Abstract
Background
Nursing process (NP) is a standard method of ensuring individualized holistic care through systematic assessment, diagnosis, planning, intervention and evaluation of patients. Its standard implementation is mandatory to meet the health target of “ensuring universal quality health-care services” in the sustainable development goals (SDG) launched by World Health Organization (WHO) in 2015. Being a member state of WHO, Ethiopia endorsed the SDG agenda. Therefore, determining the recent pooled estimate and associated factors of NP implementation during patient care would be of greatest importance to improve the quality of nursing care in the country.
Methods
Primary studies were systematically searched from PubMed, Scopus, Cochrane Library, Google Scholar, PsycINFO and CINAHL data bases using different search operators. Each selected primary study was critically appraised using the Joanna Briggs Institute (JBI) appraisal tool for prevalence studies. I2 and Q statistics were used to investigate heterogeneity. Given the substantial heterogeneity between the studies, random effects meta-analysis model was used to estimate the pooled magnitude of NP implementation. Subgroup analyses were performed for evidence of heterogeneity. Egger's test was considered to declare publication bias objectively. The PRISMA guideline was followed to report the results.
Results
A total of 17 primary studies with a sample of 2,819 nurses were included in this meta-analysis. The pooled estimate of NP implementation in Ethiopia was 50.22% (95% CI: 43.39%, 57.06%) with severe statistical heterogeneity (I2 = 93.0%, P < 0.001) between the studies. From regional subgroup analysis, NP was least implemented in Tigray region 35.92% (95% CI: 30.86%–40.99%, I2 < 0.001%). Egger's test showed no statistical significance for the presence of publication bias (P = 0.23). Nurses' good knowledge of NP [(Adjusted Odds Ratio (AOR) = 13.16: 9.17–17.15], nurses' Bachelor of Science (BSC) and above level of education (AOR = 4.16; 2.32–5.99), working in a stressful environment (AOR = 0.10; -0.02–0.22), training access (AOR = 3.30; 1.79–4.82) and accessibility of facility required for NP (AOR = 6.05; 3.56–8.53) were significantly associated with NP implementation at 95 % CI.
Conclusions
It was found that only half of the nurses in Ethiopia implemented NP during patient care. Fortunately, its associated factors were modifiable. Therefore, the existing national efforts of increasing nurses’ knowledge of NP and their level of education, availing facilities required for NP implementation, training access and ensuring non stressful working environment should be reinforced to meet the quality nursing care demand in Ethiopia.
Prospero ID
CRD42019138159.
Keywords: Nursing process, Ethiopia, Systematic review, Patient care
Nursing process; Ethiopia; Systematic review; Patient care.
1. Introduction
As compared to other health care professionals, nurses spend more time with patients and they play a pivotal role of the health care system in Ethiopia [1,2]. Moreover, about 80% of the health care services at hospitals of the country are provided by nurses [3]. Therefore, the Ethiopian Federal Ministry of Health is striving to provide quality health care service by improving quality of nursing care [4, 5, 6]. The quality of nursing care is measured by nursing process (NP), a systematic method of assessing, diagnosing, planning, intervening and evaluating individualized holistic care of every patient [7]. NP is a systematic approach of problem solving to identify, prevent and treat actual or potential health problems and promote wellness [8]. It is also a systematic, patient-oriented and purposive approach which provides a framework for nursing performance [9,10]. Yet, its implementation as a standard of care is poor and constrained by a variety of factors in Ethiopia [10].
Nursing process is a practical tool of guiding nurses' critical thinking to make their own independent decisions for addressing clients’ needs to improve healing [11]. Nowadays, Ethiopian healthcare institutions are majorly concerned about the standard level of NP implementation [4,7] to encourage the utilization of evidence based nursing practice for quality of care [5,6]. Moreover, standard implementation of NP is helpful to establish good patient-nurse relationship and compliance with health care regimens thereby resulting in better patient outcomes [9, 10, 11, 12, 13, 14].
In Ethiopia, nursing process is integrated within different theoretical and practical nursing courses and taught as part of the nursing curriculum [15]. However, learning the nursing process at schools doesn't necessarily qualify graduates to implement NP at their work settings [10] because its implementation is affected by diverse individual and management factors. Moreover, though there is a strong gap between theory and practice in nursing field, nursing students pay more attention to the theoretical aspects than the art of nursing [10, 11, 12, 13, 14]. Therefore, nursing managers and authorities of nursing process should make efforts to moderate these factors and provide facilities for improving the implementation of nursing process [5].
As of different individual studies in Ethiopia, the implementation of NP in the country could be determined by several professional, institutional and patient related factors [17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33]. For instance, majority of the accessed individual studies reported that nurses' knowledge of NP [17,18,20, 21, 22, 23, 24,26,30,31], surrounding physical working environment [17,18,23,25,26], facility accessibility [17,19,24, 25, 26], training access [22, 23, 24,30,33], level of education [19,25,33] and early patient discharge [21,23] are the major determinant factors of NP implementation. Besides, the significance of lack of patient's cooperation [22], nurses' skill of NP [30], patient to nurse ratio [24], nurse seeing patients' outcome [24], ward type [18], timely reporting [27], supervision [27,28], presence of uncomplicated cases [21], patient economy [22], administrative support [31], nurses' work experience [31] were reported. Therefore, working on these factors has of greatest relevance to improve the quality of nursing care [13–16].
In recent years, many individual studies have been conducted worldwide to determine the level of nursing process implementation. For instance, studies conducted in Kenya [34] and Brazil [35] showed low level of NP implementation in the respective countries. Additionally, the overall level of nursing process implementation is 57.1% in Nigeria [14], 81.77% in Brazil [35], 98% in Sweden [36] and 50.8% in Iran [10].
According to a prior systematic review and meta-analysis study [37] about the implementation of NP in Ethiopia, the pooled estimate of NP implementation was 42.44%. The study was conducted based on seven primary studies. Besides, the study assessed the effects of only two factors namely working environment and nurses’ knowledge of NP with its implementation. However, during conception of our study, there were about 13 primary studies whose NP implementation ranged from 32.7% [21] up to 74.7% [30]. These studies also revealed a wide range of factors associated with NP implementation. Therefore, this systematic review and meta-analysis was aimed to reach the pooled estimate of NP implementation and its associated factors from the aforementioned 17 discrete primary studies in Ethiopia.
Findings of this study will be an input to policy makers and program planners of the Ethiopian government in designing appropriate interventions to increase the quality of nursing care practice. Besides, it is helpful to intervene on the important impending factors of NP implementation. This review will also serve as a basis in providing the national figure for future researchers of evidence based nursing practice.
2. Methods
This systematic review and meta-analysis was conducted based on the methodology of Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) checklist [Supplementary file 1] [38]. It was undertaken through systematic synthesis of the primary studies about implementation of NP during patient care in Ethiopia. The review protocol has been registered in an international prospective register of systematic Review which can be accessed from: =https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019138159.
2.1. Search strategy
For explicit presentation of our review question and clear specification of the inclusion and exclusion criteria, we considered using adapted PICO format. The adapted PICO was comprised of Population (P), Exposure (E), Outcome (O) and Context (setting) as detailed below. In each component of the adapted PICO, search terms are given.
-
a.
Population: Nurses
-
b.
Exposure: Determinants, associated factors, factors, predictors, barriers i.e. educational status, work experience, working environment, supervision, training access, facility accessibility, patient discharge time, nurses' knowledge of NP, nurses’ skill of NP, patient to nurse ratio and administrative support.
-
c.
Outcome: Nursing process, nursing assessment, nursing diagnosis, nursing care plan, nursing care, nursing intervention, nursing implementation, nursing evaluation, patient care
-
d.
Setting (context): Ethiopia, Tigray region, Amhara region, Oromia region, Harari region, Dire Dawa, Afar region, Addis Ababa, Somali region, Southern nations nationalities and peoples region, Benishangul Gmuz rgion, Gambella region.
Using the above adapted PICO format, we developed the following review questions which were focused to retrieve as many relevant primary studies as possible:
2.2. Review questions
-
1.
What is the national magnitude of nursing process implementation during patient care in Ethiopia?
-
2.
What are the factors associated with nursing process implementation during patient care in Ethiopia?
Then, considering the aforementioned review questions, searching of primary studies was done using six international online databases (Pub Med, Scopus, Cochrane Library, Google Scholar, PsycINFO and CINAHL). Each database was searched independently with some modifications of the search strategy (e.g. human subject and English language was applied as limiters of the search). The type of searching strategy was line by line and it was done through title (TI), abstract (Ab) and full text categories. Search operators such as truncation (∗), Boolean operators (“OR” and “AND”) and phrase searching (“…”) were considered. Synonyms were also used for further searching of primary studies. We extended our search from systematic database searching to retrieving reference lists of eligible articles. Besides, the ‘cited by’ and ‘related articles’ functions of PubMed were considered for further literature searching. Literature search was conducted from February 20/2019–March 20/2019. Finally, all studies which were in agreement with the review title were retrieved and screened for inclusion criteria. The literature search was performed by two independent authors, with discrepancies resolved by discussion and consensus. A sample of the primary search string including the truncation (∗), phrase searching (“…”) and synonyms has been provided as a supplementary file for PUBMED database search (Supplementary file 2).
