Abstract
Objectives:
To compare the accuracy of bonding orthodontic attachments in a digital environment with the direct bonding procedure depending on the level of the orthodontist's clinical experience.
Materials and Methods:
A total of 1120 artificial teeth of 40 identical models (20 solid sets + 20 digital sets) were divided into four groups: (1) direct bonding (experienced clinicians). (2) direct bonding (postgraduate students), (3) virtual bonding (experienced clinicians), and (4) virtual bonding (postgraduate students). The differences in individual position of the placed attachments were measured after three-dimensional superimposition of the models using customized software.
Results:
In the interoperator comparison, experienced clinicians were more exact than postgraduate students in virtual bonding in the angular dimension. Between the bonding techniques, virtual bonding was more accurate than the direct technique. The prevalence of errors was higher in the direct procedure than virtual bonding, and the errors were more significant in the premolar and molar teeth.
Conclusions:
Clinical experience had a positive influence in achieving a higher rate of correctness/accuracy in the angular dimension only during virtual bonding. Virtual bonding was more accurate than direct bonding in the vertical and horizontal dimensions. Early diagnosis of errors in the bonding positions of attachments could be of benefit to both clinicians and patients by predicting discrepancies that may lead to undesirable orthodontic movements.
Keywords: Digital bonding, Direct bonding, Clinical experience, Accuracy
INTRODUCTION
Traditionally, orthodontic tubes and brackets (attachments) are bonded directly onto tooth surfaces or indirectly onto a plaster cast for later transfer to the teeth. Indirect bonding appears to have greater standardization and consistency of the attachment positions.1,2 Evidence does not support the conventional preference to pursue direct bonding because both methods (direct and indirect) appear to have failed to achieve the ideal position.3–6
Errors in bonding position may be due to a lack of professional dexterity and experience, subsequently prolonging chair time and overall treatment time with consequent unnecessary discomfort to the patient.7,8 Various factors potentially impact the precision of bracket positioning, such as patient cooperation, excessive salivation, limits of maximum mouth opening, variation in dental morphology,9,10 complexity of malocclusion, type of bracket,11 material and morphology of the transfer guide,12,13 and variations in perception of the ideal position.14
In an attempt to minimize human error at this critical stage of executing the treatment plan, an increasing number of studies have been directed toward refining indirect protocols, with emphasis on those that have added computer-aided design/computer-aided manufacturing (CAD/CAM) technology.2,10,15–17 Over the last few decades, different commercial systems have been made available, including multifunctional software programs that have optimized the bonding processes, especially in the planning and laboratory stages. These innovations have not, however, demonstrated significant improvements in accuracy.6,15,18
An additional factor contributing to error is the significant learning curve of the clinician performing the bonding.14 Orthodontic attachments that have been incorrectly positioned on virtual models leads to the same discrepancies as during direct bonding clinically and similarly compromise the dynamics of therapy.5 This is particularly important for preadjusted or straight wire appliance when inaccurately bonded attachments will lead to inaccurate tooth movement.
The accuracy of computer-aided bonding of preadjusted appliances has not yet been described in the literature. Similarly, investigations about the influence of clinical experience have also not been well explored. Evaluating the quality of individual positioning of attachments can make it possible to foresee how that may lead to undesirable orthodontic movements, thereby directly benefiting both the clinician and the patient.
The aim of the present study was to compare the accuracy of bonding orthodontic attachments in a digital environment with the direct procedure, while considering the impact of the experience level of the clinician.
MATERIALS AND METHODS
This was an in vitro, prospective trial with a representative sample, in which 10 experienced clinicians (over 7 years of clinical practice in orthodontics) and 10 postgraduate students (fewer than 2 years of clinical practice) performed orthodontic attachment bonding procedures (Ethics:78890217.0.0000.5149). The participants bonded 28 attachments per model, where the upper and lower central incisors, lateral incisors, canines, first and second premolars, and first molars of the right and left side had a bracket for attachment; in addition, a tube was bonded to the second molars.
