Abstract
Background
The health care workers (HCWs) at the frontline of fighting COVID-19 are at higher risk for mental health problems, including stress, anxiety, depression, and insomnia. This study aimed at assess the status of occupational stress in the three occupational groups of nurses, physicians and hospital cleaning crew facing COVID-19 patients in hospitals of Kerman province in Iran.
Methodology
This cross-sectional descriptive analytical study was performed on 290 medical staffs including nurses, physicians and cleaning crew facing COVID-19 patients working in different hospitals in Iran in 2020. Demographic information form and occupational Stress Questionnaire (HSE tool indicator) were used to collect data. The health and safety executive (HSE) questionnaire has 35 questions and 7 areas, which was developed in the 1990s by the UK Health and Safety Institute to measure occupational stress.
Results
The mean score of total dimensions among HCWs was 2.93. Communications, Manager support, Changes and Demand factors with scores of 2.76, 2.77, 2.83 and 2.87 had the greatest impact on participants' stress levels, respectively. Also, Colleague support factor with a score of 3.38 had the least effect on stress levels. Also, according to the results, 87% of nurses, 79% of cleaning crew and 67% of physicians had a partial to high levels of stress that, on average, 77.5% of the HCWs participating in this study had at least a small amount of stress.
Conclusions
The mean stress score among the participants of the present study was between high stress level and moderate stress level. Factors such as communications, manager support, change and demand had the greatest impact on employee stress levels. Therefore, by improving the communication between people working in hospitals, increasing managers' support for staff, and reducing workplace demands such as reducing workload and improving workplace environment, the stress level of staff in hospitals during the outbreak of COVID-19 can be reduced.
Keywords: Occupational stress, Health care workers (HCWs), Health personnel, HSE questionnaire, COVID-19
Occupational stress, Health care workers (HCWs), Health personnel, HSE questionnaire, COVID-19.
1. Introduction
COVID-19, formerly known as nCoV-2019 is an acute respiratory disease (pneumonia) caused by the Corona virus that was first identified in Wuhan, China [1]. According to the World Health Organization (WHO), the disease is caused by the SARS-COV-2 virus, and the resulting pandemic poses a serious threat to the health of the global community. According to the available evidence, human-to-human transmission of COVID-19 is possible through respiratory droplets containing the viral aerosol as well as contact with surfaces [2, 3, 4]. In Iran, with the identification of two cases in February 2020, the outbreak of COVID-19 was announced for the first time [5]. Not knowing the disease, lack of effective drugs for the treatment and severe effects of the disease on some patients led to a wave of stress and emotional reactions in Iranian society [6].
According to studies, different groups of people, including children, the elderly and those with special medical conditions (such as pregnant women) are more susceptible to the disease [7, 8]. Nonetheless, health care workers such as physicians, nurses, and other frontline health care workers are an important part of the population who may become infected through work and job confrontation [4, 8]. The health care workers occupied in medical sections is one of the vital assets of any country in the event of a crisis such as COVID-19 [9]. Therefore, maintaining the health and safety of this group of people is important not only to save the lives of patients but also to control the spread of the disease [10]. The HCWs are one of the high-risk groups of facing this infectious disease. In addition to exposure to this pathogen, these individuals face other occupational hazards, including long working hours, fatigue, mental burnout induced by workload, skin blemishes, stress, and other physical and psychological injuries [11]. Different quantitative studies conducted in Iran and around the world show that the frontline health care workers against COVID-19 are at higher risk for mental health-related problems such as stress, anxiety, depression and insomnia [12, 13].
The psychological stress is a condition that effects on the decision making power [14]. In the field of occupational health, stress is also known as occupational stress, which is a state of psychological and physical stress in the workplace and is due to high demand and needs of the workplace compared to the capabilities of the workforce [15, 16]. Stress is an integral part of all jobs, but it is mostly found in jobs that are closely related to health and death and life and requires more attention [17, 18]. Those involved in the medical and treatment professions are affected by various stressors in their work environment due to their responsibility to ensure the health and treatment of patients [19]. Stress causes several adverse symptoms such as insomnia, headache, fatigue, anxiety, gastrointestinal upset and decreased immunity, as well as increased family conflicts, decreased quality of work, interpersonal disorders and other negative effects [20, 21]. Furthermore, Harmful factors in the workplace, such as noise and heat, cause stress and the release of stress hormones in the body [22, 23, 24]. Medical staffs especially that work in hospitals that provide primary care to patients with COVID-19 are not only at higher risk of infection but also more vulnerable to mental health. They may experience fear of spreading the virus to others, including their loved ones. An important lesson to be learned from previous experience, such as the prevalence of SARS, is the need for adequate psychological support from health care professionals [9]. Chirico et al. also stated that in medical centers due to high workload, lack of employed personnel, as well as direct exposure to the pathogen COVID-19 and also observing the death of patients without receiving support from relatives, the possibility of depression and burnout in staff employed in these centers is higher [25]. According to a study by Sun et al., conducted on mental health care staffs in hospitals, staff serving quarantine suspects had a higher risk of depression and anxiety, as well as staying away from home for more than 3 days was identified as a risk factor for aggravation of anxiety and stress [26]. In addition, in the studies of Mirzaei Aliabadi et al., the stress factor was identified as an effective and aggravating factor of human error, the presence of which increases the likelihood of human error in the staff [27, 28]. According to Kang et al., medical staff working in Wuhan hospitals in China due to occupational exposure to high risk of infection and inadequate and low protection against infection, high workload, frustration, exposure to patients with negative emotions, long distance from family and fatigue were under a lot of stress which led to mental health problems such as stress, anxiety, depressive symptoms, insomnia, denial, anger and fear. As a result of these psychological problems affects understanding and ability of decision making of the staff occupied in fighting COVID-19, as well as their general health. This study also states that maintaining the mental health of medical staff is effective in controlling the pandemic caused by the disease and their long-term health [29].
With all these conditions, Due to the effect of mental health of medical staff in controlling the pandemic caused by COVID-19 virus, the effect of high stress on the incidence of human error in the staff, less examination of the mental health problems of medical staff during COVID-19 pandemic and also considering the fact that so far, no holistic study is done on occupational stress caused by this disease in these staff in Iran hospitals, the present study is designed to Determining the status of occupational stress in HCWs (including nurses, cleaning crew, physicians) exposed to COVID-19 patients.
