Abstract
The Oregon Health Plan (OHP) has been widely heralded as an important innovation in medical care policy and rationing. Oregon's pioneering method of prioritizing funding for health care through systematic and public ranking of medical services has drawn substantial international interest. This paper reviews the experience of the Oregon plan since it began operation in 1994. We argue that widespread misconceptions persist about the significance of the OHP. In particular, there is little evidence that the OHP has operated as a model of explicit rationing. In reality, Oregon has not rationed services, nor has its policy of cutting public coverage for services produced substantial savings. These findings have important implications regarding the desirability and feasibility of adopting a policy of removing items from the list of insured medicare services in Canada. Oregon's experience suggests that drawing the line on medicare coverage would be more difficult and less financially rewarding than advocates claim.
The Oregon Health Plan (OHP) has been widely heralded as an innovation in health policy as the first public insurance program to ration medical care explicitly, systematically and openly by denying coverage for health care services. Consequently, the OHP has attracted substantial international attention, especially from health systems such as the British National Health Service that are engaged in debates over setting priorities for public coverage of medical services within financial constraints. For many health care analysts, as well as providers, Oregon stands out today as a pioneer in its willingness to embrace rationing and make the hard decisions raised by the dilemmas of modern medicine. Indeed, the Oregon story has seemed so compelling, and is by now so familiar, that it has attained “nearly mythical status” in the international health policy community.1
At the same time, the Oregon plan has been beset by controversy regarding its apparent embrace of rationing. From the beginning, what appeared to be brave innovation to some seemed to be dangerous and morally dubious experimentation to others. The debate between advocates and critics of the OHP has continued to this day, with the advocates of transparency pitted against the defenders of humane treatment of the most disadvantaged.
Yet a substantial gap exists between widespread perceptions of the Oregon model and its actual performance. Thus far, the reality of rationing has not lived up to the rhetoric of either the supporters or the critics of the Oregon plan. To clarify that experience for medical policy-making is the purpose of this article. In our conclusion, we suggest how this experience might be of particular relevance to Canadian discussions of priority setting, the removal of items from the list of insured medical services and the rationalization of policy-making within medicare.
The OHP: a brief history
The state of health care in Oregon first came to prominence in 1987 with the case of Coby Howard, a 7-year-old boy diagnosed with leukemia. Howard required a bone marrow transplant. The Oregon legislature, however, had decided earlier that year not to fund transplant operations, which were an optional service at the discretion of states under the Medicaid program that provides insurance to low-income Americans. The state consequently refused to pay for the operation. The case drew substantial media attention, and private efforts to raise money for the operation were undertaken, but Coby Howard died later that year before sufficient funds were raised.2 In response to the Howard case, an Oregon state representative introduced legislation to restore Medicaid funding for bone marrow transplants. However, the bill was opposed by John Kitzhaber, a former emergency medicine physician and then president of the state senate who later became Oregon's governor. Kitzhaber noted that in Oregon, as in all other US states, substantial segments of the population were uninsured and lacked coverage for even the most basic medical services. Kitzhaber contended that, in this context, it made little sense for the state to pay for costly services, such as transplants, that would benefit relatively few Medicaid recipients. He argued that, although Oregon could not conceivably afford to pay for every medical care service for every person, it could expand insurance to cover all the uninsured while controlling expenditures if it was willing to ration care.2
In 1989, the Oregon legislature enacted a health reform bill sponsored by Kitzhaber that aimed to extend insurance coverage to all Oregonians. The bill contained 2 major provisions: a mandate for private employers to provide their workers with health insurance and an expansion of the state Medicaid program to cover all people in the state below the federal poverty line. At the time, Medicaid covered only 42% of low-income Americans, and other states had been tightening eligibility requirements in response to growing program expenditures, thus adding to the already substantial ranks of the uninsured in the United States. In contrast, Oregon pursued a “pincer strategy” of expanding both public and private sources of medical insurance to produce a system of universal coverage. Oregon's employer mandate, which was beset by business opposition and hampered by the election of a conservative Republican legislative majority in 1994, never received the federal waiver necessary for its implementation. Consequently, Oregon's aim of achieving universal coverage, which is something that no US state has yet attained, was not met. Yet the state's Medicaid reforms, after considerable national debate, were approved by the Clinton administration, and the OHP began operation in 1994.
