Abstract
Objective
The COVID-19 pandemic has quickly transformed healthcare systems with expansion of telemedicine. The past year has highlighted risks to immunosuppressed cancer patients and shown the need for health equity among vulnerable groups. In this study, we describe the utilization of virtual visits by patients with gynecologic malignancies and assess their social vulnerability.
Methods
Virtual visit data of 270 gynecology oncology patients at a single institution from March 1, 2020 to August 31, 2020 was obtained by querying a cohort discovery tool. Through geocoding, the CDC Social Vulnerability Index (SVI) was utilized to assign social vulnerability indices to each patient and the results were analyzed for trends and statistical significance.
Results
African American patients were the most vulnerable with a median SVI of 0.71, Asian 0.60, Hispanic 0.41, and Caucasian 0.21. Eighty-seven percent of patients in this study were Caucasian, 8.9% African American, 3.3% Hispanic, and 1.1% Asian, which is comparable to the baseline institutional gynecologic cancer population. The mean census tract SVI variable when comparing patients to all census tracts in the United States was 0.31 (range 0.00 least vulnerable to 0.98 most vulnerable).
Conclusions
Virtual visits were utilized by patients of all ages and gynecologic cancer types. African Americans were the most socially vulnerable patients of the cohort. Telemedicine is a useful platform for cancer care across the social vulnerability spectrum during the pandemic and beyond. To ensure continued access, further research and outreach efforts are needed.
Keywords: Telemedicine, Virtual visit, COVID-19 pandemic, Social vulnerability index, Health disparities
1. Introduction
Prior to the COVID-19 pandemic, telemedicine in oncology was used primarily for large geographic areas needing access to care [1,2]. Implementation of telemedicine within gynecologic oncology specifically has varied; while some institutions have elected to perform initial consultations in-person followed by virtual visits, others have utilized virtual platforms for both initial consultations and follow-up encounters [3,4]. Several benefits of telemedicine have been noted for oncology patients including improved quality of life and a heightened sense of independence [5,6]. Additionally, several studies evaluating the efficacy of telemedicine in rural areas described convenience and cost-effectiveness as key patient-reported benefits [7,8].
The COVID-19 pandemic has rapidly transformed healthcare systems worldwide with a significant expansion in existing virtual health and telemedicine platforms and capabilities. In response to need for enhanced telehealth services, the Centers for Medicare and Medicaid Services eliminated geographic restrictions and enhanced reimbursement so providers could continue to provide care during the pandemic [9,10]. Telemedicine has been recommended by the Society of Gynecologic Oncology for use in gynecologic oncology when appropriate [11]. In a study investigating practice pattern changes in gynecology oncology early in the pandemic, 95.7% of survey respondents' institutions were encouraging telemedicine and 81.3% of respondents were cancelling outpatient in-person visits [12].
Oncology patients, especially those on active treatment, represent a subset of patients most at risk for severe COVID-19 infection [13]. Additionally, cancer patients require frequent medical care due to treatment plans, therapeutic toxicities, and necessary surveillance visits [14]. There is concern that with diagnostic appointments and screening exams postponed due to COVID-19, there will be delays in cancer diagnosis and care that will not be fully realized until years from now.
The COVID-19 pandemic has also brought health disparities to the forefront—both contraction of the coronavirus and more broadly health equity in general. There are many racial and ethnic disparities in cancer care. For more than 40 years, African Americans have had a higher cancer death rate than all other racial and ethnic groups in the United States [15]. These disparities exist in access to treatment and outcomes for patients with gynecologic malignancies [16]. In a study analyzing 29,777 patients with high grade endometrial cancer, African Americans had higher rates of stage IV disease, carcinosarcoma, clear cell carcinoma, papillary serous carcinoma, and lower rate of grade 3 endometrioid carcinoma compared to their white counterparts [17]. Similar disparities exist in enrollment in gynecologic oncology clinical trials. Discrepancies exist between the race and ethnicity of patients accrued to trial compared to the incidence of each malignancy in the general population. Ovarian cancer trials included an over representation of Caucasian patients (92.4% of accrual) as compared to 83.6% of the population, and under representation of African American patients (4.4% in trial) as compared to 11.5% in the population. Hispanic patients were under represented in ovarian cancer trials (4.4% vs 17.7% in population) [18].
Milwaukee is a city known for segregation. In 2020, Milwaukee was one of the top five most segregated cities in the United States based on the white/non-white dissimilarity index [19,20]. With a racial dissimilarity index of 60.8 in 2019, nearly 61% of the non-Hispanic white population in Milwaukee county would have to move to change census tracts in order to equalize the racial distribution between white and non-white population in the county [20]. Our institution cares for socially vulnerable patients including urban minority patients in addition to patients who travel from rural areas to the north, south, and west of Milwaukee. Social vulnerability is defined by the Centers for Disease Control and Prevention (CDC) as “the degree to which a community exhibits certain social conditions, including high poverty, low percentage of vehicle access, or crowded households, may affect that community's ability to prevent human suffering and financial loss in the event of disaster” [21]. Here we describe the utilization of virtual visits by patients with gynecologic malignancies during the first six months of the COVID-19 pandemic and assess the social vulnerability of these patients.
2. Methods
2.1. Database creation
Following Institutional Review Board (PRO00039103) approval, eligible participants were identified by querying a cohort discovery tool (I2B2: Informatics for integrating biology and the bedside) for patients who had participated in a virtual visit with a gynecology oncology provider from 3/1/2020 to 8/31/2020. Clinical information was then extracted for each identified participant using the Honest Broker tool. Demographic information such as race and ethnicity was self-reported from each patient's electronic medical record. Additional chart review was completed for clinical information not available through the initial database query. This included cancer clinical information and data pertaining to the reason for the virtual visit.
