Abstract
In this paper, we describe a rare case of coronary artery aneurysms occasionally found on a pre interventional Coronary Computed Tomography Angiography performed on a 67-year-old man with a history of aneurysm of the ascending aorta previously treated with Bentall surgery, who arrived at our hospital to have a percutaneous valve-in-valve implantation procedure. Even though the patient was considered not eligible for the procedure, due to his many comorbidities, and conservatively managed, at 1-year followup his angiographic condition remained stable.
Keywords: Coronary artery aneurysm, Transcatheter aortic valve replacement, Coronary computed tomography angiography
A coronary artery aneurysm (CAAs) is defined as a coronary artery dilation exceeding the diameter of the normal adjacent segments or the diameter of the largest coronary artery by 1.5 times [1]. The incidence of CAAs increased with the advent of coronary angiography and it varies from 0.3%-5.3% [2]. When the diameter of the vessel is greater than 20.0 mm, the aneurysm can be defined as a giant coronary artery aneurysm, which is an extremely rare entity with an incidence rate as low as 0.02% [3]. Many causes have been recognized in the etiology of this disease, the most frequent of which are atherosclerosis, Kawasaki disease, iatrogenic wall injury (eg after Percutaneous Transluminal Coronary Angioplasty - PTCA), endocarditis and connective tissue disorders (Marfan or Ehlers-Danlos syndromes), with some differences depending on the geographic area [1].
In this case report, we describe a giant coronary aneurysm of the left circumflex artery (LCX) and the left anterior descending artery (LAD) occasionally found in a patient with no history of the common etiologic factors for this disease, who underwent a Bentall procedure 10 years before to treat an aneurysm of the ascending aorta more likely related to atherosclerosis. Bentall procedure was first described in 1968 by Bentall and De Bono [4] and consists of the replacement of both the ascending aorta and the aortic valve through a composite graft followed by direct side-to-side coronary arteries reimplantation and graft wrapping by the residual aneurysmal wall. Post Bentall complications involving the coronary arteries are more often located at the level of the ostial anastomosis and can be differentiated in pseudoaneurysms, more frequent, and true ostial aneurysms, that are strongly correlated with hereditary collagen defects, such as Marfan syndrome [5]. Instead, true aneurysms of the coronary artery extending along the vessel itself are very rare [6].
Case study
A 67-year-old man with a history of an ascending aorta aneurysm operated in the past with Bentall procedure arrived at our cardiology department to have percutaneous valve-in-valve implantation. The patient had a history of hypertension, diabetes, Chronic Obstructive Pulmonary Disease (COPD), obesity and severe dyslipidemia. He also had previously undergone a stenting procedure due to an inferior-posterior ST-Segment Elevation Myocardial Infarction (STEMI) and a right hemicolectomy because of colorectal cancer still in follow up [7], [8]–9]. Due to this complex clinical scenario associated with an increased likelihood of intra- and peri-procedural complications, the patient was considered to be at high surgical risk by the Heart Team of our institution. Therefore, the final decision was to perform a valve-in-valve Transcatheter Aortic Valve Implantation (TAVI) [10].
A pre-interventional imaging investigation was performed with a 512-slice CT (GE-Healthcare CT Revolution System, General Electric, Milwaukee, WI, USA) using a retrospectively ECG-triggered high-pitch spiral acquisition mode. All the acquired images were transferred to an external workstation (ADW-6,7; GE-Healthcare) for the post processing analysis. After the non–contrast CT scan, a bolus of nonionic iso-osmolar contrast agent with an iodine concentration of 400.0 mg/ml was injected into an antecubital vein of the patient through a 20 gauge catheter using a dual-short injector (Nemoto Kyorindo, Tokyo, Japan) [11], [12], [13], [14]–15].
The pre interventional basal scan showed abnormal findings on the coronary arteries. Precisely, we observed a complete occlusion of the right coronary artery at its middle tract that has never been documented in the previous exams.