To obtain identical experimental models, a single dental mannequin (Dent-Art, São Paulo, Brazil) in normal occlusion and with complete dentition, except for the third molars, was digitized using a bench scanner (3Shape R700 Orthodontic Scanner, 3Shape, Copenhagen, Denmark). After scanning the mannequin's dentition, the digital model was imported and prepared (OrthoAnalyzer, 3Shape) for segmentation of the tooth units. Then, specific positional changes were incorporated into multiple units (12 teeth in the horizontal component; 6 in the angulation; 10 in the vertical, horizontal, and angular dimensions; and 6 remaining aligned and leveled). The resultant configuration (Class I malocclusion of the teeth with slight/moderate crowding) served as a basis for obtaining the reference model; intervention models were obtained by prototyping (Eden500, Stratasys, Israel).
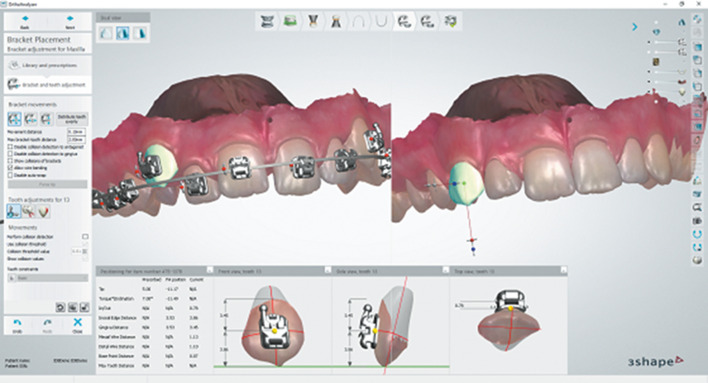
To generate the reference model, the incorporated malocclusion was virtually treated by a specialized laboratory technician in the presence and under supervision of the principal investigator. For this purpose, the library of the program was used to select the same brand and prescription of brackets that would subsequently be used on the intervention models: 0.022 × 0.028 inches, preadjusted metal brackets with MBT prescription, Mini Master series (American Orthodontics, Sheboygan, Wis) and simple preadjusted tubes, MBT prescription, iFit nonconvertible buccal series (American Orthodontics). Initially, the digital bracket-dental setup was made with an ideal digital stainless steel archwire of 0.021 × 0.025 inches to show the attachments in the virtual positions in the ideal arch, with the purpose of simulating the respective posttreatment positions. After this, the configuration of the final positions obtained was reverted using OrthoAnalyzer software (3Shape) to the malocclusion under study (Figure 1).
Figure 1.
Development of the reference model: the teeth were segmented into individual units and the malocclusion was virtually incorporated in the digital cast. The brackets were selected (0.022 × 0.028 inch, preadjusted metal brackets, MBT prescription, Mini Master series, American Orthodontics®, Sheboygan, Wis; and, simple preadjusted tubes, MBT prescription, iFit nonconvertible buccal series, American Orthodontics) and virtually positioned in the ideal position for each tooth by the principal operator. To simulate the posttreatment positions of the teeth and to double-check if the attachments were in the ideal position, the digital bracket dental setup was treated with an ideal digital stainless steel archwire of 0.021 × 0.025 inches. Subsequently, the configuration of the final positions obtained was reverted using OrthoAnalyzer software (3Shape, Copenhagen, Denmark) to the malocclusion under study.
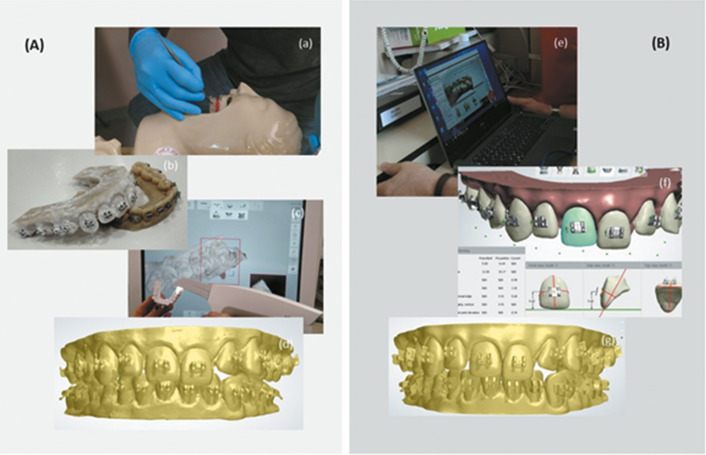
To carry out the bonding procedures, 40 sets of identical models (20 solid cast sets + 20 digital sets) were equally distributed into four groups: group 1, direct bonding (experienced clinicians); group 2, direct bonding (postgraduate students); group 3, virtual bonding (experienced clinicians); group 4, virtual bonding (postgraduate students).The direct bonding procedures were performed under preclinical conditions. The solid casts were individually coupled to the head of the mannequins, and the vestibular surfaces were prepared with a thin layer of adhesive (Transbond XT, 3M Unitek, St Paul, Minn). Each participant performed the bonding with no prescription restriction and no work flow or time restrictions. The clinicians performed the bonding procedures with resin (Transbond XT, 3M Unitek) and using a light-emitting diode light for 20 seconds on each tooth (Figure 2A, a and b).
