Summary
We report findings in five patients who presented with venous thrombosis and thrombocytopenia 7 to 10 days after receiving the first dose of the ChAdOx1 nCoV-19 adenoviral vector vaccine against coronavirus disease 2019 (Covid-19). The patients were health care workers who were 32 to 54 years of age. All the patients had high levels of antibodies to platelet factor 4–polyanion complexes; however, they had had no previous exposure to heparin. Because the five cases occurred in a population of more than 130,000 vaccinated persons, we propose that they represent a rare vaccine-related variant of spontaneous heparin-induced thrombocytopenia that we refer to as vaccine-induced immune thrombotic thrombocytopenia.
The European Medicines Agency has approved five vaccines against coronavirus disease 2019 (Covid-19), and more than 600 million doses have been administered globally.1 In Norway, older adults living in institutional settings and health care professionals who are in close contact with patients with Covid-19 have been prioritized to receive the BNT162b2 mRNA Covid-19 vaccine (Pfizer–BioNTech). In addition, the ChAdOx1 nCoV-19 vaccine (AstraZeneca) has been administered to health care professionals younger than 65 years of age who do not have close contact with patients with Covid-19. As of March 20, 2021, when administration of the vaccine was paused, a total of 132,686 persons in Norway had received the first dose of the ChAdOx1 nCoV-19 vaccine and none had received the second dose.2
Within 10 days after receiving a first immunization with ChAdOx1 nCoV-19, five health care workers 32 to 54 years of age presented with thrombosis in unusual sites and severe thrombocytopenia. Four of the patients had major cerebral hemorrhage. Here we describe this vaccine-induced syndrome of severe thrombosis and thrombocytopenia found among these five patients admitted to Oslo University Hospital.
Case Reports
Patient 1 was a 37-year-old woman with headaches that developed 1 week after vaccination with ChAdOx1 nCoV-19. At presentation to the emergency department the next day, she had fever and persistent headaches. She was found to have severe thrombocytopenia (Table 1). Computed tomography (CT) of the head showed thrombosis in the left transverse and sigmoid sinuses. Because of the low platelet count, a reduced dose of dalteparin (2500 IU daily) was given. The next day, her clinical condition deteriorated, and a new CT scan showed a massive cerebellar hemorrhage and edema in the posterior fossa. She was treated with platelet transfusions and decompressive craniectomy. During surgery, massive and uncontrollable edema developed. The patient died on day 2 after surgery.
Table 1. Characteristics of the Patients.*.
| Characteristic | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 |
|---|---|---|---|---|---|
| Age — yr | 37 | 42 | 32 | 39 | 54 |
| Sex | Female | Female | Male | Female | Female |
| Preexisting conditions | Pollen allergy | Pollen allergy | Asthma | None | Hypertension |
| Medication on admission | Contraceptive pill | Contraceptive vaginal ring | None | None | Hormone-replacement therapy, antihypertensive agents |
| Time from vaccination to admission — days | 8 | 10 | 7 | 10 | 7 |
| Symptoms | Fever, headaches, visual disturbances | Headaches, drowsiness | Back pain | Headaches, abdominal pain | Headaches, hemiparesis |
| Location of thrombosis | Cortical veins, left transverse sinus, and sigmoid left sinus | Cortical veins, left transverse sinus, and left sigmoid sinus | Portal vein, left hepatic vein, splenic vein, azygos vein, hemiazygos vein, and several basivertebral veins | Inferior sagittal sinus, vein of Galen, straight sinus, right transverse sinus, and right sigmoid sinus | Cortical veins, superior sagittal sinus, both transverse sinuses, and left sigmoid sinus |
| Platelet count nadir — per mm3 | 22,000 | 14,000 | 10,000 | 70,000 | 19,000 |
| d-dimer peak — mg/liter | >35 | >35 | >35 | 13 | >35 |
| INR peak | 1.2 | 1.0 | 1.1 | 1.3 | 1.1 |
| aPTT peak — sec | 25 | 31 | 25 | 25 | 29 |
| Fibrinogen nadir — g/liter† | 2.1 | 0.8 | 2.3 | 1.2 | 1.2 |
| SARS-CoV-2 antibody test results | |||||
| Nucleocapsid protein | Negative | Negative | Negative | Negative | Negative |
| Spike protein | Positive | Positive | Positive | Positive | Positive |
| Anticoagulation treatment | Initial low dose of LMWH | Reduced dose of LMWH | Reduced dose of LMWH | Reduced dose of LMWH | Heparin (5000 IU) |
| No. of platelet units transfused | 7 | 19 | 2 | 0 | 2 |
| Other treatment | None | Methylprednisolone (1 mg/kg), IVIG (1 g/kg) | Prednisolone (1 mg/kg), IVIG (1 g/kg) | Prednisolone (1 mg/kg), IVIG (1 g/kg) | Methylprednisolone (1 mg/kg), IVIG (1 g/kg) |
| Outcome | Fatal | Fatal | Full recovery | Full recovery | Fatal |
The abbreviation aPTT denotes activated partial thromboplastin time, INR international normalized ratio, IVIG intravenous immune globulin, LMWH low-molecular-weight heparin, and SARS-CoV-2 severe acute respiratory syndrome coronavirus 2.