2. Materials and methods
2.1. Subjects and sampling method
This cross-sectional descriptive-analytical study was performed on 290 medical staff exposed to COVID-19 patients working in different hospitals in the spring of 2020. Also the study was conducted in hospitals of Kerman province in Iran. All hospitals were COVID-19 related treatment centers. Participants in this study worked in COVID-19 related wards, including the emergency, intensive care unit (ICU), internal medicine and infectious wards. The HCWs were included 180 nurses, 69 hospital cleaning crew and 41 physicians. Sampling method was done randomly. A Simple random sampling was selected to choose participants. In this study, the shift of HCWs was as three times in the morning, three times in the evening and three times in the night. And also, each shift lasted 8 h. Inclusion criteria were willingness to participate in the research and work experience of at least one year. Also, people with less than one year of work experience and people taking anti-anxiety drugs were excluded from the study.
2.2. Study design
Before the experiment, the purpose of the study was fully explained to the subjects. The researchers refused to go to the hospital and talk to the treatment staff participating in the study in order to follow the COVID-19 health protocols, and an electronic version of the questionnaire was sent to the participants via email and WhatsApp social media.
2.3. Data collection tools
Demographic information form and occupational Stress Questionnaire (health and safety executive (HSE) tool indicator) were used to collect the data. The health and safety executive (HSE) questionnaire has 35 questions and 7 areas, which was developed in the 1990s by the British Institute for Health and Safety to measure occupational stress [26]. These seven areas are: 1. Role (correct perception of staff of their organization) with five questions; 2. Communication (increasing practice and positive traits to increase mass communication and reduce conflict and struggle in the workplace) with four questions; 3. Support for managers (the amount of support a person receives from their management and service institution) with five questions; 4. Colleague support (the amount of support a person receives from their colleagues) with four questions; 5. Control (the extent to which could be said that a person is on the way to do his job) with six questions; 6. Demand (including topics such as workload, characteristics and work environment) with eight questions; 7. Changes (how to organize and change the forces of an organization) with three questions. The questions of this questionnaire include a five-point Likert scale including never, rarely, sometimes, often and always which are scored from 1 to 5, respectively [30]. A high score in this questionnaire indicates low and appropriate occupational stress, and a low score indicates a high level of stress. The final stress score according to this questionnaire is divided into 5 categories as follows: very partial stress (score 5), partial stress (score 4), moderate stress (score 3), high stress (score 2), very high stress (Score 1) [31]. Validity and reliability of the Persian version of HSE occupational stress questionnaire was conducted in Marzabadi et al.'s study, the reliability of which, based on Cronbach's alpha coefficient was 78% [32].
2.4. Statistical analysis
Descriptive statistic indices (frequency, percentage, mean and standard deviation) were used to analyze the data. independent t-test and one way ANOVA were used to compare quantitative variables between two groups and for more than two groups, respectively. Data were analyzed using IBM SPSS software version 20 made by SPSS Inc. in USA. The significance level in this study was less than 0.05 (P-value≤ 0.05). And also all variables of present study had a normal distribution.
2.5. Ethics approval and consent to participate
This study was approved at 2020-02-24 as a research project in the ethics committee of Kerman University of Medical Sciences with code number IR.KMU.REC 1399.006. In the present study all participants were above 18 years old and signed an informed consent form prior to taking part in the study.
3. Results
According to power analysis of 80%, a total of 350 questionnaires were sent to different HCWs and then 290 questionnaires were returned. Therefore, the response rate of this study is 83%.
3.1. Demographic information
The demographic information among study groups was indicated in Table 1.
Table 1.
Demographic information of the study groups (N = 290).
| Gender |
Marital Status |
Work experience | Age range | Shift work selection |
Shift work satisfaction |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Single | Married | Obligatory | Voluntary | Yes | No | |||
| Nurses (N = 180) | 100 | 80 | 70 | 110 | 8 ± 5.3 | 29 ± 7.5 | 167 | 13 | 130 | 50 |
| Cleaning crews (N = 69) | 50 | 19 | 32 | 37 | 3 ± 2.1 | 26 ± 3.2 | 53 | 16 | 29 | 40 |
| Physicians (N = 41) | 23 | 18 | 11 | 30 | 16 ± 6.8 | 34 ± 8.3 | 32 | 9 | 35 | 6 |
3.2. Occupational stress assessment
According to the objectives explained above, occupational stress assessment in the present study in the three occupational groups of nurses, cleaning crew and physicians was performed as follows:
3.2.1. Occupational stress assessments of nurses
The results of occupational stress assessment findings in nurses are shown in Table 2. The mean total score of the dimensions among nurses was obtained in the range between moderate to high stress level (2.31). 87% of nurses had low to high levels of occupational stress. There was a significant relationship between the mean score of total dimensions and work experience (p-value = 0.013), type of shift works (p-value = 0.037) and job satisfaction (p-value = 0.013). According to statistical tests in nurses, there was no statistically significant relationship between the mean score of total dimensions with gender, age and marital status (p-value> 0.05). There was a significant relationship between work experience and role (p-value = 0.043). Also, the relationship of manager support with work experience (p-value <0.001), type of shift work (with p-value = 0.04) and work satisfaction (p-value <0.001) was significant. There was also a significant relationship between colleague support and marital status (p-value <0.001). There was a significant relationship between dimensions of control and demand with work experience and type of shift work (p-value <0.001). Finally, results showed that the relationship between work satisfaction with dimension of manager support, demand and control was significant (P-value <0.001).
Table 2.
Mean and standard deviation (SD) of occupational stress score and its dimensions among nurses and effects of occupational factors (n = 180).
