Abstract
Background:
Although sleep problems are well characterized in pre-school and school-age children with neurogenetic syndromes, little is known regarding the early emergence of these problems in infancy and toddlerhood. To inform syndrome-specific profiles and targets for intervention, we contrasted parent-reported sleep problems in infants and toddlers with Angelman Syndrome (AS), Williams Syndrome (WS), and Prader-Willi Syndrome (PWS) to patterns observed among same-aged typically developing (TD) controls.
Methods:
Mothers of 80 children (18 AS, 19 WS, 19 PWS, 24 TD) completed the Brief Infant Sleep Questionnaire. Primary dependent variables included: (1) sleep onset latency (2) total sleep duration, (3) daytime and nighttime sleep duration, and (4) sleep problem severity, as measured by both maternal impression and National Sleep Foundation guidelines.
Results:
Sleep problems were relatively common in children with neurogenetic syndromes, with 41% of mothers reporting problematic sleep and 29% of children exhibiting abnormal sleep durations per national guidelines. Across genetic subgroups, problems were most severe in AS and WS, particularly in relation to nighttime sleep duration. Although atypical sleep is characteristically reported in each syndrome later in development, infants and toddlers with PWS exhibited largely typical patterns, potentially indicating delayed onset of sleep problems in concordance with other medical features of PWS.
Conclusions:
Our findings suggest that sleep problems in neurogenetic syndromes emerge as early as infancy and toddlerhood, with variable profiles across genetic subgroups. This work underscores the importance of early sleep screenings as part of routine medical care of neurosyndromic populations and the need for targeted, syndrome-sensitive treatment.
Keywords: Sleep, Angelman Syndrome, Williams Syndrome, Prader-Willi Syndrome, Infants
1. Introduction
Children with neurogenetic syndromes are high-risk for comorbid sleep problems, including increased sleep latency, frequent and prolonged night waking, and short sleep duration1. Sleep problems in preschool and school-aged children with neurogenetic syndromes have been well-documented, occurring in up to 86% of children,2 and are known to impact child behavior problems3 and parental stress4. In typically developing infants, sleep problems have been associated with a number of negative outcomes including impaired cognitive development5, emotion dysregulation6, and attention problems7. However, despite the pervasive rates of sleep problems and debilitating impact of sleep on child and family functioning, few studies have examined sleep problems in neurogenetic syndromes during infancy and early childhood. The paucity of research in this area substantially limits our knowledge of when and how sleep problems emerge, constraining targeted and effective early treatment options.
To address this need, the present study evaluated parent-reported sleep problems in infants and toddlers with three low-incidence neurogenetic syndromes: Angelman syndrome (AS; prevalence 1:10,000-20,0008), Prader-Willi syndrome (PWS; 1:7,500-10,0008), and Williams syndrome (WS; 1:15,000-30,0008), relative to typically developing (TD) controls. In later childhood and adulthood, sleep problems in AS include reduced total sleep time9, increased sleep onset latency10, and frequent and prolonged night wakings11. In contrast, PWS is associated with excessive daytime sleepiness2, sleep apnea, reduced sleep quality1, and early waking12. Individuals with WS are generally reported to exhibit the mildest sleep concerns of these groups, with increased sleep onset latency, decreased sleep efficiency13, daytime sleepiness13,14, and more frequent night arousals and wakings14. Thus, although sleep problems are expected across these syndromes, variations in topography and severity in childhood suggests that infant profiles may similarly vary across groups, requiring syndrome-specific plans of care.
The goals of this study were to (1) contrast early childhood sleep profiles across infants and toddlers with and without neurogenetic syndromes, including sleep latency, duration, night waking, and global parent impressions, and (2) examine the magnitude of sleep problems relative to established national guidelines.
