Abstract
Objectives:
To compare achieved and predicted tooth movements of maxillary first molars and central incisors in first premolar extraction cases treated with Invisalign.
Materials and Methods:
The present study included 30 patients who received maxillary first premolar extraction treatment with Invisalign. The actual posttreatment model was registered with the pretreatment model on the palatal stable region and superimposed with the virtual posttreatment model. Achieved and predicted tooth movements of maxillary first molars and central incisors were compared using paired t-test. Linear mixed-effect model analyses were used to explore the influence of age (adolescents vs adults), attachment (G6-optimized vs 3-mm vertical, 3-mm horizontal, and 5-mm horizontal), and initial crowding on the differences between predicted and achieved tooth movement (DPATM).
Results:
First molars achieved greater mesial tipping, mesial translation, and intrusion than predicted. Central incisors achieved less retraction and greater lingual crown torque and extrusion than predicted. Adolescents showed greater DPATM in the mesiodistal translation of first molars and labiolingual translation of central incisors and smaller DPATM in the occlusogingival translation of the first molars and crown torque of the central incisors than adults. The 3-mm vertical attachment group showed greater DPATM in the mesiodistal translation of the first molars vs the G6-optimized attachment group. Initial crowding had an inverse correlation with DPATM in angulation and mesiodistal translation of the first molars.
Conclusions:
First molar anchorage control and central incisor retraction were not fully achieved as predicted in first premolar extraction treatment with Invisalign. Age, attachment, and initial crowding affected the differences between predicted and achieved tooth movement.
Keywords: Invisalign, Extraction treatment, Tooth movement
INTRODUCTION
Since the introduction of Invisalign as an esthetic alternative to fixed labial braces for orthodontic treatment, orthodontists have been concerned about the efficacy of tooth movement with Invisalign. By comparing virtual models of achieved and predicted tooth positions, Kravitz et al.1 evaluated the efficacy of expansion, constriction, intrusion, extrusion, mesiodistal tip, labiolingual tip, and rotation in anterior teeth. Similarly, Simon et al.2 evaluated the efficacy of incisor torque, premolar derotation, and molar distalization. Grünheid et al.3 evaluated the accuracy of tooth movement for each tooth type in the mesial-distal, facial-lingual, and occlusal-gingival directions as well as for tip, torque, and rotation in nonextraction cases. However, the accuracy of Invisalign in extraction cases has not been explored.
Both molar anchorage control and incisor torque control are extremely vital during space closure for extraction orthodontic treatment. One advantage of Invisalign for extraction treatment is that orthodontists can design molar anchorage and incisor torque control by using the ClinCheck program (Align Technology Inc, Santa Clara, Calif). They design how much of the extraction space should be used to displace molars forward, relieve crowding, and retract anterior teeth, and they set molar angulation and incisor torque according to treatment goals. Nevertheless, actual anchorage control may not be achieved as planned. Baldwin et al.4 evaluated the movement of teeth adjacent to premolar extraction spaces during space closure and found significant tipping, with a mean change in interdental angle of >17° as measured on models and panoramic radiographs. In another study, loss of incisor torque was observed in almost 50% of cases, even when torque control was supported with horizontal ellipsoid attachments or power ridges.2
In 2015, Align Technology proposed the G6 protocol by using SmartForce (optimized anchorage attachment on posterior teeth and optimized retraction attachment on the canine) and SmartStage (optimized tooth movement stage) to achieve maximum anchorage control with a mesial translation of ≤2 mm in molars. However, the actual effectiveness of this protocol has not been explored. In addition, anchorage loss is a multifactorial response in fixed orthodontic treatment,5 and whether these previously identified factors have similar effects on anchorage control in clear aligner treatment remains unknown.
Thus, the present study aimed to evaluate the actual movement of maxillary first molars and central incisors during space closure in first premolar extraction cases with Invisalign, compare it with predicted tooth movement, and explore the effects of age, attachment, and crowding on molar anchorage control.