| Dimensions of occupational stress | Role | Communication | Manager support | Colleague support | Control | Demand | Changes | Mean score of total dimensions | |
|---|---|---|---|---|---|---|---|---|---|
| Gender | Male | 2.03 ± 0.63 | 2.48 ± 0.86 | 2.37 ± 0.78 | 3.11 ± 0.51 | 2.08 ± 0.51 | 2.14 ± 0.83 | 2.03 ± 0.62 | 2.32 ± 0.71 |
| Female | 2.26 ± 0.58 | 2.23 ± 0.91 | 2.49 ± 0.61 | 2.79 ± 0.46 | 2.17 ± 0.72 | 2.20 ± 0.86 | 2.01 ± 0.68 | 2.30 ± 0.64 | |
| P. Value | 0.059 | 0.065 | 0.411 | 0.064 | 0.608 | 0.632 | 0.637 | 0.208 | |
| Marital status | Single | 2.06 ± 0.64 | 2.46 ± 0.78 | 2.30 ± 0.64 | 2.44 ± 0.76 | 2.01 ± 0.78 | 2.27 ± 0.77 | 1.87 ± 0.62 | 2.20 ± 0.81 |
| Married | 2.19 ± 0.60 | 2.30 ± 0.43 | 2.52 ± 0.82 | 3.30 ± 0.51 | 2.20 ± 0.45 | 2.09 ± 0.92 | 2.13 ± 0.78 | 2.39 ± 0.59 | |
| P. Value | 0.430 | 0.408 | 0.320 | <0.001 | 0.245 | 0.134 | 0.065 | 0.230 | |
| Work experience | 0–10 | 2.21 ± 0.57 | 2.31 ± 0.89 | 2.03 ± 0.41 | 3.02 ± 0.58 | 2.39 ± 0.84 | 2.01 ± 0.69 | 2.02 ± 0.74 | 2.28 ± 0.76 |
| 10–20 | 1.96 ± 0.61 | 2.42 ± 0.81 | 2.33 ± 0.80 | 2.96 ± 0.63 | 1.94 ± 0.70 | 2.04 ± 0.64 | 2.03 ± 0.61 | 2.24 ± 0.74 | |
| 20–30 | 2.19 ± 0.65 | 2.35 ± 0.76 | 2.95 ± 0.83 | 2.96 ± 0.75 | 2.03 ± 0.72 | 2.43 ± 0.78 | 2.01 ± 0.49 | 2.41 ± 0.69 | |
| P. Value | 0.043 | 0.530 | <0.001 | 0.110 | <0.001 | <0.001 | 0.740 | 0.013 | |
| Age range | 20–30 | 2.08 ± 0.62 | 2.54 ± 0.92 | 2.41 ± 0.81 | 3.2 ± 0.83 | 2.14 ± 0.67 | 2.29 ± 0.75 | 2.07 ± 0.59 | 2.39 ± 0.51 |
| 30–40 | 2.20 ± 0.70 | 2.31 ± 0.58 | 2.45 ± 0.74 | 2.91 ± 0.41 | 2.09 ± 0.61 | 2.11 ± 0.78 | 2.11 ± 0.67 | 2.31 ± 0.85 | |
| 40–50 | 2.11 ± 0.61 | 2.23 ± 0.76 | 2.43 ± 0.49 | 2.77 ± 0.79 | 2.13 ± 0.81 | 2.08 ± 0.64 | 1.93 ± 0.60 | 2.24 ± 0.73 | |
| P. Value | 0.320 | 0.170 | 0.760 | 0.470 | 0.713 | 0.132 | 0.420 | 0.650 | |
| Shift work selection | Voluntary | 2.32 ± 0.78 | 2.57 ± 0.63 | 3.00 ± 0.84 | 2.73 ± 0.63 | 2.77 ± 0.91 | 2.95 ± 0.88 | 2.08 ± 0.82 | 2.63 ± 0.89 |
| Obligatory | 2.12 ± 0.61 | 2.35 ± 0.93 | 2.39 ± 0.37 | 2.98 ± 0.76 | 2.07 ± 0.48 | 2.10 ± 0.61 | 2.02 ± 0.49 | 2.29 ± 0.72 | |
| P. Value | 0.132 | 0.091 | 0.040 | 0.210 | <0.001 | <0.001 | 0.420 | 0.037 | |
| work satisfaction | Yes | 2.17 ± 0.67 | 2.39 ± 0.87 | 2.70 ± 0.58 | 3.01 ± 0.78 | 2.42 ± 0.68 | 2.46 ± 0.38 | 2.04 ± 0.92 | 2.45 ± 0.51 |
| No | 2.06 ± 0.51 | 2.30 ± 0.73 | 1.75 ± 0.73 | 2.85 ± 0.77 | 1.34 ± 0.63 | 1.40 ± 0.69 | 2.00 ± 0.84 | 1.95 ± 0.64 | |
| P. Value | 0.380 | 0.580 | <0.001 | 0.140 | <0.001 | <0.001 | 0.690 | 0.013 | |
Significance level was considered as p-value <0.05.
3.2.2. Occupational assessment of cleaning crew
Table 3 shows the results of the occupational stress assessment findings among the cleaning crew of COVID-19 sections. The mean score of total dimensions among the cleaning crew was 2.91 which were in the range between moderate and high stress level and also 79% of the participants had a slight to high stress level. There is a statistically significant relationship between the mean score of total dimensions of occupational stress with type of shift work (p-value <0.001) and job satisfaction (p-value = 0.02). However, the study of statistical tests in the cleaning crew showed that there is no statistically significant relationship between the mean score of total dimensions with gender, age and marital status and work experience (P > 0.05). There was a significant relationship between communications and work experience (p-value <0.001). There was also a significant relationship between the dimension of manager support and type of work shift (p-value <0.001). In addition, there was a significant correlation between colleague support and work experience and the type of work shift (p-value <0.001). And also, There was a significant correlation between control and age (p-value <0.001).
Table 3.
Mean and standard deviation (SD) of occupational stress score and its dimensions among the cleaning crew group and effects of occupational factors (n = 69).
