Abstract
Childhood obesity recommendations advise providers to use family-based care for the treatment of youth and adolescent obesity. Family-based care, defined as the inclusion of a caregiver and a youth, is commonly conducted through behavioral interventions that target the dietary and physical activity behaviors of the attending parent-youth dyads. However, focusing on behaviors isolated to the parent and youth neglects the rest of the family members, and the larger rules, routines, communication, and dynamics in the family. Family-based interventions grounded in family systems theory (FST) target family dynamics to influence weight-related behaviors through higher-level changes in the family. The utility of using FST in childhood obesity treatment has not been extensively conceptualized or applied. Few outcome studies have reported on variables representative of FST, and even fewer FST interventions have been conducted. Because of the lack of detail on the application of FST to childhood obesity treatment, providers are left with little clarity on how to use FST in clinical encounters. We provide the background and evidence for use of FST, detail how families organize around weight-related behaviors that contribute to obesity, and on the basis of their organization, what type of treatment might be beneficial, FST-informed or family-based behavioral interventions. Finally, a suggested family-based clinical algorithm is provided detailing the use of FST through assessment, intervention, and follow-up that can be refined over time by providers and researchers committed to viewing obesity in the context of the family and family dynamics.
Keywords: family environment, family intervention, obesity, systems change, weight management, youth
Approximately one-third of youth and half of adults living in the United States are overweight or obese.1 Youth with 1 parent with obesity have a 2 to 3 times greater odds of becoming obese.2 The strong correlation between youth and parental obesity is evident in childhood obesity treatment, in which youth and parents experience congruent changes in their weight status.3,4 Because of the high prevalence of overweight and obesity, it is likely that many parent-youth dyads currently have or will develop obesity.
In 2007, Barlow and colleagues developed expert committee recommendations,5 which state that providers should be family-based in their treatment of youth with obesity, focusing on weight-related behavior change, not just education. Family-based treatment typically involves a targeted caregiver (often a parent) and youth.5 Behavioral approaches to weight loss, primarily delivered through family-based behavioral therapy (FBBT), effectively produce weight loss and behavior change.6,7 Interventions using FBBT target youth and parents’ specific weight-related skills and behaviors including: monitoring, goal setting, rewards, problem-solving, behavioral contracting, and relapse prevention.8-10 FBBT interventions have shown robust short-11,12 and modest long-term (10-year) success.8 However, the homogeneous samples of middle to upper class, Caucasian, 2-parent families used in these studies challenge their generalizability to all families.8-10
Although FBBT interventions have shown some success, changing youth and/or parent behaviors has an unknown effect on the overall interpersonal dynamics of families in treatment. Family dynamics might have a reciprocal and undetermined effect on the weight-related behaviors of youth and their family. Without addressing the dynamics among families, youths’ newly adopted behaviors might not be sustainable without reorganization of family routines, rules, and communication around weight-related (diet and physical activity) behaviors that contribute to obesity.
Family Systems Theory And Childhood Obesity Treatment
Family systems theory (FST) views the family as a complex, interacting system, and provides a framework for understanding family functioning as an “open, ongoing, goalseeking, self-regulating social system,13” with 4 basic assumptions:
Elements of a system are interconnected.
Systems are best viewed as a whole.
Environment interacts with the system in a feedback loop.
System is a heuristic model used for understanding, and is not reality.
The tenets of FST include: families determine membership; subsystems exist, such as parent-child, spouse, and sibling relationships; families strive to maintain equilibrium; resources are needed for adaptation and change; existence of family rules; and likely the most important tenet describing behaviors, first- and second-order change. First-order change is how a family receives input from their surrounding environment. Second-order changes require the reorganization of rules and routines to make lasting first-order changes and changes to the overall family environment.
FST-based interventions expand the treatment plan beyond individual behaviors to the dynamics and relationships among family members.14 Relevant to childhood obesity, overall family dynamics around weight-related behaviors are targeted in treatment, either indirectly through FBBT, or inadvertently by engaging multiple family members in treatment.15,16 According to FST, change happens at the family level to influence overall family functioning and long-term individual behavioral change.17 Few researchers have conceptualized FST for the treatment of childhood obesity,15-18 and fewer yet have designed interventions to evaluate outcomes consistent with FST.19,20 Exploration of FST-based treatment is warranted, because it has been used in disease states for which adherence is vital to positive health outcomes, such as substance use,21 HIV,22 and type 1 diabetes mellitus.23-26 Additionally, impaired family dynamics, in FST-informed studies, have been associated with adolescent depression, anxiety,27,28 substance use,29 and eating disorders.30
Few scholars have conceptualized how the core tenets of FST can be applied to childhood obesity treatment.12,15,17,18,31 For example, Skelton et al described use of FST for childhood obesity treatment, including “…understanding family rules and rituals to facilitate the goal setting process.”17 pp 893 However, previous conceptualizations of FST applied to childhood obesity treatment do not describe how change actually happens for families in treatment, and how family routines, habits, and overall processes can contribute to obesity; this can be described as families “organizing” around weight-related behaviors, and is a more nuanced view of youth and family routines specific to diet and activity. This is a significant limitation of previous work, which approached the treatment of all families the same way, regardless of their interpersonal dynamics and their organization around diet and activity. On the basis of their family functioning and organization, families might be better served by FST or FBBT interventions to target overall family dynamics or individual youth and/or parent behaviors, respectively; further guidance on determining which families could benefit from the different approaches are discussed.
