Abstract
High blood pressure awareness, advice received from health care providers, and adoption of heart‐healthy behaviors were assessed using the Healthstyles 2002 survey. About 20% of respondents reported that they had high blood pressure, and 53% of these were currently taking medications to lower blood pressure. Black men had the highest adjusted prevalence of high blood pressure (32%). Medication use among persons with high blood pressure was lower among Hispanics (45%) than among blacks (54%) and whites (54%). Persons reporting having high blood pressure were five times more likely to report having received advice from a health care professional to go on a diet or change eating habits (p<0.05) and reduce salt or sodium in their diet (p<0.05), but five times less likely to have received advice to exercise (p<0.05) than those reporting not having high blood pressure, after adjustment for differences in sex, race/ethnicity, and age. Persons with self‐reported high blood pressure were also more likely to be making these modifications (p<0.05). Among people with high blood pressure, current medication use was associated with both receiving and following advice for diet change and salt reduction (p<0.05). Future initiatives are needed to improve the proportion of Hispanics and blacks taking prescribed medications to improve high blood pressure control and reduce risk for serious sequelae such as heart disease and stroke.
Hypertension awareness, treatment, and control have improved during the 30‐year period between 1960 and 1991 1 but, unfortunately, most hypertensive individuals still do not have their blood pressure (BP) under control. 2 , 3 High blood pressure (HBP) is a major risk factor for heart disease, stroke, end‐stage renal disease, and peripheral vascular disease, as well as a contributor to adult disability. 3 The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) 2 defines hypertension as systolic BP ≥140 mm Hg, or diastolic BP ≥90 mm Hg, or use of an antihypertensive medication. Healthy People 2010 4 objectives for the nation include reducing the proportion of US adults with HBP, increasing the proportion of US adults with HBP who are taking action to control it, and increasing the proportion of US adults with controlled BP. Despite JNC 7 recommendations for primary care clinicians, 2 , 3 awareness and control of hypertension remain disappointing at national and community levels. 5
More than 65 million Americans had HBP in 1999–2000, 6 an increase over the 50 million estimated for the 1988–1994 period. 7 The increase in the US hypertension burden may point toward an increase in the incidence of new‐onset HBP in adults and/or the prevalence of adults with HBP who live longer as a result of healthier lifestyles. 7 During the past decade, self‐reported awareness of HBP and prevalence of hypertension increased for blacks, Hispanics, and whites—but both measures were lower in Hispanic populations. 8 , 9 While treatment and control of hypertension increased between 1988 and 2000, prevalence levels were much lower among Mexican Americans. 8 There is a paucity of data about the current prevalence of self‐reported HBP in the United States and advice received and taken to reduce HBP through lifestyle modification. Using data from a recent mail survey of the US population (Healthstyles), we estimated the prevalence of self‐reported HBP, use of medication, advice received from a health care provider, and health behaviors adopted to lower BP.
METHODS
The Healthstyles survey is an assessment of the American public's health orientations and practices. Healthstyles is one of three annual mail surveys administered to about 10,000 households that are randomly selected from a mail panel. 10 The survey is designed to collect data about health beliefs, attitudes, social norms, and behaviors surrounding important public health concerns such as physician advice and action taken to make specific lifestyle modifications. A stratified, random sample of 5500 participants was generated based on age, race, sex, marital status, income, region, household size, and population density. Supplemental mailings (n=1500) were sent out to ensure adequate inclusion of low‐income individuals and minorities. From the 6027 selected participants, 4397 (73%) completed surveys were returned in 2002. Of these, 4286 (97.4%) responded to the question about HBP. The entire sample is weighted for age, sex, race/ethnicity, income, and household size to reflect the US population. 11
The 2002 Healthstyles survey included questions to assess awareness of HBP, use of antihypertensive medication, advice received by health care providers, and adoption of health‐related behaviors to lower BP. To determine the prevalence of HBP, respondents were asked “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” Respondents were also asked whether they had received advice from a doctor, nurse, or other health professional to go on a diet or change eating habits, cut down on salt or sodium in their diet, or exercise to lower BP. Respondents also reported whether they were engaged in any of these actions to lower BP and current medication use to lower BP. In this survey, HBP was not defined for respondents.