2.3. Outcome variable measurement
NP implementation: NP was said to be implemented when all its consecutive five steps (assessment, diagnosis, planning, intervention and evaluation) were serially performed during patient care [[17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33],48].
2.4. Independent variables measurement
Patient to nurse ratio: Categorized to be < 10 and >10 which is as of the included primary study where ‘10’ was median patient to nurse ratio with IQR (7–12) [24].
Stressful working environment: a disorganized atmosphere of the workplace during patient care [17,18,23,25,26].
Good knowledge of NP: nurses who answered more than 80% of the knowledge questions about NP [17,18,[20], [21], [22], [23], [24],26,30,31].
Poor knowledge of NP: Nurses who answered <55% of the knowledge questions about NP [17,18,[20], [21], [22], [23], [24],26,30,31].
Accessed training: When a nurse was reported of taking at least one round of training about NP implementation [[22], [23], [24],30,33].
Early patient discharge: When patients were decided and discharged of hospitals by case management team of the hospital before completion of their expected inpatient stay due to resource constraint [21,23].
Skill of NP: Those nurses who have scored >26 score were highly skillful, and <17 were low skillful out of a total of 30 scores for skill [30].
Timely reporting system: Regular reporting of NP implementation as stated in the hospital protocol [22].
Supportive supervision: Supervision of NP implementation by the hospitals' supervisory team for improving nurses’ standard implementation of NP [26].
Patients’ self discharge: Patients who refused to complete their plan of care at hospitals [26].
Patients with uncomplicated illness: patients admitted with problems easy to manage [20].
Accessible facility: Having enough basic equipment supplies in the working departments for nurses to implement NP as pointed out by themselves [17,19,[24], [25], [26]].
Work experience: This variable was meant for nurses’ experience of nursing care at hospitals which was categorized as ≥5 years and <5 years as reported by one primary study [31].
Level of education: Nurses' educational status classified as ‘diploma’ and ‘BSc and above’, and it was reported by only one primary study [19,25,33].
Regions: are constitutionally approved administrative states of Ethiopia. These are 9 regional states (Tigray, Afar, Amhara, Oromia, Benishangul Gumuz, Somali, Southern nation nationalities and peoples, Gambella, Harari regions and 2 town administrations (Dire Dawa and Addis Ababa) [6].
2.5. Inclusion and exclusion criteria
Primary studies of any design that reported magnitude of NP implementation and/or associated factors during patient care in Ethiopia were eligible for this study. However, primary studies were excluded due to any of the following reasons: (a) no report on either the prevalence or associated factors of NP implementation, (b) articles without full text, (c) articles with poor quality score, (d) articles whose full text not availed after 3 times of email contact with the corresponding author, and (e) narrative reviews, editorials, correspondence, abstracts, and methodological studies. Two authors (W.A.B and A.Y.A) evaluated the eligibility of all retrieved studies independently, and any disagreement and inconsistencies were resolved through participation of a tie breaking third author (B.M.B).
2.6. Study screening and selection
Search results were first downloaded into Endnote version IX and duplicates were removed. Then, selection of studies was conducted in two stages. First, title and abstract screening was conducted. Then, full-text reviewing was done. Through title and abstract screening by two independent authors (SZB and DMB), studies that mentioned the prevalence and/or associated factors of NP implementation were selected for full text review. Then, from full-text reviewing, any article classified as potentially eligible by either author was considered as a full text and screened by both authors independently. At times of disagreement where a consensus could not be reached between the authors, a third author (D.K.M) reviewed and resolved the disagreements.
2.7. Critical appraisal and reliability check
After screening, selected primary studies were critically appraised for their methodological validity. The appraisal was done using the Joanna Briggs Institute (JBI) appraisal tool for prevalence studies [39]. The tool had a total of nine questions (Q1-Q9), and those studies with positive answers (yes) for more than 50% of the questions in the tool (i.e., ‘yes’ for five or more questions) were included in this meta-analysis. The scoring was done by two authors (WAB and AYA) with discrepancies resolved through discussion and consensus. When disagreements between the two authors were not resolved by discussion, a third author (BMB) was involved as a tie breaker. The statistics (quality scores) that measured the level of agreement for the independent reviews is reported (Supplementary file 3). During critical appraisal of each primary study, more emphasis was given to the appropriateness of the study objectives, study design, sampling technique, data collection technique, statistical analysis, any sources of bias and its management technique.
2.8. Data extraction
First of all, determination of a variable for data extraction was based on two criteria: 1) Clear and consistent measurement (operational definition) of the variable in the included primary studies and 2) if the variable was statistically significant in the primary study as reported by its AOR. The variables on which data were extracted from the appraised primary studies included first author name, year of the study, aim of the study, region of the study, study design, sample size, operational definition of NP, data collection technique and primary outcome of the study (i.e. overall prevalence of NP and associated factors with their respective Adjusted Odds Ratio (AOR). These important data were extracted using a data extraction format prepared on Microsoft excel spreadsheet which was first validated through extracting sample data from some eligible articles based on which important modifications were made for actual data extraction. During extraction, we faced inconsistent reporting of data for some variables in the included primary studies. Therefore, data transformation was undertaken to resolve the inconsistencies. For example, among the five primary studies that reported ‘working environment’, there was one study whose reference category was ‘stressful’ when compared to the rest 4 primary studies having the category of ‘non-stressful’ as reference category in their respective multivariable binary logistic regression output. Hence, the reciprocal ‘AOR’ and confidence interval of ‘working environment’ were considered for this particular study. Moreover, similar fashion was followed for nurses' knowledge of NP (poor and good response categories).
2.9. Statistical analysis
The extracted data were exported to Stata version 14 for meta-analysis. Given the substantial statistical heterogeneity of NP implementation between the included primary studies (I2 = 93%; P < 0.001), pooling of the magnitude of NP implementation was carried out using a random effects model with 95% confidence interval (CI) [42,43]. The pooled effect of associated factors were also independently analyzed and presented using forest plot and AORs at 95% CI. We performed subgroup analysis by study region, study year and data collection technique for evidence of the aforementioned heterogeneity. Publication bias was checked subjectively by a funnel plot while its objective assessment was made from Egger's regression test. A p-value of less than 0.05 was considered significant for absence of publication bias [44]. Finally, we performed a sensitivity analysis to describe whether the pooled effect size was influenced by individual studies.
3. Results
3.1. Search results
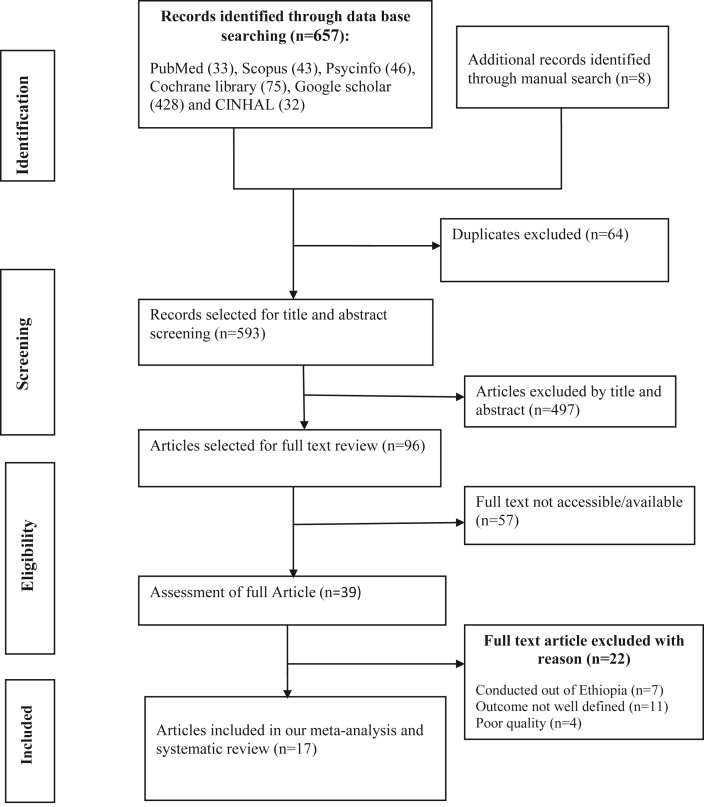
The electronic online and manual search yielded 665 records, of which 64 duplicate records were identified and removed. Title and abstract screening resulted in the exclusion of 497 non-relevant articles. From the remaining 96 articles, 57 articles were excluded because their full text wasn't accessed. Then, 39 articles underwent for full-text screening. However, 22 articles were excluded because these studies reported neither magnitude nor associated factors of NP implementation during patient care in Ethiopia. Finally, a total of 17 primary studies were included in this systematic review and meta-analysis (Figure 1).
Figure 1.
Flow diagram of the study selection process.