Rationing as public policy: the list
The OHP expanded Medicaid to cover all state residents below the federally established poverty line. The price for that expansion, though, was to be paid by rationing services. Oregon's model of rationing revolved around the creation of a list of medical services. A state-appointed Health Services Commission reduced over 10 000 medical procedures to a list of 709 medical conditions and their related treatments (known as “condition/treatment pairs”). Through a process of community meetings, public opinion surveys on quality of life preferences, cost–benefits analyses and medical outcomes research, the commission then ranked these condition/treatment pairs according to their “net benefit.”3 These rankings were intended to reflect community priorities regarding different medical conditions and services, physicians' opinions on the value of clinical procedures and objective data on the effectiveness of various treatment outcomes. The list itself was meant to create an objective and scientific vehicle for setting priorities for medical spending. The initial incarnation of the rankings was generated by a mathematical formula that integrated the data from clinicians, the public and outcomes research. Future reorderings and additions of services were to be incorporated into the list on the basis of that formula. The Oregon approach to rationing, which simultaneously drew on public preferences and cost–benefit analyses, thus represented an unusual marriage of health services research and deliberative democracy (Table 1).3
Table 1

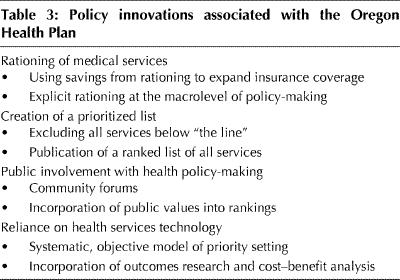
The core idea behind the Oregon reforms was that the legislature would decide each session how much money to allocate for the OHP, and a line would literally be drawn on the list according to how many services that allocation covered. All the services above the line would be covered by the state; however, the OHP would not pay for any of the services below the line. Moreover, the legislature was not permitted to reduce payments to medical providers nor to cut people off from Medicaid coverage. In the event of a financial shortfall, the choice was either to move higher up the list, thereby excluding more services, or to earmark more revenues for the program. The initial list touched off a firestorm of national controversy. Some questioned the ethics of rationing services only for the poor and predicted that, over time, benefits would be increasingly reduced to the point of inadequacy.4 Others questioned the logic of the list itself, especially since its initial version produced some rankings that defied common sense.5 In order to implement the OHP, state policy-makers were forced to make changes to satisfy federal administrators and public concerns about quality of life for people with disabilities. Oregon has used the list since 1994, with the most recent OHP benefit package in 1999 covering 574 of 743 conditions (Table 2).6 As intended, the state legislature has been forced to draw a line publicly in service coverage every 2 years (Table 3).
Table 2
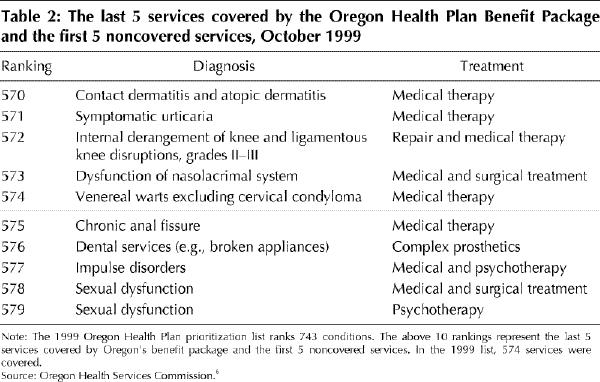
Table 3
The OHP in operation
How has rationing that is based on the explicit ranking of services worked in practice? International interpretations of the Oregon model as an exemplar of policy innovation in rationing still largely reflect impressions formed during the debate over the plan's enactment. This is unfortunate, because the implementation of the OHP bears little resemblance to that debate. Consequently, the significance of the Oregon model has been widely misinterpreted.7 After 6 years of operation, 5 conclusions stand out about the OHP.8,9,10,11 First, contrary to expectations, there has been no widespread rationing of services in the state. The total number of services excluded from the list has been relatively small and their medical value generally marginal. Even as the state now seeks federal approval to move the list up 10 spots, there is no targeting of widely used, medically necessary services. On the contrary, the benefit package covered by the OHP under its rationing system is more generous than under the state's old Medicaid system, and for some crucial services, such as mental health and dental care, it is considered superior to commercial insurance in Oregon. The absence of wide-scale rationing in Oregon, as well as the gap between impressions of the plan and the reality of its operation, is illustrated by the fact that coverage for transplants — which were singled out rhetorically as a target for cutbacks by the plan's architects — is actually more generous and comprehensive today than before the OHP rationing scheme was enacted.