The reference range used for fibrinogen at Oslo University Hospital is 1.9 to 4.0 g per liter.
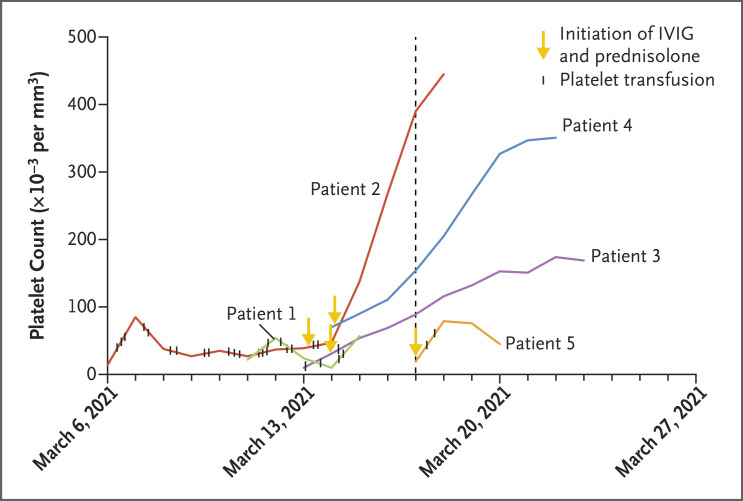
Patient 2 was a 42-year-old woman who had headaches 1 week after vaccination with ChAdOx1 nCoV-19. Her condition worsened rapidly, and she presented with reduced consciousness at presentation to the emergency department 3 days later. Her platelet count was 14,000 per cubic millimeter. ADAMTS13 activity was found to be normal. CT venography revealed venous thrombosis with occlusion of the transverse and sigmoid sinuses and hemorrhagic infarction in the left hemisphere. Hemicraniectomy was performed, and treatment with dalteparin at a dose of 2500 IU daily was initiated. She received multiple platelet transfusions over the following days. On day 8, methylprednisolone (1 mg per kilogram of body weight per day) and intravenous immune globulin (1 g per kilogram per day) were administered. The platelet count increased thereafter (Figure 1). However, the patient died after 2 weeks in the intensive care unit (ICU) from increased intracranial pressure and severe cerebral hemorrhagic infarction on day 15.
Figure 1. Platelet Count Responses to Treatment.
The vertical dashed line indicates the time at which the results of platelet factor 4 (PF4)–polyanion antibody tests were known. IVIG denotes intravenous immune globulin.
Patient 3, a 32-year-old man, presented to the emergency department with a backache 7 days after vaccination with ChAdOx1 nCoV-19. He had no preexisting conditions apart from asthma. No clinical signs of bleeding and no neurologic deficits were evident. Blood tests showed severe isolated thrombocytopenia (Table 1). A thoracoabdominal CT scan showed thrombosis of several branches of the portal vein with occlusion of the left intrahepatic portal vein and left hepatic vein. In addition, thrombosis was observed in the splenic vein, the azygos vein, and the hemiazygos vein. Contrast-enhanced magnetic resonance imaging (MRI) of the spine showed areas of hypointensity in several thoracic vertebrae and basivertebral veins, indicating compromised venous drainage. He was treated with intravenous immune globulin (1 g per kilogram per day for 2 days) and prednisolone (1 mg per kilogram per day). Dalteparin was administered at a dose of 5000 IU (one dose on the first day and two doses on the second day), after which the platelet count returned to normal and the dose was increased to 200 IU per kilogram per day (Figure 1). An abdominal CT scan indicated partial resolution of thrombosis. He was discharged from the hospital on day 12 in good health with warfarin and tapering doses of prednisolone.