All analyses were performed using SAS statistical software (Version 8.02, SAS Institute Inc., Cary, NC) and weighted according to the distribution of sociodemographic characteristics in the United States. Weighted frequency analyses provided the proportion of respondents reporting HBP, use of antihypertensive medication, advice received from a health care provider, and actions taken to lower BP for groups defined by select characteristics. Sociodemographic characteristics included race/ethnicity (black, Hispanic, or white), sex, age group (18–44, 45–64, or 65 years or older), and attained educational level (<12, 12, or >12 years). Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were obtained from multivariate logistic models that included age, sex, and race/ethnicity.
RESULTS
The 2002 Healthstyles eligible survey study population consisted of 4286 respondents, aged 18 years and older, including 2612 (61%) women. Among respondents, 12% were black, 11% were Hispanic, 71% were white, and 5% were other races or missing race information. The distribution of age groups included 47% aged 18–44 years, 37% aged 45–64 years, and 16% aged 65 years or older. An education level of <12 years was reported by 7%, while 23% reported 12 years, 62% reported >12 years of education, and 8% were missing information on education.
More than one fifth of respondents reported that they had been told by a health professional that they had HBP (Table I). This was higher among men than women (p<0.0001) and increased among successive age groups (p<0.0001). After adjustment for age and sex, there was a higher proportion of self‐reported HBP among blacks (OR, 1.8; 95% CI, 1.5–2.3) and Hispanics (OR, 1.3; 95% CI, 1.0–1.6) than among whites. The lowest prevalence of self‐reported HBP was observed among persons with >12 years of education; however, this difference was not statistically significant after adjustment for age, race, and sex.
Table I.
Weighted Proportion of Respondents Told by a Health Professional That They Had High Blood Pressure and of Respondents Who Are Currently Taking Medication to Lower Their Blood Pressure Among Those With Self‐Reported High Blood Pressure, by Select Characteristics
| Self‐Reported High Blood | Reported Currently Taking Medication | ||
|---|---|---|---|
| Characteristic | n | Pressure (n [%]) | For High Blood Pressure (n [%])* |
| Total | 4286 | 865 (20.1) | 487 (53.0) |
| Sex | |||
| Men | 1674 | 398 (22.9) | 214 (51.4) |
| Women | 2612 | 467 (17.6)** | 273 (54.8) |
| Age (yr) | |||
| 18–44 | 2011 | 301 (15.5)** | 107 (30.9)** |
| 45–64 | 1585 | 380 (24.6) | 238 (62.7) |
| 65 and older | 690 | 184 (27.1) | 142 (77.6) |
| Race/ethnicity† | |||
| White | 3041 | 566 (19.2)** | 322 (53.7) |
| Black | 535 | 160 (28.2) | 98 (53.8) |
| Hispanic | 489 | 112 (21.3) | 53 (45.1) |
| Race/ethnicity/sex† | |||
| White | |||
| Men | 1202 | 271 (22.1) | 148 (52.1) |
| Women | 1839 | 295 (16.5) | 174 (55.8) |
| Black†† | |||
| Men | 164 | 58 (32.1)** | 34 (55.4) |
| Women | 371 | 102 (25.8) | 64 (52.6) |
| Hispanic†† | |||
| Men | 213 | 50 (22.8) | 21 (37.6) |
| Women | 276 | 62 (19.6) | 32 (54.9) |
| Education‡ (yr) | |||
| <12 | 291 | 72 (21.0) | 51 (68.4) |
| 12 | 1000 | 217 (22.5) | 125 (57.9) |
| >12 | 2659 | 493 (18.6) | 274 (53.5) |
| *Among persons reporting high blood pressure; **χ2 p<0.0001; †race/ethnicity missing for 221 respondents; ††sample size too small for statistical reliability or inference; ‡education missing for 336 respondents | |||
Of the respondents who had been told that they have HBP, 53% were currently taking antihypertensive medications (Table I). Medication use increased among successive age groups (p<0.0001), was lower among Hispanics (45%), similar for blacks and whites (54%), and was lowest among those with >12 years of education. Differences between groups defined by race, sex, or education, however, did not reach statistical significance in multivariate logistic regression models.