Patient information including addresses were obtained and deidentified prior to database incorporation. Geocodio (Dotsquare LLC, 2020, https://www.geocod.io/) was used to identify census tract and FIPS codes for each address based on the 2018 census data. Patients' census tracts were then linked with the CDC's social vulnerability index (SVI) data. The SVI is a value between 0 and 1, with values closer to 1 indicating increasing vulnerability [21]. Both data for the US and state of Wisconsin were obtained [22]. The sum of the series and theme ranking variable for each of four SVI themes (socioeconomic status, household composition and disability, minority status and language, and housing type and transportation) and the overall tract summary series sum and ranking were incorporated into the database. Each of these four SVI themes variable is determined based on factors of the American Community Survey 5-year data: Socioeconomic status: estimates of below poverty, unemployed, income, no high school diploma; Household composition and disability: aged 65 or older, aged 17 or younger, older than age 5 with a disability, single-parent households; Minority status and language: minority, speaks English ‘less than well’; Housing type and transportation: multi-unit structures, mobile homes, crowding, no vehicle, group quarters [21].
2.2. Database refinement
Honest broker identified 310 patients with an encounter coded as “mychart virtual visit” or “virtual check in (telephone).” Fourteen patients who cancelled or did not complete a virtual visit, 2 patients with colon cancer, 2 patients with gestational trophoblastic disease, 18 patients with benign pathology, 1 patient who was no longer residing within the larger geographic area of our population, and 3 patients whose disease was not completely evaluated and deemed inoperable were excluded from further analysis. In total, 40 patients were excluded, leaving 270 unique patients who completed 321 virtual visits.
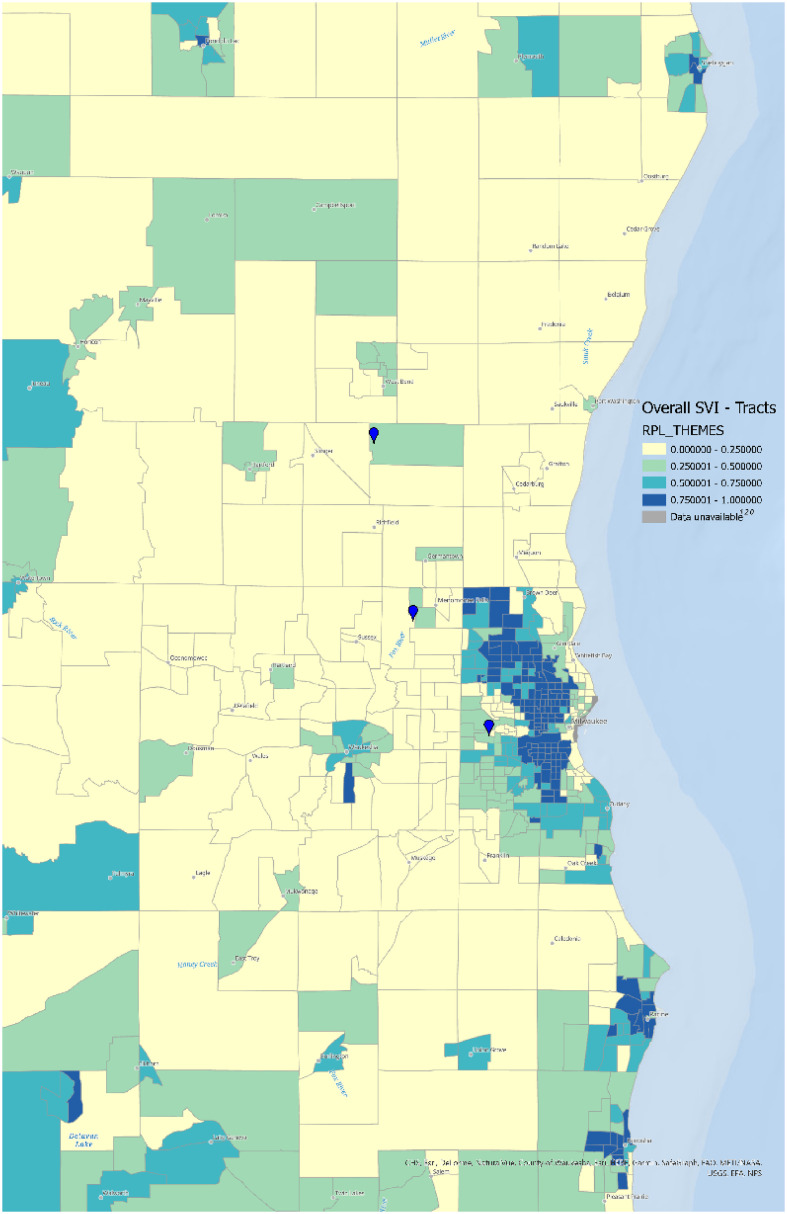
2.3. Map creation
ARCGIS pro (Esri Inc., 2020, https://www.esri.com/en-us/arcgis/about-arcgis/overview) was utilized to map the catchment area of the cancer center. The US SVI by census tract was plotted and each of the three cancer center locations was indicated.
2.4. Statistics
All statistical analyses were carried out using R (R Core Team, 2020, http://www.R-project.org/) and a 2-sided P value of less than 0.05 was considered to be statistically significant, unless otherwise noted. For continuous data such as age, mean, median, interquartile range (IQR) and standard deviation (SD) were utilized. For categorical data, both nominal and ordinal, such as race, results were summarized as percentages and compared by Chi-square or Fisher's exact test. Continuous variables between groups were compared using Mann-Whitney, Wilcoxon, or Kruskal-Wallis tests.