Figure 2.
Stages for obtaining the models for measurement: Direct bonding (A): performing the direct bonding procedure on the solid cast model (a); solid cast model with surface prepared for scanning (b); scanning the solid cast model with the intraoral scanner (c); digital 3D model after direct bonding (d). (B) Virtual bonding: virtual bonding via web (e); partial presentation of the report issued by the software defining the final bonding positions (f); digital 3D model after virtual bonding (g).
Fifteen days later, the same operators performed virtual bonding in the digital environment. In the interval between the two bonding procedures, an institutional video explaining the process of virtual bonding (3Shape) was sent by e-mail to each participant. Also, written explanatory text about how the interaction with the virtual bonding software would occur was given to the participants. All the participants performed the virtual bonding procedure using the same computer. The communication was done via Skype, with interaction between the anonymous clinician participant and the software operator who manipulated the virtual bonding. Bonding occurred according to the clinician's perception of ideal bonding (Figure 2B, e and f).
Once the bonding interventions were concluded, the solid cast models were scanned (Figure 2A, c and d) with an intraoral scanner (Scanner 3D, Ultrafast Optical Sectioning, Trios Orthodontic, 3Shape) to make up the final sample totaling 40 sets of digital models. After this scanning procedure, the principal clinician investigator measured the positions of the bonds by superimposing the 3D digital images of the digitalized real casts and the virtual casts (Appliance Designer, 3Shape) with the ideal position of the attachments in the reverted reference model. The ideal bonding position was defined by the absence of a discrepancy in the position of each attachment in the three dimensions (vertical [height], horizontal [mesiodistal]. and angular [angulation]) compared with the validated virtual bond reference.
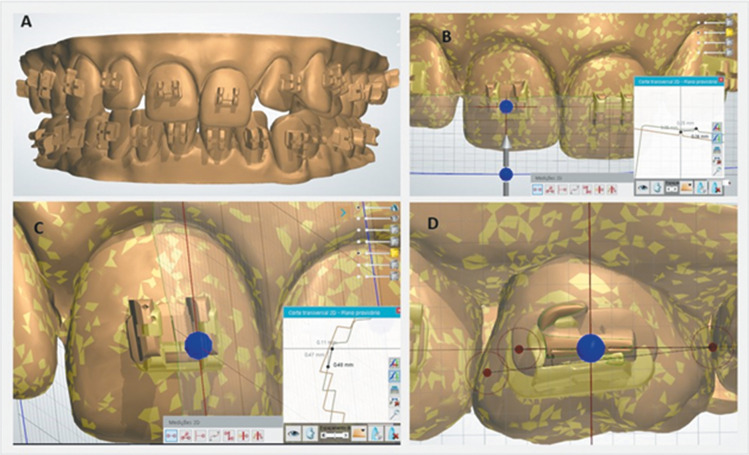
Vertical deviation was defined as distance projected in millimeters, between the central interline points when the plane of visualization resulted in a transverse section along the central vertical axis of the reference attachment. Displacements in the gingival direction were positive and those in the incisal/occlusal direction, negative. Horizontal deviation was defined as the distance projected, in millimeters, between the central interline points when the plane of visualization resulted in a transverse section along the central horizontal central axis of the reference accessory. Displacements in the mesial direction were positive, and displacements in the distal direction were negative. Angular deviation was defined as the right angular measurement represented when the transverse section passed through the base of the reference bracket and its line assumed an angle of zero in relation to the horizontal axis of the frontal plane of visualization. When this readout was taken from the mesial aspect of the attachment, displacements in the anticlockwise direction were positive, and displacements in the clockwise direction were negative (Figure 3A through D).
Figure 3.
