Abstract
Introduction:
Anterior cruciate ligament (ACL) is a common injury which has been conventionally managed by various graft reconstruction using bone patellar tendon bone, or quadruple hamstring autograft, to name a few. However, all these grafts are associated with many complications. Lately, peroneus longus tendon (PLT) autograft has shown promising results in this field, although there is still a dearth of data on its use. We, therefore, aimed at carrying out a study to evaluate the functional outcome and knee stability results of ACL reconstruction using PLT graft.
Patients and Methods:
Patients with a completely torn ACL were included in the study. The PLT was harvested, and graft length, thickness, and harvesting time were noted intraoperatively. Knee stability and functional scores were evaluated clinically and using Lachman test (primarily) and KT-2000 arthrometer and subjectively with International Knee Documentation Committee (IKDC) score at 6, 12, and 24 months (secondary outcome) postoperatively. Ankle scores were also recorded by making use of American Orthopedic Foot and Ankle Score (AOFAS)–Hindfoot Scale.
Results:
Forty-eight patients met the inclusion criteria. The graft harvest time was 7.4 min (5–9 min). The mean thickness of the graft on doubling was 7.9 mm (7–9 mm). Ninety-six percent of the patients were satisfied with their results of the knee surgery, and 95% of the patients had no complaints of ankle joint. The mean IKDC score postoperatively was 78.16 ± 6.23, and the mean AOFAS score was 98.4 ± 4.1. None of the patients had any neurovascular deficit.
Conclusion:
ACL reconstruction using PLT graft yields a good functional score (IKDC, KT-2000 arthrometer) even at 2-year follow-up. It is a safe and effective autograft option for ACL reconstruction.
KEYWORDS: Anterior cruciate ligament, autograft, peroneus longus tendon, reconstruction
INTRODUCTION
Ligament and tendon injuries constitute a major chunk of sports medicine surgeries.[1] Among them, anterior cruciate ligament (ACL) injuries have a high incidence, and most of its patients require repair or reconstruction. These injuries in a nonathletic patient, depending on the grade and willingness of the patient to make lifestyle changes and to avoid activities that can cause recurrent instabilities, do not always require reconstruction. Moreover, the knees of these patients are not subjected to stress and tension unlike an athletic patient. ACL is the major stabilizing ligament of knee as it prevents anterior translation of the tibia over the femur. It also contributes to the dynamic stability of the knee, so it is an important structure for maintaining normal knee movements.[2] If ACL injuries are left untreated, they can further result in meniscal injuries and ultimately degenerative arthritis of knee joint.[3]
ACL injuries can be treated both conservatively with a knee brace and physical therapy and operatively by repair (isolated or augmented) or reconstruction (allograft or autograft) of the ligament. For the decision to be made on this aspect, there are several criteria to be considered like activity level of the patient, comorbid injury, age group, and functional demand of the patient.[4]
When reconstruction of ACL is indicated, the option of both allografts and autografts can be considered. Allograft has a drawback of being higher in cost, delayed incorporation, higher chances of disease transmission, and immunological reactions. The most commonly used autografts are bone patellar tendon bone (BPTB) or double-looped/quadruple-looped semitendinosus or gracilis autograft (hamstring autograft). Other options include fascia lata, iliotibial band, and quadriceps tendon with or without bone.[5]
The bone patellar bone autograft, while having the longest history of use, can be complicated by anterior knee pain and can be associated with postoperative patella fracture, fat pad fibrosis, or patellar tendon contracture.[6,7,8,9,10] Another important drawback of this autograft is that the surgeon cannot control the length of the graft being harvested, which may further complicate the procedure if there is excessive shortening or lengthening of the bone. An alternative to this, the hamstring tendon (HT) autograft, can be used, but it can cause a significant change in hamstring muscle strength.[11,12,13,14,15] If medial collateral ligament injury is present along with ACL injury, then harvesting the HT can lead to medial instability of the knee joint. Normal hamstring function is important in ACL-reconstructed patients as it protects the newly reconstructed ACL from anterior drawer force which is excreted by quadriceps contraction.[16,17] Harvesting hamstring from medial side can damage the saphenous nerve leading to anesthesia over medial aspect of leg.