MATERIALS AND METHODS
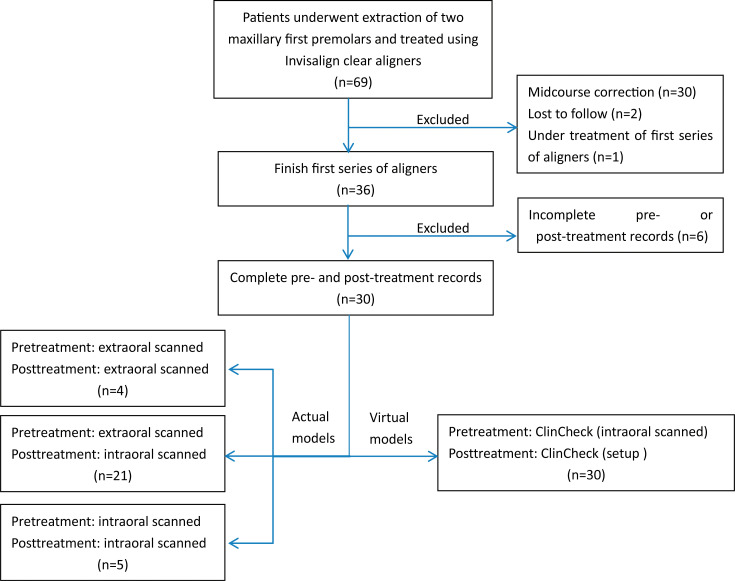
Among patients who started orthodontic treatment at the Second Dental Center, Peking University School and Hospital of Stomatology, from January 2014 to December 2016, 30 patients (4 males, 26 females; age 19.4 ± 6.3 years) who underwent extraction of two maxillary first premolars, were treated using Invisalign clear aligners, and had finished the first series of aligners were included. Inclusion criteria were (1) no missing permanent maxillary teeth before treatment (except third molars), (2) the first series of aligners were finished without midcourse correction, (3) no combined treatment with fixed appliances or other auxiliary appliances, and (4) complete records of pre- and posttreatment dental models. The sampling flow chart is shown in Figure 1. All patients changed aligners every 1–2 weeks following the manufacturer's protocol. The average treatment time for wearing the first series of aligners was 22.3 ± 4.6 months. Nine patients used Class II elastics. Of the 30 patients, 15 had Class I, 11 had Class II, and 4 had Class III molar occlusions (all <2 mm). The protocol for this retrospective study was approved by the institutional review board at the Peking University School and Hospital of Stomatology (No. PKUSSIRB-201630093).
Figure 1.
The sampling flow chart.
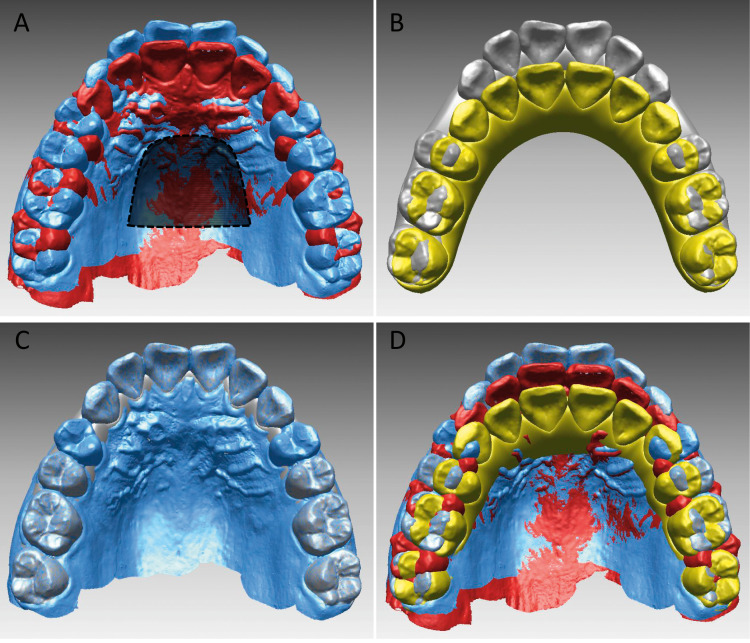
Actual pre- and posttreatment digital models were acquired using two methods. The first method was to record alginate impressions, pour them into plaster casts, and digitize the casts by using an R700 orthodontic model scanner (3Shape A/S, Copenhagen, Denmark). The second method was intraoral scanning using iTero (Align Technology Inc). Most pretreatment digital models were obtained using the first method, and most posttreatment digital models were obtained using the second method (as intraoral scanning of both dental arches and palatal soft tissues was implemented since July 2016). By using the Rapidform 2007 software, actual pre- and posttreatment maxillary digital models were superimposed based on the palatal vault region, which was validated to be relatively stable (Figure 2A).6
Figure 2.
Superimposition of pre- and posttreatment models. (A) Registration of actual pre- (blue) and posttreatment (red) models on the palatal stable region (dotted line). (B) Virtual pre- (gray) and posttreatment (yellow) models from ClinCheck. (C) Registration of actual and virtual pretreatment models on the dental arch. (D) Final superimposition of all four models.