Second, establishing an explicit limit on service coverage is much more difficult in practice than in theory. Although the Oregon legislature has drawn a line across the list of prioritized services, that line has been rather fuzzy. Put simply, many Medicaid recipients continue to receive services that are supposedly excluded by the OHP. In large part, this can be attributed to the reticence of providers when it comes to abiding by the rules. The OHP pays for all diagnostic visits and procedures even if treatment is not covered, and physicians have taken advantage of this loophole to provide uncovered medical services. Patients presenting with comorbidities have also been diagnosed with conditions covered by the list in efforts by physicians to secure patients' access to services below the line.
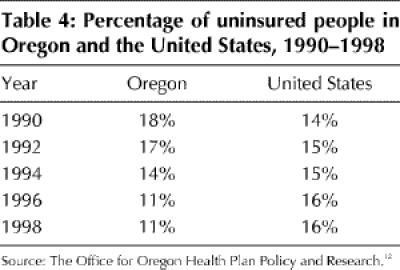
Third, Oregon's system of priority setting through the list has not produced significant savings. Administrators estimate that during its first 5 years of operation, the list saved the state only 2% of total expenditures from the amount that it would have spent under the previous system.8 That the list has not produced generous savings should not come as a surprise given the relative paucity of services excluded. Nevertheless, Oregon has managed to expand health insurance coverage to over 600 000 people, reducing the state's uninsured rate from 17% in 1992 to 11% by 1997 (Table 4).12 (This is an achievement that is hardly exceptional by international standards, yet still qualifies as impressive in the United States, where the national rate of uninsurance exceeded 16% in 1998.) However, the expansion of state insurance in Oregon was not funded by rationing and savings from the list, as is commonly (and mistakenly) assumed, but by raising revenues (primarily through a cigarette tax) and moving Medicaid recipients into managed-care plans. The notion that rationing through the list would produce enough savings for Oregon to finance universal coverage has proven to be an illusion.
Table 4
Fourth, the OHP has not operated as the scientific vessel of rationing that it was advertised to be. Although initial rankings were based in large part on mathematical values, controversies around the list forced administrators to make political concessions and move medical services “by hand” to satisfy constituency pressures and the federal government. Analyses of the original list have shown that subjective judgements, not the initial formula, are the primary influence on service rankings.3 Once the methodology of the list was compromised, the aspiration that the list could function as a self-regulating mechanism according to formula had to be abandoned. New services and revised rankings are determined according to the preferences of the Health Services Commission. In short, the OHP provides no evidence for the presumption that a working system of medical service prioritization can be implemented on the basis of available cost–benefit analyses and outcomes data.
