carcinoma; TT, total thyroidectomy; UCND, unilateral central neck dissection.
Table 1.
The clinical characteristics of the patients in the 3 groups.
| Variables | Group A (n = 383) | Group B (n = 297) | Group C (n = 22) | P value* | P value† |
|---|---|---|---|---|---|
| Age (years) | 42.8 ± 12.8 | 42.3 ± 13.2 | 43.7 ± 10.3 | 0.643 | 0.736 |
| Gender (male/female) | 112/271 | 75/222 | 5/17 | 0.261 | 0.633 |
| BMI (kg/m2) | 23.6 ± 3.4 | 23.2 ± 3.4 | 22.8 ± 2.5 | 0.082 | 0.275 |
| Hypertension | 47 | 36 | 1 | 1 | 0.495 |
| Diabetes | 11 | 7 | 0 | 0.811 | 1 |
| Thyroiditis | 116 | 77 | 8 | 0.230 | 0.635 |
| Graves’ disease | 12 | 7 | 1 | 0.642 | 0.522 |
| Hypothyroidism | 3 | 5 | 0 | 0.306 | 1 |
| Nodular goiter | 228 | 175 | 9 | 0.875 | 0.118 |
| Calcium (mmol/L) | 2.32 ± 0.37 | 2.30 ± 0.22 | 2.31 ± 0.11 | 0.322 | 0.859 |
| PTH (pmol/L) | 5.42 ± 1.65 | 5.65 ± 2.27 | 5.74 ± 1.82 | 0.421 | 0.553 |
| Surgical extent (UCND/≥BCND) | 125/258 | 123/174 | 5/17 | 0.020 | 0.481 |
*Groups A vs B; †groups A vs C.
BCND, bilateral central neck dissection; BMI, body mass index; PTH, parathyroid hormone; UCND, unilateral central neck dissection.
Characteristics of tumors and central lymph nodes
Table 2 shows the characteristics of tumors and central lymph nodes. There were no significant differences between groups A and B or groups A and C in the largest tumor size, multifocality, primary tumor location, T classification, N classification, AJCC stage and gross extrathyroidal extension. Significantly more central lymph nodes and metastatic central lymph nodes were retrieved in the group A than in the group B (P = 0.001 and P = 0.024, respectively). However, there was no significant difference of the two parameters between groups A and C (P = 0.731 and P = 0.368, respectively).
Table 2.
The characteristics of tumors and central lymph nodes in the 3 groups.
| Variables | Group A (n = 383) | Group B (n = 297) | Group C (n = 22) | P value† | P value‡ |
|---|---|---|---|---|---|
| Largest tumor size (mm) | 14.4 ± 9.7 | 13.2 ± 9.9 | 13.6 ± 7.6 | 0.133 | 0.709 |
| Multifocality | 106 | 70 | 3 | 0.251 | 0.216 |
| Primary tumor location | 1 | 0.217 | |||
| Upper | 108 | 84 | 3 | ||
| Middle | 162 | 122 | 14 | ||
| Lower | 103 | 80 | 3 | ||
| Isthmus | 10 | 11 | 2 | ||
| T classification | 0.384 | 0.655 | |||
| T1 | 145 | 123 | 7 | ||
| T2 | 12 | 8 | 1 | ||
| T3 | 206 | 158 | 14 | ||
| T4 | 20 | 8 | 0 | ||
| N classification | 0.079 | 0.822 | |||
| N0 | 132 | 122 | 8 | ||
| N1 | 251 | 175 | 14 | ||
| AJCC stage | |||||
| I–II | 250 | 194 | 11 | 1 | 0.171 |
| III–IV | 133 | 103 | 11 | ||
| Gross extrathyroidal extension | 155 | 123 | 5 | 0.814 | 0.118 |
| Number of harvested lymph nodes* | 12.2 ± 6.5 | 10.6 ± 6.1 | 11.7 ± 6.5 | 0.001 | 0.731 |
| Number of metastatic lymph nodes* | 3.1 ± 4.2 | 2.5 ± 3.5 | 2.3 ± 3.2 | 0.024 | 0.368 |
*Central lymph nodes; †groups A vs B; ‡groups A vs C.