The virtual pretreatment model for treatment planning created using Align Technology's ClinCheck program was obtained by intraoral scanning with iTero. The virtual pretreatment model and the final-stage model of each patient's virtual treatment plan were exported as STL files and imported into the Rapidform software as virtual pretreatment and posttreatment models (Figure 2B).
Virtual and actual pretreatment models had the same dental arches, on which the virtual and actual pretreatment models were registered and final superimposition of all four models was achieved (Figure 2C,D).
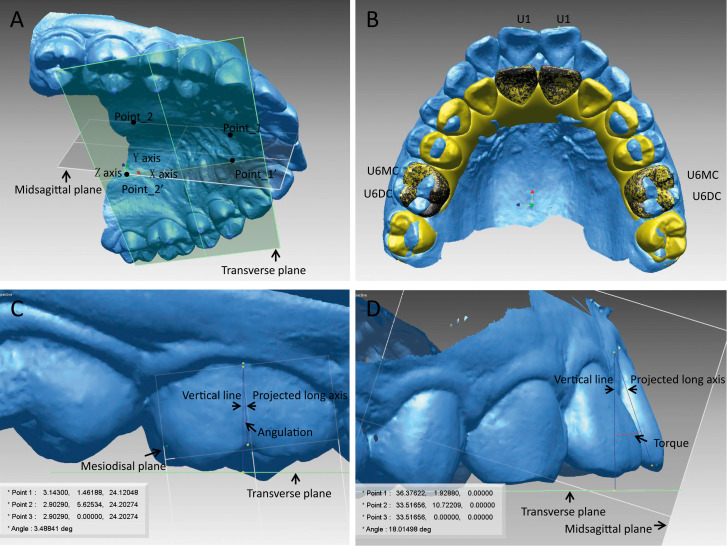
After superimposition, a three-dimensional (3D) coordinate system was generated for tooth movement measurements. In the pretreatment model, cusps of bilateral maxillary first molars, second premolars, and first premolars were used to fit the mutual transverse plane. Two points (point_1: at the level of first rugae; point_2: at the level of the distal surface of first molar) were located on the palatal suture and projected onto the transverse plane, generating another two points (point_1′ and point_2′); these four points were used to fit the midsagittal plane. The coordinate system was set up with point_2′ as the original point, point_1′ directed to the X axis, and point_2 directed to the Y axis (Figure 3A).
Figure 3.
Tooth movement measurements. (A) Three-dimensional coordinate system. (B) The U6MC, U6DC, and U1 points for measurement of tooth translation were transferred from pretreatment to posttreatment models through tooth crown surface superimposition. (C) Measurement of first molar angulation. (D) Measurement of central incisor torque.
Mesial and distal buccal cusps of the maxillary first molars (U6MC and U6DC) and the midpoint of the edge of central incisors (U1) were located on the pretreatment model and transferred onto actual and virtual posttreatment models through tooth crown surface superimposition (Figure 3B). Anteroposterior translation along the X axis and occlusal-gingival translation along the Y axis of points U6MC, U6DC, and U1 were then measured to evaluate achieved and predicted sagittal translation of maxillary first molars and central incisors.
For first molar angulation (U6_Angulation), the most mesial and distal edge points along the occlusal central groove and their projected points onto the transverse plane determined the mesiodistal plane of the tooth. The long axis of the first molar crown, generated by connecting the most occlusal and gingival points along the buccal groove, was projected onto the mesiodistal plane, and the angle between the projected line with the vertical line perpendicular to the transverse plane was defined as first molar angulation (Figure 3C). For central incisor crown torque (U1_Torque), the long axis of the central incisor crown, generated by connecting the most occlusal and gingival points along the midline of the buccal surface, was projected onto the midsagittal plane, and the angle between the projected line with the vertical line perpendicular to the transverse plane was defined as central incisor crown torque (Figure 3D). In addition, reference points were transferred onto actual and virtual posttreatment models through tooth crown surface superimposition, and first molar angulation and central incisor torque were measured again. Subsequently, achieved and predicted changes in first molar angulation and central incisor torque were calculated.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics for Windows (version 19.0; IBM, Armonk, NY). Superimposition of actual pre- and posttreatment models and measurements were repeated twice by a single operator. Intraoperator agreement was evaluated using Pearson's correlation coefficients and Bland-Altman analyses. Relationships between predicted and achieved changes were described using scatter diagrams and linear regression analyses. The paired t-test was used to compare predicted and achieved changes. Linear mixed-effect model analyses were used to explore the influence of predicted tooth movement, age, attachment, and initial crowding on the differences between predicted and achieved tooth movement (DPATM). Age (1 = adolescent, 2 = adult) and attachment (1 = 3-mm vertical, 2 = 3-mm horizontal, 3 = 5-mm horizontal, 4 = G6-optimized) were coded. Predicted tooth movement and initial crowding were used as covariates. Bilateral measurements were pooled to obtain a doubled sample (n = 60). Side differences and interaction effect of variables were not found in the linear mixed-effect model and were hence deleted. A P value <.05 was considered statistically significant.