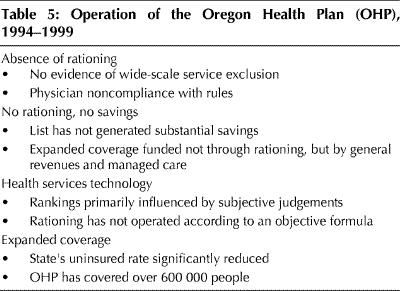
Fifth, despite the OHP's status as a celebrated US policy innovation, no US state or other nation has emulated the Oregon model. In part, this is because what other jurisdictions presumed was the key to Oregon's ability to expand coverage — the list and a formulaic system for rationing — turned out to be illusory. The real innovation in Oregon has been drawing on public participation to build public support and raising revenues for expanding insurance for the poor (Table 5). It is also the case that the furor over the Oregon plan has dissuaded others from similar efforts. The considerable political controversy that comes with the decision to terminate coverage for medical services explicitly and publicly is baggage that no other US state has been willing to take on and few nations have found appealing.
Table 5
Lessons for Canada
The extent of Canadian interest in removing items from the list of insured services, or “delisting,” is not obvious, of course. When he was Newfoundland's premier, Brian Tobin, citing the aging of the Canadian population and the financial pressures of new technologies, publicly pondered whether “new therapies that benefit the very few [should be] insured by the government, even if they are very costly?”13 Tobin's premise, that delisting is a serious policy option for “sustaining” medicare, is by no means the subject of Canadian consensus. But both delisting and the concomitant commitment to explicitness are so much part of the international health policy discussion that Oregon's realities are worth pondering.
The most important lesson from the Oregon experience for Canada, or any other industrialized democracy, is that explicit delisting of services is unlikely to produce substantial savings. Governments seeking such savings by opening public debate on what services their health systems should exclude are likely, we contend, to be disappointed. The political paradox of rationing, as we term it, is that the more public the decisions about priority setting and rationing, the harder it is to ration services to control costs. Paradoxically, more discussion about setting substantial limits on medicare's benefit package could actually increase costs, as it did in Oregon, because legislators and health ministers are placed in the precarious position of confronting public pressures not to cut services, as well as to include future services. Indeed, the OHP moved debates over Medicaid policy and service coverage from the quiescence of legislative corridors to the front pages of the state's newspapers. The prominence of public discussions in Oregon regarding state health policy is quite rare by US standards, where Medicaid policy-making generally receives scant public attention.14 Thus, the OHP created what Canada already has, namely, a policy-making process that inevitably leads to high-profile media coverage and public debate over health care.15
Yet, as the Oregon case demonstrates, that process does not guarantee, and in fact may inhibit, the success of explicit efforts to cancel coverage for particular services. That delisting is unlikely to succeed as a cost containment strategy is supported by the British experience. In the National Health Service, British health authorities initiated a policy of no longer insuring certain services, only to retreat after several years back to the core benefits package.1 In New Zealand, a government-appointed commission charged with defining a core benefits package for the public insurance program failed to reach agreement and thus refused to exclude any services.16 In the Netherlands, reformers have persistently appealed for explicit choice about core benefits, without making a substantial change in Dutch medical practices or outlays. These international experiences were echoed in Ontario, where hospital and physician services were reviewed with the aim of delisting those of little or no value. However, the review ultimately produced a small list of services to be cut whose cumulative costs amounted to small change, but nonetheless generated considerable controversy (Steven Lewis, Access Consulting Ltd., Saskatoon, Sask.: personal communication, 2000). In short, the appeal for transparency in medical decision-making is like a zombie, an idea that refuses to die despite its limited utility.
All of these experiences underline a point that many advocates of explicit rationing have so far largely ignored: the more that rationing decisions are made public and explicit, the less likely that a public insurance system is able to ration services. If cost containment is the goal, implicit rationing, when governments set budgetary caps and limit the supply of costly technology, leaving most so-called bedside rationing decisions to physicians, is a more sound financial strategy for Canadian policy-makers.