Almost 75% of all eligible respondents had reported receiving advice from a health professional to exercise, but only 21% received advice to cut down on dietary salt or sodium or to change eating habits to lower their BP levels (Table II). Since <6% reported being told to reduce alcohol consumption among the different characteristic categories, advice and action about alcohol consumption is not addressed in this report. The proportion of respondents receiving advice about diet change and salt reduction increased among successive age groups (p<0.0001) while advice to exercise declined with age (p<0.0001). Men were more likely to receive advice about diet change and salt reduction (p<0.05) but less likely to receive advice about exercise (p<0.0001) than women, after adjustment for age and race/ethnicity. Compared with men, women were less likely to report being told to go on a diet (p<0.005) but more likely to report being told to exercise (p<0.0001), after adjustment for age and race/ethnicity. Blacks were more likely to receive advice about diet changes (OR, 2.9; 95% CI, 2.3–3.6) and salt reduction (OR, 2.7; 95% CI, 2.2–3.4) but less likely to receive advice about exercise (OR, 0.5; 95% CI, 0.4–0.6) than whites after adjustment for age and sex differences. Hispanics were also more likely to receive advice about diet change (OR, 1.4; 95% CI, 1.1–1.8) and salt reduction (OR, 1.5; 95% CI, 1.2–2.0) and less likely to receive advice about exercise (OR, 0.7; 95% CI, 0.5–0.8) than whites. Advice about diet change and salt reduction declined with increasing education, while advice to exercise increased with education level; the association was significant only for salt reduction (p<0.01). Respondents with self‐reported HBP were more likely to report that they received advice from a health professional to go on a diet or change eating habits (OR, 5.0; 95% CI, 4.2–6.0) and to reduce salt or sodium from diet (OR, 5.2; 95% CI, 4.3–6.2) and less likely to have received advise to exercise (OR, 0.20; 95% CI, 0.17–0.24) than those without HBP after adjustment for sex, age, and race/ethnicity (Figure 1).
Table II.
Weighted Proportion of Respondents Who Reported Receiving Advice From a Physician or Other Health Professional to Make Specific Lifestyle Modifications to Lower Blood Pressure, by Select Characteristics
| Respondents (n [%]) Who Reported Receiving Advice to: | |||
|---|---|---|---|
| go on a Diet or | Cut Down on Salt or | ||
| Characteristic | Change Eating Habits | Sodium in Diet | Exercise |
| Total | 981 (21.0) | 1012 (21.7) | 3176 (75.0) |
| Sex | |||
| Men | 430 (22.9) | 426 (22.8) | 1177 (71.9) |
| Women | 551 (19.2)* | 586 (20.6) | 1999 (77.8)** |
| Age (yr) | |||
| 18–44 | 310 (13.3)** | 278 (12.0)** | 1687 (84.2)** |
| 45–64 | 458 (29.4) | 437 (27.4) | 1082 (67.1) |
| 65 and older | 213 (31.5) | 297 (42.5) | 407 (59.4) |
| Race/ethnicity† | |||
| White | 606 (18.7) | 624 (19.6) | 2327 (76.8) |
| Black | 208 (35.9) | 215 (34.3) | 334 (65.3) |
| Hispanic | 121 (21.2) | 124 (22.4) | 350 (72.8) |
| Education†† (yr) | |||
| <12 | 87 (24.8) | 103 (29.2)** | 195 (70.3) |
| 12 | 228 (21.2) | 268 (25.6) | 748 (74.9) |
| >12 | 573 (20.4) | 549 (19.6) | 2001 (75.8) |
| *χ2 p<0.005; **χ2 p<0.0001; †race/ethnicity missing for 221 respondents; ††education missing for 336 respondents | |||
Figure 1.