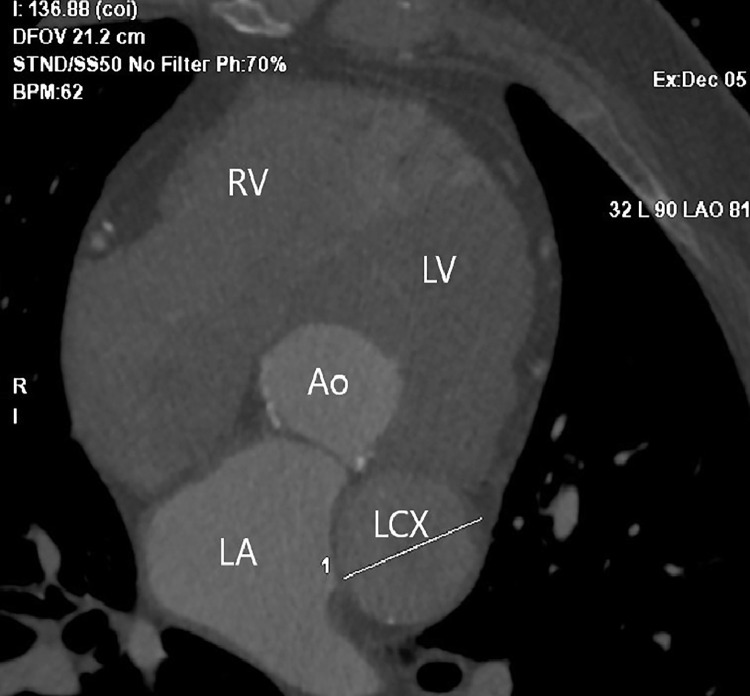
Moreover, the Coronary Computed Tomography Angiography (CCTA) scan showed a giant aneurysm of LCX at its proximal and middle tract characterized by an oval shape and with axial diameters of almost 40.0 mm × 60.0 mm (Figs. 1 and 2).
Fig. 1.
Cardiac CT scan evaluation shows the transverse diameter of the giant aneurysm of the left circumflex coronary artery (LCX) measured on an axial view obtained detecting the real axial plane of the vessel with multi-planar reconstruction (MPR). Ao, aorta; LA, left atrium; LV, left ventricle; RV, right ventricle; LCX, left circumflex coronary artery.
Fig. 2.
(A) Axial Cardiac CT scan showing the origin of the left circumflex coronary artery (LCX). (B) Coronal Cardiac CT Multiplanar Reconstruction (MPR) showing the origin of LCX. (C) Axial Cardiac CT scan showing the distal tract of LCX.
Due to his high surgical risk related to the general conditions and the many risk factors, the Heart Team decided not to operate on the patient to correct the CAAs but to manage him conservatively with a regular follow-up.
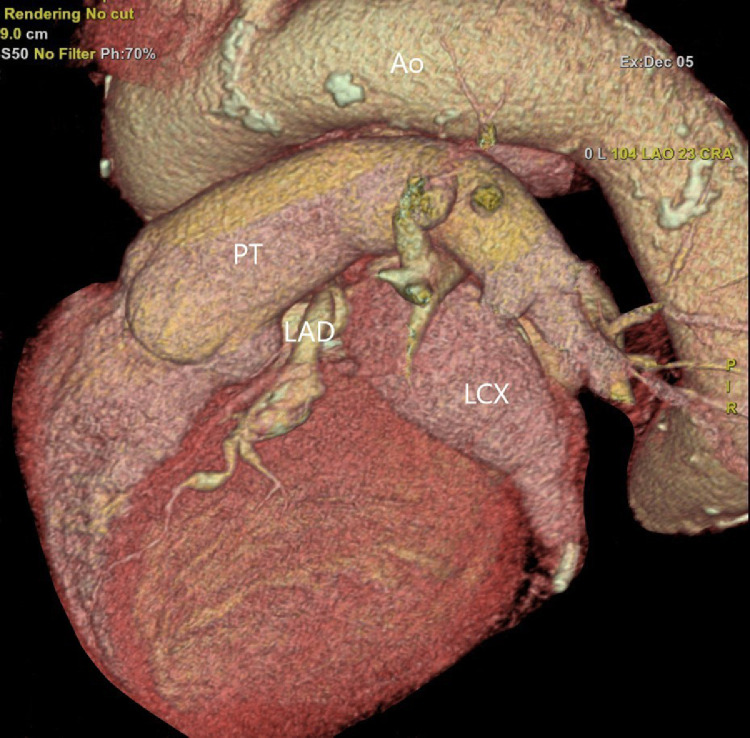
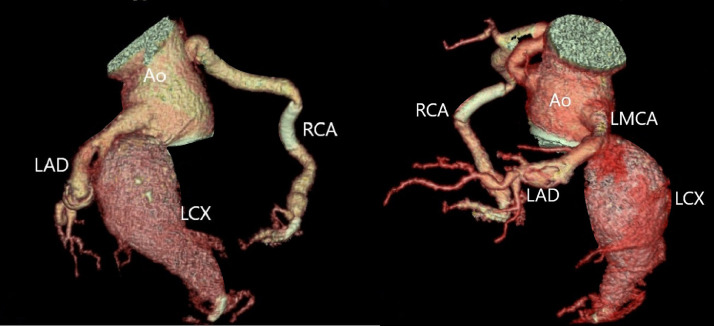
A coronary computed 3D tomography was also performed to precisely evaluate the size and morphology of the aneurysm as well as its relationship with the surrounding structures (Figs. 3 and 4).