3.2. Study characteristics
A total of 17 crossectional primary studies with pooled sample size of 2,819 nurses were included in this meta-analysis. All these primary studies were aimed at reporting the implementation status of NP and/its associated factors during patient care in Ethiopia. Among these 17 primary studies, five studies [20,26,29, 30, 31] were conducted in Amhara region while the rest studies were conducted in Tigray [19,25,27], SNNPR [21,28,33], Addis Ababa [17,18], Harar and dire Dawa [23,24] and other region [22,32] of the country. Twelve of the included primary studies [18,22, 23, 24, 25, 26,28, 29, 30, 31, 32, 33] were conducted at ≥ 2015. All the primary studies included in this systematic review and meta-analysis [17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33] had no considerable risk of bias i.e quality score ≥6 (Table1).
Table 1.
Characteristics of the primary studies included in this meta-analysis of nursing process implementation during patient care in Ethiopia, 2020.
| First author | Study year | Aim | Study region | Sample size | Data collection technique of NP | Primary outcome |
Quality score | |
|---|---|---|---|---|---|---|---|---|
| Magnitude of NP implementation (%) | Associated factors | |||||||
| Aseratie M etal/[17] | 2014 | Determine magnitude of NP implementation and associated factors | Addis Ababa | 192 | self-administered questionnaire | 52.08 | Facility accessibility, working environment and nurses' knowledge of NP | 8 |
| Wube T et al [18] | 2019 | Determine level of NP implementation and associated factors | Addis Ababa | 151 | Self-administered questionnaire | 56.95 | Ward type, working environment and nurses's knowledge of NP | 7 |
| Semachew A [29] | 2018 | To evaluate level of NP implementation | Amhara | 338 | Document review | 47.04 | ………………….. | 8 |
| Abebe N etal [20] | 2014 | to describe the level of NP implementation and associated factors | Amhara | 124 | Self-administered questionnaire | 37.10 | Patients' disease condition and nurses knowledge of NP | 8 |
| Shewangizaw Z etal [21] | 2014 | To assess magnitude and determinants of NP implementation | SNNPR | 98 | Self-administered questionnaire and document review | 32.65 | Patients' disease condition and nurses knowledge of NP | 7 |
| Miskir Y etal [22] | /2018 | To assess implementation of nursing process and its hindering factors | Afar | 102 | Self-administered questionnaire | 42.16 | Training access and nurses' knowledge of NP | 8 |
| Atnafe G etal [23] | 2017 | to assess the practice of nursing process and associated factors |
Harar and Dire Dawa | 174 | Self-administered questionnaire | 48.85 | Nurse seeing patient outcome, early patient discharge time, training access, working environment | 6 |
| Habte S et al [24] | 2015 | To assess the status of nursing process utilization and its affecting factors | Harar and Dire Dawa | 232 | Self-administered questionnaire and document review | 36.64 | nurse to patient ratio, training access, nurses' knowledge of NP and facility accessibility | 7 |
| Baraki Z etal [25] | 2017 | to assess the implementation of nursing process and associated factors | Tigray | 200 | self-administered questionnaire and document review | 35.00 | Nurses level of education, facility accessibility and working environment | 8 |
| Tadie C et al [26] | 2018 | to assess the implementation of NP and associated factors | Amhara | 364 | Self-administered questionnaire and document review | 60.99 | Nurses level of education, facility accessibility and working environment | 8 |
| Hagos F et al [19] | 2014 | To assess the application of nursing process and its affecting factors | Tigray | 97 | Self-administered questionnaire | 37.11 | Nurses level of education, facility accessibility and working environment | 9 |
| Zeleke S et al [30] | 2019 | To asses NP implementation and its barriers | Amhara | 241 | Self-administered questionnaire | 74.69 | nurses' knowledge of NP, nurses' skill of NP and nurses' attention to the importance of NP | 8 |
| Alemu et al [32] | 2016 | To asses NP implementation | Oromia | 82 | self-administered questionnaire | 68.3 | …………… | 7 |
| Adraro [33] | 2015 | to asses NP implementation and associated factors | SNNPR | 138 | self-administered questionnaire | 73.9 | Administrative support, training access, nurses' level of education | 7 |
| Getie et al [31] | 2019 | to asses NP implementation and associated factors | Amhara | 113 | Self administered Questionnaires |
62.8 | Nurses' work experience, administrative support and nurses' knowledge of NP | 8 |
| Haftom G et al [27] | 2013 | To assess the implementation of Nursing Care Process | Tigray | 48 | Document review | 37.5 | ………… | 6 |
| Feleke A et al [28] | 2018 | To asses level of NP implementation | SNNPR | 125 | Document review | 47.00 | …………. | 7 |
SNNPR:Southern Nations Nationalities and Peoples Region.
All the included primary studies measured NP implementation by using similar operational definition of NP implementation (Table 2).
Table 2.
Measurement of NP implementation as of the included primary studies.
| First author year | Operational definition |
|---|---|
| Aseratie M etal/2014 [17] | NP implementation is the practice of nursing process by licensed nurses in which the nurses rendered nursing care based on the five steps of the nursing process |
| Wube T et al/2019 [18] | NP implementation is the level of nursing process application in which the nurses rendered nursing care based on all steps of the nursing process and did documentation in the patient's record |
| Semachew A/2018 [29] | Nurses that document all the components of nursing process in the patient file were labeled as ‘nursing process implemented’ |
| Abebe N etal/2014 [20] | NP implementation is the practice of nursing process by licensed nurses in which the nurses rendered nursing care based on the five steps of the nursing process |