RESULTS
In general, Pearson's correlation coefficients and results of Bland-Altman analyses showed high intraoperator agreement for all measurements (Table 1).
Table 1.
Pearson's Correlation Coefficients (r) and Results of Bland-Altman Analyses for Intraoperator Agreementa
| Measurement |
r |
Mean Difference |
Limits of Agreement |
| U6_Angulation, ° | 0.994 | 0.0060 | −0.9843, 0.9963 |
| U6MC_MDT, mm | 0.983 | −0.0228 | −0.5065, 0.4609 |
| U6DC_MDT, mm | 0.984 | −0.0213 | −0.5175, 0.4749 |
| U6MC_OGT, mm | 0.975 | 0.0130 | −0.3717, 0.3977 |
| U6DC_ OGT, mm | 0.972 | 0.0110 | −0.3939, 0.4159 |
| U1_Torque, ° | 0.998 | 0.0088 | −0.9904, 1.0080 |
| U1_LLT, mm | 0.997 | −0.0225 | −0.2761, 0.2311 |
| U1_OGT, mm | 0.977 | 0.0143 | −0.4257, 0.4543 |
U6MC indicates mesial buccal cusp of upper first molar; U6DC, distal buccal cusp of upper first molar; MDT, mesiodistal translation; LLT, labiolingual translation; OGT, occlusogingival translation.
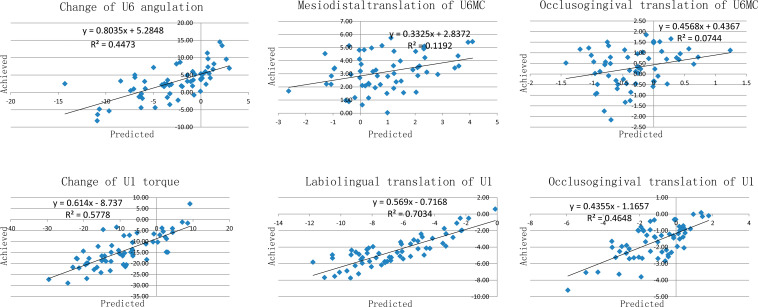
Table 2 summarizes differences between predicted and achieved tooth movements. First molars were predicted to tip distally but actually tipped mesially, with a difference of 5.86° ± 3.51°, and translated mesially more than predicted by 2.26 ± 1.58 mm as indicated by the mesial buccal cusp, and 2.31 ± 1.67 mm as indicated by the distal buccal cusp. Occlusogingivally, the distal buccal cusp was relatively stable, and the mesial buccal cusp intruded more than predicted by 0.61 ± 0.89 mm. Central incisors tipped more lingually by 5.16° ± 5.92°, retracted less by 2.12 ± 1.51 mm, and extruded more by 0.50 ± 1.17 mm relative to predicted changes. Pearson's correlation coefficients revealed a weak to high correlation between achieved and predicted tooth movement; the relationships are also described using a scatter diagram and a linear regression equation (Figure 4).
Table 2.
Comparison of Predicted and Achieved Tooth Movement and Pearson's Correlation Coefficients (r; n = 60)a
| Measurement |
Predicted |
Achieved |
Difference |
P Valueb |
r |
P Valuec |
| U6_Angulation, ° | −2.94 ± 3.84 | 2.92 ± 4.62 | 5.86 ± 3.51 | .000 | .669 | .000 |
| U6MC_MDT, mm | 0.87 ± 1.40 | 3.13 ± 1.35 | 2.26 ± 1.58 | .000 | .345 | .007 |
| U6DC_ MDT, mm | 0.88 ± 1.50 | 3.19 ± 1.39 | 2.31 ± 1.67 | .000 | .338 | .008 |
| U6MC_OGT, mm | −0.32 ± 0.52 | 0.29 ± 0.88 | 0.61 ± 0.89 | .000 | .273 | .035 |
| U6DC_OGT, mm | −0.02 ± 0.44 | 0.00 ± 0.86 | 0.01 ± 0.91 | .930 | .142 | .279 |
| U1_Torque, ° | −9.27 ± 9.09 | −14.43 ± 7.34 | −5.16 ± 5.92 | .000 | .760 | .000 |
| U1_LLT, mm | −6.60 ± 2.66 | −4.47 ± 1.81 | 2.12 ± 1.51 | .000 | .839 | .000 |
| U1_OGT, mm | −1.18 ± 1.60 | −1.68 ± 1.02 | −0.50 ± 1.17 | .002 | .682 | .000 |
U6MC indicates mesial buccal cusp of upper first molar; U6DC, distal buccal cusp of upper first molar; MDT, mesiodistal translation; LLT, labiolingual translation; OGT, occlusogingival translation.