The above-described drawbacks of the commonly used autografts warrant us to find an alternative graft material to these. The characteristic of an ideal graft for ACL reconstruction would be the one with an acceptable amount of strength, be of adequate size, and easily and safely harvested. Zhao and Huangfu[18] found that anterior half of PLT has enough length and strength to be effective as an autograft of choice in ACL reconstruction.
In our study, we evaluated the knee stability and the functional outcome of arthroscopic ACL reconstruction using PLT as an alternative graft for ACL reconstruction.
PATIENTS AND METHODS
This was a prospective interventional study that was conducted at our tertiary care center after obtaining a formal approval from the institute's ethical committee. The time duration of the study was from February 2017 to November 2019. During this time, we encountered 378 patients with ACL tear, out of which 62 (16.4%) were nonathletic patients. All patients who were diagnosed with ACL tear on clinical and radiological examination (magnetic resonance imaging [MRI]) and who were willing to undergo surgery were included in our study. Athletes were excluded from our study. Patients with a concurrent injury to meniscus and collateral ligaments were also included in our study. Duration since the injury and the mechanism of injury were noted. Preoperative demographic data of patients along with their body mass index were noted.
Patients were taken to operation theater according to the standard protocol of the institution. With patients in supine position and knee in full extension, a 4-cm long longitudinal incision was made, 3 cm above and 1 cm behind the lateral malleoli [Figure 1a]. Dissecting through the subcutaneous tissue and superficial fascia, the PLT and peroneus brevis tendon were identified. PLT was divided 2 cm above the tip of malleoli, and the distal stump was sutured sideways to peroneus brevis with an absorbable polyglactin suture 2-0 [Figure 1b] Then, PLT was stripped using a stripper until 5 cm below the femoral head to prevent peroneal nerve injury. Donor site was closed with a nylon sutures, and sterile dressing was applied. Then the length of the graft was noted [Figure 2a].
Figure 1.
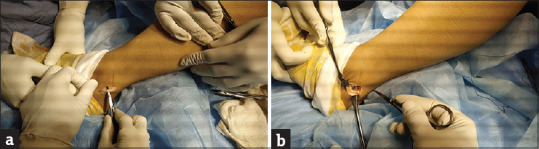
Peroneus longus tendon (a) Distal of the peroneus longus tendon was found using an oblique incision which was performed 2 cm below the lateral malleolus, (b) Peroneus longus tendon was sutured to polybutylene terephthalate before closure
Figure 2.

The peroneus longus graft after harvesting (a) Length of the tendon, (b) Thickness of the tendon
Then, the ACL repair was done arthroscopically by making use of the regular portals. The intercondylar notch was cleared of fibrous tissue to ease the visualization during procedure, but some remnants were preserved as a reference to tunnel placement and for property of proprioception. Femoral tunnel and tibial tunnel were drilled using a jig. After tensioning the graft with an appropriate tensioner, it was secured on femoral edge of the tunnel with the help of button and tibial end by a bioabsorbable screw [Figure 3].
Figure 3.