AJCC, American Joint Committee on Cancer.
Details of parathyroid glands, hypoparathyroidism and 6-month follow-up
Among the 3 groups, less parathyroid glands were identified intraoperatively in the patients with inadvertent removal of a parathyroid gland. Rates of transient and permanent hypoparathyroidism for the entire cohort were 37.6% (264/702) and 1.0% (7/702), respectively. The incidence of transient hypoparathyroidism was 43.9% (168/383) in patients with autotransplantation of a parathyroid gland, 29.0% (86/297) in those with preservation of all the parathyroid glands and 45.5% (10/22) in those with inadvertent removal of a parathyroid gland (43.9% vs 29.0%, P = 0.000 and 43.9% vs 45.5%, P = 1.000). The incidence of permanent hypoparathyroidism in the 3 groups was 1.0, 0.7 and 4.5%, respectively (P > 0.05). Table 3 shows the serum PTH levels in the 3 groups at 6-month follow-up. Compared to the patients with in situ preservation of all the parathyroid glands, significantly lower serum PTH level was found in patients with autotransplantation of a parathyroid gland on postoperative day 1. However, similar levels of serum PTH were found in the 3 groups after 1 month and 6 months (P > 0.05). After 6 months of follow-up, the recovery rates of serum PTH level were 71.4, 72.2 and 66.0% in the 3 groups.
Table 3.
The details of parathyroid glands, hypoparathyroidism and the results of follow-up in the 3 groups.
| Variables | Group A (n = 383) | Group B (n = 297) | Group C (n = 22) | P value* | P value† |
|---|---|---|---|---|---|
| Parathyroid identification | 3.5 ± 0.8 | 3.4 ± 0.8 | 2.7 ± 0.8 | 0.677 | 0.000 |
| Hypoparathyroidism | |||||
| Transient | 168 | 86 | 10 | 0.000 | 1 |
| Permanent | 4 | 2 | 1 | 0.701 | 0.245 |
| Postoperative PTH (pmol/L) | |||||
| 1 day | 1.76 ± 1.18 | 2.34 ± 1.41 | 1.93 ± 1.34 | 0.001 | 0.664 |
| 1 month | 3.45 ± 1.63 | 3.74 ± 1.70 | 3.50 ± 1.65 | 0.220 | 0.920 |
| 6 months | 3.87 ± 1.61 | 4.08 ± 1.61 | 3.79 ± 1.63 | 0.372 | 0.879 |
*Groups A vs B; †groups A vs C.
PTH, parathyroid hormone.
Risk factors for transient and permanent hypoparathyroidism
Perioperative factors, which influenced the incidence of transient and permanent hypoparathyroidism, were sought by univariate and multivariate analyses. Gender, surgical extent and parathyroid autotransplantation had significant effects on the formation of transient hypoparathyroidism and the number of parathyroid glands preserved in situ was associated with permanent hypoparathyroidism on univariate analyses (Table 4). Multivariate analysis found female, bilateral central neck dissection and autotransplantation of a parathyroid gland to be independent risk factors of transient hypoparathyroidism (Table 5). Preservation of less than 2 parathyroid glands was an independent risk factor of permanent hypoparathyroidism (OR, 9.085; 95% CI, 1.981–44.660; P = 0.005).
Table 4.