Paired t-test; statistical significance at P ≤ .05.
Pearson correlation analysis; statistical significance at P ≤ 0.05.
Figure 4.
Scatter diagram and linear regression analyses of predicted and achieved tooth movement.
The study included eight 3-mm vertical, fifteen 3-mm horizontal, fourteen 5-mm horizontal, and 23 G6-optimized attachment cases in 13 adolescents (age 13.6 ± 1.4 years) and 17 adults (age 23.6 ± 4.1 years), according to the attachment designed on the maxillary first molar. Table 3 presents the influence of predicted tooth movement, age, attachment, and initial crowding on DPATM. Predicted tooth movement affected the differences in all measurements. Adolescents exhibited greater DPATM in the mesiodistal translation of the first molars and labiolingual translation of the central incisors and smaller DPATM in the occlusogingival translation of the first molars and crown torque of the central incisors than adults. The 3-mm vertical attachment group had greater DPATM in the mesiodistal translation of the first molars than the G6-optimized attachment group. Initial crowding had an inverse correlation with DPATM in the angulation and mesiodistal translation of the first molars.
Table 3.
Results From Linear Mixed-Effect Model Analyses for Differences Between Predicted and Achieved Tooth Movementa
| Effectb |
Mean ± SDc |
Estimate |
SE |
df |
t Value |
P Valued |
95% CI |
|
| Lower |
Upper |
|||||||
| U6_Angulation | ||||||||
| Intercept | 6.0521 | 0.9565 | 53 | 6.327 | <.0001 | 4.1336 | 7.9706 | |
| Predicted tooth movement | −0.2560 | 0.1135 | 53 | −2.256 | .028 | −0.4837 | −0.0284 | |
| Age | ||||||||
| Adolescent | 6.45 ± 3.22 | 1.7990 | 0.9251 | 53 | 1.945 | .057 | −0.0565 | 3.6544 |
| Adult | 5.42 ± 3.70 | Referent | – | – | – | – | – | |
| Attachment | ||||||||
| 3-mm vertical | 7.00 ± 4.14 | 0.3133 | 1.3843 | 53 | .226 | .822 | −2.4633 | 3.0899 |
| 3-mm horizontale | 5.34 ± 3.53 | −1.5286 | 1.1667 | 53 | −1.310 | .196 | −3.8688 | 0.8115 |
| 5-mm horizontal | 5.28 ± 1.56 | −1.0073 | 1.1226 | 53 | −.897 | .374 | −3.2589 | 1.2443 |
| G6-optimized | 6.17 ± 4.16 | Referent | – | – | – | – | – | |
| Crowding | −0.5780 | 0.2364 | 53 | −2.445 | .018 | −1.0521 | −0.1038 | |
| U6MC_MDT | ||||||||
| Intercept | 3.1002 | 0.2281 | 53 | 13.592 | <.0001 | 2.6427 | 3.5577 | |
| Predicted tooth movement | −0.7024 | 0.0813 | 53 | −8.644 | <.0001 | −0.8654 | −0.5394 | |
| Age | ||||||||
| Adolescent | 2.79 ± 1.67 | 1.1622 | 0.2366 | 53 | 4.911 | <.0001 | 0.6876 | 1.6368 |
| Adult | 1.85 ± 1.40 | Referent | – | – | – | – | – | |
| Attachment | ||||||||
| 3-mm vertical | 3.22 ± 1.37 | 0.8484 | 0.3615 | 53 | 2.347 | .023 | 0.1232 | 1.5735 |
| 3-mm horizontale | 2.02 ± 1.49 | −0.3351 | 0.3102 | 53 | −1.081 | .285 | −0.9573 | 0.2870 |
| 5-mm horizontal | 1.78 ± 1.60 | −0.1702 | 0.2942 | 53 | −.579 | .565 | −0.7603 | 0.4199 |