Using the FST concepts of first- and second-order change,32 clinicians can assist families to enact sustainable long-term behavior modification. For example, as a first-order change, parents might decide to limit a child’s screen time (individual behavior).32 Second-order changes could include scheduling time to play active games together instead of unscheduled sedentary activities like television (family routines),32 establishing family-wide limits on media use (family rules), and having conversations during family meals around positive health messages (family communication). FBBT interventions promote first-order change (change in parent and/or child behavior), but overall family functioning remains the same without changing family routines, rules, and dynamics. FST-informed interventions promote second-order change, in which the family as a whole changes their interactions (family functioning), establishing new routines, rules, and communication dynamics. Table 1 lists first-order change targets using FBBT and second-order targets on the basis of FST.
Table 1.
Targets of FBBT and FST Interventions
| FBBT |
FST |
||
|---|---|---|---|
| Behaviors and Practices | Routines and Dynamics | ||
| First-order Change | Self-monitoring | Second-order Change | Family structure |
| Goal setting | Family rules | ||
| Problem solving | Family communication | ||
| Behavioral contracting | Family responsiveness | ||
| Relapse | Family involvement | ||
| Prevention | Family strengths | ||
FBBT indicates family-based behavioral treatment; FST, family systems theory.
FBBT and FST-Informed Intervention Outcomes
In the most recent systematic review evaluating the methodological rigor of pediatric weight management through FBBT and FST, only 2 FST-informed interventions were published, versus 13 FBBT.27 Flodmark and colleagues randomized 10- to 11-year-old youth into 3 different groups: treatment as usual, diet/exercise, and diet/exercise with 6 family therapy sessions; the family therapy group maintained a significantly smaller increase in body mass index (BMI) than the treatment as usual group at 1 year.33 This study had one of the lowest attrition rates (11%), second highest rating for methodological rigor, highest treatment effect score, and was the second most effective study of the entire review. Kitzman-Ulrich et al randomized 12- to 15-year-old adolescents into 3 different arms for 16 weeks: family-group therapy (ie, multiple families in group) with psychoeducation, psychoeducation only, and wait-list control.34 There were no significant differences between groups for BMI z-score after 16 weeks, methodological rigor was average, and the treatment effect score was among the lowest in the review. On the basis of treatment effect score alone, the studies grounded in FBBT scored higher than the FST-based studies (3.2 vs 2.5), although it is clear that there are evident differences between the 2 FST-based studies (score of 4 vs 1), bringing down the FST mean score. Because there were only 2 FST and 13 FBBT studies, limited conclusions can be drawn.27 The authors recommended that future work is needed to explore potential uses of FST-informed interventions.27
Others have used specific strengths-based models of FST in childhood obesity. Similar to how FBBT is combined with motivational interviewing35,36 to identify strengths to propel families forward with their goals, FST scholars have sought methods to expand family-wide strengths to challenges with behavior change. The most common strengths-based FST approach is solution focused,37 in which providers work with families to identify what is working well, and how to extend these strengths to their current challenges. For example, a parent and child might work together to ensure the child completes her homework every night; this could be extended to engaging in discussions about meal preparation and engaging in physical activity together. These interventions have been used in other countries with mixed results.38,39 Additional studies are needed to determine what family-level factors (ie, family functioning) to target as outcomes to fully explore the utility of FST in obesity treatment.