2. Methods
2.1. Participants and procedure
Participants included 80 infants and toddlers with AS (n=18), WS (n=19), PWS (n=19), and TD (n=24). Data were drawn from the Early Phenotype Survey and, an ongoing longitudinal study of early development in low-incidence neurogenetic syndromes. Families were recruited through web-based support groups and social networks, including the Angelman Syndrome Foundation and Registry (www.angelman.org) and Williams Syndrome Association and Registry (www.williams-syndrome.org/registry). All recruitment, consent, and procedures were approved by the Institutional Review Board at Purdue University. Families were required to primarily speak English for enrollment, and the TD group was excluded if they were born <37 weeks, had significant surgeries that may impact sleep, or had a family history of developmental delay, intellectual disability, or other neurogenetic conditions. Groups were matched for age and sex (% male: AS=53%, PWS=42%, WS=58%). Eighteen percent of syndromic participants were born preterm (AS n=3, PWS n=6, WS n=1), consistent with higher rates of preterm birth in these populations. Analyses repeated without preterm infants generally yielded similar effect sizes, and any inconsistencies are reported in-text. Groups did not differ across socio-economic variables, as detailed in Supplemental Table 1.
Parents reported child genetic status and completed syndrome-specific screening questions, with 74% of cases confirmed with genetic report (AS=63%, PWS=89%, WS=68%). AS subtypes included maternal deletion (83%, n=15), UBE3A mutation (11%, n=2), and uniparental disomy (6%, n=1). PWS subtypes included paternal deletion (68%; n=13) and maternal uniparental disomy (32%, n=6). Medications to target sleep and seizures were most common in the AS group (sleep=3, seizure=9; PWS sleep=0, seizure=1; WS sleep=0, seizure=0).
2.2. Measures
Biological mothers completed the Brief Infant Sleep Questionnaire (BISQ)15, a 12-item parent-report measure of sleep-related behaviors previously validated against both actigraphy and parent-report sleep diaries.15 Mothers were instructed to complete the BISQ on their child’s sleep over the past week. Primary dependent variables included: (1) nighttime sleep onset latency in minutes (Item 7), (2) total sleep duration per 24-hours (Items 3 & 4), (3) daytime (Item 4) and nighttime sleep duration (Item 3), and (4) whether mothers rated sleep as a “very serious problem” rather than “a small problem” or “not a problem at all” when asked “Do you consider your child’s sleep a problem?” (Item 10). We also determined whether total sleep duration fell outside of “recommended” sleep duration ranges set by the National Sleep Foundation16 (ages 4-11 months: 12-15h; 1-2 years: 11-14h; 3-5 years: 10-13h).
2.3. Statistical analyses
Analyses were performed in SAS 9.4 (SAS Institute, Cary, NC) using nonparametric methods appropriate to small samples and outliers. We contrasted sleep in TD versus each syndromic group using Wilcoxon-Mann-Whitney Tests (sleep latency, duration, and waking variables) and Fisher Exact Tests (categorical parent impressions and national guidelines) using α<.05. Effect sizes are reported using Cohen’s d or odds ratios, as appropriate. We also calculated a Levene’s homogeneity of variance statistic for each continuous pairwise comparison to determine whether variability in sleep parameters differed by group. Next, we conducted several supplemental analyses to contextualize our primary findings, including (1) pairwise syndromic comparisons, (2) post-hoc within-group analysis of AS-specific factors (e.g. subtype, medication use) that may have contributed to group differences, and (3) within-group comparisons of age across participants with and without clinically-indicated sleep concerns (Wilcoxon-Mann-Whitney Tests). See Supplemental Tables 2-4.
3. Results
Sleep Latency.
Table 1 includes primary analyses contrasting each syndrome group to TD controls. Across syndromic groups, parents reported a median sleep latency of 15 minutes, relative to 30 minutes in controls. Relative to TD controls, sleep latency was significantly shorter in PWS (d=0.95) and marginally shorter in AS (d=0.43). Supplemental pairwise comparisons (Supplemental Table 2) indicated the PWS and AS groups did not differ from each other. Variability in sleep latency did not differ by group (Supplemental Table 3).