Patient 4, a previously healthy 39-year-old woman who was vaccinated with ChAdOx1 nCoV-19, presented to the emergency department with abdominal pain and headaches 8 days after vaccination. A mild thrombocytopenia was revealed. An abdominal ultrasound examination was normal, and she was discharged. The headaches increased in intensity, and she returned to the emergency department 2 days later. Cerebral CT with venography showed massive thrombosis in the deep and superficial cerebral veins and right cerebellar hemorrhagic infarction. The platelet count was 70,000 per cubic millimeter. She was afebrile and had no signs of infection and no neurologic deficits. Treatment with dalteparin (200 IU per kilogram per day), prednisolone (1 mg per kilogram per day), and intravenous immune globulin (1 g per kilogram per day for 2 days) was started. The platelet count was normalized within 2 days (Figure 1). Follow-up CT venography showed recanalization in the affected cerebral venous sinuses. When she was discharged after 10 days, the symptoms had resolved. Her anticoagulation treatment was changed from dalteparin to warfarin, and treatment with prednisolone was continued in tapering doses.
Patient 5, a 54-year-old woman with a history of hypertension who was receiving hormone-replacement therapy, presented to the emergency department with stroke symptoms that had been present when she woke up from sleep, including hemiparesis on the left side of her body, 1 week after vaccination with ChAdOx1 nCoV-19. The platelet count was 19,000 per cubic millimeter, and CT of the head showed a right frontal hemorrhage. She received a platelet transfusion before she was transferred to our hospital, where treatment with methylprednisolone (1 mg per kilogram per day) and intravenous immune globulin (1 g per kilogram per day for 2 days) was commenced. A CT scan with venography showed a massive cerebral vein thrombosis with global edema and growth of hematoma (Table 1, and Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Venous recanalization was achieved 4 hours after admission by endovascular intervention with thrombectomy after administration of 5000 IU of unfractionated heparin. During the procedure, a fully dilated right pupil was observed, and decompressive hemicraniectomy was performed immediately. Two days later, treatment was withdrawn because of an uncontrollable increase in intracranial pressure.
Methods
Ethical Considerations
Written informed consent for publication was obtained from all patients. In the event that the patient was not able to provide consent, a relative of the patient provided written informed consent. The authors vouch for the accuracy and completeness of the data in this report.
Immunoassays and Functional and Serologic Testing
Antibodies to platelet factor 4 (PF4) in complex with poly(vinyl sulfonate) (heparin analogue) in patient serum were tested with a LIFECODES PF4 IgG enzyme-linked immunosorbent assay (ELISA) (Immucor) in accordance with the manufacturer’s instructions (dilution, 1:50), including a confirmatory inhibition test with heparin in high concentration. Serial dilution of serum in an ELISA was also performed.3 Patient serum was also evaluated in a functional test with the use of heparin-induced multiple-electrode aggregometry on a Multiplate analyzer (Dynabyte Medical).4,5 Here, the ability of serum to aggregate platelets was measured in the presence of saline buffer and in the presence of unfractionated heparin at high concentration (96 IU per milliliter) and low concentration (0.96 IU per milliliter).
Serum antibodies to the spike and nucleocapsid proteins of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were measured with the Roche Elecsys platform and with an in-house bead-based assay for IgG antibodies to full-length recombinant proteins.6
Results
Laboratory Testing
Levels of d-dimer were elevated at the time of admission in all patients. The international normalized ratio (INR) and activated partial thromboplastin time were within the normal range. The fibrinogen level was lower than normal in Patient 2 and was slightly lower than normal in Patients 4 and 5 (Table 1). The C-reactive protein level was moderately elevated in Patients 1, 3, and 5. Screening for thrombophilia with proteins C and S and antithrombin was negative. Antiphospholipid antibodies were detected only in Patient 3, who had a slightly elevated anticardiolipin IgG antibody level of 43 IgG phospholipid (GPL) units. Levels of complement proteins (C1q, C4, and C3) and activation products (sC5b-9) were within the normal range in all patients. No patients had signs of hemolysis, and ADAMTS13 activity was normal in the one patient in whom it was assessed.