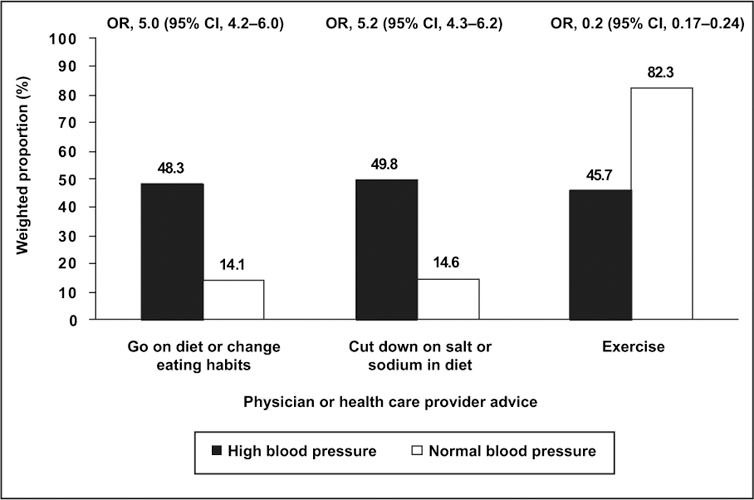
Weighted proportion of respondents who reported receiving advice from a physician or other health professional to make lifestyle modifications to help lower blood pressure (by self‐reported high blood pressure status)—Healthstyles 2002. Odds ratio (OR) and 95% confidence interval (CI) were obtained from multivariate logistic regression models with sex, age, and race/ethnicity as covariates.
Overall, few respondents reported following advice to take action to go on a diet or change eating habits (13.4%), to reduce salt or sodium in diet (16.7%), or to exercise (6.3%) to lower their BP levels (Table III). Men were more likely to exercise than women (OR, 1.5; 95% CI, 1.1–1.9). Following advice to take action for diet change or salt reduction increased among successive age groups (p<0.0001). Following advice to take action was higher among blacks than whites for changing diet (OR, 2.6; 95% CI, 2.0–3.2), salt reduction (OR, 3.4; 95% CI, 2.7–4.3), and exercise (OR, 1.6; 95% CI, 1.2–2.3). Hispanics were also more likely to follow action to change diet (OR, 1.5; 95% CI, 1.1–2.0) and reduce salt (OR, 3.4; 95% CI, 2.7–4.3) than whites after adjustment for sex and age. Persons with >12 years of education were less likely to reduce salt intake (p<0.05). Respondents with self‐reported HBP were more likely to report following advice to change diet (OR, 4.1; 95% CI, 3.4–5.0), to reduce salt or sodium from diet (OR, 5.3; 95% CI, 4.4–6.4), and to exercise (OR, 3.6; 95% CI, 2.8–4.7) than those without HBP, after adjustment for sex, age, and race/ethnicity (Figure 2).
Table III.
Weighted Proportion of Respondents Who Reported Following Advice to Take Action to Make Specific Lifestyle Modifications to Lower Blood Pressure, by Select Characteristics
| Respondents (n [%]) Who Reported Taking Action to: | |||
|---|---|---|---|
| go on a Diet or Change | Cut Down on Salt or | ||
| Characteristic | Eating Habits | Sodium in Diet | Exercise |
| Total | 621 (13.4) | 784 (16.7) | 277 (6.3) |
| Sex | |||
| Men | 260 (14.4) | 311 (16.8) | 134 (7.5)* |
| Women | 361 (12.4) | 473 (16.6) | 143 (5.2) |
| Age (yr) | |||
| 18–44 | 170 (7.2)** | 188 (8.2)** | 99 (4.8) |
| 45–64 | 296 (19.1) | 345 (21.2) | 132 (9.0) |
| 65 and older | 155 (22.9) | 251 (36.2) | 46 (6.3) |
| Race/ethnicity† | |||
| White | 384 (12.0) | 467 (14.5) | 190 (6.3) |
| Black | 130 (22.7) | 183 (30.4) | 54 (9.2) |
| Hispanic | 79 (14.1) | 99 (18.4) | 26 (4.9)†† |
| Education‡ (yr) | |||
| <12 | 57 (15.3) | 80 (22.3) | 18 (6.0)†† |
| 12 | 134 (12.3) | 210 (20.1) | 66 (6.2) |
| >12 | 368 (13.3) | 426 (15.2) | 159 (5.6) |
| Percentages are based on number of respondents in the category who reported receiving advice to take the respective action (see Table II). *χ2 p<0.005; **χ2 p<0.0001; †race/ethnicity missing for 221 respondents; ††sample size too small for statistical reliability; ‡education missing for 336 respondents | |||
Figure 2.
