Abstract
Lymphoma is one of the most common cancers of the orbital and lacrimal glands, after squamous cell carcinoma and melanoma. Based on cell origin, most lymphoma cases are classified as non–Hodgkin lymphoma. Orbital lymphoma can be either primary or secondary. The clinical manifestations of lymphoma are diverse, with the most common symptoms being bilateral or unilateral proptosis, limited eye motility, swelling, pain, changes in visual acuity, and diplopia. In this article, we describe the case of a 6-year-old male who presented with bilateral rapid orbital swelling for 10 days. This patient underwent surgical biopsy, and the final diagnosis was bilateral orbital secondary non–Hodgkin lymphoma.
Keywords: Orbital lymphoma, Diffuse large B-cell lymphoma, Non–-Hodgkin's lymphoma
Introduction
Orbital lymphoma is an uncommon form of extranodal lymphoma; however, it is one of the most common malignant tumors of the orbit [1]. Orbital lymphoma represents approximately 4%-13% of malignant orbital tumors [1]. Non–Hodgkin lymphoma has been reported to be the most common type of ocular lymphoma, accounting for 55% of all orbital tumors [2]. Olsen et al. [3] reported that up to 97% of orbital lymphoma tumors originate from B-cells. Orbital lymphoma typically affects adults older than 50 years [4]. Proptosis and eyelid swelling are the 2 most common clinical symptoms [1]. Our study aimed to illustrate a rare case of bilateral, orbital, secondary, non–Hodgkin lymphoma.
Case report
A 6-year-old male presented to the hospital with rapid bilateral orbital swelling for 10 days. This patient had a 2-months’ history of weight loss, losing 3 kg without anorexia or fever. The patient had previously been diagnosed with L2 acute lymphoblastic leukemia and was treated with the French Acute Lymphoblastic Leukemia (FRALLE) B2 regimen. The clinical examination revealed no changes in visual acuity or diplopia. Laboratory studies showed a normal complete blood count. Facial magnetic resonance imaging (MRI) displayed bilateral lacrimal gland enlargement, with well-defined boundaries and intermediate intensity on T2-weighted and fluid attenuation inversion recovery (FLAIR) imaging (Fig. 1). Both lacrimal glands were diffusely iso-intense compared with the white matter on the T1-weighted image and were homogenously enhanced on the T1-weighted image with contrast agent (Fig. 2). The histologic examination of the right lacrimal surgical biopsy revealed the diffuse infiltration of malignant large lymphoid cells. Immunohistochemical staining results were compatible with diffuse large B-cell lymphoma. Ten days after admission, the patient reported pain in the pelvis and both hip joints. The pathologic results for pelvic biopsy revealed diffuse large B-cell lymphoma (Fig. 3). The definitive diagnosis was diffuse large B-cell lymphoma with secondary bilateral lacrimal involvement.
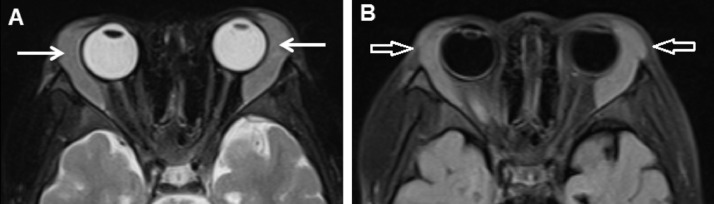
Fig. 1.
Bilateral lacrimal glands were enlarged, with well-circumscribed borders, and intermediate intensity on T2-weighted (A, arrows) and FLAIR (B, arrows) imaging.
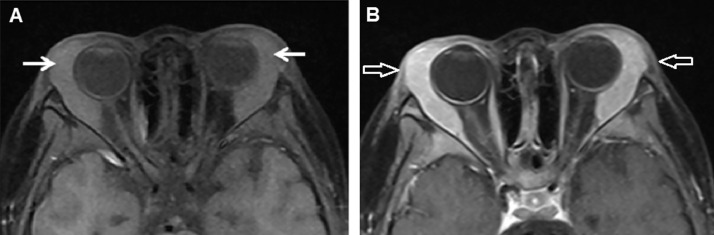
Fig. 2.
The lesions are iso-intense compared to the white matter on T1-weighted imaging (A, arrows) and homogenously enhanced (B, arrows).
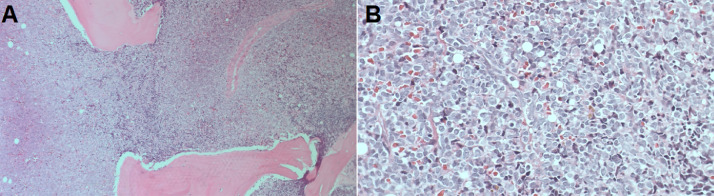
Fig. 3.
Hematoxylin and eosin (HE) staining, (A) × 10, (B) × 40. The normal bone marrow structure was completely replaced by the diffuse infiltration of large malignant lymphoid cells.