Potential Predictors and Outcomes Representative of FST
FST-specific variables are rarely assessed in childhood obesity treatment studies, especially as predictors of outcomes. Yet, they likely exert great influence on health behaviors of the family. Most research has centered on constructs of parenting.15 Family functioning (FST-pertinent variable) is mistakenly combined with concepts of parenting,19 however, family functioning is distinctively different from parenting. Previous reviews conducted on parenting style and obesity40-42 have connected aspects of the parent-child dynamic (ie, parenting style, parenting behavior, parenting practices) and obesity, but have not captured family dynamics, which extends beyond the parent-child interaction to the entire family and other specific relationships (sibling, couple, etc). Despite the existence of FST-based studies, most of these studies have still relied on assessments of the constructs of parenting, likely because of the ease in measurement, in which consistently impaired parenting styles are associated with youth obesity.31,40-42 Specifically, an authoritative parenting style is associated with lower weight status in youth and healthier behaviors.31 Unfortunately, associations between parenting and the overall family dynamic have not been explored with respect to childhood obesity. Capturing the reciprocal nature of parenting and family dynamics would provide important data to consider for family-based treatment, and interest in this area continues to grow.43
Family Functioning and Relationship to Childhood Obesity
Although less frequently assessed in childhood obesity treatment, family functioning is also associated with youth obesity.44-46 The most comprehensive review to date found 17 studies that assessed the relationship between family functioning and youth overweight/obesity.19 Twelve noted significant associations between impaired family functioning, risk of developing overweight/obesity, and current overweight/obesity in youth. Recently, Zeller and colleagues assessed family functioning among adolescents undergoing weight loss surgery.20 Impaired family functioning was prevalent in a third to a half of families; better family functioning was positively correlated with adolescent weight loss 1-year post-surgery. Haines and colleagues reported that patients with higher family functioning and positive family relationships had healthier weight-related behaviors.46 Although the evidence suggests that assessing family functioning in childhood obesity clinical encounters is warranted, there is essentially no information about how family functioning might change over the course of treatment, nor have these studies evaluated the effect of intervening on family functioning.
Family Organization Around Weight-Related Behaviors
According to FST, families organize around the routines, rules, and dynamics that are established over time. This organization becomes the way the family operates, and can either promote healthy or impaired family functioning. Families might have healthy functioning with respect to weight-related behaviors, such as having leisure-time activities that are physically active. Conversely, families can also have impaired functioning, such as frequently eating fast food with little to no meal planning, preparation, or quality time conversing during a meal. By using FST to inform childhood obesity treatment, 2 types of family patterns might emerge—families that organize around unhealthy weight-related behaviors that lead to obesity, or around healthy weight-related behaviors that assist the family in maintaining a healthy weight. This way of viewing organization around weight-related behaviors (heathy or unhealthy) can assist providers in tailoring their encounters to focus on family dynamics that support healthy behaviors, and modify those organized around unhealthy behaviors. Table 2 provides examples of family organization around behaviors that might contribute to obesity.
Table 2.
Characteristics of Families’ Organization Around Healthy and Unhealthy WRB
| Characteristic | Unhealthy WRB | Healthy WRB |
|---|---|---|
| Food preparation | Individually done | Family-wide participation |
| Limited family participation | ||
| Family meals | Limited | Frequent |
| Unscheduled | Scheduled | |
| Meals away from home | Frequent | Limited |
| Physical activity | Limited family participation | Family-wide participation |
| Individually done | ||
| Screen time | No/limited rules for use | Clear rules and limits for use |
| Messages communicated | Shape, size, weight | Health |
| Sleep | No/limited routine, rules | Clear routine, rules |
WRB indicates weight-related behaviors.
Families that organize around healthy as well as unhealthy weight-related behaviors might be particularly receptive to first-order change through FBBT interventions, because they might have some positive established rules, routines, and communication that could be extended to address unhealthy weight-related behaviors. These families might only need to change 1 or 2 specific behaviors, not their overall family dynamic. Conversely, families who predominantly organize around unhealthy weight-related behaviors are unlikely to have implicit rules that support health, established routines, and overall family dynamics that support changing unhealthy behaviors to healthy ones. They might benefit from second-order change through FST interventions, in which the family changes the way they operate through higher-level changes around family rules, routines, and dynamics. It is hypothesized that families who are organized around healthy behaviors tend to have established rules and routines and positive communication, whereas those who organize around unhealthy behaviors might lack those traits.
In short, FST-informed interventions should be designed, conducted, and evaluated for their short- and long-term effectiveness in childhood obesity treatment. Implementation of FST within primary- and tertiary-care programs is likely to be a challenge, with unknown acceptability by families and clinicians alike. Additionally, assessments should measure variables representative of FST (family functioning) across treatment to determine which variables should be targeted (as strengths as well as growth areas) in future interventions. Finally, and arguably most relevant for treatment, providers who view youth with obesity in the context of his/her family need to know how to counsel families who organize around healthy or unhealthy weight-related behaviors, and how to incorporate components of FST into their encounters. The authors of this report recently assessed family functioning in a sample of youth (ages 2–18 years) and parents (N = 329) in pediatric primary care to assess for associations between reports of family functioning and youth weight status; parents who reported impaired family functioning also reported that their youth had a higher BMI z-score compared with families who reported healthy family functioning (Pratt et al, unpublished data, November 2017). Future research should seek to: 1) assess family functioning among youth in pediatric weight management programs, 2) assess for changes in family functioning throughout treatment, 3) assess how changes in family functioning correlate with changes in weight-related behaviors and weight status, 4) determine if family functioning can predict youth and family members’ behavior change and weight loss, and 5) compare family functioning between families in pediatric weight management programs and non-treatment-seeking families with youth with obesity. Additionally, future feasibility and acceptability studies, particularly performed with a diverse group of families, are essential to ensure that future targets (like family functioning) are received well by youth and families.