3. Results
3.1. Demographics
Our analysis included 270 patients who completed 321 virtual visits. Seventy two percent (230 patients) completed one virtual visit. Thirty-two patients had two visits, six patients had three visits, and one patient had each four and five virtual visits, respectively. Of the 270, 265 patients (98%) were Wisconsin residents, compared with four from Illinois and one from the upper peninsula of Michigan (Table 1 ).
Table 1.
Demographics of the 270 patients participating in virtual visits between 3/1/2020 and 8/31/2020.
| Characteristic | N = 270 |
|---|---|
| Age | Mean 64 standard deviation 12 |
| State of residence | |
| Wisconsin | 265 (98%) |
| Illinois | 4 (1.5%) |
| Michigan | 1 (0.4%) |
| Race/Ethnicity | |
| Asian | 3 (1.1%) |
| Black or African American | 24 (8.9%) |
| Hispanic | 9 (3.3%) |
| White or Caucasian | 234 (87%) |
| Marital Status | |
| Married | 166 (61%) |
| Divorced | 23 (8.5%) |
| Single | 43 (16%) |
| Widowed | 34 (13%) |
| Other | 4 (1.5%) |
| Employment Status | |
| Full Time | 65 (24%) |
| Part Time | 20 (7.4%) |
| Retired | 135 (50%) |
| Disabled | 16 (5.9%) |
| Other | 34 (13%) |
| Cancer Site | |
| Cervix | 11 (4.1%) |
| Ovary | 139 (51%) |
| Uterus | 115 (43%) |
| Vulva/Vaginal | 5 (1.9%) |
| Disease Stage | |
| I | 121 (45%) |
| II | 18 (6.7%) |
| III | 103 (38%) |
| IV | 28 (10%) |
The mean age in our population was 64 years. One hundred thirty-nine patients had ovarian cancer (51%), compared with 115 patients with uterine cancer (43%), 11 with cervical cancer (4.1%), and 5 with vulva/vaginal cancer (1.9%) (Table 1). Patients' cancer stages and histology are described in supplemental table 1.
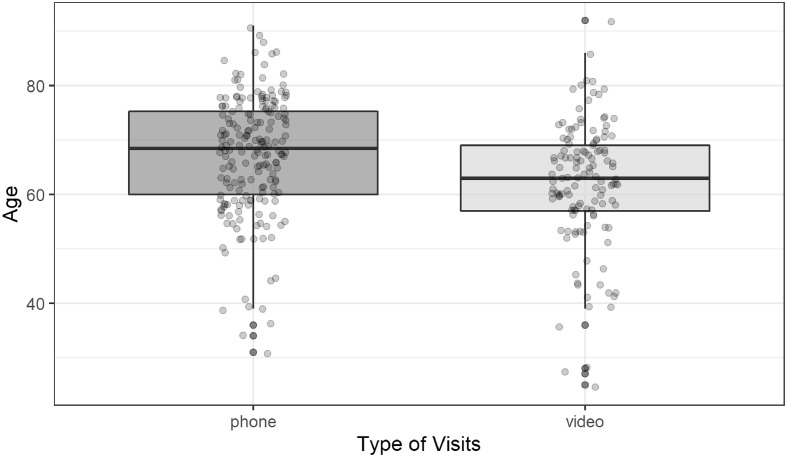
3.2. Visit type
Sixty percent (192 visits) of virtual visits were phone virtual visits, compared to 40% video visits (129 visits). Older patients were more likely to engage in phone virtual visits compared to video virtual visits (p < 0.001) (Fig. 1 ). The median age of patients partaking in phone virtual visits was 68 compared to 63 for video virtual visits. We also noted significant differences in visit type preferred by patients of different race/ethnicities (p = 0.011). Of 129 video virtual visits, 91% (117 visits) of them were completed by Caucasian patients, 6.2% (8 visits) by African American patients, 2.3% (3 visits) by Asian patients, and 0.8% (1 visit) by a patient who identified as Hispanic (Table 2 ). There was no significant difference in virtual visit type based on site of disease (p = 0.088) (Table 2).
Fig. 1.
Age and visit type box plot. Ages were significantly different between the two groups (p < 0.001). The median age for phone visits was 68 (IQR 60–75). The median age for video visits was 63 (IQR 57–69).
Table 2.
Characteristics with significant differences between phone and video virtual visits. Patients partaking in phone virtual visits were older than those participating in video visits (p < 0.001). Caucasian patients made up 91% of the video visits. More African Americans participated in phone visits than video visits. Patients with cervix cancer tended to participate in phone visits, and there was only 1 cervix cancer video visit recorded. Surveillance visits made up the greatest proportion of video visits (55%) compared to treatment visits, which made up 49% of the phone visits.
| Characteristic | Overall N=3211 | Phone N=1921 | Video N=1291 | p-value2 |
|---|---|---|---|---|
| Age | 66 (59–73) | 68 (60–75) | 63 (57–69) | <0.001 |
| Race/Ethnicity | 0.011 | |||
| Asian | 3 (0.9%) | 0 | 3 (2.3%) | |
| Black or African American | 29 (9%) | 21 (11%) | 8 (6.2%) | |
| Hispanic | 10 (3.1%) | 9 (4.7%) | 1 (0.8%) | |
| White or Caucasian | 279 (87%) | 162 (84%) | 117 (91%) | |
| Cancer Site | 0.088 | |||
| Cervix | 11 (3.4%) | 10 (5.2%) | 1 (0.8%) | |
| Ovary | 177 (55%) | 105 (55%) | 72 (56%) | |
| Uterus | 127 (40%) | 75 (39%) | 52 (40%) | |
| Vulva/Vaginal | 6 (1.9%) | 2 (1.0%) | 4 (3.1%) | |
| Reason for visit | 0.024 | |||
| Postop | 14 (4.4%) | 7 (3.6%) | 7 (5.4%) | |
| Surveillance | 148 (46%) | 77 (40%) | 71 (55%) | |
| Treatment | 141 (44%) | 94 (49%) | 47 (36%) | |
| Treatment Discussion | 18 (5.6%) | 14 (7.3%) | 4 (3.1%) |
Median (IQR); n(%).