Fig. 3.
Volume Rendering of the heart with projections dedicated to the visualization of the giant aneurysm of the left circumflex coronary artery (LCX). Ao, aorta; PT, pulmonary trunk; LAD, left anterior descending artery; LCX, left circumflex coronary artery.
Fig. 4.
Volume Rendering of a giant aneurysm of the left circumflex coronary artery (LCX). It is observed a reduced enhancement of the aneurysmatic sac due to the turbulence of the blood flow. The left anterior descending artery (LAD) and right coronary artery (RCA) appear ectatic. Drug eluted stents are documented downstream of the aneurysm on the origin of the first marginal branch and right coronary artery. Ao, aorta; LAD, left anterior descending artery. LCX, left circumflex coronary artery; RCA, right coronary artery; LMCA, left main coronary artery.
The patient was dismissed after a few days with a medical therapy based on aspirin 100.0 mg, clopidogrel 75.0 mg and oral anticoagulation (warfarin) as a means to prevent thromboembolic events.
After 1 year of follow up, the angiographic condition of the patient remained stable.
Discussion-conclusion
A diagnosis of CAAs is very rare and occasional, often occurring as an incidental finding at coronary angiography (1%-4.9% of all coronary angiogram and 1.4% of autopsies) [16]; giant CAAs are even rarer.
Atherosclerosis is the leading cause of CAAs accounting for more than 50% of cases in adults, especially in those arteries with vulnerable plaques characterized by a higher inflammatory setting [17]; Kawasaki disease is the second most common cause of CAAs in adults, but it typically affects children. Other possible causes of CAAs are inflammatory arterial diseases (such as polyarteritis nodosa or Takayasu arteritis), connective tissue disorders, hereditary collagen defects (Marfan or Ehler-Danlos syndromes), percutaneous coronary intervention and, with a very low percentage, post surgical coronary reimplantation in Bentall surgery, even though this is not the most common complication of the procedure and when spotted they are mainly located at the level of the ostial anastomosis [18].
Aneurysmal dilation may also affect other vascular structures, such as renal arteries, therefore generating hypertension, or carotid arteries [19]. These extra cardiac aneurysms need to be treated using stents, respectively, due to the high risk of renal hypertension and cerebrovascular stroke related to an increased risk of thrombus embolization provoked by the higher blood turbulence at the level of the carotid bifurcation [20]. As regards CAAs, there is still no consensus on their management, the choice of which is strictly influenced by the patient characteristics [3].
To our knowledge, this is the first case reported in the medical literature describing a giant aneurysm of LCX involving the vessel's length distant from its origin that occurred in a patient who had undergone a Bentall procedure 10 years before, had a previously normal coronary angiogram and did not have a history of Kawasaki disease [21], inflammatory disease or connective tissue disorder, such as Marfan or Ehlers-Danlos syndromes [22,23]. Considering the location and morphology of the aneurysmal dilation diagnosed in our patient (Fig. 2), we assumed that its formation did not correlate with the previous Bentall procedure.
Until now the natural history and treatment of giant CAAs remain unclear; even though there are no specific guidelines on a standardized procedure [24,25], surgical repair is considered to be the right strategy when feasible.
However, most patients are asymptomatic, so conservative treatment with a regular follow-up to make sure that no complication occurs (for instance: rupture, progressive enlargement, mechanical interference or compression of the surrounding structures) may be taken into account.