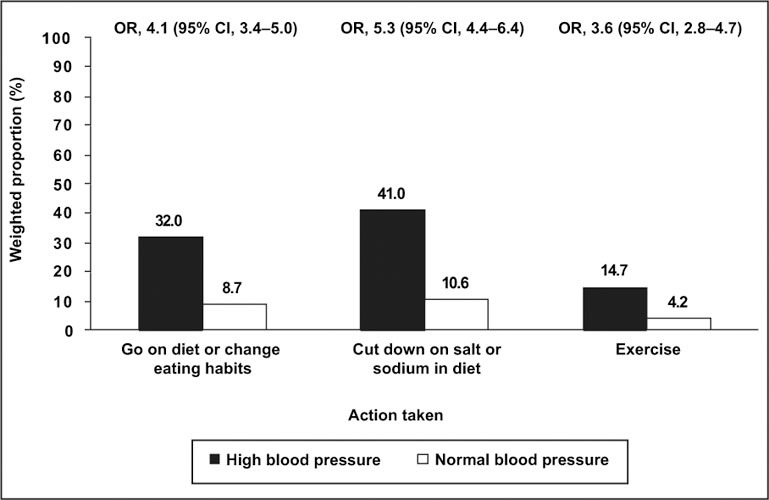
Weighted proportion of respondents who reported taking action following advice from a physician or other health professional to make lifestyle modifications to help lower their blood pressure (by self‐reported high blood pressure status)—Healthstyles 2002. Odds ratio (OR) and 95% confidence interval (CI) were obtained from multivariate logistic regression models with sex, age, and race/ethnicity as covariates.
Among self‐reported HBP respondents who were prescribed antihypertensive medication, the prevalence of receiving advice from a health professional for diet and salt categories was significantly higher among those taking their medication than those not taking their medication (p<0.0001) (Table IV). Conversely, those not taking their medication reported receiving advice to exercise significantly more often than those taking their medication (p<0.0001). Similarly, among self‐reported HBP respondents, current medication use was associated with a higher likelihood of following the advice for lifestyle modifications (p<0.0001).
Table IV.
Weighted Proportion of Respondents With Self‐Reported High Blood Pressure Who Reported Receiving Advice From a Physician or Other Health Professional and Taking Actions to Make Specific Lifestyle Modifications (n=865), by Current Medication Status
| Prescribed Antihypertensive (n [%]) | ||
|---|---|---|
| Lifestyle Behavior Change | Taking (n=487) | Not Taking (n=378) |
| Received advice | ||
| Go on diet or change eating habits* | 315 (63.6) | 135 (31.1) |
| Cut down on salt or sodium in diet* | 337 (67.9) | 131 (29.4) |
| Exercise* | 133 (26.6) | 240 (67.2) |
| Taking action | ||
| Go on diet or change eating habits* | 220 (45.6) | 71 (16.7) |
| Cut down on salt or sodium in diet* | 292 (58.9) | 92 (20.8) |
| Exercise* | 89 (19.7) | 37 (9.1)** |
| *χ2 p<0.0001 for unadjusted differences between medication groups; **sample size too small for statistical reliability | ||
DISCUSSION
These 2002 findings provide important information about the current prevalence of self‐reported HBP, advice received from health care providers, and related health behaviors. In this survey population, we observed that 20% of respondents reported that they have been advised that they have HBP. This estimate, based on self‐reported information, is lower than the most recently reported prevalence (28.6%) of hypertension obtained from actual BP measurements and diagnosis in the National Health and Nutrition Examination Survey III (NHANES III), 1999–2002. 12 Among Healthstyles respondents, the adjusted prevalence of self‐reported HBP was higher in men than women. Black men had the highest prevalence of self‐reported HBP compared with all others in this report. Similar disparities have been observed among persons with measured and diagnosed hypertension. 5 , 6 , 7 , 8 , 12
We found that almost 53% of those who had been advised they had HBP were also taking medication to control it compared to 46% of hypertensives in the NHANES III, 1999–2002. 12 This may reflect an increased awareness among the general public about the importance of controlling BP to prevent heart attack and/or stroke or a change in physician behaviors such that pharmacologic treatment is considered a necessary first action for controlling BP. In a study of physician behavior regarding the diagnosis and treatment of hypertension, it was found that 98% of participating physicians (n=175) reported that they prescribed antihypertensive medication for patients with a diagnosis of hypertension. 13