Univariate analysis of risk factors for the development of transient and permanent hypoparathyroidism.
| Variables | No permanent | Permanent (n = 7) | P value† | P value‡ | ||
|---|---|---|---|---|---|---|
| Normal (n = 431) | Transient (n = 264) | Total (n = 695) | ||||
| Age (<45/≥45, years) | 241/190 | 152/112 | 393/302 | 2/5 | 0.694 | 0.250 |
| Gender (male/female) | 138/293 | 53/211 | 191/504 | 1/6 | 0.001 | 0.680 |
| BMI (<25/≥25, kg/m2) | 303/128 | 195/69 | 498/197 | 5/2 | 0.340 | 1 |
| Hypertension | 57 | 26 | 83 | 1 | 0.228 | 0.592 |
| Diabetes | 12 | 6 | 18 | 0 | 0.808 | 1 |
| Thyroiditis | 121 | 78 | 199 | 2 | 0.730 | 1 |
| Graves’ disease | 12 | 8 | 20 | 0 | 0.820 | 1 |
| Hypothyroidism | 5 | 3 | 8 | 0 | 1 | 1 |
| Nodular goiter | 251 | 158 | 409 | 3 | 0.692 | 0.456 |
| Preoperative calcium (mmol/L) | 2.31 ± 0.16 | 2.32 ± 0.44 | 2.31 ± 0.30 | 2.26 ± 0.09 | 0.658 | 0.676 |
| Preoperative PTH (pmol/L) | 5.73 ± 1.98 | 5.28 ± 1.75 | 5.54 ± 1.16 | 4.28 ± 2.33 | 0.145 | 0.129 |
| Surgical extent (UCND/≥BCND) | 172/259 | 79/185 | 251/444 | 2/5 | 0.009 | 1 |
| Largest tumor size (mm) | 13.6 ± 8.4 | 14.6 ± 10.3 | 14.0 ± 9.2 | 14.4 ± 5.4 | 0.223 | 0.832 |
| Multifocality | 101 | 76 | 177 | 2 | 0.127 | 1 |
| Tumor location (upper/middle/lower/isthmus) | 127/174/116/14 | 64/121/70/9 | 191/295/186/23 | 4/3/0/0 | 0.138 | 0.098 |
| T classification (T1–2/T3–4) | 175/256 | 118/146 | 293/402 | 3/4 | 0.304 | 1 |
| N classification (N0/N1) | 166/265 | 94/170 | 260/435 | 2/5 | 0.468 | 1 |
| AJCC stage (I–II/III–IV) | 272/159 | 179/85 | 451/244 | 4/3 | 0.220 | 0.701 |
| Gross extrathyroidal extension | 174 | 106 | 280 | 3 | 1 | 1 |
| Harvested lymph nodes (<10/≥10)* | 205/226 | 107/157 | 312/383 | 5/2 | 0.071 | 0.254 |
| Parathyroid identification (<3/≥3) | 55/376 | 39/225 | 94/601 | 3/4 | 0.493 | 0.059 |
| Parathyroid autotransplantation (0/1) | 220/211 | 96/168 | 316/379 | 3/4 | 0.000 | 1 |
| Inadvertent parathyroidectomy (0/1) | 420/11 | 254/10 | 674/21 | 6/1 | 0.369 | 0.201 |
| Parathyroid preservation (<2/≥2) | 29/402 | 23/241 | 52/643 | 3/4 | 0.373 | 0.013 |
*Central lymph nodes; †normal vs transient; ‡no permanent (total) vs permanent.
AJCC, American Joint Committee on Cancer; BCND, bilateral central neck dissection; BMI, body mass index; PTH, parathyroid hormone; UCND, unilateral central neck dissection.
Table 5.
Multivariate analysis of risk factors for the development of transient hypoparathyroidism.
| Variables | OR | 95% CI | P value |
|---|---|---|---|
| Gender (female) | 1.977 | 1.366–2.861 | 0.000 |
| Surgical extent (≥BCND) | 1.554 | 1.114–2.168 | 0.009 |
| Parathyroid autotransplantation (1) | 1.834 | 1.332–2.526 | 0.000 |
BCND, bilateral central neck dissection; CI, confidence interval; OR, odds ratio. (1) autotransplantation of one parathyroid gland increases the incidence of transient hypoparathyroidism.