Wilcoxon rank sum test; Fisher's exact test; Pearson's Chi-squared test.
The majority of virtual visits were for surveillance (46%, 148 visits) or pre-treatment (44%, 141 visits), as compared with treatment discussion (5.6%, 18 visits), or postop visit (4.4%, 14 visits). There was a significant difference in visit type based on reason for the visit (p = 0.024) with more video virtual visits being performed for surveillance (55% of video visits, 71 visits); and more phone virtual visits for pre-treatment (49% of phone virtual visits, 94 visits) (Table 2).
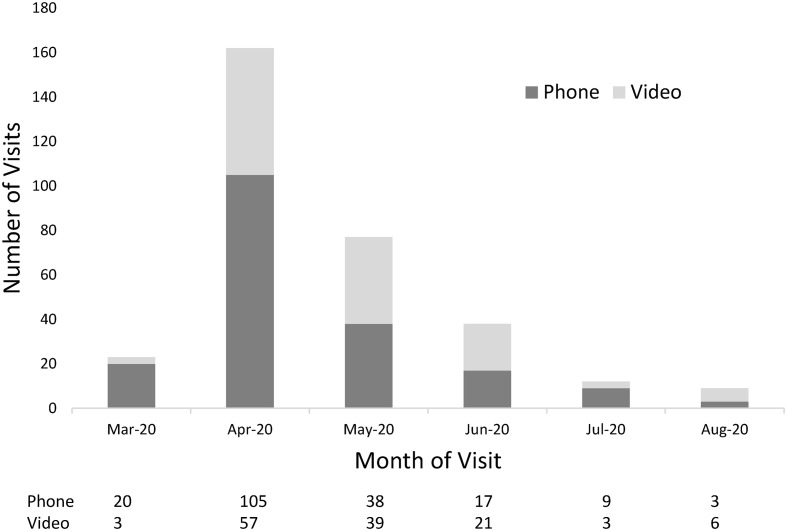
Temporal trends in visit type were noted with half (162 visits) of the total number of virtual visits occurring during the month of April. In March and April 2020, phone virtual visits were the preferred modality as compared to video virtual visits (20 vs 3 visits in March, 105 vs 57 visits in April). However, in the months of May and June video virtual visits increased (39 vs 38 visits in May, 21 vs 17 visits in June) (Fig. 2 ). This likely corresponds to increased familiarity with telemedicine by both providers and patients as the pandemic progressed.
Fig. 2.
Temporal trends in virtual visits and type of visit. Half of the total visits were completed in the month of April 2020, which corresponds to the state-wide ‘stay at home’ mandate. In the months of May and June 2020, the number of video visits was greater than the number of phone visits.
3.3. Geospatial mapping
When the US SVI data by census tract is placed on a map of the catchment area of the institution, the most vulnerable patients live in the urban census tracts of Milwaukee (Fig. 3 ). Stark differences in vulnerability can be visualized in census tracts where the most vulnerable quartile tracts share a geographic border with the least vulnerable quartile. Patients in the most vulnerable census tracts tend to be geographically closer to the main academic center. Those patients in the more rural areas were nearly all residing in census tracts with SVI values less than 0.5, indicating social vulnerability less than the median for all US census tracts.
Fig. 3.
Geographic representation of the catchment area of the academic cancer center with the US SVI by census tract mapped. The three cancer center locations are identified with the main academic center most closely geographically to the urban areas of Milwaukee. Patients in urban areas tended to be most vulnerable with the most vulnerable quartile (SVI 0.75–1.0) identified in dark blue. Teal represents SVI 0.5–0.75, light green SVI 0.25–0.5, and yellow 0–0.25. Stark differences in vulnerability can be visualized in census tracts where the most vulnerable quartile tracts (dark blue) share a geographic border with the least vulnerable quartile (yellow). Patients residing in more rural census tracts had median US SVI indices less than the median (yellow and light green). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.4. Visit type and SVI
Social vulnerability did not appear to impact the utilization of phone versus video virtual visits. The median United States SVI value for patients participating in phone virtual visits was 0.23 (IQR 0.12, 0.40) compared to 0.25 for those participating in video virtual visits (IQR 0.09, 0.52) (p = 0.5). The SVI themes of socioeconomic status and transportation similarly did not reveal significant differences between visit type (p = 0.3 for socioeconomic theme; p = 0.6 for transportation theme).
3.5. SVI and disease site, stage, race
Compared to US vulnerability ranks, our 270 patients had median SVI of 0.23 (IQR 0.10–0.48). When examining geospatial trends in the SVI, patients who were the most vulnerable resided in urban areas, while less vulnerable patients lived in more rural areas (Fig. 3). As shown on the map which displays the main catchment area of the institution, the most vulnerable census tracts were mainly inner city in relation to the location of the Cancer Center locations.