A non–invasive technique, like pre interventional CCTA, gave us the chance to diagnose and follow the evolution of CAAs in a patient not eligible for surgery.
Ethics human rights
The authors declare that the work described has been carried out following the Declaration of Helsinki of the World Medical Association revised in 2013 for experiments involving humans.
Patient consent
The authors declare that this report does not contain any personal information that could lead to the identification of the patient. Informed consent was obtained from the patient.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
Availability of data and material
Not applicable.
Footnotes
Acknowledgments: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing Interests: The authors declare that they have no competing interest.
References
- 1.Syed M, Lesch M. Coronary artery aneurysm: a review. Prog Cardiovasc Dis. 1997;40(1):77–84. doi: 10.1016/s0033-0620(97)80024-2. [DOI] [PubMed] [Google Scholar]
- 2.Abou Sherif S, Ozden Tok O, Taskoylu O, Goktekin O, Kilic ID. Coronary Artery Aneurysms: A Review of the Epidemiology, Pathophysiology, Diagnosis, and Treatment. Front Cardiovasc Med. 2017;4:24. doi: 10.3389/fcvm.2017.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li D, Wu Q, Sun L, Song Y, Wang W, Pan S. Surgical treatment of giant coronary artery aneurysm. J Thorac Cardiovasc Surg. 2005;130(3):817–821. doi: 10.1016/j.jtcvs.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax. 1968;23(4):338–339. doi: 10.1136/thx.23.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meijboom LJ, Nollen GJ, Merchant N, Webb GD, Groenink M, David TE. Frequency of coronary ostial aneurysms after aortic root surgery in patients with the Marfan syndrome. Am J Cardiol. 2002;89(9):1135–1138. doi: 10.1016/s0002-9149(02)02290-7. [DOI] [PubMed] [Google Scholar]
- 6.Yoshimura K, Tanaka H, Wada T, Shuto T, Kawano M, Anai H. True aneurysm of the left main trunk in a marfan syndrome patient at remote period after bentall operation and total arch replacement: a case report. Ann Thorac Cardiovasc Surg. 2019 doi: 10.5761/atcs.cr.18-00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferroni P, Roselli M, Spila A, D’Alessandro R, Portarena I, Mariotti S. Serum sE-selectin levels and carcinoembryonic antigen mRNA-expressing cells in peripheral blood as prognostic factors in colorectal cancer patients. Cancer. 2010;116(12):2913–2921. doi: 10.1002/cncr.25094. [DOI] [PubMed] [Google Scholar]
- 8.Ferroni P, Palmirotta R, Spila A, Martini F, Formica V, Portarena I. Prognostic value of carcinoembryonic antigen and vascular endothelial growth factor tumor tissue content in colorectal cancer. Oncology. 2006;71(3–4):176–184. doi: 10.1159/000106072. [DOI] [PubMed] [Google Scholar]
- 9.Roselli M, Guadagni F, Buonomo O, Belardi A, Ferroni P, Diodati A. Tumor markers as targets for selective diagnostic and therapeutic procedures. Anticancer Res. 1996;16(4B):2187–2192. [PubMed] [Google Scholar]
- 10.Acconcia MC, Caretta Q, Monzo L, Tanzilli G, Sili Scavalli A, Sergi D. Effectiveness of the new generation transcatheter aortic valve in the real life studies. Review and meta-analysis. Eur Rev Med Pharmacol Sci. 2019;23(18):8018–8027. doi: 10.26355/eurrev_201909_19018. [DOI] [PubMed] [Google Scholar]
- 11.Chiocchi M, Forcina M, Morosetti D, Pugliese L, Cavallo AU, Citraro D. The role of computed tomography in the planning of transcatheter aortic valve implantation: a retrospective analysis in 200 procedures. J Cardiovasc Med (Hagerstown) 2018;19(10):571–578. doi: 10.2459/JCM.0000000000000695. [DOI] [PubMed] [Google Scholar]