| Shewangizaw Z etal/2015 [21] | Nursing process were operationalized as a process in which nurses are used to solve patient's problems by using the five steps i.e. Assessment, Nursing Diagnoses, Planning, Implementation and Evaluation |
| Miskir Y etal/2018 [22] | Implementation of nursing process in the five Likert scale is never, sometimes, I do not know, usually, and always; those responses of usually and always were taken as implemented and the other responses as not implemented. |
| Atnafe G etal/2017 [23] | If nurses perform nursing process using the five steps of nursing process was taken as nursing process practiced, and those who performed less than five steps of nursing process was taken as nursing process not practiced. |
| Habte S et al/2015 [24] | NP implementation is the level of nursing process application in which the nurses rendered nursing care based on all steps of the nursing process and did documentation in the patient's record |
| Baraki Z etal/2017 [25] | Nurses who answer “yes” for the six nursing process implementation questions and observed for their performance were as implementing the nursing process properly. |
| Tadie C et al/2018 [26] | If the nurse performed and documented all the nursing process components these are, Nursing assessment, nursing diagnosis, nursing care plan, Nursing intervention and evaluation |
| Hagos F et al/2014 [19] | NP implementation is the practice of nursing process by licensed nurses in which the nurses rendered nursing care based on the five steps of the nursing process |
| Zeleke S et al/2019 [30] | NP implementation is the practice of nursing process by licensed nurses in which the nurses rendered nursing care based on the five steps of the nursing process |
| Alemu et al/2016 [32] | If the nurse performed nursing process components these are, Nursing assessment, nursing diagnosis, nursing care plan, Nursing intervention and evaluation |
| Adraro/2015 [33] | When nurses follow all the steps of the nursing process during patient care Np was said implemented |
| Getie et al/2019 [31] | If nurses perform nursing process using the five steps of nursing process was taken as nursing process practiced, and those who performed less than five steps of nursing process was taken as nursing process not practiced. |
| Haftom G et al/2013 [27] | When nurses follow all the steps of the nursing process during patient care Np was said implemented |
| Feleke A et al/2018 [28] | Nursing process considered as practiced if nurse use five consecutive steps of nursing process based on the standard for each patient. These were: Assessment (11 components of Gordens approach), Diagnosis (using NANADA list, use problem etiology and sign/symptom format, and prioritizing problems), Planning (set SMART expected outcome, setting nursing interventions), Implementation (Does the planned intervention implement as planned?) and Evaluation (Appraisal of patient's response to the implemented care). |
3.3. Meta-analysis
3.3.1. Pooled magnitude of nursing process implementation in Ethiopia
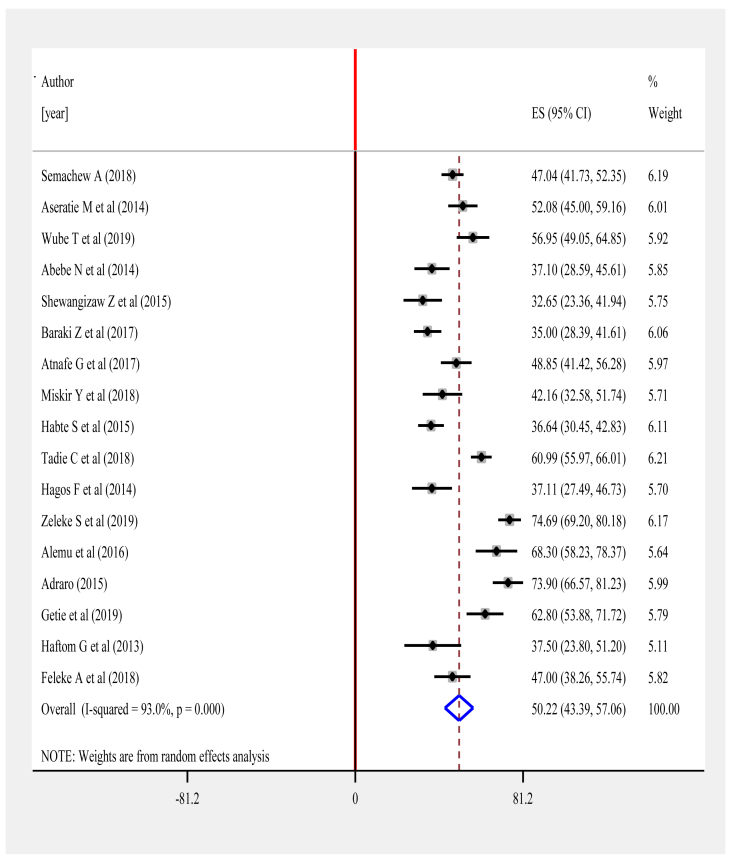
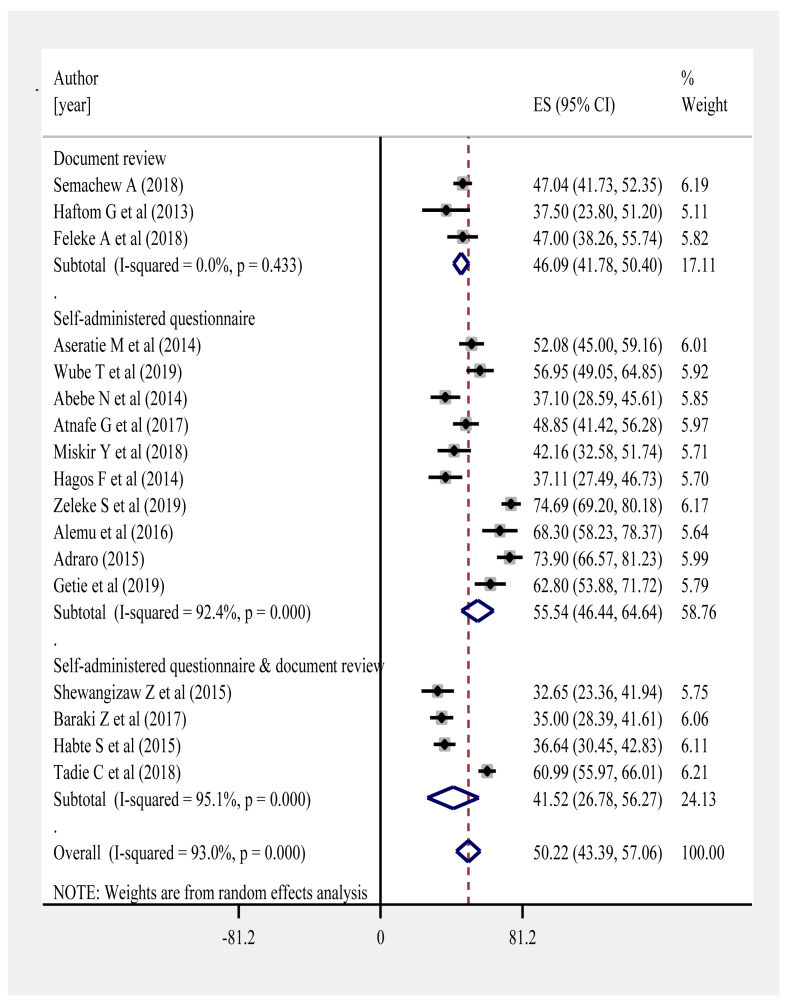
Before meta-analyzing effect sizes about magnitude of NP implementation, we checked whether there was statistical variability between the included primary studies. The checking was done using both visual inspection of forest plot and statistical tests of variation. From visual inspection of the forest plot, there were outlier studies and poor overlap between the confidence intervals for each magnitude of NP implementation on the forest plot suggesting possible statistical heterogeneity between the primary studies. More objectively, we checked the variability based on the Stata generated statistical tests of variation (I squared statistic = 93% and Chi-squared = 229.85 (d.f. = 16); p < 0.001) indicating substantial heterogeneity. Therefore, a random effect meta-analysis model was employed. From the model, the overall pooled estimate of NP implementation was 50.22% (95% CI: 43.392%, 57.057%; I2 = 93.0%, P < 0.001) as reported by the 17 studies Furthermore (Figure 2).
Figure 2.
Forest plot showing the pooled estimate of nursing process implementation.
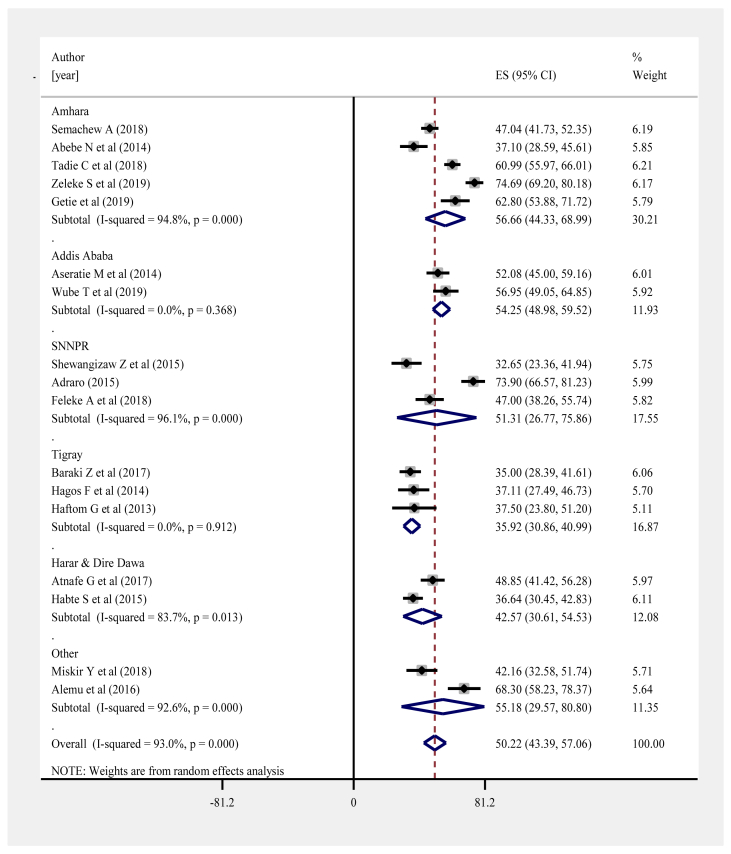
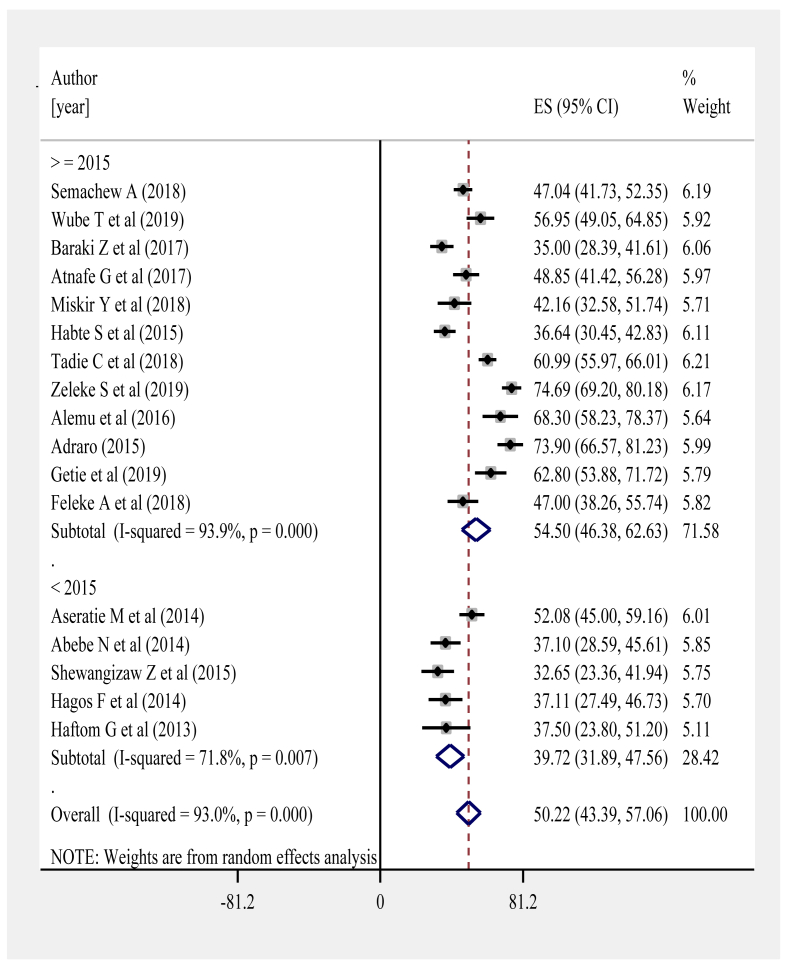
3.3.2. Subgroup analysis
In response to heterogeneity, we performed subgroup analyses based on the following criteria: a) the subgroup analysis hypothesis was pre-specified (a priori) in the registered review protocol; b) there were large subgroup effect sizes; c) Consistent interaction across the effect sizes of NP implementation; and d) the sub-grouping factors (region of study, study year and data collection technique) were characteristics of interest measured at baseline across the studies. All the aforementioned criteria enabled us to place high confidence on the results of our subgroup analyses. From regional subgroup analysis, the highest level of NP implementation was observed in Amhara region 56.66% (95% CI: 44.33%, 68.99%; I2 = 94.8%] whereas it was least implemented in Tigray region 35.92% (95% CI: 30.86%, 40.99%, I2 < 0.001%) (Figure 3). According to subgroup analysis by study year (i.e. study year <2015 and ≥2015), pooled estimate of NP implementation among studies conducted during ≥2015, 54.50% (95% CI: 46.38%, 62.63%; I2 = 93.9%) was higher than before 2015, 39.72% (95% CI: 31.89%, 47.56%; I2 = 71.8%) (Figure 4). Regarding subgroup analysis of NP implementation by data collection techniques, the least prevalence was observed for self-administered questionnaire and document review category 41.52% (95% CI: 26.78%, 56.27%); I2 = 95.1%, p < 0.001) whereas the highest was noticed for the category of self-administered questionnaire 55.54% (95% CI: 46.44%, 64.64%; I2 = 92.4%, p < 0.001) (Figure 5).