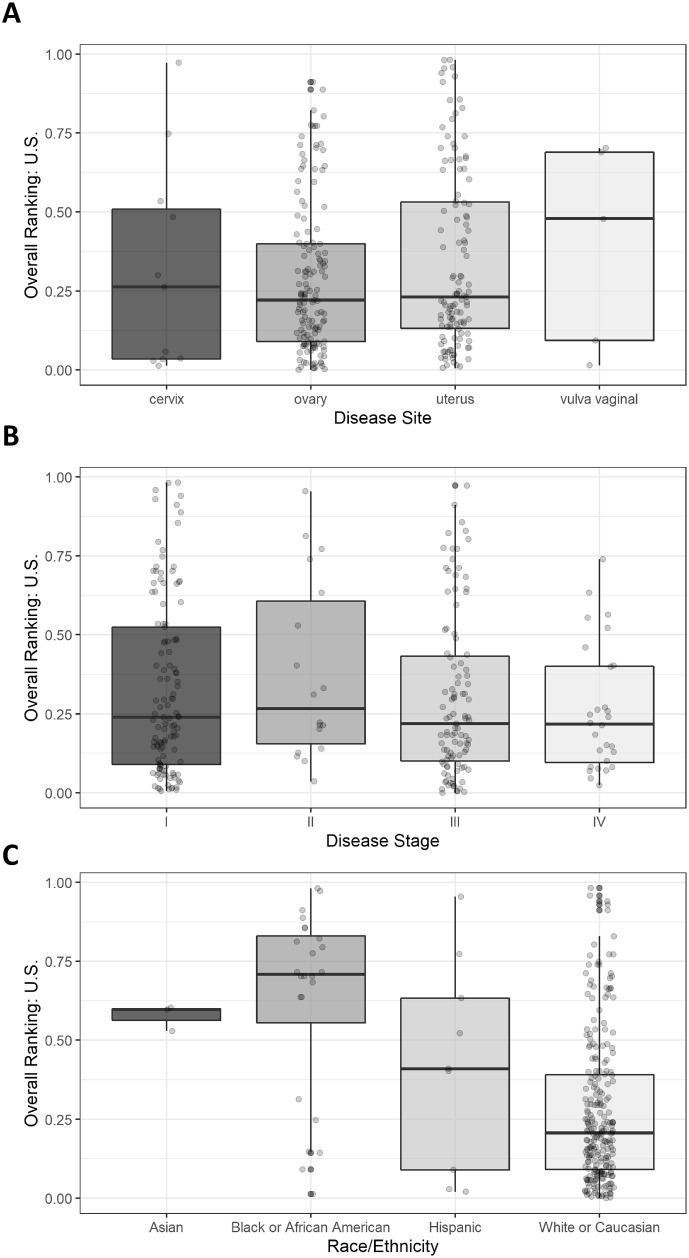
The median US SVI did not differ by sites of disease among those patients participating in virtual visits (p = 0.5) (Fig. 4A). Patients with vulvar/vaginal cancer had a median US SVI value of 0.48 (IQR 0.09, 0.69) compared to uterine 0.23 (IQR 0.13, 0.53), ovary 0.22 (IQR 0.09, 0.4), and cervix 0.26 (IQR 0.03, 0.51). Similarly the median US SVI did not differ by disease stage (p = 0.5)(Fig. 4B). Patients with stage I disease had a median US SVI of 0.24 (IQR 0.09, 0.52), compared with 0.27 (IQR 0.15, 0.61) for stage II disease, 0.22 (IQR 0.1, 0.43) for stage III disease, and 0.22 (IQR 0.1, 0.4) for stage IV, respectively.
Fig. 4.
Boxplots of social vulnerability index (SVI) overall for the United States by A: gynecologic disease site. B: Disease stage. C. Race/Ethnicity. A: There was no significant difference in SVI by disease site. Patients with vulvar/vaginal cancer had a median US SVI value of 0.48 (IQR 0.09–0.69), uterine 0.23 (IQR 0.13–0.53), ovary 0.22 (IQR 0.09–0.4), and cervix 0.26 (IQR 0.03–0.51), respectively. B: The US SVI did not differ by disease stage (p = 0.5). Stage I disease had a median US SVI of 0.24 (IQR 0.09, 0.52), stage II 0.27 (IQR 0.15, 0.61), stage III 0.22 (IQR 0.1, 0.43), and stage IV 0.22 (IQR 0.1, 0.4) respectively. C: SVI was significantly different across race groups (p < 0.001). African Americans were the most vulnerable group, median SVI 0.71 (IQR 0.56–0.83), followed Asian median SVI 0.60 (IQR 0.56–0.6), Hispanic median SVI 0.41 (IQR 0.09–0.63), and Caucasian median SVI 0.21 (IQR 0.09–0.39), respectively.
SVI was significantly different across racial groups (p < 0.001) (Fig. 4C). African Americans were the most vulnerable group with median SVI 0.71 (IQR 0.56–0.83). The next most vulnerable group was patients who identified as Asian with median SVI 0.60 (IQR 0.56–0.6) followed by patients identifying as Hispanic with median SVI 0.41 (IQR 0.09–0.63). Caucasian patients were the least vulnerable with median SVI 0.21 (IQR 0.09–0.39). When we investigated the socioeconomic and transportation themes of the SVI by race, there was a significant difference between racial groups in the socioeconomic theme of the SVI (p < 0.001), and the transportation theme did not exhibit a significant difference among races, but trended toward significance (p = 0.051) (Supplemental Fig. 1). Patients who were African American or Asian were the most vulnerable as compared to Hispanic and Caucasian patients: socioeconomic median for African American 0.74 (IQR 0.54–0.87); transportation median for African American 0.49, (IQR 0.37–0.72); socioeconomic median for Asian 0.56 (IQR 0.46–0.6); transportation median for Asian 0.67 (IQR 0.61–0.71); socioeconomic median for Hispanic 0.42 (IQR 0.22–0.51); transportation median for Hispanic 0.28 (IQR 0.14–0.70); socioeconomic median for Caucasian 0.18 (IQR 0.07–0.38); transportation median for Caucasian 0.34 (IQR 0.17–0.62).
4. Discussion
This study investigates utilization of virtual visits in the first six months of the COVID-19 pandemic among gynecologic oncology patients at a single institution. The greatest number of virtual visits occurred in April 2020, corresponding to the state-wide lockdown when in-person visits were greatly reduced. Telephone and virtual visits during this time were completed by providers who were working from home. As the months progressed, the number of video visits increased, reflecting adaptation to technology and video aspects of telehealth by both providers and patients. Subsequently, in both May and June 2020, the number of video visits was greater than the telephone virtual visits in this population (Fig. 2). In these months, however, a return to clinic and decrease in COVID-19 cases prompted more in-person visits and fewer virtual visits overall.