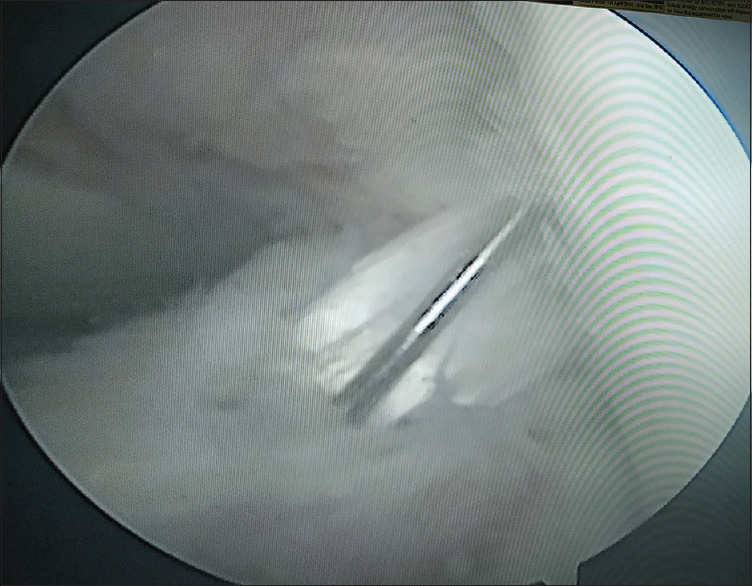
Peroneus longus tendon used as a graft for anterior cruciate ligament reconstruction arthroscopically
Postoperatively, patients' knee joint was immobilized with a long leg knee brace. Isometric quadriceps and flexion, ankle dorsiflexion, and planter flexion exercises were commenced on postoperative day 1. On the 10th day after surgery, active knee flexion was allowed through a range of 45–90° and up to 120° during the 4th–6th weeks of the operation, r espectively. All patients were on axillary type of crutches for the next 6 weeks and were allowed to return to daily activity by 3 months and full physical activity by 1 year.
Knee stability and function were evaluated clinically and using Lachman test and KT-2000 arthrometer as well as subjectively with the International Knee Documentation Committee (IKDC) score at 6, 12, and 24 months postoperatively. The Lachman test was given grades (1, 2, and 3) depending on the amount of anterior translation (3–5 mm, 5–10 mm, and >10 mm, respectively) for the tibia over the femur. KT-2000 was graded as 0–2 mm, 3–5 mm, and >6 mm displacement. Functional assessment of the ankle joint was done making use of the American Orthopedic Foot and Ankle Score (AOFAS)–Hindfoot Scale. Patients were subjectively asked for the satisfaction of their return of function of the affected knee, and movements of ankle joint restriction were noted down with comparison to the other ankle joint.
RESULTS
Among the 48 patients in our study, 36 were male and 12 were female. The mean age of the patients was 27.2 years, with a range of 18–36 years [Table 1]. The duration between the injury and the surgery is given in Table 2. Among 48 patients, 19 (39.58%) of them had injuries due to road traffic accidents, 17 (35.41%) due to sports, 7 (14.5%) assault, and 5 (10.41%) domestic accidents. The graft harvest time was 7.4 min ranging from 5 to 9 min. The mean thickness of the graft on doubling was 7.9 mm (7–9 mm) [Figure 2b]. Forty-six (95.83%) patients were satisfied with their results of the knee surgery, and 45 (93.75%) patients had no complaints of ankle joint postoperatively. The mean IKDC score and lachman tests postoperatively was 78.16 ± 6.23 [Tables 3 and 4]. There was one patient with superficial infection (Staphylococcus aureus) at the graft donor site which was treated with oral antibiotics (cefoperazone). None of the patients had any neurovascular deficit. The mean follow-up duration was 19.4 months (15–24 months).
Table 1.
Clinical features of the patients in study
| Parameters studied | Mean±SD |
|---|---|
| Age (years) | 27.2±4.4 |
| Graft harvest time (min) | 7.4±1.3 |
| Thickness of graft (mm) | 7.9±0.7 |
| Mean length (cm) | 29.4±2.34 |
| IKDC score | 78.16±6.23 |
| AOFAS score | 98.4±1.23 |
IKDC: International Knee Documentation Committee, AOFAS: American Orthopedic Foot and Ankle Score, SD: Standard deviation
Table 2.
Duration of injury prior to surgery
| Time duration from the injury to surgery (months) | Number of patients |
|---|---|
| Within 1 | 6 |
| 1-3 | 24 |
| 3-6 | 12 |
| >6 | 6 |
Table 3.