Figure 3.
Subgroup analysis of the magnitude of NP implementation by study region.
Figure 4.
Subgroup analysis of the magnitude of NP implementation by study year.
Figure 5.
Subgroup analysis of the magnitude of NP implementation by data collection technique.
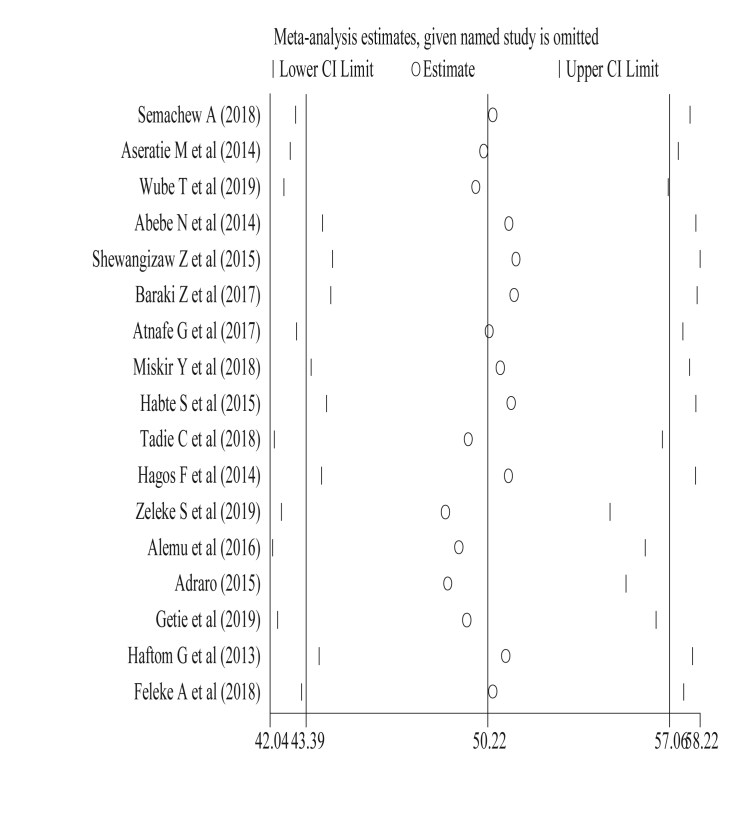
3.4. Sensitivity analysis
The result of sensitivity analyses using random effects model suggested that Zeleke et al influenced the overall estimate significantly. Besides, the aforementioned outlier article (Zeleke et al) can be diagrammatically appreciated from Figure 6.
Figure 6.
Sensitivity analysis of the 17 studies.
3.5. Associated factors analysis
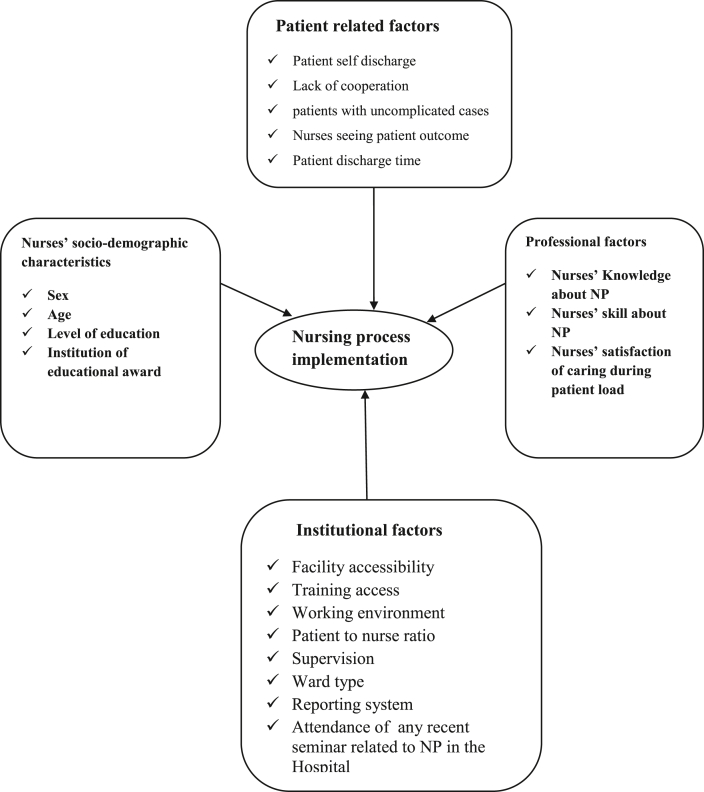
Based on this review, the different factors that could influence the practice of nursing process have been presented as socio-demographic, professional, institutional and patient related categories as discussed below respectively.
3.5.1. Socio-demographic factors
According to a study in Eastern Ethiopia [22], male nurses (AOR = 2.37 (95%CI: 1.05, 5.33) and nurses whose age ≥30 years (AOR = 4.14; 95%CI: 1.10, 15.52) were more likely to practice NP during the care of hospitalized patients.
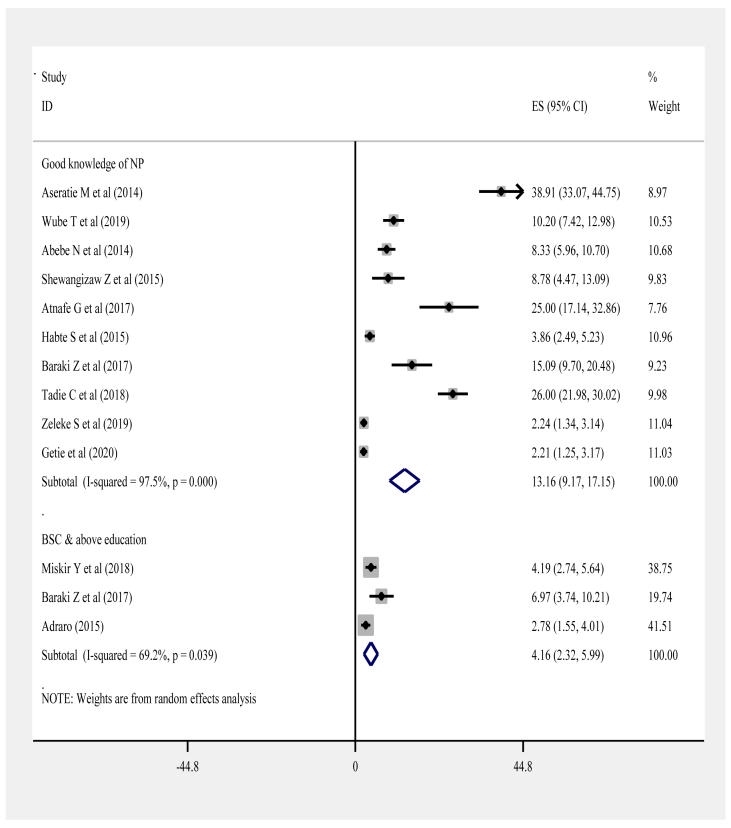
Regarding educational status, pooling of three studies [19,25,33] showed that nurses’ BSC and above level of education was positively associated with NP implementation (Figure 7). Moreover, getting their educational award from governmental institution [22] (AOR = 4.2; 95%CI: 1.435, 12.293) has significant positive association with implementing nursing process in the care of patients as compared to the award from private institutions.
Figure 7.
The pooled effect of nurses' good knowledge of NP and their BSC and above level of education on the implementation of NP during patient care.
3.5.2. Professional factors
A single study [25] showed that nurses dissatisfied from patient load were 98.7% less likely (AOR = 0.013; 95% CI: 0.001–0.130) to implement nursing process in patient care. Furthermore, another study [30] showed that nurses who were not skilled of NP were 59% less likely to implement NP (AOR = 0.41: 95% CI: 0.23, 0.43) in patient care when compared to those skilled ones. As of a study [31], Nurses who had greater than or equal to five years work experience were twice (AOR = 1.79; 95% CI:1.31, 4.84) more likely to implement NP during patient care compared to those having below 5 years experience.