Measurement of bonding accuracy after superimposition of 3D models. Model with reference bonding positions (A); transverse section at the horizontal axis of tooth 21 and the two-dimensional projection of the mesiodistal positions of the respective brackets (B); transverse section at the vertical axis of tooth 11 and the two-dimensional projection of the heights of the respective brackets (C); transverse section in the frontal plane of tooth 16 with right side view of the angles of the respective simple tubes (D).
Statistical Analysis
Results are expressed as means ± standard deviation (SD). Because data sets presented a normal distribution (D'Agostino and Pearson omnibus normality test and Shapiro-Wilk normality test), and there were multiple variables, two-way analysis of variance (ANOVA) was used to analyze differences between groups (intraoperator and interoperator), followed by a Bonferroni posttest. The data obtained from all evaluations were processed with GraphPad Prism version 5.01 (GraphPad Software, San Diego, Calif). The level of significance for all statistical tests was predetermined at 5%. The frequency of errors that exceeded the clinical limits was compared by means of the χ2 test. Accepted limits for the grouping of ranges included a deviation of 0.5 mm for the linear dimensions and 0.5° for angulation.
RESULTS
A total of 1120 orthodontic attachments (560 solid and 560 virtual attachments) were bonded. Sample losses and exclusions occurred due to debonding before scanning and scanner readout error.
In the intraoperator analysis, virtual bonding was more accurate than direct bonding in the vertical and horizontal dimensions but not in the angular (Table 1). In the interoperator comparison, no difference was observed between the experienced clinicians and postgraduate students in the two different bonding methods, except in the angular dimension where experienced clinicians were more accurate than postgraduate students in the virtual bonding (Table 1).
Table 1.
Interoperator and Intraoperator Comparison of the Position of the Orthodontic Attachments, Measured According to the Bonding Technique in the Three Parameters Evaluateda
| Dimension |
Direct Bonding |
Virtual Bonding |
||||||
| Experienced Clinicians |
Postgraduate Students |
Experienced Clinicians |
Postgraduate Students |
|||||
| Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
| Vertical | –0.81 a | 0.34 | –0.96 a | 0.24 | –0.31 b | 0.14 | –0.42 b | 0.07 |
| Horizontal | –0.01 c | 0.06 | 0.00 c | 0.11 | 0.10 d | 0.07 | 0.13 d | 0.09 |
| Angular | 0.17 ef | 1.11 | –0.36 ef | 0.64 | –0.03 e | 0.46 | –0.84 f | 0.55 |
Data shown as mean ± standard deviation (SD); N = 10 participants per group. For each dimension, different letters mean statistically different values among groups. Vertical: (a) P < .001 compared with (b) for the same professional group. Horizontal: (c) P < 0.01 compared with (d) for the same professional group. Angular: (e) P < .05 compared with (f) for the virtual bonding method. Two-way analysis of variance followed by the Bonferroni posttest.
Relative to the distribution of errors that exceeded the clinical limits, the intraoperator comparison showed that the number of errors was lower for both the experienced clinicians and the postgraduate students in the virtual bonding compared with direct bonding only in the vertical dimension (Table 2). No difference was seen in the horizontal and angular dimensions of the intraoperator comparison and none in the interoperator analysis (Table 2).
Table 2.
Frequency of Bonding Errors for Each Dimension Analyzed That Exceeded the Clinical Limits (Above 0.5 mm in the Linear Dimensions and Above 0.5° in Angulation), According to the Time of Clinical Experience and Type of Bonding Method (n = 10 Participants per Group)
| Dimension |
|||||||||
| Vertical |
Pa |
Horizontal |
Pa |
Angular |
Pa |
||||
| Exceeded |
Did Not Exceed |
Exceeded |
Did Not Exceed |
Exceeded |
Did Not Exceed |
||||
| Operator who performed procedure | |||||||||
| Experienced clinicians | |||||||||
| Direct | 9 | 1 | .0017 | 0 | 10 | – | 7 | 3 | .1775 |
| Virtual | 2 | 8 | 0 | 10 | 4 | 6 | |||
| Postgraduate students | |||||||||
| Direct | 10 | 0 | <.0001 | 0 | 10 | – | 8 | 2 | .6056 |
| Virtual | 1 | 9 | 0 | 10 | 7 | 3 | |||
| Bonding method | |||||||||
| Direct | |||||||||
| Experienced clinicians | 9 | 1 | .3049 | 0 | 10 | – | 7 | 3 | .6056 |
| Postgraduate students | 10 | 0 | 0 | 10 | 8 | 2 | |||
| Virtual | |||||||||
| Experienced clinicians | 2 | 8 | .5312 | 0 | 10 | – | 4 | 6 | .1775 |
| Postgraduate student | 1 | 9 | 0 | 10 | 7 | 3 | |||
χ2 test.