Discussion
Parathyroid autotransplantation, first described in humans by Lahey in 1926 (29), is regarded as a major technical and physiological breakthrough in the field of thyroid surgery. In recent years, it has been increasingly employed to prevent postoperative hypoparathyroidism (10, 11, 12, 13, 14, 15). However, there is no good evidence to prove that parathyroid grafts do in fact prevent this complication because the recovery of parathyroid function depends on both preserved and autotransplanted parathyroid glands (19). As shown in the present study, there is large consensus that autotransplantation increases the risks of transient hypoparathyroidism and postoperative hypocalcemia (8, 30, 31). It is still controversial whether it can reduce the incidence of permanent hypoparathyroidism. Although two studies reported that autotransplantation of all identifiable parathyroid glands could lower the risk of permanent hypoparathyroidism (14, 15), Kihara and coworkers (17) found that the strategy led to a higher permanent hypoparathyroidism rate. The effect of autotransplantation on permanent hypoparathyroidism is closely related to the number of autotransplanted parathyroid glands (8, 17). Kikumori and coworkers (15) revealed that the incidence of permanent hypoparathyroidism was inversely correlated with the number of autotransplanted parathyroid glands. Several studies reported that autotransplantation of at least one parathyroid gland effectively decreased the incidence of permanent hypoparathyroidism (12, 13, 30). A multicenter study also investigated the impact of autotransplantation of a parathyroid gland on postoperative hypoparathyroidism and drew a similar conclusion (32). These conclusions, however, are questioned by the confounding factors, including different number of parathyroid glands autotransplanted and preserved, a variety of thyroid gland disorders (benign and malignant tumors) and different surgical times (first-time surgery and resurgery). In addition, these studies did not provide the comparison with inadvertent parathyroidectomy and the change of serum PTH levels after follow-up.
There is no doubt that parathyroid autotransplantation is an effective procedure to preserve parathyroid function. Direct evidence of grafts function can be obtained through the comparison of serum PTH levels between the transplanted and non-transplanted arms (33, 34). The reported success rate of autotransplantation ranges from 55 to 100% (5). In our study, although there was no significant difference of the serum PTH levels among the 3 groups at 6-month follow-up, the recovery rates were higher in patients with autotransplantation of a parathyroid gland or in situ preservation of all the parathyroid glands than those with inadvertent removal of a parathyroid gland (71.4%/72.2% vs 66.0%). The parathyroid function of the patients without inadvertent parathyroidectomy in the 2 groups did not recover to 100% of the preoperative levels at 6-month follow-up, which is attributed to the thermal and/or mechanical injury of parathyroid glands, dysfunction of parathyroid glands preserved in situ, loss of part of parathyroid tissue for intraoperative frozen biopsy, dysfunction of the grafts and/or short-term follow-up period.
Most available reports on parathyroid autotransplantation have overestimated its impact and underestimated the effect of in situ preservation on parathyroid function (12, 13, 30, 32). In our study, the prevalence of permanent hypoparathyroidism after total thyroidectomy with central lymph node dissection was similar whether a parathyroid gland was autotransplanted, preserved or inadvertently removed when the rest of parathyroid glands were preserved in situ. This observation implies that the part of function preserved by autotransplantation of a parathyroid gland has no significant effect on the incidence of permanent hypoparathyroidism. Therefore, parathyroid glands preserved in situ, instead of the one autotransplanted, are critical in preventing permanent hypoparathyroidism (2). This finding can be explained by the fact that preserving at least 2 parathyroid glands with an intact blood supply is sufficient to prevent permanent hypoparathyroidism (35). The current study also demonstrated that in situ preservation of less than 2 parathyroid glands was a significant variable favoring permanent hypoparathyroidism. Therefore, at least 2 parathyroid glands should be carefully preserved during total thyroidectomy with central neck dissection to avoid permanent hypoparathyroidism.