Discussion
Orbital lymphomas are a heterogeneous group of tumors, most of which are low-grade tumors [5]. This disease has a male predominance [3]. The tumor may be located in the intraconal space (11%), the extraconal space (42%), the lacrimal gland (47%), conal muscles, or optic nerve [6]. The diagnosis of primary ocular adnexal lymphoma is based on (1) a biopsy consistent with orbital lymphoma, with no evidence of lymphoma in any other organs after a full clinical evaluation; and (2) no prior history of lymphoma disease [7]. Secondary orbital lymphoma is defined when orbital lymphoma is associated with lymphoma or a history of lymphoma originating from other organs [3]. Approximately 73% of orbital B-cell lymphoma cases are identified as primary lymphomas [3]. Patients with orbital lymphoma may present with variable symptoms, including periorbital tumor mass, exophthalmos, ocular pain, ocular movement, visual restrictions, and diplopia [8]. Most cases present with unilateral lesions [8]. Computed tomography (CT) scans typically show a slightly high-density, homogenous mass with mild contrast enhancement [5]. CT scans allow for the evaluation of bone invasion by the orbital lymphoma [5]. On MRI, this neoplasm appears as an isointense mass relative to the brain parenchyma on T1-weighted images and as isointense or hyperintense on T2-weighted images [5]. On MRI after contrast injection, the lesion shows moderate enhancement [9]. When tumors are located in the intraconal space, the differential diagnosis includes meningioma and glioma; however, when the mass involves both the intra- and extraconal compartments, the differential diagnosis includes inflammatory pseudotumor, lacrimal gland tumor, and orbital metastasis [6]. The treatment of orbital lymphoma depends on the histologic type and the extension of the tumor, and treatment modalities include radiation therapy, chemotherapy, and surgery [10]. The prognosis depends on the histologic type, the clinical stage at presentation, and the primary location of the disease [5]. Martinet et al. [11] reported that the 5-year overall survival of orbital lymphoma was 78%.
This patient had a history of acute lymphoblastic leukemia; therefore, the diagnosis of secondary orbital lymphoma was easy to make. The orbit is a lymphoma location that could be caused by a metastasis from leukemia; therefore, in cases associated with abnormal symptoms of the eye and a history of lymphoma, clinicians should first consider metastasis and avoid the unnecessary biopsy of multiple organs.
Conclusion
Bilateral secondary orbital lymphoma is quite uncommon. The physician should consider the tumor origins, especially in patients with primary lymphoma. CT scans and MRI play crucial roles in assessing the lesion and its relationships with neighboring structures. Chemotherapy remains a commonly applied treatment strategy for this disease.
Patient consent
Informed consent for patient information to be published in this article was obtained.
Ethical statement
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Author contributions
All authors contributed to this article as co-first authors. All authors have read the manuscript and agree to the contents.
Footnotes
Nguyen VS and Nguyen MD contributed equally to this article as co-first authors.
Acknowledgments: Self-financed.
Competing Interests: The authors do not report any conflicts of interest.
References
- 1.Sriram P. A rare case of aggressive, huge primary orbital lymphoma with intracranial extension and bone invasion. Asian J Neurosurg. 2017;12(4):766. doi: 10.4103/1793-5482.185055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Margo CE, Mulla ZD. Malignant tumors of the orbit. Ophthalmology. 1998;105(1):185–190. doi: 10.1016/S0161-6420(98)92107-8. [DOI] [PubMed] [Google Scholar]
- 3.Olsen TG, Heegaard S. Orbital lymphoma. Surv Ophthalmol. 2019;64(1):45–66. doi: 10.1016/j.survophthal.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Hassan WM, Bakry MS, Hassan HM, Alfaar AS. Incidence of orbital, conjunctival and lacrimal gland malignant tumors in USA from surveillance, epidemiology and end results, 1973-2009. Int J Ophthalmol. 2016;9(12):1808–1813. doi: 10.18240/ijo.2016.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerbino G, Boffano P, Benech R, Baietto F, Gallesio C, Arcuri F. Orbital lymphomas: Clinical and radiological features. J Cranio-Maxillofac Surg. 2014;42(5):508–512. doi: 10.1016/j.jcms.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Priego G, Majos C, Climent F, Muntane A. Orbital lymphoma: imaging features and differential diagnosis. Insights Imaging. 2012;3(4):337–344. doi: 10.1007/s13244-012-0156-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rasmussen PK, Ralfkiaer E, Prause JU, Sjö LD, Specht L, Rossing HH. Follicular lymphoma of the ocular adnexal region: A nation-based study. Acta Ophthalmol (Copenh) 2015;93(2):184–191. doi: 10.1111/aos.12525. [DOI] [PubMed] [Google Scholar]
- 8.Tőrők-Vistai T, Bojan A, Cucuianu A, Zsoldos A. Primary non-Hodgkin lymphoma of the orbit presenting with massive bilateral periorbital tumors. Clujul Med 1957. 2013;86(4):380–382. [PMC free article] [PubMed] [Google Scholar]
- 9.Sun B, Song L, Wang X, Li J, Xian J, Wang F. Lymphoma and inflammation in the orbit: Diagnostic performance with diffusion-weighted imaging and dynamic contrast-enhanced MRI: DWI and DCE-MRI of OLPDs. J Magn Reson Imaging. 2017;45(5):1438–1445. doi: 10.1002/jmri.25480. [DOI] [PubMed] [Google Scholar]
- 10.Eckardt AM, Lemound J, Rana M, Gellrich NC. Orbital lymphoma: diagnostic approach and treatment outcome. World J Surg Oncol. 2013;11(1):73. doi: 10.1186/1477-7819-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martinet S, Ozsahin M, Belkacémi Y, Landmann C, Poortmans P, Oehlere C. Outcome and prognostic factors in orbital lymphoma. Int J Radiat Oncol. 2003;55(4):892–898. doi: 10.1016/S0360-3016(02)04159-7. [DOI] [PubMed] [Google Scholar]