Lachman test postoperatively
| Follow-up period | Lachman indicators | Number of patients (%) |
|---|---|---|
| 6-month follow-up | 0 | 44 (91.67) |
| I | 4 (8.37) | |
| II | ||
| III | ||
| 12-month follow-up | 0 | 45 (93.75) |
| I | 3 (6.25) | |
| II | 0 | |
| III | 0 | |
| At 18 months | 0 | 44 (91.67) |
| I | 4 (8.37) | |
| II | 0 | |
| III | 0 |
Table 4.
KT-2000 measurements postoperatively
| Follow-up period | KT-2000 indicators (mm) | Number of patients (%) |
|---|---|---|
| 6-month follow-up | 0-2 | 43 (89.58) |
| 3-5 | 5 (10.41) | |
| >6 | 0 | |
| 12-month follow-up | 0-2 | 44 (91.67) |
| 3-5 | 4 (8.37) | |
| >6 | 0 | |
| At 18 months | 0-2 | 43 (89.58) |
| 3-5 | 5 (10.41) | |
| >6 | 0 |
DISCUSSION
ACL injuries are one of the most common knee injuries, and its satisfactory reconstruction has become a matter of utmost importance. Autografts are commonly used due to the advantage of low risk of adverse reaction and no risk of disease transmission. As a biologic graft, an autograft undergoes revascularization and recollagenation with a loss of 50% strength during early days of implantation.[19] Hence, keeping this in mind, the graft substitute for ACL should be stronger than the ACL. Native ACL has an ultimate tensile load of 2020 ± 264 N.[20] BPTB autograft has a ultimate tensile load of 2300 N[19] while the quadruple hamstring graft's ultimate tensile load is 4090 ± 265 N. However, double peroneus longus tendon has an ultimate tension load of 4268 ± 285 making it one of the effective alternatives to ACL.[20] Diameter of the autograft in ACL reconstruction surgery is an important factor contributing to failure. The exact graft diameter needed to avoid such failure rates is not clear. Xu et al.[21] concluded that when graft sizes larger than 8.5 mm were selected, the clinical outcomes were superior in the autograft group. They also suggested the importance of restoring the insertion site to at least 60%–80% of cross-sectional area during anatomic ACL reconstruction.[22] A review article by Figueroa et al.[23] recommended that even an increase of 0.5 mm up to a graft size of 10 mm is beneficial to the patient. In our study, the mean graft diameter was 8.7 mm ranging from 7.9 mm to 9.1 mm. Rhatomy et al.[24] compared the graft thickness of quadruple hamstring and peroneus and concluded that there was a mean difference of 0.6 mm in favor of peroneus longus graft.
The minimum length that is required when cortical button is used as a femoral fixation, as graft is prepared around it, is 21 cm. In our study, the mean length of autograft was 29.4 cm, ranging from 26.2 cm to 34.8 cm. This gives us an extra edge while reconstructing ACL using a bilateral bioabsorbable screw.
No study has emphasized on the surgical time needed for harvesting the peroneus longus graft. In our study, the mean time for harvesting the graft was 7.4 min. This shorter duration is important as it saves a significant amount of tourniquet time for reconstruction of the ACL per se. A less experienced surgeon can easily harvest the PLT graft, compared to BPTB and HT graft, which builds up the confidence in the surgeon. The ease of the procedure decreases the chances of mistakes during reconstruction.