Pooled analysis of 10 studies [17,18,20, 21, 22, 23, 24,26,30,31] revealed that nurses’ having good knowledge of NP were 13.16 times (AOR = 13.16: 95% CI: 9.17, 17.15) more likely to implement NP during patient care than their poor knowledgeable counterparts in Ethiopia (Figure 7).
3.5.3. Institutional factors
Regarding the effect of different organizational factors on NP implementation, attending any recent course or seminar related to NP in the ward or in the hospital (AOR = 15.0; 95% CI: 5.00–44.99) [22], presence of timely reporting system (AOR: 6.97; 95%CI: 1.76, 27.86) and good supportive supervision in the hospital (AOR: 2.50; 95%CI: 1.27–5.03) [26], working in medical ward unit (AOR = 3.43; 95% CI: 1.01, 11. 5) and surgical ward unit (AOR = 9.59; 95%CI: 2.21, 41.61) [18] were positively associated with NP implementation during patient care.
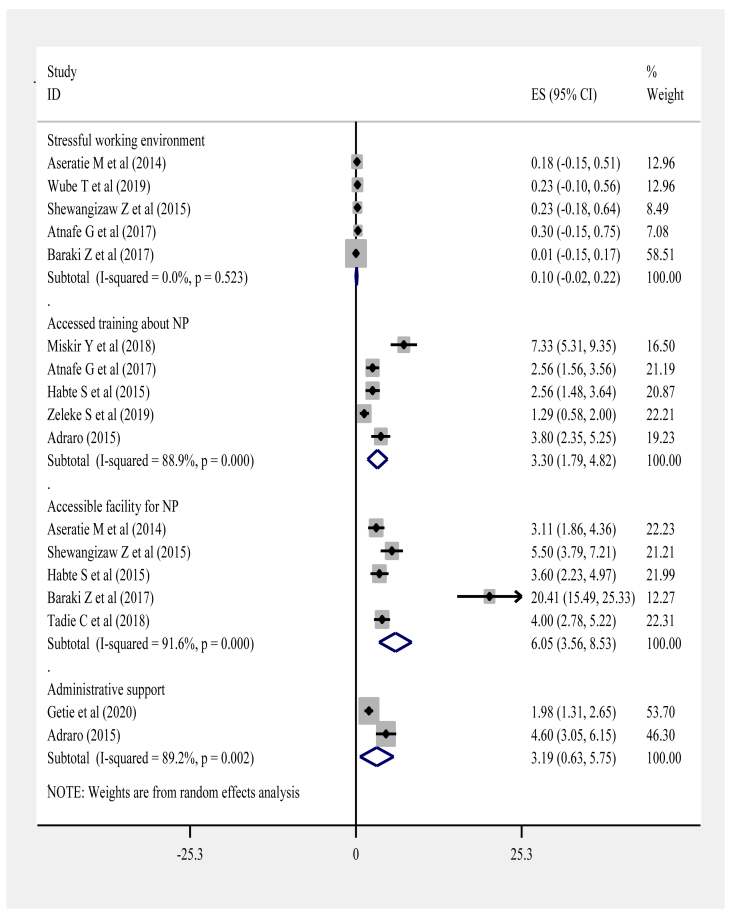
A single study [24] showed that the presence of patient to nurse ratio of >10 was positively associated with the implementation of NP. Moreover, pooling of five primary studies disclosed that stressful working environment [17,18,23,25,26], accessibility of facilities to implement NP [17,19,24, 25, 26] and getting training access [22, 23, 24,30,33] were the factors having higher odds of positive association with NP implementation during patient care in Ethiopia (Figure 8).
Figure 8.
The pooled effects of well-organized working environment, training access and facility accessibility on the implementation of NP.
3.5.4. Patient related factors
From the report of primary studies, patients' lack of cooperativeness (AOR = 0.19; 95%CI: 0.05–0.73) [21] and patients' self discharge (AOR = 0.44; 95% CI: 0.22, 0.86) [26] were negatively associated with the implementation of NP. However, presence of patients with uncomplicated illness (AOR = 5.67; 95% CI: 2.52–12.73) [20] and nurses seeing patient's treatment outcome (AOR = 2.40, 95% CI: 1.10–5.18) [23] were positively associated with its implementation.
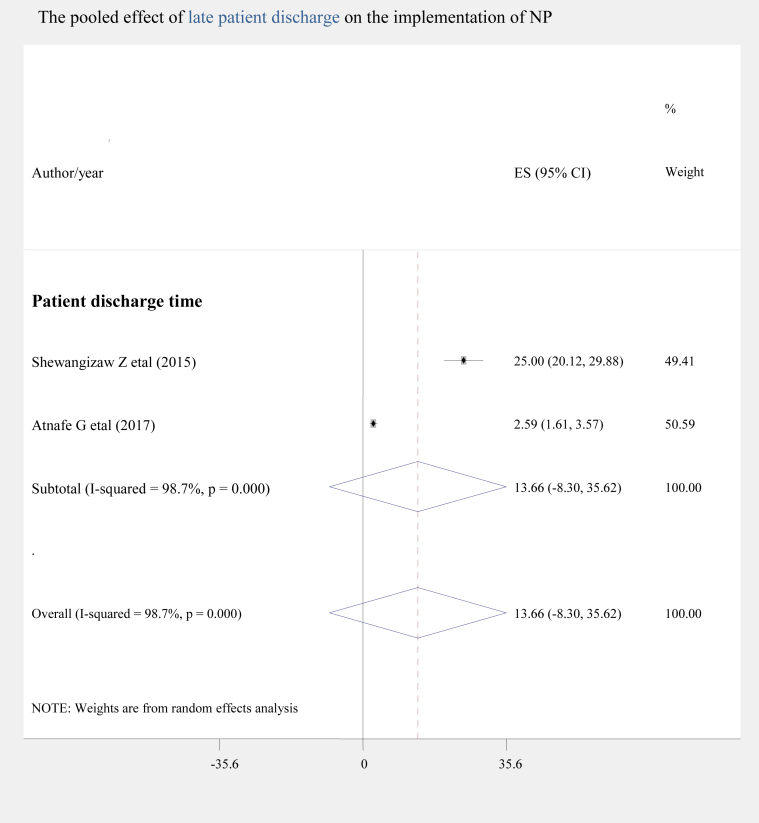
Though patients' discharge time wasn't a significant factor, pooling of two studies [21,23] revealed that the implementation of NP among late discharged patients was nearly 13.6 times higher as compared to those discharged early (AOR = 13.58; 95% CI: -8.37, 35.54) as shown by Figure 9.
Figure 9.
The pooled effect of late patient discharge on the implementation of NP.
3.5.5. Publication bias
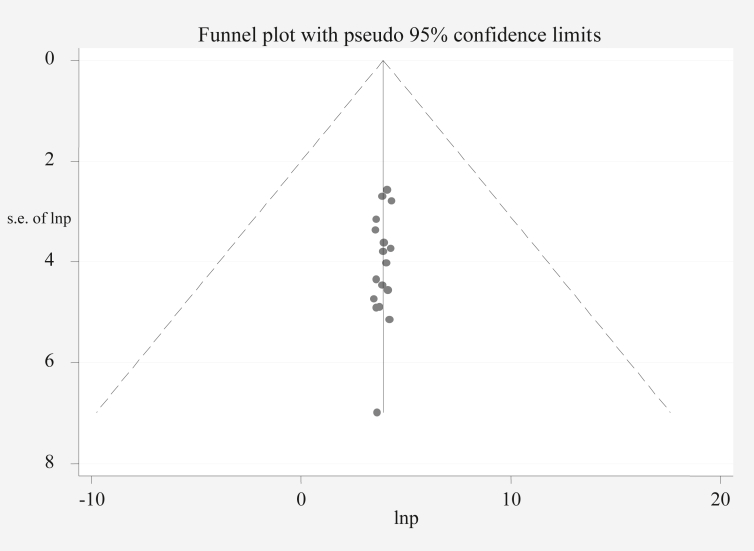
Visual inspection of the funnel plot suggests symmetry (Figure 10). Moreover, the result of Egger's test is statistically non-significant for publication bias (p = 0.234) (Table 3).
Figure 10.
Funnel plot to test publication bias of the 17 studies, lnproportion (x-axis) with standard error of ln proportion (y-axis).
Table 3.
Egger's test (quantitative evidence of no publication bias).
| Std_Eff | Coef. | Std. Err. | t | P > t | [95% Conf. Interval] | |
|---|---|---|---|---|---|---|
| slope | 4.234845 | .2639898 | 16.04 | 0.000 | 3.672164 | 4.797526 |
| bias | .0878505 | .0707695 | −1.24 | 0.234 | −.2386922 | .0629912 |
3.6. Conceptual frame work of associated factors
Figure 11 shows the summary of factors associated with NP implementation in Ethiopia.
Figure 11.