| G6-optimized | 2.36 ± 1.62 | Referent | – | – | – | – | – | |
| Crowding | −0.3654 | 0.0610 | 53 | −5.993 | <.0001 | −0.4877 | −0.2431 | |
| U6MC_OGT | ||||||||
| Intercept | 1.2629 | 0.2075 | 53 | 6.086 | <.0001 | 0.8467 | 1.6790 | |
| Predicted tooth movement | −0.4055 | 0.1855 | 53 | −2.186 | .033 | −0.7776 | −0.0334 | |
| Age | ||||||||
| Adolescent | 0.06 ± 0.70 | −0.8913 | 0.1961 | 53 | −4.545 | <.0001 | −1.2846 | −0.4979 |
| Adult | 1.03 ± 0.80 | Referent | – | – | – | – | – | |
| Attachment | ||||||||
| 3-mm vertical | 0.23 ± 0.61 | −0.5751 | 0.3138 | 53 | −1.833 | .072 | −1.2045 | 0.0543 |
| 3-mm horizontale | 0.27 ± 0.80 | −0.2647 | 0.2518 | 53 | −1.051 | .298 | −0.7697 | 0.2404 |
| 5-mm horizontal | 0.52 ± 0.73 | −0.2409 | 0.2419 | 53 | −.996 | .324 | −0.7260 | 0.2443 |
| G6-optimized | 1.02 ± 0.99 | Referent | – | – | – | – | – | |
| Crowding | −0.0987 | 0.0506 | 53 | −1.952 | .056 | −0.2002 | 0.0027 | |
| U1_Torque | ||||||||
| Intercept | −10.6046 | 0.7995 | 57 | −13.265 | <.0001 | −12.2055 | −9.0037 | |
| Predicted tooth movement | −0.3168 | 0.0574 | 57 | −5.516 | <.0001 | −0.4319 | −0.2018 | |
| Age | ||||||||
| Adolescent | −1.17 ± 5.32 | 5.7849 | 1.0448 | 57 | 5.537 | <.0001 | 3.6928 | 7.8770 |
| Adult | −8.21 ± 4.38 | Referent | ||||||
| U1_LLT | ||||||||
| Intercept | −1.0569 | 0.3301 | 57 | −3.202 | .002 | −1.7179 | −0.3959 | |
| Predicted tooth movement | −0.4284 | 0.0444 | 57 | −9.647 | <.0001 | −0.5173 | −0.3394 | |
| Age | ||||||||
| Adolescent | 2.62 ± 1.73 | 0.8297 | 0.2364 | 57 | 3.510 | .001 | 0.3563 | 1.3030 |
| Adult | 1.75 ± 1.22 | Referent | ||||||
| U1_OGT | ||||||||
| Intercept | −1.2672 | 0.1388 | 57 | −9.128 | <.0001 | −1.5451 | −0.9892 | |
| Predicted tooth movement | −0.5432 | 0.0628 | 57 | −8.643 | <.0001 | −0.6691 | −0.4174 | |
| Age | ||||||||
| Adolescent | −0.09 ± 1.18 | 0.2902 | 0.2012 | 57 | 1.442 | .155 | −0.1127 | 0.6931 |
| Adult | −0.81 ± 1.09 | Referent | ||||||
U6MC indicates mesial buccal cusp of upper first molar; MDT, mesiodistal translation; LLT, labiolingual translation; OGT, occlusogingival translation.
Variable coding: age (1 = adolescent; 2 = adult); attachment (1 = 3-mm vertical; 2 = 3-mm horizontal; 3 = 5-mm horizontal; 4 = G6-optimized).
Mean ± SD of differences between predicted and achieved tooth movement (achieved − predicted).
Linear mixed-effect model analysis; statistical significance at P ≤ .05.
Including four 4-mm horizontal attachments.
DISCUSSION
By using the ClinCheck program, orthodontists design the final 3D tooth position and expect its realization. However, findings from the present study showed that achieved tooth movement was not quite consistent with predicted tooth movement since the predicted tooth position was located simply by computer manipulation without consideration of mechanical properties of clear aligners as well as the biomechanical response of individual teeth.