Intraoperative identification of parathyroid glands is negatively correlated with inadvertent removal of parathyroid glands (36). Inadvertent parathyroidectomy is always reported to add a further risk of postoperative transient and permanent hypoparathyroidism (20, 21, 37). A recent study revealed that presence of at least 2 parathyroid glands in surgical specimens was a risk factor of transient hypoparathyroidism (38). However, one study revealed no correlation between inadvertent parathyroidectomy and permanent hypoparathyroidism (27). Current evidence suggested that inadvertent removal of a parathyroid gland had no statistically significant relation with permanent hypoparathyroidism, which is similar to the finding of the study. It further confirms that in situ preservation of at least 2 parathyroid glands effectively prevents permanent hypoparathyroidism.
As reported in the previous studies (12, 17), female gender was an independent risk factor of transient hypoparathyroidism in the present study. However, the exact mechanisms underlying the gender disparity are still not clear. It may attribute to the anatomic and morphologic differences of parathyroid glands, different effects of sex steroids on PTH secretion and different regulators of monoclonal proliferation and mitosis of parathyroid glands between male and female patients (39, 40, 41). Bilateral central neck dissection involves high risk of hypoparathyroidism due to the devascularization and/or inadvertent removal of parathyroid glands (37, 38). Patients with bilateral central neck dissection frequently suffer from higher rates of transient and permanent hypoparathyroidism than those with unilateral central neck dissection (6). According to data from the present study, however, bilateral central neck dissection had no close relationship with permanent hypoparathyroidism. This result appears to be relevant to the surgeon’s experience, which is of utmost importance to prevent permanent hypoparathyroidism (42). Therefore, patients may benefit from an experienced surgeon to perform total thyroidectomy with bilateral central neck dissection.
There are several limitations in the study. The data are from retrospective chart review. The effect of autotransplantation of a parathyroid gland is determined on the basis of the recovery of parathyroid function which depends on both the in situ normal parathyroid glands and the autotransplanted parathyroid glands. Neither the viability of the preserved parathyroid glands nor the graft function could be assessed directly. Another limitation is the short-term follow-up period. Therefore, the result will be more persuasive if a prospective trial with autotransplantation of a parathyroid gland in the forearm subcutaneous tissue or muscle and with long-term follow-up period is conducted in the future.
In conclusion, autotransplantation of a parathyroid gland does not affect the incidence of permanent hypoparathyroidism, but increases the risk of transient hypoparathyroidism when the rest of parathyroid glands are preserved in situ. At least 2 parathyroid glands should be preserved during total thyroidectomy with central neck dissection to prevent permanent hypoparathyroidism.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This study was supported by the National Natural Science Fund (81502612) and Scientific Research Fund of Science and Technology Department of Sichuan Province (2016SZ0045).
Author contribution statement
Anping Su helped in writing and revising the manuscript. Yanping Gong, Wenshuang Wu, Rixiang Gong and Zhihui Li helped in revising the manuscript. Jingqiang Zhu helped in revising the manuscript and is a corresponding author.