The summary presentation of factors associated with NP implementation in Ethiopia.
4. Discussion
This systematic review and meta-analysis was aimed at estimating the pooled magnitude and associated factors of nursing process implementation in Ethiopia. The pooled estimate of NP implementation was found to be 50.22% (95% CI: 43.392%, 57.057%) which didn't consist with findings from studies in Sweden 98% [36], Brazil 25% [35], Kenya 33.1% [34] and Nigeria 57.1% [14]. The inconsistence could be possibly attributed to the country wise differences in health care system including nursing policy, strategies of nursing care implementation and nurses' educational qualification [9,10,45,46]. Moreover, methodological variations like comprehensiveness of search strategy, eligibility criteria, quality appraisal, data extraction and statistical analysis might have played role. More importantly, in this study, the pooled estimate of NP implementation during patient care 50.22% was relatively higher than that of the prior Ethiopian study 42.4% [37]. This could be explained by the fact that seventeen primary studies with larger sample size (2,819 nurses) were included in our study as compared to the seven primary studies with a sample of 1,268 nurses in the prior study.
From subgroup analysis based on study year, the estimate of nursing process implementation obtained from pooling of studies conducted during or after 2015 was higher 54.50% (95% CI: 46.38%, 62.63%) as compared to the estimate from studies before 2015, 39.72% (95% CI: 31.89%, 47.56%). The possible justification may be due to the fact that Ethiopia signed to meet the health target entitled “ensuring universal quality health-care services” in the sustainable development goals launched by World Health Organization in 2015 [47]. Since then, as a member state, Ethiopia has been trying to address quality health care demand of its citizens by considering nursing care plan as a principal component of the national health care system [48]. Moreover, when the regional subgroups were compared to one another relative to their number of primary studies and sample size, the pooled estimate of NP implementation in Addis Ababa was the highest 54.25% (48.98%, 59.52%). This could be asserted by the presence of greater number of nurses who have good knowledge, skill and experience of NP in Addis Ababa (capital of Ethiopia) than all other regional states of the country. Furthermore, there is organized working environment, good administrative support, facility accessibility and training opportunity in Addis Ababa (capital of Ethiopia) than elsewhere in the country [6,48]. Subgroup analysis of the pooled estimate of NP implementation by method of data collection revealed the largest pooled effect size of NP implementation for the category of self-administered questionnaire 55.54% (95% CI: 46.44%, 64.64%). This may be justified by the greater likelihood of bias from nurses’ self reporting of their NP implementation than it would be from reviewing patient charts [42].
This meta-analysis disclosed the presence of significant positive association between nurses' good knowledge of nursing process and its level of implementation. This could be due to the fact that nurses' theoretical knowledge of nursing assessment, nursing diagnosis, care plan, nursing intervention and evaluation is a prerequisite for practicing NP during patient care [11,46]. Besides, nurses who had BSC and above level of education were 4.2 times more likely to implement NP which accords with the studies across different regions of the globe [10,49]. This may be due to the reason that nurses’ professional development is enabler of their NP implementation during patient care [50,51].
Regarding the impact of working environment, nurses who worked in a stressful working environment were 90% less likely to implement NP compared to those who were working in non-stressful environment. This may be due to what has been explained by Florence Nightingale, ‘to nurse a patient means to nurture the working environment most conducive so that nature can act on it for patient healing [13,52,53]. Regarding the role of training, nurses who accessed training about NP were 2.7 times more likely to practice the NP during patient care when compared to those who didn't get the training. This could be due to the fact that training helps nurses to acquire and update their knowledge of implementing NP during patient care [9,14,51]. Another factor of significance was accessibility of different facilities required for NP implementation, with higher odds of NP implementation among nurses having the facilities thereby necessitating the frequent availability of different equipment in the hospital wards [45,52,53].
4.1. Limitations of the study
Despite strengths of the study in synthesizing national evidence about the implementation of nursing process during patient care in Ethiopia, there are some limitations that need to be considered in future studies. The main limitation was lack of primary studies from 3 Ethiopian regions (Gambela, Somali and Benishangul Gumuz). Besides, some of the primary studies accessed from other regions had smaller sample size. The use of the random effect model might have overestimated the true magnitude of NP implementation. Most importantly, confounding factors that can affect NP implementation were not identified due to the nature of meta-analysis in using aggregated group data, which could have affected the pooled estimate. Because of the above mentioned reasons, our pooled estimate may not actually represent the national figure of NP implementation during patient care in Ethiopia. Therefore, we would like to forward our earnest reminder for the readers to be mindful of interpreting and using this finding in the context of both inherent limitations of the included primary studies and the current analysis. Furthermore, the pooled impact of some factors like nurses' age, nurses' supervision, nurses' satisfaction, patients' self discharge and ward type weren't studied because sufficient primary studies weren't availed about these factors in Ethiopia. It was also difficult to analyze some major factors because these factors were not reported uniformly across the included primary studies. Finally, we want to ensure that the major barriers and challenges of NP implementation during patient care weren't addressed from the perspectives of different key informants in Ethiopia. Overall, since this meta-analysis has systematically identified all the aforementioned limitations, the design of future studies can be substantially improved.
4.2. Relevance for nursing practice
Reaching the national estimate of NP implementation, this meta-analysis has policy implication for evidence based nursing practice. Therefore, top managers and institutions of nursing can adapt nursing policies appropriate to the Ethiopian context for implementing nursing process in the clinical settings.
5. Conclusion
In Ethiopia, the implementation of nursing process during patient care remains low. The main scientifically significant factors that have positive association with NP implementation include nurses' good knowledge of NP, nurses’ BSC and above level of education, well organized non stressful working environment, accessibility of facility to implement NP, training access and optimal patient to nurse ratio.
6. Recommendation
Based on the aforementioned findings, the following respective recommendations have been forwarded to the concerned stakeholders in Ethiopia.
6.1. To the Ethiopian Federal Ministry of Health (FMOH)
The FMOH should strongly work in collaboration with the federal ministry of education on designing national strategies that help nurses advance their level of education from diploma to BSC and from BSC to MSC and above. This helps to mitigate the greatest barrier of nurses’ continuous professional development, thereby increasing their theoretical and practical knowledge about nursing process in the country.
6.2. To the Ethiopian Nurses’ Association (ENA)
The ENA should enforce accomplishment of nursing process in all regional states of the country by establishing regional nursing associations to share nursing tasks. Once established, the regional nursing associations can share nursing process related phenomena of their respective regional catchment thereby facilitating the rate and comprehensiveness of NP implementation in the country. Besides, these associations are more proximal and accessible for nurses to receive feedback and then to ENA thereby forming a bridge between nurses and ENA.
6.3. To nurses, nurse educators, nurse researchers and nursing schools.
Nurses and nurse educators should continually update their theoretical knowledge and practical aspect of nursing process. Nursing schools should also exhaustively invest their curricula on certifying whether their new graduates are equipped with the required knowledge and practice of NP during patient care. Nursing researchers are strongly recommended to conduct future qualitative studies about the barriers (major challenges) of NP implementation in Ethiopia from patient, nurse and administrative perspectives.
6.4. To health institutions
Health institutions should avail all necessary facilities like nursing process forms required for NP implementation in the hospital wards. Collaborating with the regional, federal and other nursing stakeholders, the health institutions in the country should ensure safe and organized working environment. Besides, adequate staffing of hospital wards with nurses should be made to optimize patient to nurse ratio, thereby enabling nurses to have time to care inpatients by making nursing assessment, nursing diagnosis, nursing care plan, implementing the plan into action and evaluation of patients’ response to the nursing interventions. The hospital managers should also facilitate nursing process related seminars, discussions and trainings for nurses in the health institutions.
Declarations
Author contribution statement
Wubet Alebachew Bayih, Metadel Yibeltal Ayalew, Demeke Mesfin Belay, Dejen Getaneh Feleke, Demewoz Kefale Mekonen, Yared Asmare Aynalem, Tigabu Munye Aytenew and Ermias Sisay Chanie: Conceived and designed the experiments; Wrote the paper.
Abebaw Yeshambel Alemu, Binyam Minuye Birhanie, Sintayehu Asnakew and Aklilu Endalamaw: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Asmamaw Demis, Solomon Demis Kebede, Biruk Beletew Abate and Shegaw Zeleke Baih: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Dejen Getaneh Feleke, Demewoz Kefale Mekonen, Yared Asmare Aynalem, Tigabu Munye Aytenew and Ermias Sisay Chanie: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
PRISMA checklist.
Data base search strategy.
Quality assessment of primary studies using the Joanna Briggs Institute (JBI) appraisal tool for prevalence studies.
Supplementary files.