| Dimensions of occupational stress | Role | Communication | Manager support | Colleague support | Control | Demand | Changes | Mean score of total dimensions | |
|---|---|---|---|---|---|---|---|---|---|
| Gender | Male | 3.25 ± 0.41 | 2.77 ± 0.73 | 2.06 ± 0.79 | 3.88 ± 0.90 | 2.94 ± 0.85 | 2.94 ± 0.87 | 3.05 ± 0.20 | 2.98 ± 0.54 |
| Female | 2.93 ± 0.67 | 2.75 ± 0.66 | 1.92 ± 0.58 | 3.86 ± 0.83 | 3.13 ± 0.74 | 2.76 ± 0.40 | 2.81 ± 0.44 | 2.88 ± 0.64 | |
| P. Value | 0.059 | 0.650 | 0.450 | 0.765 | 0.451 | 0.342 | 0.231 | 0.430 | |
| Marital status | Single | 3.26 ± 0.37 | 2.83 ± 0.59 | 1.92 ± 0.44 | 3.99 ± 0.99 | 2.93 ± 0.87 | 3.02 ± 0.78 | 2.99 ± 0.35 | 2.99 ± 0.66 |
| Married | 3.04 ± 0.72 | 2.70 ± 0.81 | 2.11 ± 0.57 | 3.77 ± 0.80 | 3.05 ± 0.66 | 2.78 ± 0.89 | 2.98 ± 0.39 | 2.91 ± 0.34 | |
| P. Value | 0.081 | 0.341 | 0.128 | 0.087 | 0.470 | 0.076 | 0.613 | 0.067 | |
| Work experience | 0–10 | 3.22 ± 0.42 | 2.70 ± 0.91 | 1.90 ± 0.30 | 3.35 ± 0.82 | 2.83 ± 0.69 | 2.99 ± 0.67 | 3.08 ± 0.41 | 2.86 ± 0.74 |
| 10–20 | 3.20 ± 0.81 | 2.17 ± 0.73 | 2.10 ± 0.45 | 4.13 ± 0.91 | 2.04 ± 0.89 | 2.73 ± 0.79 | 2.82 ± 0.46 | 2.74 ± 0.48 | |
| 20–30 | 3.00 ± 0.64 | 3.41 ± 0.62 | 1.82 ± 0.50 | 3.35 ± 0.72 | 2.95 ± 0.79 | 2.95 ± 0.77 | 3.04 ± 0.38 | 2.93 ± 0.32 | |
| P. Value | 0.564 | <0.001 | 0.065 | <0.001 | 0.390 | 0.069 | 0.054 | 0.107 | |
| Age range | 20–30 | 3.29 ± 0.42 | 2.80 ± 0.78 | 2.10 ± 0.61 | 3.70 ± 0.53 | 2.75 ± 0.64 | 2.90 ± 0.66 | 3.01 ± 0.45 | 2.93 ± 0.56 |
| 30–40 | 3.03 ± 0.78 | 2.62 ± 0.75 | 1.66 ± 0.23 | 4.01 ± 0.88 | 3.53 ± 0.87 | 2.88 ± 0.54 | 2.83 ± 0.51 | 2.93 ± 0.71 | |
| 40–50 | 3.09 ± 0.77 | 2.86 ± 0.63 | 2.30 ± 0.25 | 3.90 ± 0.91 | 2.69 ± 0.69 | 2.89 ± 0.87 | 3.10 ± 0.33 | 2.97 ± 0.35 | |
| P. Value | 0.087 | 0.069 | 0.032 | 0.098 | <0.001 | 0.871 | 0.091 | 0.453 | |
| Shift work selection | Voluntary | 3.26 ± 0.63 | 2.89 ± 0.47 | 2.64 ± 0.33 | 4.09 ± 0.65 | 2.97 ± 0.78 | 3.06 ± 0.83 | 3.18 ± 0.65 | 3.19 ± 0.25 |
| Obligatory | 3.10 ± 0.80 | 2.70 ± 082 | 1.84 ± 0.37 | 3.13 ± 0.79 | 2.99 ± 0.90 | 2.84 ± 0.87 | 2.92 ± 0.42 | 2.78 ± 0.36 | |
| P. Value | 0.065 | 0.013 | <0.001 | <0.001 | 0.780 | 0.091 | 0.169 | <0.001 | |
| work satisfaction | Yes | 3.21 ± 0.65 | 2.89 ± 0.52 | 2.54 ± 0.51 | 4.30 ± 0.97 | 3.08 ± 0.73 | 3.58 ± 0.64 | 2.99 ± 0.63 | 3.22 ± 0.46 |
| No | 3.09 ± 0.67 | 2.67 ± 78 | 1.65 ± 0.37 | 3.29 ± 0.77 | 2.93 ± 0.88 | 2.39 ± 0.87 | 2.98 ± 0.21 | 2.71 ± 0.29 | |
| P. Value | 0.470 | 0.320 | <0.001 | <0.001 | 0.066 | <0.001 | 0.770 | 0.020 | |
Significance level was considered as p-value <0.05.
3.2.3. Occupational stress assessment of physicians
The results of occupational stress assessment findings in COVID-19 physicians can be seen in Table 4. The mean score of total dimensions among physicians was 3.53 which showed that the level of stress among physicians was between low and moderate stress levels. The results also showed that 69% of physicians had moderate to high levels of stress. There is a statistically significant relationship between the mean score of total dimensions in physicians with work experience (p-value = 0.004) and job satisfaction (p-value <0.001). However, according to the statistical study, there is no statistically significant relationship between the mean score of total dimensions of occupational stress with gender, age and marital status (p-value> 0.05). In addition, there was a significant relationship between the communication dimension and age (p-value <0.001). There was also a significant relationship between manager support and the type of work shift (p-value <0.001). There was a significant relationship between colleague support and marital status (p-value = 0.0001). In addition, a significant relationship was observed between control dimension and type of work shift (p-value <0.001). And also, the relationship between demand and work experience was significant (p-value <0.001).
Table 4.
Mean and standard deviation (SD) of occupational stress score and its dimensions among physicians and effects of occupational factors (n = 41).
| Dimensions of occupational stress | Role | Communication | Manager support | Colleague support | Control | Demand | Changes | Mean score of total dimensions | |
|---|---|---|---|---|---|---|---|---|---|