References
- 1.Hall CM, Snyder SK, Maldonado YM, Lairmore TC. Routine central lymph node dissection with total thyroidectomy for papillary thyroid cancer potentially minimizes level VI recurrence. Surgery 2016. 160 1049–1058. ( 10.1016/j.surg.2016.06.042) [DOI] [PubMed] [Google Scholar]
- 2.Sitges-Serra A, Gallego-Otaegui L, Suárez S, Lorente-Poch L, Munné A, Sancho JJ. Inadvertent parathyroidectomy during total thyroidectomy and central neck dissection for papillary thyroid carcinoma. Surgery 2017. 161 712–719. ( 10.1016/j.surg.2016.08.021) [DOI] [PubMed] [Google Scholar]
- 3.Shan CX, Zhang W, Jiang DZ, Zheng XM, Liu S, Qiu M. Routine central neck dissection in differentiated thyroid carcinoma: a systematic review and meta-analysis. Laryngoscope 2012. 122 797–804. ( 10.1002/lary.22162) [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharyya N, Fried MP. Assessment of the morbidity and complications of total thyroidectomy. Archives of Otolaryngology: Head and Neck Surgery 2002. 128 389–392. ( 10.1001/archotol.128.4.389) [DOI] [PubMed] [Google Scholar]
- 5.Lo CY. Parathyroid autotransplantation during thyroidectomy. ANZ Journal of Surgery 2002. 72 902–907. ( 10.1046/j.1445-2197.2002.02580.x) [DOI] [PubMed] [Google Scholar]
- 6.Giordano D, Valcavi R, Thompson GB, Pedroni C, Renna L, Gradoni P, Barbieri V. Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 2012. 22 911–917. ( 10.1089/thy.2012.0011) [DOI] [PubMed] [Google Scholar]
- 7.Testini M, Gurrado A, Lissidini G, Nacchiero M. Hypoparathyroidism after total thyroidectomy. Minerva Chirurgica 2007. 62 409–415. [PubMed] [Google Scholar]
- 8.Palazzo FF, Sywak MS, Sidhu SB, Barraclough BH, Delbridge LW. Parathyroid autotransplantation during total thyroidectomy – does the number of glands transplanted affect outcome? World Journal of Surgery 2005. 29 629–631. ( 10.1007/s00268-005-7729-9) [DOI] [PubMed] [Google Scholar]
- 9.Bliss RD, Gauger PG, Delbridge LW. Surgeon’s approach to the thyroid gland: surgical anatomy and the importance of technique. World Journal of Surgery 2000. 24 891–897. ( 10.1007/s002680010173) [DOI] [PubMed] [Google Scholar]
- 10.Shaha AR, Burnett C, Jaffe BM. Parathyroid autotransplantation during thyroid surgery. Journal of Surgical Oncology 1991. 46 21–24. ( 10.1002/jso.2930460106) [DOI] [PubMed] [Google Scholar]
- 11.Lo CY, Lam KY. Routine parathyroid autotransplantation during thyroidectomy. Surgery 2001. 129 318–323. ( 10.1067/msy.2001.111125) [DOI] [PubMed] [Google Scholar]
- 12.Zedenius J, Wadstrom C, Delbridge L. Routine autotransplantation of at least one parathyroid gland during total thyroidectomy may reduce permanent hypoparathyroidism to zero. Australian and New Zealand Journal of Surgery 1999. 69 794–797. ( 10.1046/j.1440-1622.1999.01697.x) [DOI] [PubMed] [Google Scholar]
- 13.Ahmed N, Aurangzeb M, Muslim M, Zarin M. Routine parathyroid autotransplantation during total thyroidectomy: a procedure with predictable outcome. Journal of the Pakistan Medical Association 2013. 63 190–193. [PubMed] [Google Scholar]
- 14.Funahashi H, Satoh Y, Imai T, Ohno M, Narita T, Katoh M, Tanaka Y, Tobinaga J, Andoh H, Miyazaki K. Our technique of parathyroid autotransplantation in operation for papillary thyroid carcinoma. Surgery 1993. 114 92–96. [PubMed] [Google Scholar]
- 15.Kikumori T, Imai T, Tanaka Y, Oiwa M, Mase T, Funahashi H. Parathyroid autotransplantation with total thyroidectomy for thyroid carcinoma: long-term follow-up of grafted parathyroid function. Surgery 1999. 125 504–508. ( 10.1016/S0039-6060(99)70201-1) [DOI] [PubMed] [Google Scholar]