References
- 1.MOH . Vol. 1. 2016. Ethiopian Hospital Service Transformation Guidelines Assessment Tool. [Google Scholar]
- 2.FMOH . 2016. Health Sector Transformation in Quality Guideline. [Google Scholar]
- 3.Darega Birhanu, Dida Nagasa, Letimo Teshale, Hunde Tolashi, Hayile Yadashi, Yeshitla Shewafere, Amare M. Perceived quality of nursing cares practices in inpatient departments of Bale zone hospitals, Oromiya regional state, southeast Ethiopia facility -based cross sectional study. Qual. Prim. Care. 2016;24(1):39–45. [Google Scholar]
- 4.FMOH . 2016. Ethiopian Hospitals Service Transformation Guidelines (EHSTG) 1. [Google Scholar]
- 5.FMOH . 2010. Training of Trainers (TOT) on Ethiopian Hospital Reform Implementation Guidelines (EHRIG) for Nursing Care Practice; pp. 1–128. [Google Scholar]
- 6.FMOH . 2016. Health Sector Transformation Plan-I Annual Performance Report 01. [Google Scholar]
- 7.Federal Ministry of Health (FMOH) 2011. Nursing Care Practice Standards RmfnahcmiAA, Ethiopia; pp. 14–16. [Google Scholar]
- 8.Potter P.A., Perry A.G. Mosby Company, Elsevier Health Sciences; St. Louis, MO: 2017. Fundamental of Nursing. [Google Scholar]
- 9.Zamanzadeh V. Challenges associated with the implementation of the nursing process: a systematic review. Iran. J. Nurs. Midwifery Res. 2015;20(4):411. doi: 10.4103/1735-9066.161002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lotfi . 2018. The implementation of the nursing process in lower and middle income countries: an integrative review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alfaro-Lefevre R. Lippincott Wiliams & Wilkins; Philadelphia: 2006. Nursing Process Overview Applying Nursing Process. [Google Scholar]
- 12.George J.B. Pearson Education India; 2011. Nursing Theories: the Base for Professional Nursing Practice, 6/e. [Google Scholar]
- 13.Selanders L.C. The power of environmental adaptation: Florence Nightingale's original theory for nursing practice. J. Holist. Nurs. 1998:247–263. doi: 10.1177/089801019801600213. [DOI] [PubMed] [Google Scholar]
- 14.Siemuri K.E., Oladayo O.F., Ugochukwu N. Factors influencing the utilization of the nursing process in Ogun State, Nigeria. Int. J. Gen. Med. Pharm. 2014;2(3):57–64. [Google Scholar]
- 15.Ministry of education of the federal democratic Republic of Ethiopia: nursing curricula. www.moe.gov.et/web/guest/home
- 16.Mamseri R.A. University of South Africa; 2012. The Nursing Process as a Means of Improving Patient Care. Master thesis. [Google Scholar]
- 17.Aseratie M. Assessment of factors affecting implementation of nursing process among nurses in selected governmental hospitals, Addis Ababa, Ethiopia; Cross Sectional Study. J. Nurs. Care. 2014;3(3):170. [Google Scholar]
- 18.Wube Tsiyon B. Implementation status of nursing process and associated factors among nurses working in Tikur anbessa specialized hospital Addis Ababa, Ethiopia. Am. J. Nurs. Sci. 2017;8(3):81–91. 2019. [Google Scholar]
- 19.Hagos F. Application of nursing process and its affecting factors among nurses working in mekelle zone hospitals, Northern Ethiopia. Nurs. Res. Pract. 2014:2014. doi: 10.1155/2014/675212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abebe N. The implementation of nursing process and associated factors among nurses working in Debremarkos and Finoteselam Hospitals, Northwest Ethiopia, 2013. J. Nurs. Care. 2014;2014:4–7. [Google Scholar]
- 21.Shewangizaw Z., Mersha A. Determinants towards implementation of nursing process. Am. J. Nurs. 2015;4(3):45–49. [Google Scholar]
- 22.Miskir Y., Emishaw S. Determinants of nursing process implementation in north east Ethiopia: cross-sectional study. Hindawi Nurs. Res. Pract. 2018 doi: 10.1155/2018/7940854. Article ID 7940854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Atnafe G. The practice of nursing process and associated factors among nurses working in public hospitals of Harari people national. Regional State EE. 2017;32 [Google Scholar]
- 24.Sisay H., Nega . 2015. Nursing Process and Factors Affecting its Utilization in Governmental Hospitals at Harari and Dire Dawa Regions. [Google Scholar]
- 25.Baraki Z. A cross sectional study on nursing process implementation and associated factors among nurses working in selected hospitals of Central and Northwest zones, Tigray Region, Ethiopia. BMC Nurs. 2017;16(1):54. doi: 10.1186/s12912-017-0248-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chalie T. North West Ethiopia; 2017. Nursing Process Implementation and Associated Factors Among Nurses in West Amhara Referral Hospitals. [Google Scholar]
- 27.Haftom G. 2013. Improving the Implementation of Nursing Care Process in Mekelle Hospital. [Google Scholar]
- 28.Feleke A.A. Compliance of nurses to national nursing process guideline in Tercha general Hospital,Southern Ethiopia 2018: case study. Adv. Pract. Nurs. 2019;4:155. [Google Scholar]
- 29.Semachew A. Implementation of nursing process in clinical settings: the case of three governmental hospitals in Ethiopia, 2017. BMC Res. Notes. 2018;11(1):173. doi: 10.1186/s13104-018-3275-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zeleke S. 2019. The Prevalence and Associated Factors of Nursing Process Implementation at Public Hospitals in South Gondar Zone, 2019. A Cross-Sectional Study. [Google Scholar]
- 31.Getie . 2019. Implementation of nursing process among nurses at Woldia Referral hospital, Northern Ethiopia: an institution-based cross-sectional study. [Google Scholar]
- 32.Alemu Birhanu, Kebede Tolessa. Factors affecting implementation of nursing process among nurses working in governmental hospitals, Oromia region, Ethiopia, 2016: cross sectional study. Int. J. Clin. Exp. Med. Sci. 2020;6(No. 3):28–34. [Google Scholar]
- 33.Adraro, Mengistu. BMC Nursing . Vol. 19. 2020. Implementation and Factors Affecting the Nursing Process Among Nurses Working in Selected Government Hospitals in Southwest Ethiopia; p. 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kamau M. 2016. Implementation of Nursing Process Among Nurses Working in In-Patients Wards in Rift Valley Provincial General Hospital. Nakuru County, Kenya. [Google Scholar]
- 35.Lopes M. International journal of nursing terminologies and classifications. Eval. Nurs. Proc. Used Brazil. Teach. Hosp. 2010;21(3) [Google Scholar]
- 36.Jansson I. Factors and conditions that influence the implementation of standardized nursing care plans. Open Nurs. J. 2010;4:25. doi: 10.2174/1874434601004010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shibabaw Implementation of nursing process and its association with working environment and knowledge in Ethiopia: a systematic review and meta-analysis. Nurs. Res. Pract. 2020;2020 doi: 10.1155/2020/6504893. Article ID 6504893, 10 pages, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liberati A. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews checklist for prevalence studies. http://joannabriggs.org/research/critical-appraisal-tools.html
- 42.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta- analysis. Stat. Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 43.Ried K. 2006. Interpreting and Understanding Meta-Analysis Graphs: a Practical Guide. [PubMed] [Google Scholar]
- 44.Egger M. Meta-analysis: principles and procedures. Br. Med. J. 1997;315(7121):1533–1537. doi: 10.1136/bmj.315.7121.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mahmoud M.H., Bayoumy H.M. Barriers and facilitators for execution of nursing process from nurses’ perspective. Int. J. Adv. Res. 2014;2(2):300–315. [Google Scholar]
- 46.Sangster-Gormley E., Martin-Misener R., Downe-Wamboldt B., DiCenso A. Factors affecting nurse practitioner role implementation in Canadian practice settings: an integrative review. J. Adv. Nurs. 2011;67(6):1178–1190. doi: 10.1111/j.1365-2648.2010.05571.x. [DOI] [PubMed] [Google Scholar]
- 47.Souza L.P.C.C. Knowledge production about nursing process: analysis of the difficulties during the period from 2003 to 2013. Int. J. Multidis. Curr. Res. 2015;6 (Mar; 3:231) [Google Scholar]
- 48.The Federal Ministry of Health (FMOH) in Ethiopia. 2016. [Google Scholar]
- 49.Fard M.G. Obstacles of nursing process application from perspective of the nursing instructor and nursing students in Zanjan faculty of nursing and midwifery. J. Med. Edu. Dev. 2012;5(8):69–77. [Google Scholar]
- 50.Yildirim B., Ozkahraman S. Critical thinking in nursing process and education. Int. J. Humanit. Soc. Sci. 2011;1(13):257–262. [Google Scholar]
- 51.Julie N.K. Barriers to the implementation of the nursing approach in public hospitals in Lubumbashi in the democratic Republic of Congo: a crossectional descriptive study. Open Acc. Lib. J. 2017;4(7):1. [Google Scholar]
- 52.Sher A.N.A., Akhtar A. Clinical application of nightingale's theory. J. Clin. Res. Bioeth. 2018;9:329. [Google Scholar]
- 53.Nightingale F. Lippincott Williams & Wilkins; 1992. Notes on Nursing: what it Is, and what it Is Not. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
Data base search strategy.
Quality assessment of primary studies using the Joanna Briggs Institute (JBI) appraisal tool for prevalence studies.
Data Availability Statement
Data included in article/supplementary material/referenced in article.