| Gender | Male | 3.64 ± 0.61 | 3.06 ± 0.69 | 3.94 ± 0.74 | 3.42 ± 0.15 | 3.66 ± 0.74 | 3.62 ± 0.90 | 3.56 ± 0.71 | 3.55 ± 0.60 |
| Female | 3.48 ± 0.93 | 3.30 ± 0.88 | 3.79 ± 0.53 | 3.20 ± 0.26 | 3.89 ± 0.81 | 3.50 ± 0.71 | 3.41 ± 0.76 | 3.51 ± 0.80 | |
| P. Value | 0.059 | 0.065 | 0.320 | 0.087 | 0.087 | 0.430 | 0.360 | 0.190 | |
| Marital status | Single | 3.57 ± 0.76 | 3.16 ± 0.93 | 3.71 ± 0.79 | 3.95 ± 0.16 | 3.60 ± 0.88 | 3.39 ± 0.91 | 3.48 ± 0.75 | 3.55 ± 0.51 |
| Married | 3.56 ± 0.90 | 3.15 ± 0.83 | 3.93 ± 0.63 | 3.10 ± 0.18 | 3.82 ± 0.71 | 3.63 ± 0.88 | 3.49 ± 0.73 | 3.54 ± 0.76 | |
| P. Value | 0.670 | 0.910 | 0.180 | <0.001 | 0.130 | 0.180 | 0.790 | 0.910 | |
| Work experience | 0–10 | 3.56 ± 0.94 | 3.15 ± 0.74 | 3.96 ± 0.54 | 3.30 ± 0.12 | 3.76 ± 0.63 | 2.20 ± 0.85 | 3.35 ± 0.79 | 3.32 ± 0.74 |
| 10–20 | 3.52 ± 0.85 | 3.16 ± 0.91 | 3.85 ± 0.78 | 3.44 ± 0.32 | 3.75 ± 0.70 | 4.90 ± 0.91 | 3.46 ± 0.80 | 3.72 ± 0.43 | |
| 20–30 | 3.60 ± 0.76 | 3.17 ± 0.85 | 3.80 ± 0.66 | 3.22 ± 0.10 | 3.77 ± 0.80 | 3.58 ± 0.70 | 3.65 ± 0.60 | 3.54 ± 0.80 | |
| P. Value | 0.470 | 0.780 | 0.430 | 0.390 | 0.810 | <0.001 | 0.470 | 0.004 | |
| Age range | 20–30 | 3.63 ± 0.88 | 4.00 ± 0.90 | 3.65 ± 0.44 | 3.22 ± 0.31 | 3.76 ± 0.89 | 3.52 ± 0.61 | 3.49 ± 0.61 | 3.61 ± 0.89 |
| 30–40 | 3.56 ± 0.86 | 3.10 ± 0.89 | 3.91 ± 0.83 | 3.32 ± 0.41 | 3.75 ± 0.51 | 3.71 ± 0.80 | 3.41 ± 0.72 | 3.53 ± 0.45 | |
| 40–50 | 3.49 ± 0.91 | 3.29 ± 0.85 | 4.05 ± 0.70 | 3.42 ± 0.23 | 3.77 ± 0.63 | 3.65 ± 0.89 | 3.57 ± 0.79 | 3.60 ± 0.72 | |
| P. Value | 0.340 | <0.001 | 0.081 | 0.180 | 0.780 | 0.540 | 0.310 | 0.380 | |
| Shift work selection | Voluntary | 3.71 ± 0.61 | 3.32 ± 0.88 | 3.02 ± 0.80 | 3.51 ± 0.21 | 2.98 ± 0.74 | 3.71 ± 0.71 | 3.60 ± 0.80 | 3.32 ± 0.76 |
| Obligatory | 3.52 ± 0.90 | 3.12 ± 0.76 | 4.11 ± 0.61 | 3.27 ± 0.16 | 3.98 ± 0.79 | 3.52 ± 0.84 | 3.46 ± 0.71 | 3.56 ± 0.61 | |
| P. Value | 0.091 | 0.083 | <0.001 | 0.068 | <0.001 | 0.080 | 0.430 | <0.001 | |
| work satisfaction | Yes | 3.57 ± 0.68 | 3.19 ± 0.77 | 4.00 ± 0.39 | 3.35 ± 0.15 | 3.60 ± 0.59 | 3.56 ± 0.55 | 3.52 ± 0.59 | 3.54 ± 0.69 |
| No | 3.49 ± 0.93 | 2.98 ± 0.89 | 3.10 ± 0.81 | 3.13 ± 0.23 | 4.70 ± 0.81 | 2.48 ± 0.89 | 3.34 ± 0.81 | 3.31 ± 0.72 | |
| P. Value | 0.570 | 0.081 | <0.001 | 0.072 | <0.001 | <0.001 | 0.089 | <0.001 | |
Significance level was considered as p-value <0.05.
3.2.4. Comparison of occupational stress among study groups
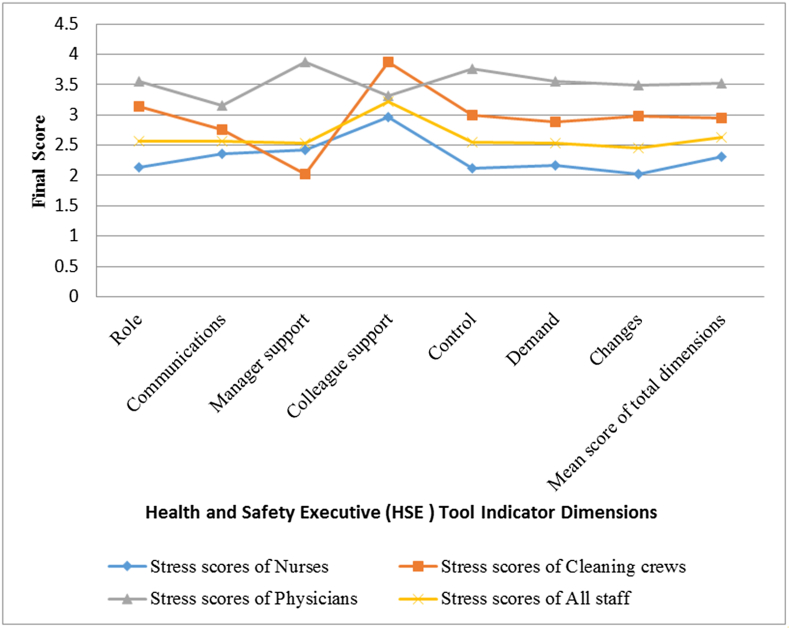
Table 5 presents the final stress scores in the occupational groups participating in this study that obtained from the HSE tool indicator. Besides that, in Figure 1 the scores f HSE questionnaire dimensions and means score of total dimensions were compared. As indicated in figure, the nurses group in comparison to the other two groups obtained lower scores in all dimensions (except for the support of colleagues). Therefore, it can be stated that the level of stress in this group was higher than others. Also, according to Figure 1, the group of physicians had the lowest level of stress in this study due to obtaining higher scores in most dimensions. The mean score of total dimensions in all study groups was 2.63, which indicates moderate to high stress levels among study participants.
Table 5.
Final scores of health and safety executive (HSE) tool indicator dimensions among study groups.
| HSE tool indicators Dimensions | Nurses |
Cleaning crew |
physicians |
All staff |
||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Role | 2.13 | 0.618 | 3.14 | 0.250 | 3.56 | 0.890 | 2.57 | 0.568 |
| Communications | 2.36 | 0.873 | 2.76 | 0.770 | 3.16 | 0.870 | 2.56 | 0.848 |
| Manager support | 2.43 | 0.744 | 2.02 | 0.340 | 3.87 | 0.690 | 2.53 | 0.640 |
| Colleague support | 2.96 | 0.496 | 3.87 | 0.960 | 3.32 | 0.180 | 3.22 | 0.561 |
| Control | 2.12 | 0.522 | 2.99 | 0.820 | 3.76 | 0.760 | 2.55 | 0.626 |
| Demand | 2.16 | 0.847 | 2.89 | 0.650 | 3.56 | 0.830 | 2.53 | 0.797 |
| Changes | 2.02 | 0.675 | 2.98 | 0.300 | 3.49 | 0.740 | 2.45 | 0.594 |
| Mean score of total dimensions | 2.31 | 0.670 | 2.95 | 0.580 | 3.53 | 0.700 | 2.63 | 0.652 |
Figure 1.
Comparison score of health and safety executive (HSE) tool indicator dimensions in study groups.