A Template for FST-Informed Assessment in Childhood Obesity Treatment and Research
Figure 1 depicts a suggested algorithm for use of FST, either in exploratory clinical or research settings. This algorithm might help determine: 1) how families organize around healthy or unhealthy weight-related behaviors, 2) which family-based approach (FST, FBBT) might be advantageous for treatment, and 3) family-based evaluation and re-methods to monitor progress. This framework should undergo further testing and refinement to determine its fit with youth and families in childhood obesity treatment. At a minimum, it provides a starting point to consider the utility of FST in obesity treatment programs, and for providers to view children’s weight status and weight-related behaviors within the context of the family system.
Figure 1.
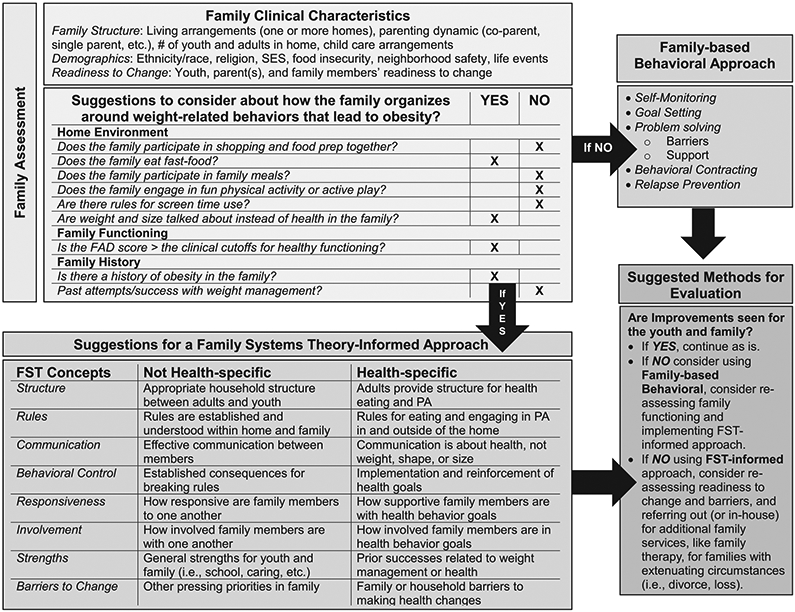
Suggested algorithm for use of FST in family-based obesity treatment. FST indicates family systems theory; SES, socioeconomic status; FAD, Family Assessment Device; and PA, physical activity.
Family Clinical Characteristics
The first step in providing family-based care using a FST framework is not just to situate the youth within the family context as previously suggested,5 but to view the “family as the patient.” This shift allows providers to assess clinical outcomes inclusive of the entire family. Thus, all family members who are willing and able should be invited to attend before the initial visit, or steps should be taken to incorporate them. At the initial visit, the team should describe their approach to family-based care: “You will meet with multiple members of our team today who are going to get to know your family, and your food and activity habits.” This example situates the family as the patient and does not target the youth and/or parent as having “a problem.”
Family history should include where the youth in treatment spends most of her time, including shared custody or childcare arrangements. Details of the family structure should include the parenting arrangements, and how many youth and adults live in the home. This helps providers determine who can support and assist the youth with goals, and if information needs to be communicated to additional family members not present in clinic. Aspects of the family’s culture should be assessed, including cultural and religious/spiritual celebrations that involve food or activity. Last, asking about recent life events (separation/divorce, death/loss, employment) will help determine the relevant needs of the family and how treatment can be tailored to their unique circumstances.
How Does the Family Organize Around Healthy or Unhealthy Weight-Related Behaviors?
Figure 1 provides a suggested template to assess family organization around weight-related behaviors that lead to obesity. Additionally, family history of obesity and previous attempts at weight loss, successful as well as unsuccessful, should be noted, along with any insights into the success and/or failures of past attempts. A genogram (Fig. 2) can be a valuable tool in this process.
Figure 2.