- 12.Blanke P, Weir-McCall JR, Achenbach S, Delgado V, Hausleiter J, Jilaihawi H. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI) /transcatheter aortic valve replacement (TAVR): An expert consensus document of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2019;13(1):1–20. doi: 10.1016/j.jcct.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Chiocchi M, Ricci F, Pasqualetto M, D’Errico F, Benelli L, Pugliese L. Role of computed tomography in transcatheter aortic valve implantation and valve-in-valve implantation: complete review of preprocedural and postprocedural imaging. J Cardiovasc Med (Hagerstown) 2020;21(3):182–191. doi: 10.2459/JCM.0000000000000899. [DOI] [PubMed] [Google Scholar]
- 14.Francone M, Budde RPJ, Bremerich J, Dacher JN, Loewe C, Wolf F. CT and MR imaging prior to transcatheter aortic valve implantation: standardisation of scanning protocols, measurements and reporting-a consensus document by the European Society of Cardiovascular Radiology (ESCR) Eur Radiol. 2020;30(5):2627–2650. doi: 10.1007/s00330-019-06357-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiocchi M, Pugliese L, Forcina M, Cavallo AU, Presicce M, De Stasio V. Pre-transcatheter aortic valve implantation assessment in patients with renal failure: computed tomography and MRI acquisition protocols in our experience. J Cardiovasc Med (Hagerstown) 2019;20(4):267–269. doi: 10.2459/JCM.0000000000000765. [DOI] [PubMed] [Google Scholar]
- 16.Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21(1):28–40. doi: 10.1002/ccd.1810210110. [DOI] [PubMed] [Google Scholar]
- 17.Pugliese L, Spiritigliozzi L, Di Tosto F, Ricci F, Cavallo AU, Di Donna C. Association of plaque calcification pattern and attenuation with instability features and coronary stenosis and calcification grade. Atherosclerosis. 2020;311:150–157. doi: 10.1016/j.atherosclerosis.2020.06.021. [DOI] [PubMed] [Google Scholar]
- 18.Chiocchi M, Spiritigliozzi L, Di Tosto F, Benelli L, D’Errico F, Presicce M. Ascending aorta pseudoaneurysm simulating mediastinal lymphoma in computed tomography, a possible diagnostic error: a case report. J Med Case Rep. 2020;14(1):167. doi: 10.1186/s13256-020-02465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gandini R, Morosetti D, Chiocchi M, Chiaravalloti A, Citraro D, Loreni G. Long-term follow-up of endovascular treatment of renal artery aneurysms with covered stent deployment. J Cardiovasc Surg (Torino) 2016;57(5):625–633. [PubMed] [Google Scholar]
- 20.Chiocchi M, Morosetti D, Chiaravalloti A, Loreni G, Gandini R, Simonetti G. Intravascular ultrasound assisted carotid artery stenting: randomized controlled trial. Preliminary results on 60 patients. J Cardiovasc Med (Hagerstown) 2019;20(4):248–252. doi: 10.2459/JCM.0b013e32835898f1. [DOI] [PubMed] [Google Scholar]
- 21.Matsuoka R, Furuno K, Nanishi E, Onoyama S, Nagata H, Yamamura K. Delayed development of coronary artery aneurysm in patients with kawasaki disease who were clinically responsive to immunoglobulin. J Pediatr. 2020;227:224–230. doi: 10.1016/j.jpeds.2020.08.032. e3. [DOI] [PubMed] [Google Scholar]
- 22.Nichols L, Lagana S, Parwani A. Coronary artery aneurysm: a review and hypothesis regarding etiology. Arch Pathol Lab Med. 2008;132(5):823–828. doi: 10.5858/2008-132-823-CAAARA. [DOI] [PubMed] [Google Scholar]
- 23.Pahlavan PS, Niroomand F. Coronary artery aneurysm: a review. Clin Cardiol. 2006;29(10):439–443. doi: 10.1002/clc.4960291005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheikh AS, Hailan A, Kinnaird T, Choudhury A, Smith D. Coronary artery aneurysm: evaluation, prognosis, and proposed treatment strategies. Heart Views. 2019;20(3):101–108. doi: 10.4103/HEARTVIEWS.HEARTVIEWS_1_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pham V, Hemptinne Q, Grinda JM, Duboc D, Varenne O, Picard F. Giant coronary aneurysms, from diagnosis to treatment: A literature review. Arch Cardiovasc Dis. 2020;113(1):59–69. doi: 10.1016/j.acvd.2019.10.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.