Because of the increased errors that exceeded the clinical limits in the vertical dimension, the frequency of bonding errors for each tooth group in this dimension was examined in more depth. The results demonstrated that there were significant differences among the teeth in the direct bonding of the experienced clinicians but not in the virtual bonding by the same professional group (Table 3). The premolars and molars had an increased frequency of errors. In addition, the postgraduate students demonstrated statistical differences in the frequency of bonding errors for each tooth group in the vertical dimension in both bonding methods, direct and virtual; similar to the experienced clinicians, the errors were more frequent in the premolars and molars (Table 3).
Table 3.
Frequency of Bonding Errors for Each Teeth in the Vertical Dimension That Exceeded the Clinical Limits (Above 0.5 mm in the Linear Dimensions and Above 0.5° in Angulation), According to the Time of Clinical Experience (n = 10 Participants per Group)
| Operator Who Performed Procedure |
Dimension |
||
| Vertical |
Pa |
||
| Exceeded |
Did Not Exceed |
||
| Experienced clinicians | |||
| Direct | |||
| Incisor | 5 | 5 | .0078 |
| Canine | 3 | 7 | |
| Premolar | 9 | 1 | |
| Molar | 9 | 1 | |
| Virtual | |||
| Incisor | 2 | 8 | .0626 |
| Canine | 0 | 10 | |
| Premolar | 5 | 5 | |
| Molar | 2 | 8 | |
| Postgraduate students | |||
| Direct | |||
| Incisor | 8 | 2 | .0018 |
| Canine | 4 | 6 | |
| Premolar | 10 | 0 | |
| Molar | 10 | 0 | |
| Virtual | |||
| Incisor | 1 | 9 | .0002 |
| Canine | 0 | 10 | |
| Premolar | 8 | 2 | |
| Molar | 2 | 8 | |
χ2 test.
DISCUSSION
This study compared the accuracy of the position of orthodontic attachments when bonded in a Class I malocclusion using direct and virtual bonding methods performed by experienced clinicians and postgraduate students. The results showed that, only in the angular dimension, the experienced clinicians achieved greater accuracy than the postgraduate students in the virtual bonding technique and that virtual bonding was more exact in the vertical and horizontal dimension for both professional groups. The experienced clinicians had fewer errors that exceeded the clinical limits in the vertical dimension in the premolars and molars when using the virtual bonding technique compared with direct bonding, while no improvement was seen within the postgraduate students in the same group of teeth between the two different methods.
The accuracy of computer-aided bonding has not yet been described in the literature. Similarly, no comparative study has showed the influence of operator experience on attachment positioning with the digital methodology. The repeatability and reproducibility of the placements were considered in a virtual bonding study only.2 Other investigations involving digital indirect protocols have analyzed the quality of placing the appliance by quantification of the posttreatment benefit6,10,19 and never by quantification of the individual positioning of the attachments.
The influence of clinical experience in obtaining am accurate direct bonding procedure has rarely been explored. A previous study that compared experienced orthodontists and postgraduate students showed that obtaining accuracy did not appear to be related to clinical experience.14 In that study, the postgraduate students were more precise in positioning the brackets vertically. The current findings, however, were in disagreement with those results because the experienced clinicians were more exact than the postgraduate students in the vertical dimension and in angulation.