Although financial savings have been the primary banner for delisting, the rationalization of services has also been touted as a benefit. Here the Oregon model offers a decidedly mixed lesson. Guided by the list, the OHP arguably offers a more sensible Medicaid benefits package today than it did a decade ago, with more emphasis on mental health and preventive services. On the other hand, rationalization of coverage has had little to do with scientific formulae and more to do with the subjective judgements of Oregon's health administrators. Certainly, research on clinical outcomes and quality of care can enlighten such decisions. Yet ultimately, setting priorities on health care cannot be systematically derived from cost–benefit analyses. Moreover, there is a fundamental problem with the strategy of excluding entire categories of services. Whereas there may be wide agreement to exclude services of questionable medical necessity such as tattoo removal, agreement on what is fair game for exclusion is not likely to reach very far. There are few medical services for which no substantial medical benefit will accrue to some patients. Excluding entire categories of services, regardless of individual circumstances, puts policy-makers in the uncomfortable position of insuring medical care for patients unlikely to benefit from covered services, while denying care to patients requiring services that are not covered. Such a policy not only makes little sense, it is also, as the behaviour of physicians in Oregon indicates, difficult to implement.
In sum, the OHP has not been the model of rationing that its advocates hoped for or its critics feared. Rather, Oregon's experiment with an explicit process of ranking services has underlined how difficult it is to draw the line and cut off public coverage for services. The Oregon case suggests that delisting is neither viable nor desirable as a strategy for controlling medicare costs in Canada.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Reprint requests to: Dr. Jonathan Oberlander, Department of Social Medicine, School of Medicine, University of North Carolina–Chapel Hill, Chapel Hill NC 27599-7240, USA; fax 919 966-7499; oberland@med.unc.edu
References
- 1.Klein R, Day P, Redmayne S. Managing scarcity: priority setting and rationing in the National Health Service. Buckingham (UK): Open University Press; 1996.
- 2.Fox DM, Leichter HM. Rationing care in Oregon: the new accountability. Health Aff (Millwood) 1991;10:7-27. [DOI] [PubMed]
- 3.United States Office of Technology Assessment. Evaluation of the Oregon Medicaid Proposal. Washington: The Office; 1992.
- 4.Rosenbaum S. Poor women, poor children, poor policy: the Oregon Medicaid experiment. In: Strosberg M, Wiener J, Baker R, Fein IA, editors. Rationing America's medical care: the Oregon plan and beyond. Washington: Brookings Institution; 1992. p. 103-4.
- 5.Aaron HJ. The Oregon experiment. In: Strosberg M, Wiener J, Baker R, Fein IA, editors. Rationing America's medical care: the Oregon plan and beyond. Washington: Brookings Institution; 1992. p. 107-11.
- 6.Oregon Health Services Commission. Proritization of health services. A report to the govenor and legislature. Salem (Ore): The Commission; 1999.
- 7.Ruggie M. Realignments in the welfare state: health policy in the United States, Britain, and Canada. New York: Columbia University Press; 1996.
- 8.Jacobs L, Marmor T, Oberlander J. The Oregon Health Plan and the political paradox of rationing: what advocates and critics have claimed and what Oregon did. J Health Polit Policy Law 1999;24(1):161-80. [DOI] [PubMed]
- 9.Leichter HM. Oregon's bold experiment: Whatever happened to rationing? J Health Polit Policy Law 1999;24(1):147-60. [DOI] [PubMed]
- 10.Bodenheimer T. The Oregon Health Plan — lessons for the nation. First of two parts. N Engl J Med 1997;337(9):651-5. [DOI] [PubMed]
- 11.Bodenheimer T. The Oregon Health Plan — lessons for the nation. Second of two parts. N Engl J Med 1997;337(10):720-3. [DOI] [PubMed]
- 12.The Office for Oregon Health Plan Policy and Research. The uninsured in Oregon, 1998. Salem (Ore): The Office; 1999.
- 13.Kennedy M. Canadians must ‘draw line’ on medicare. Ottawa Citizen 2000 May 2; Sect A:1.
- 14.Marmor T. Understanding health care reform. New Haven (Conn): Yale University Press; 1994.
- 15.Marmor T, Mashaw J. Canada's health insurance and ours: the real lessons, the big choices. Am Prospect 1990;(3):18-29.
- 16.Coulter A, Ham C. The global challenge of health care rationing. Buckingham (UK): Open University Press; 2000.