Cancer surveillance visits represented 55% of the video visits in our study. The use of telemedicine for cancer surveillance has been described previously [4,23] and may involve consultation with a gynecologic oncology provider to review symptoms and a physical exam conducted by an OB/GYN or primary care provider. During the COVID-19 pandemic, our surveillance patients participated in video visits to assess symptoms, and for providers to visually assess functional status. Patients were then scheduled for an in-person exam with a provider in the subsequent 3–4 months or earlier if an issue was reported.
When comparing social vulnerability index by visit type, there was no significant difference between the visit types, indicating that a patient's vulnerability did not appear to hinder their ability to utilize or choose between telephone or video platforms. There was a difference based on age and race with a greater median age of patients participating in phone virtual visits compared to video virtual visits. Patients who were African American or Hispanic made up greater proportions of the telephone visits, while patients who were Caucasian made up a greater percentage of the video visits. These findings may indicate that perhaps the reason patients participate in either a video or telephone virtual visit may be more related to their age, race, cultural perceptions of a doctor visit, or technology usage preferences and abilities than their social vulnerability, socioeconomic means, or access to technology. A similar trend was observed in a study of virtual care appointments at a cancer center in Canada. This study found that patients identifying as minority, foreign born, through the ethnocultural composition index rated virtual care visits favorably but with a lower likelihood of requesting virtual care for future appointments [24].
Using the SVI we were able to investigate the interaction between social vulnerability and race/ethnicity. Our findings indicate that there was a significant difference in vulnerability based on race. African Americans were the most vulnerable group, followed by patients who identified as Asian, Hispanic, and Caucasian, respectively. It is important to note that patients belonging to the three minority groups in this study (African American, Asian, and Hispanic) had IQR values which crossed 0.5 or the median vulnerability index threshold, where Caucasian patients had a median of 0.21 and IQR or 0.09–0.39. This study includes 87% Caucasian patients. While this demographic is not reflective of the racial/ethnic makeup of the city of Milwaukee or the southeastern Wisconsin region, this study is more reflective of the racial/ethnic demographic of our gynecology oncology clinic population. Based on internal data averaged across three clinical sites, our clinic comprises approximately 88.2% patients who are white, 7.5% black, and 4.3% other. Given the similar demographic between the virtual visit population and the in-person gynecologic oncology clinic population, this study demonstrates the inclusive nature of virtual visits across the vulnerability spectrum. Ensuring minority access to telehealth will continue to be a goal of our clinic, particularly as virtual visits are likely to be utilized in the post-COVID era.
Previous studies have identified increased risk of complications or death among minority patients with high social vulnerability based on the SVI who are undergoing surgical procedures such as colon resection or coronary artery bypass graft [25]. Cancer patients who were of a minority race had reduced odds of hospice utilization and early hospice initiation as their social vulnerability value increased [26]. This trend did not apply for cancer patients who were white [26]. The SVI offers a valuable metric for identifying patients who may be at risk for social determinants of health to profoundly affect their cancer care and outcomes. Using the SVI, providers can identify vulnerable patients early in their cancer journey, at the time of diagnosis or at the time of initiation of adjuvant therapy, and initiate referrals to social workers or financial counselors who can assist by providing information about community resources, insurance applications, and cancer center resources. Transportation is a factor that impacts many vulnerable patients, even those who may reside in close proximity to a cancer center location. Linking patients with community organizations who provide rides to treatment or hospital-provided public transportation vouchers can help patients attend in-person visits and treatments. As demonstrated in this study, virtual visits can be a viable and accessible option for care of socially vulnerable gynecologic cancer patients. Providing the option of both video and telephone visits when a patient establishes care allows patients more flexibility and fewer interruptions as they navigate their cancer journey.
To our knowledge this study is the first to discuss telemedicine and virtual visits in relation to social vulnerability. This provides a unique perspective with which to characterize aspects of telemedicine utilization and cancer care. This study was conducted in an academic medical center with a large catchment area serving patients of both urban and rural backgrounds. We show the usability of virtual visits for gynecologic cancer patients of all ages, histologies, stages, and reasons for visit. Virtual visits are an accessible option for all patients regardless of social vulnerability.
The SVI tracked 15 specific social factors including transportation, unemployment, and disability, and while we were able to link this variable to the precise geographic entity of a patient's census tract, this variable cannot account for each detail of an individual patient's experience of the social determinants of health.
Given the six-month study period and recent proximity to study period, this study did not include data on oncologic outcomes of patients. However, the literature suggests that telemedicine may not compromise disease-specific outcomes [27]. Additionally, we did not elicit patient satisfaction nor survey patients about their experience with virtual visits. However, the preference to participate in virtual visits despite an in-person clinic option highlights acceptance of telemedicine by our patient population. Patient satisfaction with virtual visits in gynecologic cancer clinics is high [28,29]. Greater than 80% of gynecologic cancer patients would use telemedicine again [29].
Though there are many benefits of virtual visits, some concerns still remain. In one systematic review of telemedicine implementation in oncology, between 41 and 75% of patients noted anxiety about the absence of physical examinations during virtual visits [30]. Other barriers to implementing telemedicine include the cooccurrence of poor internet connection and the rural areas that are generally located farther from cancer centers [31]. Virtual visits undoubtedly assisted patient adherence to cancer surveillance visits during the pandemic and can continue to allow for versatility beyond the pandemic. For situations where in-person visits may involve barriers related to transportation, work, or childcare among others, virtual visits may offer a solution.