4. Discussion
The aim of this study was to assess occupational stress among HCWs exposed to COVID-19 patients in selected wards of three hospitals in of the cities in Iran. For this aim, the demographic information form and the questionnaire of the British HSE indicator tool were used. According to the results, the mean total score of the dimensions obtained by the nurses, cleaning crew, physicians was 2.31, 2.95 and 3.53, respectively. The results showed a higher level of stress in nurses compared to the cleaning crew and physicians. Accordingly, the stress level of the cleaning crew is higher compared to doctors. Besides that, the mean total score of the dimensions obtained by all occupational was 2.93 which indicate the level of stress between moderate to high levels among HCWs. Among nurses, the lowest score is obtained for changes (2.02) and also the scores related to control (2.12), role (2.13) and demand (2.16) have low values. Although the score related to the dimension of manager support (2.43) has a higher value compared to other dimensions, but it is still at the red level (stress level between medium and high) and shows its effect on stress levels in this occupational group. In the cleaning crew, the lowest score obtained was related to manager support (2.02), which had the main effect on the stress level of this job group. In this occupational group, the score obtained in the dimensions of communication (2.76), demand (2.89) and changes (2.98) also have lower values compared to other dimensions. In the physicians, the lowest score obtained was related to the dimension of communication (3.16). Also, the scores related to changes (3.49) and role (3.56) and control (3.76) were at a low level. Furthermore, the highest score obtained is related to the manager support (3.87) and shows the high support of managers in this occupational group. Hence, one of the reasons for obtaining a higher score and lower stress level of physicians compared with nurses and cleaning crews was manager support.
In a study conducted by Akbari et al., the mean final stress score obtained by the nurses was 3.17, which was in the range of partial to moderate stress [33]. It seems that the reason for the difference between the two studies is the effect of critical conditions caused by COVID-19 such as lack of previous familiarity with the disease (newness), direct exposure to previously unexperienced infectious disease, and lack of access to adequate personal protective equipment for nurses in the present study.
In the study by Cedrone et al. [34] performed on neurophysiological technicians the mean score of stress was 3.74. which was same with the results of present study. Also, In the Cedrone et al. study [30], the scores related to communication and role were 4.01 and 4.35, respectively. This was different with present study. It seems the difference is caused by the existence of stressful conditions, lack of familiarity with critical conditions induced by the pandemic, as well as lack of proper allocation of roles by higher managers in critical situations due to the outbreak of COVID-19 in the present study.
According to a study conducted by Khanam et al., the increase in government and manager support was identified as a factor in reducing the stress of COVID-19 outbreaks at the frontline of the fight against the virus [35] In addition, other previous studies confirm the effect of support, including manager, colleague, and even family support on staff stress and mental health levels [34, 36, 37, 38]. These studies results were same with the results of present study.
Demand is recognized as an aspect of the job that is difficult for an employee to achieve. These aspects can be named as workload, work response speed, and work environment conditions. One of the reasons for the low scores and also high stress level obtained by the occupational groups of this study (especially nurses and cleaning crews), were high workload and the need for high response speed and inappropriate working environment conditions compared to the conditions before COVID-19 pandemic. The results are consistent with previous studies performed on radiology staff [39, 40] Also the results are consistent with a study by Eisapareh et al. [41], which states that social support is effective in reducing stress.
In the of Hosseinabadi et al. study, which was performed on nurses, a significant correlation was found between different dimensions of occupational stress (demand, control, support, etc.) and job satisfaction [42]. Also in this study, there was a significant correlation between the mean dimension score and job satisfaction in all occupational groups and the results showed that job satisfaction has an effect on the stress level.
In this study, in the group of nurses and physicians, there is a significant relationship between the mean total score of dimensions with work experience and job satisfaction and this correlation is a positive correlation in the sense that with increasing work experience and job satisfaction, the mean total score of dimensions increases and indicates a reduction in stress levels in them. Also in the cleaning crew, there is a significant relationship between the mean total score of dimensions and job satisfaction. Accordingly, in the study of Kerr et al., which was conducted on occupational stress of jobs related to health and social services, a positive correlation was observed between the final score of the HSE questionnaire and job satisfaction [43] Also in the study of Ferrie et al., a positive correlation was observed between different parts of the HSE questionnaire (such as role and changes) and mental health [44] Which are in consistent with findings.
In accordance to the results, 87% of nurses, 79% of the cleaning crew and 67% of physicians had partial to high stress levels, with a mean of 77.5% of the medical staff participating in this study had at least a partial amount of stress. This level of stress can be due to the high workload and the resulting high work pressure on personnel compared to pre-pandemic conditions, direct exposure to the risks of COVID-19 and also the fear of transmitting the disease to them. In studies by Bao et al., Lai et al and Carmassi et al. [44, 45, 46, 47] they stated that HCWs who work in the field of diagnosis, treatment, and care of COVID-19 patients, are facing a high risk of stress and spiritual and psychological problems caused by them; which are completely consistent with the results of the present study. Also in the study of Lai et al. [46] who examined the level of stress in the HCWS (including nurses and physicians) exposed to COVID-19 patients in Wuhan, China, about 71.5% of participants had partial to high stress levels. The results were similar to the results of the present study. Also, in the study performed on the frontline health care workers (FHCWs) of the fight against COVID-19, it was stated that the level of stress in the occupational group of nurses was higher than that of physicians [35], which is consistent with the results of the present study. In addition, in a study by Khalid et al., which was performed on HCWs (including nurses, physicians, and respiratory therapists) exposed to MERS-CoV, stress was divided into four levels of very low (score 0), partial (score 1), and moderate (score 2) and very high (score 3), which the mean score of the participants in this study was about 2.43 (moderate to very high stress level) [48]. The mean stress score obtained by all job groups in the present study was 2.63 (moderate to high stress level), which shows a close similarity with the study of Khalid et al.
The main advantage of the present study is the assessment of occupational stress caused by COVID-19 pandemic conditions for the first time in Iran, which was used to achieve this goal of the HSE questionnaire. The advantages of this questionnaire include low number of questions, use of appropriate dimensions for occupational stress assessment, standard occupational stress assessment and high level of validity and reliability. These features make this questionnaire a convenient tool for assessing staff conditions. Thus, this tool allows the researcher to quickly assess occupational stress in critical situations in order to help make subsequent decisions. Among the limitation of this study are the problems with the Hospitals and not cooperating of some HCWs in filling questionnaire. However, an attempt was made to involve a large number of staff in the studied hospitals.