Table 1.
Sleep Problems in Children with Neurogenetic Syndromes Compared to Typical Controls
| Median (range) | Wilcoxon Z p | ||||||
|---|---|---|---|---|---|---|---|
| Angelman (AS) | Prader-Willi (PWS) | Williams (WS) | Control (TD) | AS v TD | PWS v TD | WS v TD | |
| n | 18 | 19 | 19 | 24 | |||
| Sex (% male) | 52.63 | 42.11 | 58.33 | 57.89 | |||
| Age in Months | 18 (8-45) | 22 (10-44) | 20 (6-46) | 24 (6-44) | |||
| Night Sleep Latency | 15 (0-120) | 10 (0-60) | 20 (0-120) | 30 (2-90) | −1.94(.051) | −2.74(.006) | −.58(.562) |
| Total Sleep Duration | 660 (360-870) | 765 (630-900) | 720 (570-840) | 728 (630-960) | −2.14(.031) | .70(.482) | −1.81(.070) |
| Daytime | 120 (0-480) | 120 (60-330) | 120 (0-240) | 120 (0-300) | 1.14(.256) | 1.38(.167) | .35(.725) |
| Nighttime | 540 (240-660) | 630 (480-720) | 600 (480-720) | 630 (390-840) | −3.46(.001) | −.41(.681) | −2.07(.039) |
| Night Waking Frequency | 1 (0-10) | 1 (0-2) | 1 (0-5) | 1 (0-3) | .32(.584) | −.81(.420) | −.69(.495) |
| Night Waking Duration | 40 (0-300) | 0 (0-60) | 5 (0-60) | 3 (0-150) | 2.26(.029) | −.49(.629) | −.07(.948) |
| % Endorsed (n) | Fisher’s Exact Test p | ||||||
| AS | PWS | WS | TD | AS v TD | PWS v TD | WS v TD | |
| Any Parent Problem | 50 (9) | 16 (3) | 61 (11) | 38 (9) | .533 | .174 | .212 |
| Small Problem | 22 (4) | 16 (3) | 56 (10) | 38 (9) | .333 | .174 | .350 |
| Very Serious Problem | 28 (5) | 0 (0) | 5 (1) | 0 (0) | .010 | n/a | .429 |
| NSF Guidelines | 50 (9) | 16 (3) | 26 (5) | 17 (4) | .020 | .320 | .220 |
Note. National Sleep Foundation Guidelines were used to determine whether total sleep duration fell outside of “recommended” ranges based on participants’ chronological ages.
Sleep Duration.
The median sleep duration was 720 minutes (12 hours) per 24-hours across syndromic groups, with both AS (d=1.22) and WS (d=0.62) groups displaying atypically short total nighttime sleep, and the AS group also exhibiting greater variability in sleep duration relative to TD controls. Pairwise contrasts indicated marginally less nighttime sleep in AS than WS. When preterm infants were excluded, the PWS group displayed atypically longer total sleep (d=0.75), and the WS group difference approached significance in nighttime sleep (d=−0.56).
Night Waking Frequency and Duration.
Across syndromic groups, the median number of parent-reported night wakings was 1, lasting approximately 5 total minutes. The AS group exhibited atypically long night wakings (d=0.70), with waking durations over three times as long as controls. Children with AS also exhibited greater variability in duration of night wakings. Night waking frequency was not atypical across syndromic groups.
Overall Impressions.
Parents of 41% of children with neurogenetic syndromes reported “small” or “very serious” sleep problems, with atypically high rates of “very serious” problems in AS (p=.010). Although most parents of children with WS endorsed small sleep problems, this endorsement was relatively common amongst parents of control children (38%) and was therefore not statistically atypical. A substantial minority of children with neurogenetic syndromes (29%) exhibited sleep durations outside of the NSF’s “recommended” ranges, with nearly three times higher likelihood of AS relative to controls (OR=2.94).