Previous studies have shown good results after ACL reconstruction with peroneus longus autograft, in terms of functional outcome and knee stability.[25,26,27] Rhatomy et al.[24] compared hamstring with PLT autograft and did not find any significant difference between the 2 in 1 year follow-up, although considered only the functional outcome. In our study, we evaluated both the functional outcome and stability of the knee joint after peroneus longus autograft repair of ACL, which has shown comparable results with Kerimoglu et al.[26] Donor site morbidity is an important consideration while looking for a graft for ACL reconstruction. Most widely used BPTB autograft is associated with complaints of anterior knee pain and kneeling pain postoperatively.[28,29]. A meta-analysis of studies has shown an increased incidence of osteoarthritis in a BPTB autograft ACL reconstruction of knee.[30] It has also documented that this autograft has an increased incidence of adhesions leading to extension deficit.[31]
On considering autograft of hamstring, there was an electromechanical delay in knee flexors/weakness.[17] Harvesting HT may be deleterious in postoperative rehabilitation of ACL reconstruction as HT protects the reconstructed ACL from anterior drawer force, which is exerted by the quadriceps.[15] It might also hinder active knee flexion.[31]
The function of PLT is to plantar flex the first ray of the foot along with the plantar flexion and eversion of the foot at the ankle joint.[32] The first ray plantar flexion of foot is important for the stance phase of gait. Kerimoglu et al.[26] reported a deficit in plantar flexion of the first ray of foot after harvesting PLT. They reported functional deteriorations of push off during the stance phase. However, this push off strength of the first ray is significant for athletes, and as our study consisted of nonathletes, there was no such complication in any of the patients. When foot eversion is considered, the loss of power of inversion is not so significant as peroneus brevis is considered a more effective evertor of ankle than PLT (Rhatomypaper).[24] However, there were controversial evidences when ankle functional outcomes were evaluated. Angthong and Chernchujit et al.[25] had reported a reduction in ankle peak torque eversion and inversion. However, a study by Rhatomy et al. showed normal functional scores of ankle joint on follow-up. In our study, we used AOFAS score for deducing the ankle functional outcome, and it had a mean score of 98.4 (range, 94–100) which was similar to Rhatomy et al.[24]
In our study, while examining the arch of the foot, there was no obvious effect of harvesting PLT. On checking ankle stability by anterior and posterior drawer test, we found no difference from the contralateral limb. None patients had any complaints pertaining to the ankle joint. This can be attributable to the regeneration potential of harvested full-thickness tendon. This has been shown both clinically and by MRI,[33,34,35] thus making patient free from any complaints of ankle joint.
Sural nerve is the nerve that runs around the PLT. Injuring the sural nerve will cause loss of sensation over the lateral border of foot. Numbness in this area is generally well tolerated making sural nerve one of the most frequently used nerves for autograft elsewhere in the body.[36] However, none of our cases reported any of such complaints.
However, a long-term follow-up and a larger number of cases are required to confirm the findings. This study only considered nonathletic individuals who lead a sedentary lifestyle, i.e., individuals who do not exert much pressure on knee and ankle joint.
CONCLUSION
PLT has a greater ultimate tensile load, more thickness and length, less graft harvesting time, and almost no donor site morbidity and a good functional outcome and knee stability scores, making it an effective and a safe autograft option for ACL reconstruction.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nazem K, Barzegar M, Hosseini A, Karimi M. Can we use peroneus longus in addition to hamstring tendons for anterior cruciate ligament reconstruction? Adv Biomed Res. 2014;3:115. doi: 10.4103/2277-9175.132696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johansson H, Sjölander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthop Relat Res. 1991;268:161–78. [PubMed] [Google Scholar]