Platelet Immunologic Testing
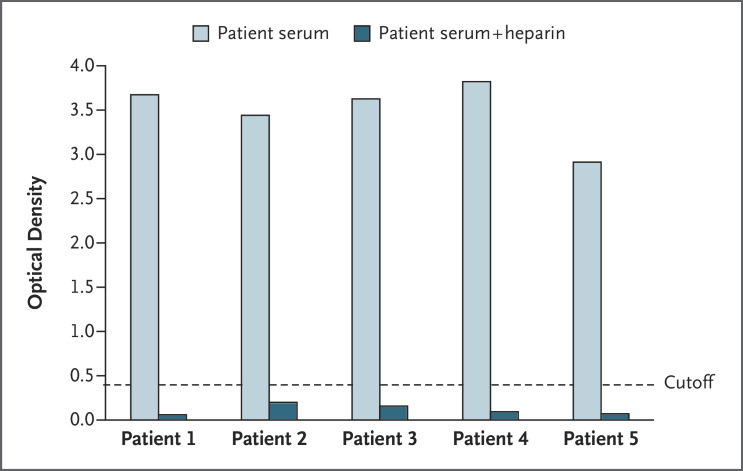
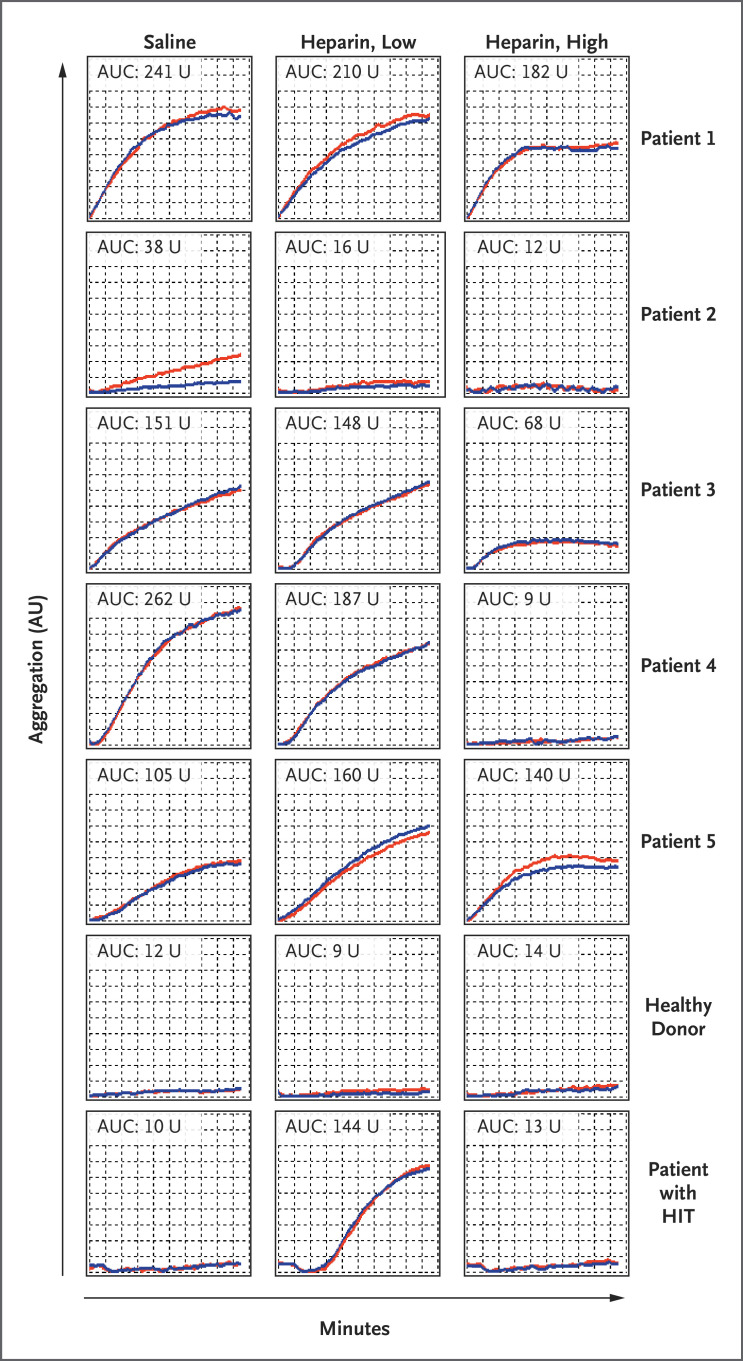
All five patients had high levels of IgG antibodies to PF4–polyanion complexes, as indicated by strikingly high optical density values — in the range of 2.9 to 3.8 — measured by ELISA. The reactivity was efficiently inhibited by heparin in all samples (Figure 2). Functional activity of serum from a patient with typical heparin-induced thrombocytopenia was compared with that of serum from our patients. Platelets from the patient with heparin-induced thrombocytopenia were not activated unless low levels of heparin were added, and platelet aggregation was efficiently reduced by high heparin levels (Figure 3). Platelets in serum from Patients 1, 3, 4, and 5 were clearly activated in the absence of added heparin. The platelet aggregation curve for Patient 2 was not a sigmoid curve and was considered to be inconclusive. Platelet aggregation was inhibited efficiently by high-dose heparin in Patients 3 and 4 but was inhibited less efficiently in Patients 1 and 5.