Variable Profiles in AS.
Three AS participants exhibited statistically atypical scores (outliers) within continuous analyses (Figure 1). These participants varied in age (8-41 months), were born full-term, and varied in medication use (sleep n=1; seizure n=1) and AS subtype (deletion n=2, paternal uniparental disomy n=1). Children with AS who took sleep-related medications (classified as medications to target sleep or seizures) slept significantly less during the day than children who did not take sleep-related medications.
Figure 1.
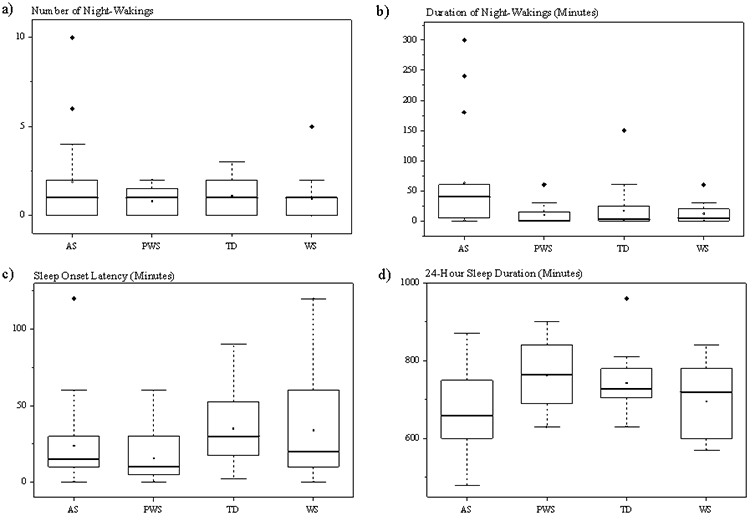
Box-and-whisker plots detailing raw score variability and outliers for core continuous sleep variables
Group Specific Age Effects.
Severity of parent-reported sleep problems did not differ by child age for parent-reported sleep concerns (AS: Wilcoxon Z=−0.88, p=.377; WS: Z=.05, p=.964; PWS: Z=−0.06, p=.955; TD: Z = 1.37, p=.170) or NSF’s “recommended” ranges (AS: Z=1.02, p=.307; WS: Z=0.32, p=.746; PWS: Z=−0.06, p=.955; TD: Z = −1.43, p = .152).
4. Discussion
Although sleep problems are common in neurogenetic syndromes, the onset and nature of sleep problems in infancy is poorly understood. The present study examined sleep profiles in three understudied neurogenetic syndromes to inform best practice clinical care and future directions for treatment. Our findings suggest that sleep problems in a subset of children with neurogenetic syndromes emerge in early development, particularly in Angelman and Williams syndromes. As sleep is a modifiable risk factor for developmental progress, our findings support the importance of screening, diagnosing and treating sleep problems in high-risk syndromic infants, laying the foundation for optimal developmental outcomes.
Angelman Syndrome.
We observed particularly atypical sleep patterns in AS, including shorter and more variable sleep duration, and longer and more variable periods of night waking. However, infants and toddlers with AS did not display abnormal sleep onset latencies or frequent night waking as observed in older children10,11. These patterns suggest that problems initiating and maintaining sleep, which are present in 48-70%17 of older children with AS,10 likely emerge in early infancy and may be targeted proactively. The variable nature of sleep and waking durations in children with AS may contribute to increased and more serious parent concerns. Indeed, 17% of our AS sample were reported to take sleep-related medications, suggesting interventions are already underway at young ages, and impairments we describe may underestimate true rates of sleep problems in non-medicated samples. These findings suggest that sleep problems in AS are more extensive than problems observed in several other neurogenetic syndromes, warranting further research to develop syndrome-specific screening and intervention protocols that may minimize the negative developmental implications for this population.
Williams Syndrome.