In summary, our study shows virtual visits allow equitable access to gynecologic oncology providers across all demographics. Virtual visits can be a useful tool in cancer care for socially vulnerable groups during the pandemic and beyond.
CRediT authorship contribution statement
Lindsey A. McAlarnen: Conceptualization, Data curation, Methodology, Writing - original draft, Writing - review & editing. Shirng-Wern Tsaih: Data curation, Formal analysis, Methodology, Software, Writing - review & editing. Rana Aliani: Data curation, Methodology, Writing - review & editing. Natasha M. Simske: Data curation, Methodology, Writing - review & editing. Elizabeth E. Hopp: Conceptualization, Data curation, Methodology, Supervision, Writing - review & editing.
Funding
This project was funded in part by the Advancing a Healthier Wisconsin endowment at the Medical College of Wisconsin. This project was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant number 5UL1TR001436–02. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ygyno.2021.04.037.
Appendix A. Supplementary data
Supplementary material: Supplemental Table 1: Stage and histology data for the 270 patients who participated in virtual visits between 3/1/2020 and 8/31/2020.
Supplemental Fig. 1: Socioeconomic (A) and transportation (B) SVI indices by race. There was a significant difference between racial groups in the socioeconomic theme of the SVI (p < 0.001), and the transportation theme trended toward significance (p = 0.051). A: African Americans were the most vulnerable based on the socioeconomic theme of the SVI: median for African American 0.74 (IQR 0.54–0.87), Asian 0.56 (IQR 0.46–0.6), Hispanic 0.42 (IQR 0.22–0.51), and Caucasian 0.18 (IQR 0.07–0.38), respectively. B Patients identifying as Asian were the most vulnerable based on the transportation theme of the SVI: transportation median for Asian 0.67 (IQR 0.61–0.71), African American 0.49, (IQR 0.37–0.72), Hispanic 0.28 (IQR 0.14–0.70), and Caucasian 0.34 (IQR 0.17–0.62), respectively.
References
- 1.Palkhivala A. Canada develops models of teleoncology. J. Natl. Cancer Inst. 2011;103:1566–1568. doi: 10.1093/jnci/djr449. [DOI] [PubMed] [Google Scholar]
- 2.Sabesan S., Larkins S., Evans R., Varma S., Andrews A., Beuttner P., Brennan S., Young M. Telemedicine for rural cancer care in North Queensland: bringing cancer care home. Aust J Rural Health. 2012;20:259–264. doi: 10.1111/j.1440-1584.2012.01299.x. [DOI] [PubMed] [Google Scholar]
- 3.Sabesan S. Medical models of teleoncology: current status and future directions. Asia Pac J Clin Oncol. 2014;10:200–204. doi: 10.1111/ajco.12225. [DOI] [PubMed] [Google Scholar]
- 4.Shalowitz D.I., Smith A.G., Bell M.C., Gibb R.K. Teleoncology for gynecologic cancers. Gynecol. Oncol. 2015;139:172–177. doi: 10.1016/j.ygyno.2015.06.042. [DOI] [PubMed] [Google Scholar]
- 5.Chen Y.-Y., Guan B.-S., Li Z.-K., Li X.-Y. Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: a meta-analysis. J. Telemed. Telecare. 2018;24:157–167. doi: 10.1177/1357633X16686777. [DOI] [PubMed] [Google Scholar]
- 6.Cox A., Lucas G., Marcu A., Piano M., Grosvenor W., Mold F., Maguire R., Ream E. Cancer Survivors’ experience with telehealth: a systematic review and thematic synthesis. J. Med. Internet Res. 2017;19 doi: 10.2196/jmir.6575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scurrey S., Garland S.N., Thoms J., Laing K. Evaluating the experience of rural individuals with prostate and breast cancer participating in research via telehealth. Rural Remote Health. 2019;19:5269. doi: 10.22605/RRH5269. [DOI] [PubMed] [Google Scholar]
- 8.Sharma J.J., Gross G., Sharma P. Extending oncology clinical services to rural areas of Texas via Teleoncology. J Oncol Pract. 2012;8:68. doi: 10.1200/JOP.2011.000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers, (2021) 26.