In order to minimize the factors that could potentially induce experimental errors, all of the operators individualized the bonding position on the same pattern of malocclusion. Additionally, all the solid cast models were prototyped with the same type of resin and scanned with a single scanner.20,21
The methods for measuring the positions of the orthodontic attachments have improved over time. Most recently, the use of superimposed three-dimensional (3D) images with cone beam computed tomography incorporated a new level of precision into analyses.13 In the present study, the position of individual attachments was quantified by superimposing 3D models. In an attempt to minimize errors of superimposition, single coronal segmentation was accomplished and used for both the setup that generated the reference model and for virtual incorporation of the study malocclusion. This process ensured that the measurements of the bonding positions would be made among models with equal configuration. The intercenter distances between the line of the reference attachments and those of the experimental units were measured so that possible distortions due to the margins of metal brackets would not influence the readouts.2
The various preadjusted appliance systems come in numerous prescriptions. These variations include differences in angles, torques, and inclination, as well as adjustments for facial type, malocclusion, and cases with or without extraction. There is also an inherent subjectivity of esthetic evaluation, making it difficult to reach consensus about the ideal dental position in orthodontics. These standardizations may result in discrepancies of bonding position that are not necessarily reflected as significant clinical differences among treated patients.22,23 In this context, evaluating the frequency of errors that exceed the clinical limit becomes more clinically relevant than the values expressed by the mean and SD.7
The findings demonstrated that the percentages of these errors were lower in the bonding positions of the virtual environment in the horizontal and vertical dimensions; however, for angulation, the prevalence was higher in virtual bonding than it was in the direct procedure. When comparing the groups with respect to operator experience, experienced clinicians committed a lower percentage of errors in the angular dimension. The results of errors that exceeded the clinical limit were reported in relation to the types of guides13,21 and influence of the cusp height of posterior teeth,10 but they have not been specific about the positioning of the attachments.
In computed bonding as performed in the present project, the possibility of 3D visualization of the models, simultaneously moving and measuring the individual positions of the orthodontic attachments and comparing them in relation to the opposing tooth or side; even checking the final positions more quickly would hypothetically provide greater accuracy of attachment positions. The inexperience of participants in individualizing the bonding position in the digital model may have influenced the results. All participants, experienced and inexperienced, performed the procedure for the first time during the development phase of this research project. Another, no less important. factor was the training methodology used. Watching an instructional video about the bonding software under investigation may have been insufficient as a method of learning.
Although direct bonding showed less bonding accuracy, the main error are focused in the premolars and molars, irrespective of clinical experience. This suggest that by positioning the fixed appliance directly to the teeth in the malocclusion, the orthodontist must be aware of this problem and must play closer attention to the process.
CONCLUSIONS
Clinical experience had a positive influence on the higher rate of correctness/accuracy in the angular dimension only during virtual bonding.
Virtual bonding was more accurate than direct bonding in the vertical and horizontal dimensions.
The frequency of errors that exceeded the clinical limits in virtual bonding was significantly lower than those in direct bonding in the vertical linear dimension.
Premolars and molars were the group of teeth with the highest frequency of bonding errors in the vertical dimension in all groups, except during virtual bonding by the experienced clinicians.
REFERENCES
- 1.Kalange JT. Indirect bonding: a comprehensive review of the advantages. World J Orthod. 2004;5:301–307. [PubMed] [Google Scholar]
- 2.Nichols DA, Gardner G, Carballeyra AD. Reproducibility of bracket positioning in the indirect bonding technique. Am J Orthod Dentofacial Orthop. 2013;144:770–776. doi: 10.1016/j.ajodo.2013.04.023. [DOI] [PubMed] [Google Scholar]