5. Conclusion
According to our findings, mean score of total dimensions was 2.93, which indicates the stress level between high stress to moderate stress. The factors such as Communications, Manager support, Changes and Demand with scores of 2.76, 2.77, 2.83 and 2.87 had the greatest impact on participants' stress levels, respectively. Colleague support with a final score of 3.38 had the least effect on stress levels in all three occupational groups. Therefore, by improving the communication between people working in hospitals, increasing managers' support for staff and reducing workplace demands such as reducing workload and improving workplace conditions, staff stress levels in hospitals can be reduced during the outbreak of COVID-19. Accordingly, It seems factors such as high workload, low response time at the peak of hospital visits, lack of adequate support from top managers of all job groups equally, lack of access to adequate personal protective equipment, unpreparedness of managers and staff to respond to the critical and emergency situations influenced stress level among participants. Due to the possibility of recurrence of COVID-19 peak and re-increase of involvement of medical staff, preparation of work environment conditions as well as staff to respond to COVID-19 emergencies (also due to the recent outbreak of a new type of coronavirus in the UK) is one of the requirements in medical centers. Therefore, the results of this study can be used as a reference for further measures, including the implementation of interventions during the pandemic to reduce occupational stress and maintain work stability and increase the quality of life of medical staff.
Declarations
Author contribution statement
Sajad Zare: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data.
Moslem Mohammadi Dameneh, Sahar Naseri: Performed the experiments.
Reza Esmaeili: Analyzed and interpreted the data; Wrote the paper.
Reza Kazemi: Contributed reagents, materials, analysis tools or data.
Davoud Panahi: Analyzed and interpreted the data.
Funding statement
This work was supported by Kerman University of Medical Sciences (99000002).
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We are deeply grateful of Clinical Research Development Unit of Afzalipour Hospital at Kerman University of Medical Sciences.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020 Jan 24 doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones R.M. Relative contributions of transmission routes for COVID-19 among healthcare personnel providing patient care. J. Occup. Environ. Hyg. 2020 Jul 8;17(9):408–415. doi: 10.1080/15459624.2020.1784427. [DOI] [PubMed] [Google Scholar]
- 3.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S., Lau E.H., Wong J.Y., Xing X. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020 Jan 29 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2020. WHO COVID-19 Preparedness and Response Progress Report-1 February to 30 June 2020. [Google Scholar]
- 5.Ministry of Health and Medical Education, Public Relations and Information Center . MoHME; Tehran: 2020. Death of Two Patient with New Coronavirus in Qom.https://cutt.ly/etW0SIQ [updated 2020 Feb 19; cited 2020 Feb 19]. Available from: [Google Scholar]
- 6.Raoofi A., Takian A., Sari A.A., Olyaeemanesh A., Haghighi H., Aarabi M. COVID-19 pandemic and comparative health policy learning in Iran. Arch. Iran. Med. 2020 Apr 5;23(4):220–234. doi: 10.34172/aim.2020.02. [DOI] [PubMed] [Google Scholar]
- 7.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020 Feb 26:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lancet T. COVID-19: protecting health-care workers. Lancet. 2020 Mar 21;395(10228):922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith G.D., Ng F., Li W.H. COVID-19: emerging compassion, courage and resilience in the face of misinformation and adversity. J. Clin. Nurs. 2020 May;29(9-10):1425. doi: 10.1111/jocn.15231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Q., Luo D., Haase J.E., Guo Q., Wang X.Q., Liu S., Xia L., Liu Z., Yang J., Yang B.X. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Global Health. 2020 Apr 29 doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . Vol. 19. World Health Organization, Interim guidance; 2020 Mar. Coronavirus Disease (COVID-19) Outbreak: Rights, Roles and Responsibilities of Health Workers, Including Key Considerations for Occupational Safety and Health. [Google Scholar]
- 12.Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatr. 2020 Apr 1;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aziziaram S., Basharpoor S. The role of rumination, emotion regulation and responsiveness to stress in predicting of Corona anxiety (COVID-19) among nurses. Q. J. Nurs. Manag. 2020 Oct 10;9(3):8–18. [Google Scholar]
- 14.Starcke K., Brand M. Decision making under stress: a selective review. Neurosci. Biobehav. Rev. 2012 Apr 1;36(4):1228–1248. doi: 10.1016/j.neubiorev.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Nanda A., Soelton M., Luiza S., Saratian E.T. 4th International Conference on Management, Economics and Business (ICMEB 2019) Atlantis Press; 2020 Feb 12. The effect of psychological work environment and work loads on turnover interest, work stress as an intervening variable; pp. 225–231. [Google Scholar]
- 16.Zare S., Hemmatjo R., Allahyari T., Hajaghazadeh M., Hajivandi A., Aghabeigi M., Kazemi R. Comparison of the effect of typical firefighting activities, live fire drills and rescue operations at height on firefighters’ physiological responses and cognitive function. Ergonomics. 2018 Oct 3;61(10):1334–1344. doi: 10.1080/00140139.2018.1484524. [DOI] [PubMed] [Google Scholar]
- 17.Wu S., Zhu W., Wang Z., Wang M., Lan Y. Relationship between burnout and occupational stress among nurses in China. J. Adv. Nurs. 2007 Aug;59(3):233–239. doi: 10.1111/j.1365-2648.2007.04301.x. [DOI] [PubMed] [Google Scholar]
- 18.Najafi Ghezeljeh T., Moradi F., Rafii F., Haghani H. Relationship between job stress, sleep quality and fatigue in nurses. Iran J. Nurs. 2014 Aug;27(89):40–49. [Google Scholar]
- 19.Khaghanizadeh M., Ebadi A., Cirati nair M., Rahmani M. The study of relationship between job stress and quality of work life of nurses in military hospitals. J. Mil. Med. 2008;10(3):175–184. [Google Scholar]
- 20.Reardon M., Abrahams R., Thyer L., Simpson P. Prevalence of burnout in paramedics: a systematic review of prevalence studies. Emerg. Med. Australasia (EMA) 2020 Apr;32(2):182–189. doi: 10.1111/1742-6723.13478. [DOI] [PubMed] [Google Scholar]