Sleep problems were also elevated in infants and toddlers with WS, consistent with evidence that 36-57% of older children with WS exhibiting problems related to sleep initiation, night waking, and sleep duration17. Indeed, our results suggest that, even in early childhood, parents report shorter nighttime sleep duration in WS, with the majority indicating sleep is problematic for their child. Notably, previous studies report atypically long sleep onset latencies and frequent night waking14 in older children with WS18,19, whereas sleep onset latencies and waking frequency in our infant and toddler sample did not differ from TD controls. This discrepancy may indicate that the topography of sleep problems changes across development in WS, with minor sleep problems emerging in infancy that may continue to intensify with age.
Prader-Willi Syndrome.
Although sleep problems are reported in 35-69%2,12,20 of older children with PWS, parent-reported sleep problems were minimal in our infant and toddler sample. This discrepancy likely reflects that core PWS symptoms associated with sleep problems, such as hyperphagia and obesity20, emerge later in development. The BISQ also does not capture many sleep concerns associated with PWS, such as excessive daytime sleepiness12 and sleep-disordered breathing20. Our data suggest that infants and toddlers with PWS sleep more than children with other syndromes, which may indicate the early emergence of excessive sleepiness seen in older children2. Although the low rates of parent-reported sleep concerns we observed suggest these sleep problems are likely minimal or absent in our PWS sample, future work is needed to characterize the emergence of these features in PWS across childhood.
Summary, Limitations and Conclusions.
Together, our findings suggest that sleep problems emerge as early as infancy and toddlerhood in a subset of children with neurogenetic syndromes, with different profiles emerging across genetic subgroups. Specifically, children with AS and WS exhibit reduced nighttime sleep durations that likely persist and intensify later in development, whereas children with PWS exhibit largely typical sleep patterns, potentially indicating delayed onset of problems in concordance with other medical features of PWS. This study provides novel information about the nature and severity of infant and toddler sleep profiles across AS, PWS, and WS—thus laying the foundation for the development of higher quality, targeted, and preventative treatment approaches. Despite these strengths, limitations include reliance on parent-reported sleep data and small sample sizes common to low-incidence infant neurogenetic studies. Future work is needed to replicate our findings in larger samples, assess the stability of sleep problems across childhood, and investigate the intersection of sleep with other problem behaviors and family functioning over time. This program of research will clarify best practice for screening, diagnosing and treating emergent sleep problems in neurogenetic syndromes, maximizing positive outcomes for affected children and families.
Supplementary Material
Acknowledgements
We thank the families enrolled in the Early Phenotype Survey for their participation in this research. We also thank the Angelman Syndrome Foundation and Registry (www.angelman.org) and Williams Syndrome Association and Registry (www.williams-syndrome.org/registry) for facilitating recruitment. We also thank Natalie Bengert and Maddie Holen for study coordination. Families may learn more about the Early Phenotype Survey by visiting http://nddfamilylab.weebly.com/.
Footnotes
Conflict of Interest
The authors report no conflicts of interest.