- 16.Lorente-Poch L, Sancho JJ, Ruiz S, Sitges-Serra A. Importance of in situ preservation of parathyroid glands during total thyroidectomy. British Journal of Surgery 2015. 102 359–367. ( 10.1002/bjs.9676) [DOI] [PubMed] [Google Scholar]
- 17.Kihara M, Miyauchi A, Kontani K, Yamauchi A, Yokomise H. Recovery of parathyroid function after total thyroidectomy: long-term follow-up study. ANZ Journal of Surgery 2005. 75 532–536. ( 10.1111/j.1445-2197.2005.03435.x) [DOI] [PubMed] [Google Scholar]
- 18.Kirdak T, Dundar HZ, Uysal E, Ocakoglu G, Korun N. Outcomes of parathyroid autotransplantation during total thyroidectomy: a comparison with age- and sex-matched controls. Journal of Investigative Surgery 2017. 30 201–209. ( 10.1080/08941939.2016.1232768) [DOI] [PubMed] [Google Scholar]
- 19.Lorente-Poch L, Sancho J, Muñoz JL, Gallego-Otaegui L, Martínez-Ruiz C, Sitges-Serra A. Failure of fragmented parathyroid gland autotransplantation to prevent permanent hypoparathyroidism after total thyroidectomy. Langenbeck’s Archives of Surgery 2017. 402 281–287. ( 10.1007/s00423-016-1548-3) [DOI] [PubMed] [Google Scholar]
- 20.Mann B, Buhr HJ. Lymph node dissection in patients with differentiated thyroid carcinoma--who benefits? Langenbeck’s Archives of Surgery 1998. 383 355–358. ( 10.1007/s004230050148) [DOI] [PubMed] [Google Scholar]
- 21.Paek SH, Lee YM, Min SY, Kim SW, Chung KW, Youn YK. Risk factors of hypoparathyroidism following total thyroidectomy for thyroid cancer. World Journal of Surgery 2013. 37 94–101. ( 10.1007/s00268-012-1809-4) [DOI] [PubMed] [Google Scholar]
- 22.Ondik MP, McGinn J, Ruggiero F, Goldenberg D. Unintentional parathyroidectomy and hypoparathyroidism in secondary central compartment surgery for thyroid cancer. Head and Neck 2010. 32 462–466. [DOI] [PubMed] [Google Scholar]
- 23.Rix TE, Sinha P. Inadvertent parathyroid excision during thyroid surgery. Surgeon 2006. 4 339–342. ( 10.1016/S1479-666X(06)80108-3) [DOI] [PubMed] [Google Scholar]
- 24.Lin DT, Patel SG, Shaha AR, Singh B, Shah JP. Incidence of inadvertent parathyroid removal during thyroidectomy. Laryngoscope 2002. 112 608–611. ( 10.1097/00005537-200204000-00003) [DOI] [PubMed] [Google Scholar]
- 25.Su A, Wang B, Gong Y, Gong R, Li Z, Zhu J. Risk factors of hypoparathyroidism following total thyroidectomy with central lymph node dissection. Medicine 2017. 96 e8162. ( 10.1097/MD.0000000000008162) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Su AP, Wei T, Liu F, Gong YP, Li ZH, Zhu JQ. Use of carbon nanoparticles to improve lymph nodes dissection and identification of parathyroid glands at thyroidectomy for papillary thyroid cancer. International Journal of Clinical and Experimental Medicine 2016. 9 19529–19536. [Google Scholar]
- 27.Song CM, Jung JH, Ji YB, Min HJ, Ahn YH, Tae K. Relationship between hypoparathyroidism and the number of parathyroid glands preserved during thyroidectomy. World Journal of Surgical Oncology 2014. 12 200. ( 10.1186/1477-7819-12-200) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.NCCN guidelines: thyroid carcinoma. Version 3, 2011. Fort Washington, PA, USA: NCCN. [Google Scholar]
- 29.Lahey FH. The transplantation of parathyroids in partial thyroidectomy. Surgery, Gynecology and Obstetrics 1926. 62 508–509. [Google Scholar]