- 3.Aguirre MJ, King GJ, Waldron JM. Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. Am J Orthod. 1982;82:269–276. doi: 10.1016/0002-9416(82)90461-4. [DOI] [PubMed] [Google Scholar]
- 4.Koo BC, Chung CH, Vanarsdall RL. Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. Am J Orthod Dentofacial Orthop. 1999;116:346–351. doi: 10.1016/s0889-5406(99)70248-9. [DOI] [PubMed] [Google Scholar]
- 5.Hodge TM, Dhopatkar AA, Rock WP, Spary DJ. A randomized clinical trial comparing the accuracy of direct versus indirect bracket placement. J Orthod. 2004;31:132–137. doi: 10.1179/146531204225020427. [DOI] [PubMed] [Google Scholar]
- 6.Israel M, Kusnoto B, Evans CA, Begole E. A comparison of traditional and computer-aided bracket placement methods. Angle Orthod. 2011;81:828–835. doi: 10.2319/072110-425.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Germane N, Bentley BE, Jr, Isaacson RJ. Three biologic variables modifying faciolingual tooth angulation by straight-wire appliances. Am J Orthod Dentofacial Orthop. 1989;96:312–319. doi: 10.1016/0889-5406(89)90350-8. [DOI] [PubMed] [Google Scholar]
- 8.Poling R. A method of finishing the occlusion. Am J Orthod Dentofacial Orthop. 1999;115:476–487. doi: 10.1016/s0889-5406(99)70268-4. [DOI] [PubMed] [Google Scholar]
- 9.Miethke RR, Melsen B. Effect of variation in tooth morphology and bracket position on first and third order correction with preadjusted appliances. Am J Orthod Dentofacial Orthop. 1999;116:329–335. doi: 10.1016/s0889-5406(99)70246-5. [DOI] [PubMed] [Google Scholar]
- 10.Kim J, Chun YS, Kim M. Accuracy of bracket positions with a CAD/CAM indirect bonding system in posterior teeth with different cusp heights. Am J Orthod Dentofacial Orthop. 2018;153:298–307. doi: 10.1016/j.ajodo.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Birdsall J, Hunt NP, Sabbah W, Moseley HC. Accuracy of positioning three types of self-ligating brackets compared with a conventionally ligating bracket. J Orthod. 2012;39:34–42. doi: 10.1179/14653121226806. [DOI] [PubMed] [Google Scholar]
- 12.Castilla AE, Crowe JJ, Moses JR, Wang M, Ferracane JL, Covell DA., Jr Measurement and comparison of bracket transfer accuracy of five indirect bonding techniques. Angle Orthod. 2014;84:607–614. doi: 10.2319/070113-484.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grunheid T, Lee MS, Larson BE. Transfer accuracy of vinyl polysiloxane trays for indirect bonding. Angle Orthod. 2016;86:468–474. doi: 10.2319/042415-279.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Armstrong D, Shen G, Petocz P, Darendeliler MA. Accuracy of bracket placement by orthodontists and inexperienced dental students. Aust Orthod J. 2007;23:96–103. [PubMed] [Google Scholar]
- 15.Larson BE, Vaubel CJ, Grunheid T. Effectiveness of computer-assisted orthodontic treatment technology to achieve predicted outcomes. Angle Orthod. 2013;83:557–562. doi: 10.2319/080612-635.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El-Timamy AM, El-Sharaby FA, Eid FH, Mostafa YA. Three-dimensional imaging for indirect-direct bonding. Am J Orthod Dentofacial Orthop. 2016;149:928–931. doi: 10.1016/j.ajodo.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Muller-Hartwich R, Jost-Brinkmann PG, Schubert K. Precision of implementing virtual setups for orthodontic treatment using CAD/CAM-fabricated custom archwires. J Orofac Orthop. 2016;77:1–8. doi: 10.1007/s00056-015-0001-5. [DOI] [PubMed] [Google Scholar]
- 18.Mayhew MJ. Computer-aided bracket placement for indirect bonding. J Clin Orthod. 2005;39:653–660. [PubMed] [Google Scholar]
- 19.Brown MW, Koroluk L, Ko CC, Zhang K, Chen M, Nguyen T. Effectiveness and efficiency of a CAD/CAM orthodontic bracket system. Am J Orthod Dentofacial Orthop. 2015;148:1067–1074. doi: 10.1016/j.ajodo.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 20.Huanca Ghislanzoni LT, Lineberger M, Cevidanes LH, Mapelli A, Sforza C, McNamara JA., Jr Evaluation of tip and torque on virtual study models: a validation study. Prog Orthod. 2013. 26:14:19. [DOI] [PMC free article] [PubMed]
- 21.Schmid J, Brenner D, Recheis W, Hofer-Picout P, Brenner M, Crismani AG. Transfer accuracy of two indirect bonding techniques—an in vitro study with 3D scanned models. Eur J Orthod. 2018;40:549–555. doi: 10.1093/ejo/cjy006. [DOI] [PubMed] [Google Scholar]
- 22.Jain M, Varghese J, Mascarenhas R, Mogra S, Shetty S, Dhakar N. Assessment of clinical outcomes of Roth and MBT bracket prescription using the American Board of Orthodontics Objective Grading System. Contemp Clin Dent. 2013;4:307–312. doi: 10.4103/0976-237X.118361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moesi B, Dyer F, Benson PE. Roth versus MBT: does bracket prescription have an effect on the subjective outcome of preadjusted edgewise treatment? Eur J Orthod. 2013;35:236–243. doi: 10.1093/ejo/cjr126. [DOI] [PubMed] [Google Scholar]