- 21.Begat I., Ellefsen B., Severinsson E. Nurses’ satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses’ experiences of well-being–a Norwegian study. J. Nurs. Manag. 2005 May;13(3):221–230. doi: 10.1111/j.1365-2834.2004.00527.x. [DOI] [PubMed] [Google Scholar]
- 22.Nassiri P., Zare S., Monazzam M.R., Pourbakht A., Azam K., Golmohammadi T. Evaluation of the effects of various sound pressure levels on the level of serum aldosterone concentration in rats. Noise Health. 2017 Jul;19(89):200. doi: 10.4103/nah.NAH_64_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zare S., Baneshi M.R., Hemmatjo R., Ahmadi S., Omidvar M., Dehaghi B.F. The effect of occupational noise exposure on serum cortisol concentration of night-shift industrial workers: a field study. Safety Health Work. 2019 Mar 1;10(1):109–113. doi: 10.1016/j.shaw.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zare S., Shirvan H.E., Hemmatjo R., Nadri F., Jahani Y., Jamshidzadeh K., Paydar P. A comparison of the correlation between heat stress indices (UTCI, WBGT, WBDT, TSI) and physiological parameters of workers in Iran. Weather Clim. Extrem. 2019 Dec 1;26:100213. [Google Scholar]
- 25.Chirico F., Nucera G., Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych Int. 2020:1–2. [Google Scholar]
- 26.Sun Y., Song H., Liu H., Mao F., Sun X., Cao F. Occupational stress, mental health, and self-efficacy among community mental health workers: a cross-sectional study during COVID-19 pandemic. Int. J. Soc. Psychiatr. 2020 Nov 11 doi: 10.1177/0020764020972131. 0020764020972131. [DOI] [PubMed] [Google Scholar]
- 27.Mirzaei Aliabadi M., Esmaeili R., Mohammadfam I., Ashrafi M. Human reliability analysis (HRA) using standardized plant analysis risk-human (SPAR-H) and Bayesian network (BN) for pipeline inspection gauges (PIG) operation: a case study in a gas transmission plant. Health Scope. 2019 Aug 31;8(3) [Google Scholar]
- 28.Aliabadi M.M., Esmaeili R., Mohammadfam I., Ashrafi M. Application of a standardized plant analysis risk-human reliability method to pipeline inspection gauge operations. J. Occup. Hyg. Eng. 2019;6(3):34–43. [Google Scholar]
- 29.Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., Wang Y., Hu J., Lai J., Ma X., Chen J. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatr. 2020 Mar 1;7(3):e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cousins R., Mackay C.J., Clarke S.D., Kelly C., Kelly P.J., McCaig R.H. ‘Management standards’ work-related stress in the UK: practical development. Work. Stress. 2004 Apr 1;18(2):113–136. [Google Scholar]
- 31.Sharafi H., Gholami P., Sadeghi S., Ghorbani M., Rezaei F. Job stress and related factors among staff of the operation room in Bandar Abbas. Iran. IJRN. 2018 Feb 10;4(2):29–34. [Google Scholar]
- 32.Marzabadi E.A., Fesharaki M. Reliability and validity assessment for the HSE job stress questionnaire. Int. J. Behav. Sci. 2011;4(4):291–297. [Google Scholar]
- 33.Akbari H., Satkin M., Gangi M., Akbari H., Gholami Fesharaki M. Standardization and study of psychological properties of the HSE stress questionnaire. Iran. Red Crescent Med. J. 2017;19(3) [Google Scholar]
- 34.Cedrone F., Lungo F., Feliciangeli A., Muccino F., Greco E. The perception of psychosocial risks through the HSE questionnaire of a population of neurophysiology technicians: a cross-sectional study. La Clinica Terapeutica. 2018;169(6):e281–6. doi: 10.7417/CT.2018.2094. [DOI] [PubMed] [Google Scholar]
- 35.Khanam A., Dar S.A., Wani Z.A., Shah N.N., Haq I., Kousar S. Healthcare providers on the frontline: a quantitative investigation of the stress and recent onset psychological impact of delivering health care services during COViD-19 in Kashmir. Indian J. Psychol. Med. 2020 Jul;42(4):359–367. doi: 10.1177/0253717620933985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van der Doef M., Maes S. The job demand-control (-support) model and psychological well-being: a review of 20 years of empirical research. Work. Stress. 1999 Apr 1;13(2):87–114. [Google Scholar]
- 37.Gerberich S.G., Church T.R., McGovern P.M., Hansen H.E., Nachreiner N.M., Geisser M.S., Ryan A.D., Mongin S.J., Watt G.D. An epidemiological study of the magnitude and consequences of work related violence: the Minnesota Nurses’ Study. Occup. Environ. Med. 2004 Jun 1;61(6):495–503. doi: 10.1136/oem.2003.007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gholami Fesharaki M., Aghamiri Z., Mohamadian M., Habibi M., Anvari S.S., Azad Marzabad E.I. Effect of manager leadership behavior and demographical factors on job satisfaction of military healthcare personnel. J. Mil Med. 2013 Apr 10;15(1):37–42. [Google Scholar]
- 39.Nayak K., Kumar N., Panakkal N.C. Occupational stress among radiographers working in tertiary care hospital in Udupi and Mangalore. Medico legal update. 2020 Nov 18;20(4):281–285. [Google Scholar]
- 40.Gam N.P. 2015. Occupational Stressors in Diagnostic Radiographers Working in Public Health Facilities in the eThekwini District of KwaZulu-Natal (Doctoral Dissertation) [Google Scholar]
- 41.Eisapareh K., Nazari M., Kaveh M.H., Ghahremani L. The relationship between job stress and health literacy with the quality of work life among Iranian industrial workers: the moderating role of social support. Curr. Psychol. 2020 May 14:1–9. [Google Scholar]
- 42.Hosseinabadi M.B., Etemadinezhad S. Evaluating the relationship between job stress and job satisfaction among female hospital nurses in Babol: an application of structural equation modeling. Health Promot. Perspect. 2018;8(2):102. doi: 10.15171/hpp.2018.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kerr R., McHugh M., McCrory M. HSE Management Standards and stress-related work outcomes. Occup. Med. 2009 Dec 1;59(8):574–579. doi: 10.1093/occmed/kqp146. [DOI] [PubMed] [Google Scholar]
- 44.Ferrie J.E., Shipley M.J., Marmot M.G., Stansfeld S., Smith G.D. The health effects of major organisational change and job insecurity. Soc. Sci. Med. 1998 Jan 1;46(2):243–254. doi: 10.1016/s0277-9536(97)00158-5. [DOI] [PubMed] [Google Scholar]
- 45.Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020 Feb 22;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020 Mar 2;3(3) doi: 10.1001/jamanetworkopen.2020.3976. e203976-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carmassi C., Cerveri G., Bui E., Gesi C., Dell’Osso L. Defining effective strategies to prevent post-traumatic stress in healthcare emergency workers facing the COVID-19 pandemic in Italy. CNS Spectr. 2020 Jul 14:1–2. doi: 10.1017/S1092852920001637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khalid I., Khalid T.J., Qabajah M.R., Barnard A.G., Qushmaq I.A. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin. Med. Res. 2016 Mar 1;14(1):7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.