- 30.Lo CY, Lam KY. Postoperative hypocalcemia in patients who did or did not undergo parathyroid autotransplantation during thyroidectomy: a comparative study. Surgery 1998. 124 1081–1086. ( 10.1067/msy.1998.92560) [DOI] [PubMed] [Google Scholar]
- 31.Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. British Journal of Surgery 2014. 101 307–320. ( 10.1002/bjs.9384) [DOI] [PubMed] [Google Scholar]
- 32.Testini M, Rosato L, Avenia N, Basile F, Portincasa P, Piccinni G, Lissidini G, Biondi A, Gurrado A, Nacchiero M. The impact of single parathyroid gland autotransplantation during thyroid surgery on postoperative hypoparathyroidism: a multicenter study. Transplantation Proceedings 2007. 39 225–230. ( 10.1016/j.transproceed.2006.10.192) [DOI] [PubMed] [Google Scholar]
- 33.Cavallaro G, Iorio O, Centanni M, Porta N, Iossa A, Gargano L, Del Duca S, Gurrado A, Testini M, Petrozza V, et al. Parathyroid reimplantation in forearm subcutaneous tissue during thyroidectomy: a simple and effective way to avoid hypoparathyroidism. World Journal of Surgery 2015. 39 1936–1942. ( 10.1007/s00268-015-3070-0) [DOI] [PubMed] [Google Scholar]
- 34.Cavallaro G, Iorio O, Centanni M, Gargano L, Del Duca S, Gurrado A, Porta N, Petrozza V, Testini M, De Toma G. Parathyroid reimplantation with PR-FaST technique in unselected patients during thyroidectomy. A case series with long term follow up confirming graft vitality and parathormone production. International Journal of Surgery 2017. 39 202–205. ( 10.1016/j.ijsu.2017.01.117) [DOI] [PubMed] [Google Scholar]
- 35.Thomusch O, Machens A, Sekulla C, Ukkat J, Brauckhoff M, Dralle H. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: a multivariate analysis of 5846 consecutive patients. Surgery 2003. 133 180–185. ( 10.1067/msy.2003.61) [DOI] [PubMed] [Google Scholar]
- 36.Sorgato N, Pennelli G, Boschin IM, Ide EC, Pagetta C, Piotto A, Toniato A, De Salvo GL, Hindié E, Al-Nahhas A, et al. Can we avoid inadvertent parathyroidectomy during thyroid surgery? In Vivo 2009. 23 433–439. [PubMed] [Google Scholar]
- 37.Cho JN, Park WS, Min SY. Predictors and risk factors of hypoparathyroidism after total thyroidectomy. International Journal of Surgery 2016. 34 47–52. ( 10.1016/j.ijsu.2016.08.019) [DOI] [PubMed] [Google Scholar]
- 38.Docimo G, Ruggiero R, Casalino G, Del Genio G, Docimo L, Tolone S. Risk factors for postoperative hypocalcemia. Updates in Surgery 2017. 69 255–260. ( 10.1007/s13304-017-0452-x) [DOI] [PubMed] [Google Scholar]
- 39.Sandelin K, Skoog L, Humla S, Farnebo LO. Oestrogen, progesterone, and glucocorticoid receptors in normal and neoplastic parathyroid glands. European Journal of Surgery 1992. 158 467–472. [PubMed] [Google Scholar]
- 40.Almaden Y, Felsenfeld AJ, Rodriguez M, Cañadillas S, Luque F, Bas A, Bravo J, Torregrosa V, Palma A, Ramos B, et al. Proliferation in hyperplastic human and normal rat parathyroid glands: role of phosphate, calcitriol, and gender. Kidney International 2003. 64 2311–2317. ( 10.1046/j.1523-1755.2003.00331.x) [DOI] [PubMed] [Google Scholar]
- 41.Dufour DR, Wilkerson SY. Factors related to parathyroid weight in normal persons. Archives of Pathology and Laboratory Medicine 1983. 107 167–172. [PubMed] [Google Scholar]
- 42.Toniato A, Boschin IM, Piotto A, Pelizzo MR, Guolo A, Foletto M, Casalide E. Complications in thyroid surgery for carcinoma: one institution’s surgical experience. World Journal of Surgery 2008. 32 572–575. ( 10.1007/s00268-007-9362-2) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a