Figure 2. IgG PF4–Polyanion Detection in Serum.
IgG PF4–polyanion antibodies in serum from the patients were measured by enzyme-linked immunosorbent assay. Serum from all the patients showed strong reactivity that was efficiently inhibited (>97%) by the addition of a saturating dose of heparin (100 IU per milliliter). Samples were run in duplicate. A mean optical density of 0.4 or higher indicates the presence of antibodies.
Figure 3. Platelet-Aggregating Potential of Serum in Functional Testing.
Aggregation of donor platelets after incubation with serum from the patients was measured by whole-blood impedance aggregometry. The measurements were performed in the presence of low or high heparin concentrations and in the absence of added heparin (saline). Serum from a healthy donor and serum from a patient with typical heparin-induced thrombocytopenia (HIT) are also shown. The red and blue lines represent duplicate measurements. AU denotes arbitrary units, and AUC the area under the curve.
Covid-19 Serologic Testing
All five patients were negative for antibodies to SARS-CoV-2 nucleocapsid protein. Thus, previous infection with SARS-CoV-2 was highly unlikely. The levels of antibodies to spike protein varied with the assay, but anti-spike binding was detected in at least one assay in all five patients. The variation most likely reflects the fact that the anti-spike vaccine response was in an early phase.
Discussion
We present five cases of severe venous thromboembolism in unusual sites and concomitant thrombocytopenia that occurred 7 to 10 days after vaccination for Covid-19. Four of the patients had severe cerebral venous thrombosis with intracranial hemorrhage, and the outcome was fatal in three. Thrombotic thrombocytopenic purpura and immune thrombocytopenic purpura were not suspected because of the absence of hemolysis and because of the good response to platelet transfusions, respectively. A common denominator in all five patients was a high level of antibodies to PF4–polyanion complexes. We therefore propose that these cases represent a vaccine-related variant of spontaneous heparin-induced thrombocytopenia that we refer to as vaccine-induced immune thrombotic thrombocytopenia (VITT).
All the patients had strikingly high levels of antibodies to PF4–polyanion complexes. Although the optical density values may not be directly comparable between studies, it is worth noting that 5 to 7% of blood donors have detectable PF4–heparin antibodies; however, typical blood donors rarely have levels yielding an optical density higher than 1.6.7 Moreover, in patients with typical heparin-induced thrombocytopenia, optical density values higher than 2 are unusual.8 Nearly all healthy adults have a reservoir of B cells specific for PF4–heparin complexes; production of “heparin-induced thrombocytopenia–like” antibodies by these B cells is kept in check by immune regulatory mechanisms.9,10
In contrast to platelet aggregation in patients with typical heparin-induced thrombocytopenia, platelet aggregation in our patients was less dependent on physiological levels of heparin and was less sensitive to inhibition with high-dose heparin. Since Patients 1, 2, 3, and 4 had received low-molecular-weight heparin before blood samples were obtained, we cannot rule out the presence of circulating complexes containing antibodies bound to PF4 and low-molecular-weight heparin. Such complexes are generally disrupted in the presence of a high concentration of unfractionated heparin (96 IU per milliliter), but this was not observed in all cases. Moreover, Patient 5 had not received heparin. Collectively, these results suggest that the serum in these patients contained immune complexes with a mixture of antibody specificities similar to those described in the serum of patients with autoimmune heparin-induced thrombocytopenia.8 It has not yet been determined whether the serum in our patients contained antibodies that bound PF4 alone.
Our findings indicate a shared pathophysiological basis of the condition in these five patients and should raise awareness that a syndrome similar to autoimmune heparin-induced thrombocytopenia may occur in some persons after vaccination with ChAdOx1 nCoV-19. By providing a link between thrombosis and the immune system, these results strengthen the view that vaccination may have triggered the syndrome.