References
- 1.Robinson-Shelton A, Malow BA. Sleep Disturbances in Neurodevelopmental Disorders. Curr Psychiatry Rep. 2016;18(1):6. doi: 10.1007/s11920-015-0638-1. [DOI] [PubMed] [Google Scholar]
- 2.Cotton S, Richdale A. Brief report: Parental descriptions of sleep problems in children with autism, Down syndrome, and Prader-Willi syndrome. Res Dev Disabil. 2006;27(2):151–161. doi: 10.1016/j.ridd.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Didden R, Korzilius H, Van Aperlo B, Van Overloop C, De Vries M. Sleep problems and daytime problem behaviours in children with intellectual disability. J Intellect Disabil Res. 2002;46(7):537–547. doi: 10.1046/j.1365-2788.2002.00404.x. [DOI] [PubMed] [Google Scholar]
- 4.Goldman SE, Bichell TJ, Surdyka K, Malow BA. Sleep in children and adolescents with Angelman syndrome: Association with parent sleep and stress. J Intellect Disabil Res. 2012;56(6):600–608. doi: 10.1111/j.1365-2788.2011.01499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kocevska D, Rijlaarsdam J, Ghassabian A, et al. Early Childhood Sleep Patterns and Cognitive Development at Age 6 Years: The Generation R Study. J Pediatr Psychol. 2016;42(January 2016):jsv168. doi: 10.1093/jpepsy/jsv168. [DOI] [PubMed] [Google Scholar]
- 6.Mindell JA, Leichman ES, DuMond C, Sadeh A. Sleep and Social-Emotional Development in Infants and Toddlers. J Clin Child Adolesc Psychol. 2016;46(2):1–11. doi: 10.1080/15374416.2016.1188701. [DOI] [PubMed] [Google Scholar]
- 7.Sadeh AMGYAL-HY. Infant Sleep Predicts Attention Regulation and Behavior Problems at 3–4 Years of Age. Dev Neuropsychol. 2015;40(3):122–137. doi: 10.1080/87565641.2014.973498. [DOI] [PubMed] [Google Scholar]
- 8.Hansen RL, Rogers SJ, eds. Autism and Other Neurodevelopmental Disorders. Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- 9.Walz NC, Beebe D, Byars K. Sleep in individuals with Angelman syndrome: parent perceptions of patterns and problems. Am J Ment Retard. 2005;110(4):243–252. doi: 10.1352/0895-8017(2005)110[;243:SIIWAS];2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Bruni O, Ferri R, D’Agostino G, Miano S, Roccella M, Elia M. Sleep disturbances in Angelman syndrome: A questionnaire study. Brain Dev. 2004;26(4):233–240. doi: 10.1016/S0387-7604(03)00160-8. [DOI] [PubMed] [Google Scholar]
- 11.Pelc K, Cheron G, Boyd SG, Dan B. Are there distinctive sleep problems in Angelman syndrome? Sleep Med. 2008;9(4):434–441. doi: 10.1016/j.sleep.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Richdale AL, Cotton S, Hibbit K. Sleep and behaviour disturbance in Prader-Willi syndrome: A questionnaire study. J Intellect Disabil Res. 1999;43(5):380–392. doi: 10.1046/j.1365-2788.1999.043005380.x. [DOI] [PubMed] [Google Scholar]
- 13.Goldman SE, Malow BA, Newman KD, Roof E, Dykens EM. Sleep patterns and daytime sleepiness in adolescents and young adults with Williams syndrome. J Intellect Disabil Res. 2009;53(2):182–188. doi: 10.1111/j.1365-2788.2008.01140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Annaz D, Hill CM, Ashworth A, Holley S, Karmiloff-Smith A. Characterisation of sleep problems in children with Williams syndrome. Res Dev Disabil. 2011;32(1):164–169. doi: 10.1016/j.ridd.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Sadeh A A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–7. doi: 10.1016/s0022-3476(87)80571-1. [DOI] [PubMed] [Google Scholar]
- 16.Hirshkowitz M, Whiton K, Albert SM, et al. National sleep foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Heal. 2015;1(1):40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Tietze A-L, Blankenburg M, Hechler T, et al. Sleep disturbances in children with multiple disabilities. Sleep Med Rev. 2012;16(2):117–127. doi: 10.1016/j.smrv.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Esbensen AJ, Schwichtenberg AJ. Sleep in Neurodevelopmental Disorders. Vol 51. Elsevier Ltd; 2016. doi: 10.1016/bs.irrdd.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mason TBA, Arens R, Sharman J, et al. Sleep in children with Williams Syndrome. Sleep Med. 2011;12(9):892–897. doi: 10.1016/j.sleep.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Donoghue FJ, Camfferman D, Kennedy JD, et al. Sleep-disordered breathing in Prader-Willi syndrome and its association with neurobehavioral abnormalities. J Pediatr. 2005;147(6):823–829. doi: 10.1016/j.jpeds.2005.07.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