- 10.Medicare Telemedicine Health Care Provider Fact SheetHEET CMS. 2021. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (accessed March 7, 2021)
- 11.Pothuri B., Alvarez Secord A., Armstrong D.K., Chan J., Fader A.N., Huh W., Kesterson J., Liu J.F., Moore K., Westin S.N., Naumann R.W. Anti-cancer therapy and clinical trial considerations for gynecologic oncology patients during the COVID-19 pandemic crisis. Gynecol. Oncol. 2020;158:16–24. doi: 10.1016/j.ygyno.2020.04.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakayama J., El-Nashar S.A., Waggoner S., Traughber B., Kesterson J. Adjusting to the new reality: evaluation of early practice pattern adaptations to the COVID-19 pandemic. Gynecol. Oncol. 2020;158:256–261. doi: 10.1016/j.ygyno.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang H., Wang L., Chen Y., Wu Q., Chen G., Shen X., Wang Q., Yan Y., Yu Y., Zhong Y., Wang X., Chua M.L.K., Xie C. Outcomes of novel coronavirus disease 2019 (COVID-19) infection in 107 patients with cancer from Wuhan, China. Cancer. 2020;126:4023–4031. doi: 10.1002/cncr.33042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salani R., Khanna N., Frimer M., Bristow R.E., Chen L.-M. An update on post-treatment surveillance and diagnosis of recurrence in women with gynecologic malignancies: Society of Gynecologic Oncology (SGO) recommendations. Gynecol. Oncol. 2017;146:3–10. doi: 10.1016/j.ygyno.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 15.AACR Cancer Disparities Progress Report . Vol. 2020. 2020. American Association for Cancer Research, Philadelphia.http://www.cancerdisparitiesprogressreport.org [Google Scholar]
- 16.Temkin S.M., Rimel B.J., Bruegl A.S., Gunderson C.C., Beavis A.L., Doll K.M. A contemporary framework of health equity applied to gynecologic cancer care: a Society of Gynecologic Oncology evidenced-based review. Gynecol. Oncol. 2018;149:70–77. doi: 10.1016/j.ygyno.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Rauh-Hain J.A., Buskwofie A., Clemmer J., Boruta D.M., Schorge J.O., del Carmen M.G. Racial Disparities in treatment of high-grade endometrial Cancer in the Medicare population. Obstet. Gynecol. 2015;125:843–851. doi: 10.1097/AOG.0000000000000605. [DOI] [PubMed] [Google Scholar]
- 18.Mishkin G., Minasian L.M., Kohn E.C., Noone A.-M., Temkin S.M. The generalizability of NCI-sponsored clinical trials accrual among women with gynecologic malignancies. Gynecol. Oncol. 2016;143:611–616. doi: 10.1016/j.ygyno.2016.09.026. [DOI] [PubMed] [Google Scholar]
- 19.City Observatory . 2020. America’s least (and most) segregated cities., City Observatory. [Google Scholar]
- 20.U.S. Census Bureau . FRED, Federal Reserve Bank of St. Louis; 2009. White to Non-White Racial Dissimilarity (5-Year Estimate) Index for Milwaukee County, WI.https://fred.stlouisfed.org/series/RACEDISPARITY055079 (accessed March 3, 2021) [Google Scholar]
- 21.CDC SVI Documentation 2018 . ATSDR; 2020. Place and Health.https://www.atsdr.cdc.gov/placeandhealth/svi/documentation/SVI_documentation_2018.html (accessed March 3, 2021) [Google Scholar]
- 22.CDC SVI Data and Documentation Download . ATSDR; 2020. Place and Health.https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html (accessed March 3, 2021) [Google Scholar]
- 23.Shalowitz D.I., Moore C.J. Telemedicine and gynecologic Cancer care. Obstet. Gynecol. Clin. N. Am. 2020;47:271–285. doi: 10.1016/j.ogc.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 24.Berlin A., Lovas M., Truong T., Melwani S., Liu J., Liu Z.A., Badzynski A., Carpenter M.B., Virtanen C., Morley L., Bhattacharyya O., Escaf M., Moody L., Goldfarb A., Brzozowski L., Cafazzo J., Chua M.L.K., Stewart A.K., Krzyzanowska M.K. Implementation and outcomes of virtual care across a tertiary cancer center during COVID-19. JAMA Oncol. 2021 doi: 10.1001/jamaoncol.2020.6982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diaz A., Hyer J.M., Barmash E., Azap R., Paredes A.Z., Pawlik T.M. County-level social vulnerability is associated with worse surgical outcomes especially among minority patients. Ann. Surg. 2020 doi: 10.1097/SLA.0000000000004691. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 26.Abbas A., Madison Hyer J., Pawlik T.M. Race/ethnicity and county-level social vulnerability impact hospice utilization among patients undergoing cancer surgery. Ann. Surg. Oncol. 2020 doi: 10.1245/s10434-020-09227-6. [DOI] [PubMed] [Google Scholar]
- 27.Flodgren G., Rachas A., Farmer A.J., Inzitari M., Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015 doi: 10.1002/14651858.CD002098.pub2. CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zimmerman B.S., Seidman D., Berger N., Cascetta K.P., Nezolosky M., Trlica K., Ryncarz A., Keeton C., Moshier E., Tiersten A. Patient perception of telehealth Services for Breast and Gynecologic Oncology Care during the COVID-19 pandemic: a single center survey-based study. J. Breast Cancer. 2020;23:542–552. doi: 10.4048/jbc.2020.23.e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mojdehbakhsh R.P., Rose S., Peterson M., Rice L., Spencer R. A quality improvement pathway to rapidly increase telemedicine services in a gynecologic oncology clinic during the COVID-19 pandemic with patient satisfaction scores and environmental impact. Gynecol Oncol Rep. 2021;36:100708. doi: 10.1016/j.gore.2021.100708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kitamura C., Zurawel-Balaura L., Wong R.K.S. How effective is video consultation in clinical oncology? A systematic review. Curr. Oncol. 2010;17:17–27. doi: 10.3747/co.v17i3.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Satcher R.L., Bogler O., Hyle L., Lee A., Simmons A., Williams R., Hawk E., Matin S., Brewster A.M. Telemedicine and telesurgery in cancer care: inaugural conference at MD Anderson Cancer Center. J. Surg. Oncol. 2014;110:353–359. doi: 10.1002/jso.23652. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material: Supplemental Table 1: Stage and histology data for the 270 patients who participated in virtual visits between 3/1/2020 and 8/31/2020.
Supplemental Fig. 1: Socioeconomic (A) and transportation (B) SVI indices by race. There was a significant difference between racial groups in the socioeconomic theme of the SVI (p < 0.001), and the transportation theme trended toward significance (p = 0.051). A: African Americans were the most vulnerable based on the socioeconomic theme of the SVI: median for African American 0.74 (IQR 0.54–0.87), Asian 0.56 (IQR 0.46–0.6), Hispanic 0.42 (IQR 0.22–0.51), and Caucasian 0.18 (IQR 0.07–0.38), respectively. B Patients identifying as Asian were the most vulnerable based on the transportation theme of the SVI: transportation median for Asian 0.67 (IQR 0.61–0.71), African American 0.49, (IQR 0.37–0.72), Hispanic 0.28 (IQR 0.14–0.70), and Caucasian 0.34 (IQR 0.17–0.62), respectively.