- 3.Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: Trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321–8. doi: 10.2106/JBJS.H.00539. [DOI] [PubMed] [Google Scholar]
- 4.Rudy, Mustamsir E, Phatama KY. Tensile strength comparison between peroneus longus and hamstring tendons: A biomechanical study. International Journal of Surgery Open. 2017;9:41–4. https://doi.org/10.1016/j.ijso.2017.10.002. [Google Scholar]
- 5.Miller SL, Gladstone JN. Graft selection in anterior cruciate ligament reconstruction. Orthop Clin North Am. 2002;33:675–83. doi: 10.1016/s0030-5898(02)00027-5. [DOI] [PubMed] [Google Scholar]
- 6.Aglietti P, Buzzi R, Zaccherotti G, De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22:211–7. doi: 10.1177/036354659402200210. [DOI] [PubMed] [Google Scholar]
- 7.Bonamo JJ, Krinick RM, Sporn AA. Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction.A report of two cases. J Bone Joint Surg Am. 1984;66:1294–7. [PubMed] [Google Scholar]
- 8.Atkinson TS, Atkinson PJ, Mendenhall HV, Haut RC. Patellar tendon and infrapatellar fat pad healing after harvest of an ACL graft. J Surg Res. 1998;79:25–30. doi: 10.1006/jsre.1998.5387. [DOI] [PubMed] [Google Scholar]
- 9.Christen B, Jakob RP. Fractures associated with patellar ligament grafts in cruciate ligament surgery. J Bone Joint Surg Br. 1992;74:617–9. doi: 10.1302/0301-620X.74B4.1624526. [DOI] [PubMed] [Google Scholar]
- 10.Kartus J, Ejerhed L, Sernert N, Brandsson S, Karlsson J. Comparison of traditional and subcutaneous patellar tendon harvest.A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med. 2000;28:328–35. doi: 10.1177/03635465000280030801. [DOI] [PubMed] [Google Scholar]
- 11.Tashiro T, Kurosawa H, Kawakami A, Hikita A, Fukui N. Influence of medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction.A detailed evaluation with comparison of single- and double-tendon harvest. Am J Sports Med. 2003;31:522–9. doi: 10.1177/31.4.522. [DOI] [PubMed] [Google Scholar]
- 12.Burks RT, Crim J, Fink BP, Boylan DN, Greis PE. The effects of semitendinosus and gracilis harvest in anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1177–85. doi: 10.1016/j.arthro.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Goradia VK, Grana WA, Pearson SE. Factors associated with decreased muscle strength after anterior cruciate ligament reconstruction with hamstring tendon grafts. Arthroscopy. 2006;22:80. doi: 10.1016/j.arthro.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Ohkoshi Y, Inoue C, Yamane S, Hashimoto T, Ishida R. Changes in muscle strength properties caused by harvesting of autogenous semitendinosus tendon for reconstruction of contralateral anterior cruciate ligament. Arthroscopy. 1998;14:580–4. doi: 10.1016/s0749-8063(98)70053-2. [DOI] [PubMed] [Google Scholar]
- 15.Rose T, Hepp P, Venus J, Stockmar C, Josten C, Lill H. Prospective randomized clinical comparison of femoral transfixation versus bioscrew fixation in hamstring tendon ACL reconstruction – A preliminary report. Knee Surg Sports Traumatol Arthrosc. 2006;14:730–8. doi: 10.1007/s00167-006-0034-9. [DOI] [PubMed] [Google Scholar]
- 16.More RC, Karras BT, Neiman R, Fritschy D, Woo SL, Daniel DM. Hamstrings – An anterior cruciate ligament protagonist.An in vitro study. Am J Sports Med. 1993;21:231–7. doi: 10.1177/036354659302100212. [DOI] [PubMed] [Google Scholar]
- 17.Sakai H, Yajima H, Kobayashi N, Kanda T, Hiraoka H, Tamai K, et al. Gravity-assisted pivot-shift test for anterior cruciate ligament injury: A new procedure to detect anterolateral rotatory instability of the knee joint. Knee Surg Sports Traumatol Arthrosc. 2006;14:2–6. doi: 10.1007/s00167-005-0630-0. [DOI] [PubMed] [Google Scholar]