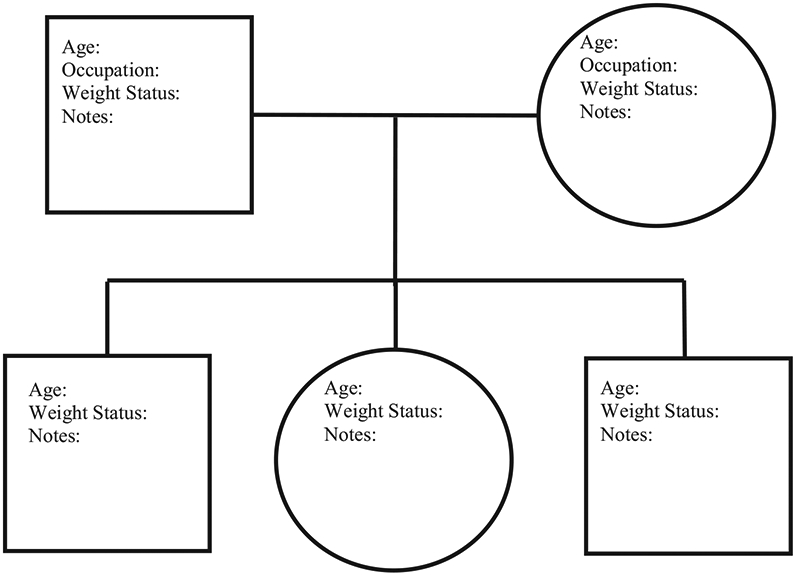
Family systems theory genogram.
Family Functioning
Because of the prevalence of impaired family functioning among families of youth with obesity,19,20,46 assessing family functioning through standardized questionnaires aids providers in determining strengths and growth areas in the family. Researchers have used the McMaster Family Assessment Device (FAD),47 the Family Adaptability and Cohesion Evaluation Scale,48 and the Family Environment Scale.49 The FAD is the most commonly used; it has 60 items and 7 scales that assess family functioning on a Likert scale of 1 to 4,47 with each scale having clinical cutoff scores.50 Examples of questions from each scale are as follows. For problem-solving: “After our family tries to solve a problem, we usually discuss whether it worked or not.”; communication: “When someone is upset the others know why.”; roles: “We make sure members meet their family responsibilities.”; affective responsiveness: “We are reluctant to show affection to each other.”; affective involvement: “You only get the interest of others when something is important to them.”; behavior control: “We have rules about hitting people.”; and general functioning: “In times of crisis we can turn to each other for support.” In the past, researchers have consistently reported α ≥ .70,49 including youth with obesity.19,20,47,51,52 The 7 scales have maintained internal consistency within Hispanic and African American families.52
The 12-item FAD General Functioning scale is an acceptable proxy for overall family functioning,52 and has been used to assess family dynamics in weight management populations.51,53 The FAD or the FAD General Functioning scale can be used to determine if families are above or below the cutoff score(s) for healthy functioning, and what areas might be a strength (ie, communication) or that are more vulnerable (ie, rules).
Assessing family organization around weight-related behaviors and family functioning could determine if families should receive FBBT or FST-informed interventions. FBBT is likely more effective for families who do not organize extensively around unhealthy weight-related behaviors and have areas of healthy family functioning, and has been extensively described elsewhere.10
FST-Informed Approach
Depending on the FAD results, specific components of FST to target in treatment could include family structure and boundaries, behavioral control, communication, rules, family involvement, and family responsiveness. Families with impaired family functioning might be best served by improvements in general family functioning first, because prioritizing weight-related goals might not be successful long-term in families not supportive of change. In other words, it will be more difficult for families with impaired family functioning to change their weight-related behaviors, particularly if these behaviors are a part of their routine, such as watching television every night during dinner to avoid having conflictual conversations.
Family structure refers to having an appropriate hierarchy or boundary between the adult and youth subsystems. Boundaries should allow outside members to come into the family as needed for support or friendship, but should not be rigid to the point at which the family might become isolated, or too flexible where the household is chaotic. Families with healthy boundaries and structure presenting for childhood obesity treatment likely have adults who take responsibility for providing healthy meals and opportunities for physical activity. In families without healthy boundaries and structure, the youth might have the “power” in the family or have chaotic organization. If so, treatment might focus on supporting the caregiver(s) to assume an authoritative parenting role, and extending those practices to weight-related behaviors such as food preparation and providing opportunities for activity.
In families with healthy functioning, rules around weight-related behaviors might be implicit; the provider can explore these rules. For example, an explicit rule in families is that they have to finish the food on their plate before having dessert. Whereas an implicit rule might be that youth know if they ask their father for a snack he will say yes, rather than their mother who will say no. In childhood obesity treatment, it is important to find effective ways to communicate families’ implicit rules around eating and physical activity explicitly, to determine how these rules can change to support a healthy lifestyle. For families with healthy family functioning, FST might not be necessary if only changes in select health behaviors are needed (first-order change), which can be accomplished through FBBT. However, if families have healthy family functioning and multiple health behaviors need to be addressed, FST could be used to ensure that changing multiple behaviors does not have undesirable effects on family functioning (second-order change). A universal challenge is long-term maintenance of changes in behaviors and weight status; it might be that FST is required to sustain successful long-term change in families, rather than individuals.