In this sample, an average distal tipping of 2.9° was planned for the upper first molars, similar to anchorage preparation; however, these molars actually tipped mesially by 2.9° during treatment. Mesial tipping was expected owing to the mesial force applied on the first molar crown during extraction space closure. Although not statistically significant, adolescents showed a tendency of greater DPATM in first molar tipping than adults. Thus, when the same predicted first molar tipping was prescribed, greater achieved mesial tipping would be observed in adolescents than in adults, which was also shown to occur in fixed orthodontics.7–9 From the linear regression equation, first molars would actually tip mesially by 5.3° even if tooth angulation was virtually set stable. On the other hand, setting a distal tipping of 6.6° on the first molars in the plan might help clinically maintain the tooth angulation, leading to bodily tooth movement.
Most cases in this study were maximum anchorage cases, with an average predicted mesial translation of 0.87 mm in first molars; however, these achieved only medium anchorage control as the first molars actually moved mesially by 3.16 mm. In addition, adolescents showed greater DPTAM in the first molar mesiodistal translation than adults. Thus, adolescents would achieve greater mesial translation than adults if the same predicted mesiodistal translation were prescribed, which was comparable with what was observed in straight wire treatment.5,7–9 This indicated that physiologic anchorage loss10 existed not only in fixed orthodontic treatment but also in clear aligner treatment.10 From the regression equation, even if the first molar were set stable, it would actually move mesially by 2.8 mm. Therefore, if maximum anchorage control is needed in aligner treatment, auxiliary anchorage such as mini-implants should be considered.
The effects of attachments on maxillary molar anchorage control was also investigated. Based on the results of the mixed-effect model analyses, the G6-optimized attachment showed similar control in first molar angulation and mesiodistal translation as did 3- and 5-mm horizontal rectangular attachments. The G6-optimized attachment has a functional surface to resist mesial tipping. The rectangular attachment will generate a couple of distal tipping when the first molar is inclined to tip mesially. The 3-mm vertical rectangular attachment showed the least anchorage control and had greater DPATM in first molar mesial translation; incomplete engagement of the gingival wall of this attachment into the aligner may explain its lower efficiency. However, the sample size of the 3-mm vertical rectangular attachment group was small, and a larger sample size would be required for further validation.
Initial crowding was demonstrated to have a marked influence on anchorage loss in fixed orthodontic treatment.5 Findings from this study showed that initial crowding and anchorage loss were also correlated in clear aligner treatment. The greater the crowding, the lower the DPATM in mesial tipping and translation of the first molars. The extraction space was primarily used to relieve crowding and retract anterior teeth. According to biomechanical principles, less anchorage is generally required to relieve crowding than to retract anterior teeth.
Owing to molar anchorage loss, the amount of achieved retraction of incisors was lower than predicted. The difference between these achieved and predicted values became larger with an increase in predicted incisor retraction. Thus, orthodontists should be cautious when prescribing a plan of substantial anterior tooth retraction for patients. Under the retraction force, the incisors inclined lingually, and the achieved amount was greater than that was predicted. The difference between these two values was somewhat similar to the torque play between archwires and bracket slots.11 The DPATM in incisor crown torque was greater in adults than in adolescents, meaning that incisor torque loss would be more obvious in adults than in adolescents when the same predicted incisor torque was prescribed, which may lead to greater incisor retraction in adults. Power ridges and attachments on central incisors that were supposed to increase incisor torque control1,2 were seldom used in this sample. Accordingly, the use of power ridges or attachments as well as overcorrection by setting less lingual crown inclination or greater buccal crown inclination during the virtual setup should be considered to achieve optimal incisor torque control.
The intrusion of first molars that was observed during this study was probably due to the occlusal splint effect12 when wearing aligners. Although the amount of intrusion was relatively small, it may contribute to the open bite of the first molars, which is commonly observed in clinical practice during clear aligner treatment, and therefore, heavy occlusal contacts on posterior teeth could be considered during setup. Adolescents showed smaller DPATM in first molar intrusion as compared with adults, which could be related to vertical growth.13 The incisors extruded after aligner treatment and the DPATM showed no significant difference between adolescents and adults; the extrusion would lead to an increase in anterior overbite.
In this study, actual pre- and posttreatment digital models were acquired using two different methods: extraoral scanning and intraoral scanning. For dental arches, although intraoral scanning was previously shown to be less accurate than extraoral scanning, differences in accuracy were quite small; hence, both techniques can be used in clinical practice.14 The palatal vault is a soft tissue and may be slightly deformed under compression while recording conventional impressions. However, deviation of the palatal vault between extraorally and intraorally scanned models was also limited.15 Thus, the errors of dental arch registration and palatal vault registration because of different sources of the models could be neglected relative to tooth movement measurements.