Among Healthstyles respondents who had ever been advised that they had HBP, <50% reported that they had received advice from a health care professional to make any lifestyle modifications regarding diet and salt. This suggests that health professionals are taking advantage of some of the opportunities to intervene on cardiovascular disease‐related lifestyle factors, but this could be improved. JNC 7 recommends lifestyle modifications for both primary and secondary prevention of hypertension. 2 , 3 Secondary prevention is important for persons with hypertension. JNC 7 recommends achieving BP treatment goals by lifestyle modification alone or with pharmacologic treatment. This report suggests missed opportunities by physicians to give lifestyle modification advice to patients with HBP regardless of whether they are prescribed medication to lower their BP. Among those with self‐reported HBP, however, persons taking their prescribed antihypertensive medications were more likely to report that physicians or other health care providers also advised them about diet change and salt reduction, while those who were not taking prescribed antihypertensive medications were more likely to report being told to exercise. Those persons with HBP who were not taking medication but reported receiving advice on exercise may have less severe levels of hypertension.
Recommended lifestyle modifications for hypertension prevention and management from JNC 7 also include more than the modifications discussed in this paper and extend to maintaining adequate dietary potassium and calcium, smoking cessation, moderation in alcohol intake, and reducing dietary saturated fat and cholesterol. These are especially key management recommendations for all persons with HBP regardless of pharmacologic treatment and among normotensives. Results from the Dietary Approaches to Stop Hypertension (DASH) 14 , 15 , 16 clinical trial also demonstrate the benefit of a diet rich in fruits and vegetables for reducing systolic and diastolic BP. In 1998, $108.8 billion in US health care spending was attributed to hypertension. 17 Lifestyle modifications may help lower medical costs since the average amount spent per hypertensive patient has been estimated at $3787 per year. 17
Focus on system‐level changes in the health care setting that enable and support effective lifestyle counseling is needed. System‐wide barriers to delivering preventive counseling by physicians and other health care providers have been identified, including a lack of clarity in the counseling role and inadequate reimbursement for the time it takes to deliver preventive counseling. 18 System‐wide changes to achieve effective training in prevention for physicians and reimbursement for delivering comprehensive preventive counseling would reinforce lifestyle counseling in the health care setting. 18 It has also been suggested that lifestyle counseling should not be restricted to physicians, but could also be delivered by nonphysician professionals, such as physician assistants, nurses, pharmacists, and dietitians. 19
It is important to note that the current survey may be subject to several limitations. Since it is a mail survey, the selection process could result in an analytic sample that excludes households wthout a mailing address (e.g., residents in the lowest income levels, high school dropouts, and minority populations). 20 Also, the Healthstyles survey requires literacy and fluency in English, which omits people who do not read or write English. Another major limitation is recall bias, in that the respondents may not recall all the advice given; they may remember just portions of what was told to them (e.g., medication instructions vs. lifestyles modifications) or may not remember exactly what health professionals told them. Therefore, with recall bias, the proportions reporting advice and action may be underestimated. Despite these potential limitations, several comparison studies have shown that results obtained from this mail survey are similar to those of conventional random samples. 20
The Healthstyles survey is valuable for its provision of the most recent prevalences of self‐reported HBP, reported receipt of advice from health care providers, and health behaviors that are associated with HBP. The Healthstyles data indicate that there are disparities in the prevalence of self‐reported HBP for groups defined by sex, age, race/ethnicity, and education. While the absence of certain disparities in taking prescribed BP medication is indeed encouraging, the fact remains that almost 80% of the survey population reported not receiving advice about lifestyle changes to lower BP from a health professional. Initiatives are needed for health care