When communication is impaired in families, teaching basic skills like “I-statements”54 can help family members effectively listen to each other without eliciting defensiveness or blaming. Instead of saying “You’re not being social when you eat in your room by yourself,” the parent could say, “I miss eating dinner with you. I want to hear about your day.” Family members can practice listening and reflecting back statements and feelings, rather than responding immediately. Family weight talk (body weight and shape, not health) and teasing are developing areas of research, especially among couple and parent-youth dyads.55,56 When determining treatment goals, clarity on how youth and parents communicate with each other is often needed. For example, youth might believe their parents are nagging them about their goals, when parents feel they are supporting their children’s efforts. To foster healthy communication around treatment goals, providers can ask the youth and family members to determine acceptable ways to reinforce goals in the home that are not perceived negatively. For example, parents and youth could agree that the parents might remind a youth once (but not twice) to wait until everyone is served dinner before taking a second helping.
Family responsiveness is how receptive family members are to one each other’s needs. In treatment this includes how willing family members are to participate in weight-related goals with youth. Family involvement is how much family members take part in each other’s life or how involved they are with each other. It is possible for family members to participate in health-related goals, but not be responsive to the youth’s needs. For example, a sibling might participate in weekly walks with the youth in treatment, but he or she might not be responsive to feedback that they are walking too fast.
Evaluation
In childhood obesity treatment, success is determined by youth behavior change and ultimately, weight loss. According to FST, success involves changing the family dynamics so that successful behavioral change can take place. If families are not successful with FBBT, determined according to clinical (absence of weight loss) or behavioral measures (sustained unhealthy behaviors) providers should consider reevaluating family functioning. If families receiving FST-informed treatment improve their family dynamics or functioning, and potentially achieve behavior change, then behavioral aspects can be incorporated into treatment. Because changes in family functioning are expected to have a “downstream effect” resulting in changes to weight-related behaviors, changes in weight status might be slower than what is expected or experienced in traditional FBBT. This is an important consideration for future research, particularly in testing the hypothesis that second-order change is needed for long-term behavior and weight change in families. Subsequently, providers will need to address the family’s expectation for youth weight loss, particularly in noting that improvements in family functioning might be necessary before improvements in youth weight status are expected. In addition, aspects of family functioning and associations with weight-related behaviors and weight status over treatment must be captured. In other words, a research priority is to identify the key aspects of family functioning and dynamics that improve youth weight status to lead to more focused family-based treatment. For example, communication might be a key element of family functioning that predicts adolescents’ weight-related behavior change, whereas family rules might not. If families are not improving their overall dynamic, then family functioning should be reassessed to determine areas needing attention, including recent life events that might warrant prioritizing (separation, job loss). If family members require more intensive therapeutic work around recent life events or stressors, referrals to family therapy can be made.
Conclusions
On the basis of the limited research that indicates impairments in family functioning among families of youth with obesity, future research needs to use assessments grounded in FST. Additionally, determining how families organize around weight-related behaviors might allow providers to tailor treatment on the basis of the needs of the family. The family-based clinical algorithm provides a framework for future testing and exploration. Details on costs and delivery of FST services also need to be further explored.
What’s New.
This report explores family functioning around weight-related behaviors that might contribute to obesity, and if different treatment approaches might be beneficial for families: family systems theory-informed or family-based behavioral interventions. A family-based clinical algorithm detailing how family systems theory could be used in the assessment and study of childhood obesity is provided.
Acknowledgments
We acknowledge the editorial assistance of Karen Klein, MA, in the Wake Forest Clinical and Translational Science Institute (UL1 TR001420; PI: McClain).
Footnotes
The authors have no conflicts of interest to disclose.
Contributor Information
Keeley J. Pratt, Department of Human Sciences, Human Development and Family Science Program, College of Education and Human Ecology, The Ohio State University, Columbus, Ohio; Department of Surgery, The Ohio State University Wexner Medical Center, Columbus, Ohio.
Joseph A. Skelton, Department of Pediatrics, Wake Forest School of Medicine, Winston-Salem, NC; Brenner FIT (Families In Training) Program, Brenner Children’s Hospital, Wake Forest Baptist Health, Winston-Salem, NC; Department of Epidemiology and Prevention, Wake Forest School of Medicine, Winston-Salem, NC.