In these cases, the characteristic antibodies were first identified after the initiation of anticoagulation treatment with low-molecular-weight heparin for life-threatening thrombosis and thrombocytopenia (Figure 1). With the antibody results in hand, the clinicians faced the dilemma of deciding which anticoagulant to administer during this syndrome, which is usually associated with heparin. However, platelet counts were increasing after concomitant treatment with intravenous immune globulin and prednisolone had been initiated, and no clinical evidence suggested that thrombosis was increasing. Moreover, there were significant concerns that administration of anticoagulation alternatives to heparin or low-molecular-weight heparin might lead to aggravation of the ongoing intracerebral hemorrhage. Fondaparinux has a longer half-life than low-molecular-weight heparin, and a well-documented reversal strategy for factor Xa inhibitors is not available. It is worth noting that platelet counts continued to increase in all the patients despite continuation of treatment with low-molecular-weight heparin (Figure 1). This finding may reflect the efficacy of early treatment with intravenous immune globulin, which has proved to be highly effective against spontaneous heparin-induced thrombocytopenia.11
Treating severely ill patients such as those described in this report is always challenging. The most important implication of our findings is that physicians should have a low threshold for requesting ELISA testing for PF4–polyanion antibodies, including confirmatory functional testing, in patients who have unexpected symptoms after vaccination.
Although rare, VITT is a new phenomenon with devastating effects for otherwise healthy young adults and requires a thorough risk–benefit analysis. The findings of our study indicate that VITT may be more frequent than has been found in previous studies in which the safety of the ChAdOx1 nCoV-19 vaccine has been investigated.12
Acknowledgments
We thank Siw Leiknes Ernstsen, M.D., of the Norwegian National Unit for Platelet Immunology at University Hospital of North Norway for important contributions to laboratory investigations of the cases.
Supplementary Appendix
Disclosure Forms
Data Sharing Statement
This article was published on April 9, 2021, at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.WHO Coronavirus (COVID-19) Dashboard. Geneva: World Health Organization. April 5, 2021. (https://covid19.who.int/). [Google Scholar]
- 2.Norwegian Institute of Public Health. COVID 19 Ukerapport — uke 10, March 17, 2021. (https://www.fhi.no/contentassets/8a971e7b0a3c4a06bdbf381ab52e6157/vedlegg/2021/ukerapport-for-uke-10-08.03---14.03.21.pdf).
- 3.Warkentin TE, Sheppard JI, Moore JC, Kelton JG. The use of well-characterized sera for the assessment of new diagnostic enzyme-immunoassays for the diagnosis of heparin-induced thrombocytopenia. J Thromb Haemost 2010;8:216-218. [DOI] [PubMed] [Google Scholar]
- 4.Galea V, Khaterchi A, Robert F, Gerotziafas G, Hatmi M, Elalamy I. Heparin-induced multiple electrode aggregometry is a promising and useful functional tool for heparin-induced thrombocytopenia diagnosis: confirmation in a prospective study. Platelets 2013;24:441-447. [DOI] [PubMed] [Google Scholar]
- 5.Morel-Kopp MC, Mullier F, Gkalea V, et al. Heparin-induced multi-electrode aggregometry method for heparin-induced thrombocytopenia testing: communication from the SSC of the ISTH. J Thromb Haemost 2016;14:2548-2552. [DOI] [PubMed] [Google Scholar]
- 6.Holter JC, Pischke SE, de Boer E, et al. Systemic complement activation is associated with respiratory failure in COVID-19 hospitalized patients. Proc Natl Acad Sci U S A 2020;117:25018-25025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hursting MJ, Pai PJ, McCracken JE, et al. Platelet factor 4/heparin antibodies in blood bank donors. Am J Clin Pathol 2010;134:774-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greinacher A, Selleng K, Warkentin TE. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost 2017;15:2099-2114. [DOI] [PubMed] [Google Scholar]
- 9.Zheng Y, Wang AW, Yu M, et al. B-cell tolerance regulates production of antibodies causing heparin-induced thrombocytopenia. Blood 2014;123:931-934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng Y, Zhu W, Haribhai D, et al. Regulatory T cells control PF4/heparin antibody production in mice. J Immunol 2019;203:1786-1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Irani M, Siegal E, Jella A, Aster R, Padmanabhan A. Use of intravenous immunoglobulin G to treat spontaneous heparin-induced thrombocytopenia. Transfusion 2019;59:931-934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramasamy MN, Minassian AM, Ewer KJ, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet 2021;396:1979-1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.