- 18.Zhao J, Huangfu X. The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med. 2012;40:662–71. doi: 10.1177/0363546511428782. [DOI] [PubMed] [Google Scholar]
- 19.Miller RH, Azar FM. Knee injuries. In: Azar FM, Beaty JH, Canale ST, editors. Campbell's Operative Orthopaedics. 13th ed. Philadelphia, PA: Elsevier/Mosby; 2017. pp. 2211–5. [Google Scholar]
- 20.Shi FD, Hess DE, Zuo JZ, Liu SJ, Wang XC, Zhang Y, et al. Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J Knee Surg. 2019;32:804–11. doi: 10.1055/s-0038-1669951. [DOI] [PubMed] [Google Scholar]
- 21.Xu H, Lin W, Jin G, Xin D, Zhang J, Kang K, et al. Graft choice for anatomic anterior cruciate ligament reconstruction: The comparison between thin autograft and thick hybrid graft.An observational study. Medicine (Baltimore) 2018;97:e11597. doi: 10.1097/MD.0000000000011597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fu FH, van Eck CF, Tashman S, Irrgang JJ, Moreland MS. Anatomic anterior cruciate ligament reconstruction: A changing paradigm. Knee Surg Sports Traumatol Arthrosc. 2015;23:640–8. doi: 10.1007/s00167-014-3209-9. [DOI] [PubMed] [Google Scholar]
- 23.Figueroa F, Figueroa D, Espregueira-Mendes J. Hamstring autograft size importance in anterior cruciate ligament repair surgery. EFORT Open Rev. 2018;3:93–7. doi: 10.1302/2058-5241.3.170038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhatomy S, Asikin AIZ, Wardani AE, Rukmoyo T, Lumban-Gaol I, Budhiparama NC. Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3552–9. doi: 10.1007/s00167-019-05455-w. [DOI] [PubMed] [Google Scholar]
- 25.Angthong C, Chernchujit B, Apivatgaroon A, Chaijenkit K, Nualon P, Suchao K. The anterior cruciate ligament reconstruction with the peroneus longus tendon: A biomechanical and clinical evaluation of the donor ankle morbidity. J Med Assoc Thai. 2015;98:555–60. [PubMed] [Google Scholar]
- 26.Kerimoğlu S, Aynaci O, Saraçoğlu M, Aydin H, Turhan AU. Anterior cruciate ligament reconstruction with the peroneus longus tendon. Acta Orthop Traumatol Turc. 2008;42:38–43. doi: 10.3944/aott.2008.038. [DOI] [PubMed] [Google Scholar]
- 27.Sasetyo DR, Rhatomy S, Pontoh LA. Peroneus longus tendon: The promising graft for anterior cruciate ligament reconstruction surgery. Asia Pac J Sport Med Arthrosc Rehabil Technol. 2017;9:25. [Google Scholar]
- 28.Freedman KB, D'Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: A metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 29.Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22:100–10. doi: 10.1016/j.knee.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 30.Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: Differences and similarities. Am J Sports Med. 2005;33:1337–45. doi: 10.1177/0363546504274145. [DOI] [PubMed] [Google Scholar]
- 31.Paschos NK, Howell SM. Anterior cruciate ligament reconstruction: Principles of treatment. EFORT Open Rev. 2016;1:398–408. doi: 10.1302/2058-5241.1.160032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wheeless CR 3rd. Peroneus longus. Wheeless' Textbook of Orthopaedics. 2012. [Last accessed on 2014 Sep 29]. Available from: http://www. wheelessonline.com/ortho/peroneus_longus .
- 33.Takeda Y, Kashiwaguchi S, Matsuura T, Higashida T, Minato A. Hamstring muscle function after tendon harvest for anterior cruciate ligament reconstruction: Evaluation with T2 relaxation time of magnetic resonance imaging. Am J Sports Med. 2006;34:281–8. doi: 10.1177/0363546505279574. [DOI] [PubMed] [Google Scholar]
- 34.Coupens SD, Yates CK, Sheldon C, Ward C. Magnetic resonance imaging evaluation of the patellar tendon after use of its central one-third for anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:332–5. doi: 10.1177/036354659202000317. [DOI] [PubMed] [Google Scholar]
- 35.Nixon RG, SeGall GK, Sax SL, Cain TE, Tullos HS. Reconstitution of the patellar tendon donor site after graft harvest. Clin Orthop Relat Res. 1995;317:162–71. [PubMed] [Google Scholar]
- 36.Thordarson DB, Shean CJ. Nerve and tendon lacerations about the foot and ankle. J Am Acad Orthop Surg. 2005;13:186–96. doi: 10.5435/00124635-200505000-00005. [DOI] [PubMed] [Google Scholar]