REFERENCES
- 1.Ogden C, Carrol M, Flegal K. Prevalence of child and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitaker R, Wright J, Pepe M, et al. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. [DOI] [PubMed] [Google Scholar]
- 3.Watson PM, Dugdill L, Pickering K, et al. A whole family approach to childhood obesity management (GOALS): relationship between adult and child BMI change. Ann Hum Biol. 2011;38:445–452. [DOI] [PubMed] [Google Scholar]
- 4.Boutelle KN, Cafri G, Crow SJ. Parent-only treatment for childhood obesity: a randomized controlled trial. Obesity (Silver Spring). 2011;19:574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barlow SE, Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192. [DOI] [PubMed] [Google Scholar]
- 6.Eneli I, Norwood V, Hampl S, et al. Perspectives on obesity programs at children’s hospitals: insights from senior program administrators. Pediatrics. 2011;128(suppl 2):S86–S90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berge JM, Everts JC. Family-based interventions targeting childhood obesity: a meta-analysis. Child Obes. 2011;7:110–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Epstein LH, Valoski A, Wing RR, et al. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994;13:373. [DOI] [PubMed] [Google Scholar]
- 9.Epstein LH, Paluch RA, Gordy CC, et al. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154:220–226. [DOI] [PubMed] [Google Scholar]
- 10.Epstein LH, Roemmich JN, Raynor HA. Behavioral therapy in the treatment of pediatric obesity. Pediatr Clin North Am. 2001;48:981–993. [DOI] [PubMed] [Google Scholar]
- 11.Golan M, Crow S. Targeting parents exclusively in the treatment of childhood obesity: long-term results. Obes Res. 2004;12:357–361. [DOI] [PubMed] [Google Scholar]
- 12.Golan M, Weizman A. Familial approach to the treatment of childhood obesity: conceptual mode. J Nutr Educ. 2001;33:102–107. [DOI] [PubMed] [Google Scholar]
- 13.White JM, Klein DM. The Systems Framework. Family Theories. 3rd ed. Thousand Oaks, CA: Sage Publications; 2008:151–177. [Google Scholar]
- 14.Bertalanffy LV. Theoretical models in biology and psychology. In: Krech D, Klein GS, eds. Theoretical Models and Personality Theory. Durham, NC: Duke University Press; 1952:24–38. [Google Scholar]
- 15.Kitzman-Ulrich H, Wilson DK, George SM St, et al. The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clin Child Fam Psychol Rev. 2010;13:231–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bishop J, Irby MB, Skelton JA. Family perceptions of a family-based pediatric obesity treatment program. Infant Child Adolesc Nutr. 2015;7:278–286. [Google Scholar]
- 17.Skelton JA, Buehler C, Irby MB, et al. Where are the family theories in family-based obesity treatment? Conceptualizing the study of families in pediatric weight management. Int J Obes. 2012;36:891–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan SG, Arnold EM, Irby MB, et al. Family systems theory and obesity treatment: application for clinicians. Infant Child Adolesc Nutr. 2014;6:24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Halliday JA, Palma CL, Mellor D, et al. The relationship between family functioning and child and adolescent overweight and obesity: a systematic review. Int J Obes. 2014;38:480–493. [DOI] [PubMed] [Google Scholar]
- 20.Zeller MH, Hunsaker S, Mikhail C, et al. Family factors that characterize adolescents with obesity and their role in weight loss surgery outcomes. Obesity (Silver Spring). 2016;24:2562–2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slesnick N, Zhang J. Family systems therapy for substance-using mothers and their 8- to 16-year-old children. Psychol Addict Behav. 2016;30:619–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gray WN, Janicke DM, Fennell EB, et al. Piloting behavioral family systems therapy to improve adherence among adolescents with HIV: a case series intervention study. J Health Psychol. 2011;16:828–842. [DOI] [PubMed] [Google Scholar]
- 23.Riley AR, Duke DC, Freeman KA, et al. Depressive symptoms in a trial behavioral family systems therapy for diabetes: a post hoc analysis of change. Diabetes Care. 2015;38:1435–1440. [DOI] [PubMed] [Google Scholar]
- 24.Harris MA, Freeman KA, Beers M. Family therapy for adolescents with poorly controlled diabetes: initial test of clinical significance. J Pediatr Psychol 2009;34:1097–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wysocki T, Harris MA, Buckloh LM, et al. Randomized, controlled trial of Behavioral Family Systems Therapy for Diabetes: maintenance and generalization of effects on parent-adolescent communication. Behav Ther. 2008;39:33–46. [DOI] [PubMed] [Google Scholar]
- 26.Fisher EB, Thorpe CT, Devellis BM, et al. Healthy coping, negative emotions, and diabetes management: a systematic review and appraisal. Diabetes Educ. 2007;33:1080–1103. [DOI] [PubMed] [Google Scholar]
- 27.Sung-Chan P, Sung YW, Zhao X, et al. Family-based models for childhood-obesity intervention: a systematic review of randomized controlled trials. Obes Rev. 2013;14:265–278. [DOI] [PubMed] [Google Scholar]
- 28.Diamond G, Siqueland L. Current status of family intervention science. Child Adolesc Psychiatr Clin N Am. 2001;10:641–661. [PubMed] [Google Scholar]