Patients who did not complete the first series of aligners and had midcourse corrections were not included in this sample; thus, the results of this study might underestimate the DPATM. In other words, first molar anchorage control and central incisor retraction achievement may be even worse in clinical practice.
CONCLUSION
In first premolar extraction cases treated with Invisalign, first molar anchorage control and central incisor retraction were not fully achieved as predicted. Age, attachment type, and initial crowding affected the differences between predicted and achieved tooth movement. Auxiliary anchorage devices, power ridges and attachment designs, and overcorrection should be considered to help achieve predicted changes.
ACKNOWLEDGMENT
We thank the statistician Li-Yuan Tao at the Research Center of Clinical Epidemiology, Peking University Third Hospital, for assistance with the statistical analyses.
REFERENCES
- 1.Kravitz ND, Kusnoto B, Begole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;135:27–35. doi: 10.1016/j.ajodo.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 2.Simon M, Keilig L, Schwarze J, Jung BA, Bourauel C. Treatment outcome and efficacy of an aligner technique—regarding incisor torque, premolar derotation and molar distalization. BMC Oral Health. 2014;14:68–74. doi: 10.1186/1472-6831-14-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grünheid T, Loh C, Larson BE. How accurate is Invisalign in nonextraction cases? Are predicted tooth positions achieved? Angle Orthod. 2017;87:809–815. doi: 10.2319/022717-147.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baldwin DK, King G, Ramsay DS, Huang G, Bollen AM. Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: premolar extraction patients. Am J Orthod Dentofacial Orthop. 2008;133:837–845. doi: 10.1016/j.ajodo.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 5.Geron S, Shpack N, Davidovitch M, Kandos S, Davidovitch M, Vardimon AD. Anchorage loss—a multifactorial response. Angle Orthod. 2003;73:730–737. doi: 10.1043/0003-3219(2003)073<0730:ALMR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Chen G, Chen S, Zhang XY, et al. Stable region for maxillary dental cast superimposition in adults, studied with the aid of stable miniscrews. Orthod Craniofac Res. 2011;14:70–79. doi: 10.1111/j.1601-6343.2011.01510.x. [DOI] [PubMed] [Google Scholar]
- 7.McKinney JR, Harris EF. Influence of patient age and sex on orthodontic treatment: evaluations of Begg lightwire, standard edgewise, and the straightwire techniques. Am J Orthod Dentofacial Orthop. 2001;120:530–541. doi: 10.1067/mod.2001.118784. [DOI] [PubMed] [Google Scholar]
- 8.Heo W, Nahm DS, Baek SH. En masse retraction and two-step retraction of maxillary anterior teeth in adult Class I women. Angle Orthod. 2007;77:973–978. doi: 10.2319/111706-464.1. [DOI] [PubMed] [Google Scholar]
- 9.Xu TM, Zhang XY, Oh HS, Boyd RL, Korn EL, Baumrind S. Randomized clinical trial comparing control of maxillary anchorage with 2 retraction techniques. Am J Orthod Dentofacial Orthop. 2010;138:544.e1–e9. doi: 10.1016/j.ajodo.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 10.Xu TM. New concept of physiologic anchorage control. APOS Trends Orthod. 2015;5:250–254. [Google Scholar]
- 11.Archambault A, Lacoursiere R, Badawi H, Major P, Carey J, Flores-Mir C. Torque expression in stainless steel orthodontic brackets: a systematic review. Angle Orthod. 2010;80:201–210. doi: 10.2319/080508-352.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Widmalm SE. Use and abuse of bite splints. Compend Contin Educ Dent. 1999;20:249–254. [PubMed] [Google Scholar]
- 13.Iseri H, Solow B. Continued eruption of maxillary incisors and first molars in girls from 9 to 25 years, studied by the implant method. Eur J Orthod. 1996;18:245–256. doi: 10.1093/ejo/18.3.245. [DOI] [PubMed] [Google Scholar]
- 14.Flügge TV, Schlager S, Nelson K, Nahles S, Metzger MC. Precision of intraoral digital dental impressions with iTero and extraoral digitization with the iTero and a model scanner. Am J Orthod Dentofacial Orthop. 2013;144:471–478. doi: 10.1016/j.ajodo.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 15.Ning G, Xiong Y, Jiao T. Accuracy of intraoral digital impressions for whole upper jaws, including full dentitions and palatal soft tissues. PLOS One. 2016;11:e0158800. doi: 10.1371/journal.pone.0158800. [DOI] [PMC free article] [PubMed] [Google Scholar]