providers to decisively promote healthy lifestyles for preventing or reducing HBP, in addition to medical therapies for HBP. Tracking systems for periodically mailing lifestyle modification recommendation reminders may be possible for those required to be seen professionally for pharmacologic management and also for those not requiring medication. Other strategies could include combined community programs, medical referrals and therapy, mass media to promote screening, and treatment to improve risk reduction and control of hypertension. Future initiatives are needed to improve how health care professionals are taking advantage of promoting heart healthy actions that can reduce risks and improve control of HBP, especially among blacks and Hispanics.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- 1. American Heart Association . Heart Disease and Stroke Statistics—2001 Update. Dallas , TX : American Heart Association; 2000. [Google Scholar]
- 2. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289: 2560–2572. [DOI] [PubMed] [Google Scholar]
- 3. National High Blood Pressure Education Program . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42: 1206–1252. [DOI] [PubMed] [Google Scholar]
- 4. US Dept of Health and Human Services . Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington , DC : US Government Printing Office; 2000. [Google Scholar]
- 5. Burt VL, Cutler JA, Higgins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population: data from the health examination surveys, 1960–1991. Hypertension. 1995; 26: 60–69. [DOI] [PubMed] [Google Scholar]
- 6. Fields LE, Burt VL, Cutler JA, et al. The burden of adult hypertension in the United States 1999 and 2000: a rising tide. Hypertension. 2004; 44: 398–404. [DOI] [PubMed] [Google Scholar]
- 7. Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001; 345: 479–486. [DOI] [PubMed] [Google Scholar]
- 8. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003; 290: 199–206. [DOI] [PubMed] [Google Scholar]
- 9. State‐specific trends in self‐reported blood pressure screening and high blood pressure—United States, 1990–1999. MMWR Morb Mortal Wkly Rep. 2002; 51: 456–460. [PubMed] [Google Scholar]
- 10. Maibach EW, Maxfield A, Ladin K, et al. Translating health psychology into effective health communication: the American Healthstyles audience segmentation project. J Health Psychol. 1996; 1: 261–277. [DOI] [PubMed] [Google Scholar]
- 11. Dutta‐Bergman MJ. Health attitudes, health cognitions, and health behaviors among internet health information seekers: population‐based survey. J Med Internet Res. 2004;6:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Glover MJ, Greenlund KJ, Ayala C, et al. Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005; 54: 7–9. [PubMed] [Google Scholar]
- 13. Hyman DJ, Pavlik VN. Self‐reported hypertension treatment practices among primary care physicians. Arch Intern Med. 2000; 160: 2281–2286. [DOI] [PubMed] [Google Scholar]
- 14. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997; 336: 1117–1124. [DOI] [PubMed] [Google Scholar]
- 15. Svetkey LP, Simons‐Morton D, Vollmer WM et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999; 159: 285–293. [DOI] [PubMed] [Google Scholar]
- 16. Karanja NM, Obarzanek E, Lin PH, et al. Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. DASH Collaborative Research Group. J Am Diet Assoc. 1999;(8 suppl):S19–S27. [DOI] [PubMed] [Google Scholar]
- 17. Hodgson TA, Cai L. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care. 2001; 39: 599–615. [DOI] [PubMed] [Google Scholar]
- 18. Merz CN, Mensah G, Fuster V, et al. Task Force #5—the role of cardiovascular specialists as leaders in prevention: from training to champion. J Am Coll Cardiol. 2002; 40: 641–651. [DOI] [PubMed] [Google Scholar]
- 19. Fletcher GF. Preventive cardiology: how can we do better? J Am Coll Cardiol. 2002; 40: 584–585. [Google Scholar]
- 20. Groeneman S. Multi‐purpose household panels and general samples: how similar and how different? Paper presented at: Annual Conference of the American Association for Public Opinion Research; May 1115, 1994; Danvers , MA . [Google Scholar]