- 29.Liddle HA. Advances in family-based therapy for adolescent substance abuse: findings from the multidimensional family therapy research program. NIDA Res Monogr. 2002;182:395–422. [Google Scholar]
- 30.Minuchin S, Rosmn BL, Baker L. Psychosomatic Families: Anorexia Nervosa in Context. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- 31.Berge JM. A review of familial correlates of child and adolescent obesity: what has the 21st Century Taught us so Far? Int J Adolesc Med Health. 2009;21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Watzlawick P, Weakland JH, Fisch R. Change: Principles of Problem Formation and Problem Resolution. New York: Norton; 1974. [Google Scholar]
- 33.Flodmark CE, Ohlsson T, Ryden O, et al. Prevention of progression to severe obesity in a group of obese schoolchildren treated with family therapy. Pediatrics. 1993;91:880–884. [PubMed] [Google Scholar]
- 34.Kitzman-Ulrich H, Hampson R, Wilson DK, et al. An adolescent weight-loss program integrating family variables reduces energy intake. J Am Diet Assoc. 2009;109:491–96. [DOI] [PubMed] [Google Scholar]
- 35.Irby M, Kaplan S, Garner-Edwards D, et al. Motivational interviewing in a family-based pediatric obesity program: a case study. Fam Syst Health. 2010;28:236–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: conceptual issues and evidence review. J Am Diet Assoc. 2006;106:2024–2033. [DOI] [PubMed] [Google Scholar]
- 37.Berg IK. Family-Based Services: A Solution-Focused Approach. New York, NY: WW Norton & Co; 1994. [Google Scholar]
- 38.McCallum Z, Wake M, Gerner B, et al. Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int J Obes. 2007;31:630–636. [DOI] [PubMed] [Google Scholar]
- 39.Kreier F, Genco SM, Boreel M, et al. An individual, community-based treatment for obese children and their families: the solution-focused approach. Obes Facts. 2013;6:424–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sleddens EF, Gerards SM, Thijs C, et al. General parenting, child overweight, and obesity-inducing behaviors: a review. Int J Pediatr Obes. 2011;6:e12–e27. [DOI] [PubMed] [Google Scholar]
- 41.Kitzman KM, Beech BM. Family-based interventions for pediatric obesity: methodological and conceptual challenges from family psychology. Couple Family Psychol. 2011;1:45–62. [DOI] [PubMed] [Google Scholar]
- 42.Norwicka P, Flodmark CE. Family in pediatric obesity management: a literature review. Int J Pediatr Obes. 2008;3:44–50. [DOI] [PubMed] [Google Scholar]
- 43.Baronwski T, O’Conner T, Hughes S, et al. Houston … We have a problem! Measurement of parenting. Child Obes. 2013;9:S1–S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wen LM, Simpson JM, Baur LA, et al. Family functioning and obesity risk behaviors: implications for early obesity intervention. Obesity (Silver Spring). 2011;19:1252–1258. [DOI] [PubMed] [Google Scholar]
- 45.Moens E, Braet C, Soetens B. Observation of family functioning at mealtime. A comparison between families of children with and without overweight. J Pediatr Psychol. 2007;32:52–63. [DOI] [PubMed] [Google Scholar]
- 46.Haines J, Rifas-Shiman SL, Horton NJ, et al. Family functioning and quality of parent-adolescent relationship: cross-sectional associations with adolescent weight-related behaviors and weight status. Int J Behav Nutr Phys Act. 2016;13:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Epstein NB, Bishop DS, Levin S. The McMaster model of family functioning. J Martial Fam Ther. 1978;4:19–31. [Google Scholar]
- 48.Olson D. Faces IV and the circumplex model: validation study. J Martial Fam Ther. 2011;3:64–80. [DOI] [PubMed] [Google Scholar]
- 49.Moos R, Moos B. Family Environment Scale Manual: Development, Applications, Research. Third ed. Palo Alto, CA: Consulting Psychologist Press; 1994. [Google Scholar]
- 50.Ryan CE, Epstein NB, Keitner GI. Evaluating and Treating Families: The McMaster Approach. New York, NY: Taylor & Francis; 2005. [Google Scholar]
- 51.Berge JM, Wall M, Larson N, et al. Family functioning: associations with weight status, eating behaviors, and physical activity in adolescents. J Adolesc Health. 2013;52:351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mansfield AK, Keitner GI, Dealy J. The family assessment device: an update. Fam Process. 2015;54:82–93. [DOI] [PubMed] [Google Scholar]
- 53.Pratt K, Ferriby M, Noria S,et al. Perceived child weight status, family structure and functioning, and support for health behaviors in bariatric surgery patients [published online ahead of print January 29, 2018]. Fam Syst Health. doi: 10.1037/fsh0000317. [DOI] [PubMed] [Google Scholar]
- 54.Burr WR. Beyond I-Statements in family communication. Fam Relations. 1990;39:266–273. [Google Scholar]
- 55.Berge JM, Pratt K, Miller L. Weight talk and weight teasing in romantic relationships: what do they sound like and how do partners respond? Fam Syst Health. 2016;34:213–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berge JM, Hanson-Bradley C, Tate A, et al. Do parents or siblings engage in more negative weight-based talk with children and what does it sound like? A mixed-methods study. Body Image. 2016;18:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]


