Abstract
Urinary incontinence remains a significant postprostatectomy sequala. While it has been found that many patient and technical factors contribute to postprostatectomy incontinence, the impact of anatomical differences by races has not been studied. Shorter preoperative membranous urethral length (MUL) on prostate magnetic resonance imaging has been associated with a higher risk of postprostatectomy incontinence. We compared MUL between Asian and non-Asian men and their postprostatectomy urinary function using the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP). We found that MUL was significantly shorter for Asian (7.9 mm, 95% confidence interval [CI] 7.5–8.3) than for non-Asian men (10.9 mm, 95% CI 10.2–11.7), with a mean difference of 3.0 mm (95% CI 2.15–3.87; p < 0.01). In addition, Asian men had significantly worse EPIC-CP urinary scores ≥12 mo after prostatectomy (3.82, 95% CI 2.47–5.17) in comparison to non-Asian men (1.95, 95% CI 1.11–2.79), with a mean difference of 1.87 (95% CI 0.32–3.42; p = 0.022). Confirmatory studies are needed to explore racial differences in MUL and its effect on postprostatectomy incontinence.
Patient summary
We compared the length of a specific section of the urethra (called the membranous urethra) and urinary function after removal of the prostate between Asian and non-Asian men. We found that the membranous urethra is significantly shorter in Asian men and they have worse urinary continence after removal of the prostate. More studies are needed to confirm our findings.
Keywords: Membranous urethral length, Urinary function, Prostate cancer, Robot-assisted radical prostatectomy
The United States Preventive Services Task Force infographic states that 19% of men will experience persistent urinary incontinence after prostate cancer treatment [1]. Approximately 60 000 men undergo radical prostatectomy (RP) in the United States annually; thus, approximately 11 400 men will experience post-RP urinary incontinence this year [2]. Post-RP incontinence may limit a physically active lifestyle, cause embarrassment and depression, and may not respond to corrective therapy. The risk of post-RP incontinence varies according to the definition and methodology applied, as well as the surgical technique and surgeon experience. Although technical modifications to decrease post-RP incontinence have been described, there is no technique that eliminates its occurrence. Therefore, better patient selection may be the most practical way to attenuate the occurrence of post-RP incontinence.
Older patient age and shorter membranous urethral length (MUL) are associated with worse post-RP incontinence [3]. A systematic review by Mungovan et al [4] suggested that longer preoperative MUL is positively associated with return of post-RP continence. However, most of the evidence on MUL arises from studies on men of European descent. Hu et al [5] recently demonstrated that Asian-American men have significantly worse urinary continence within 12 mo after RP in comparison to their non-Asian counterparts; however, the contributory factors remain unknown. We hypothesized that Asian men may have worse post-RP urinary function because of shorter MUL in comparison to non-Asian men. Therefore, we aimed to assess differences in MUL between Asian and non-Asian men and to evaluate whether these differences were associated with worse urinary function after RP.
We identified 274 men with localized prostate cancer who underwent prostate magnetic resonance imaging (MRI) compliant with Prostate Imaging-Reporting and Data System version 2.1 technical recommendations at our institution before robotic RP performed by a single surgeon (J.C.H.) between June 2015 and June 2020. Thirty-six men who self-identified as “Asian” and for whom follow-up information was available were included (Supplementary Fig. 1). We subsequently age-matched these men randomly to 36 non-Asian men to compare MUL and Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP) urinary function outcomes [6]. The EPIC-CP urinary incontinence score ranges from 0 to 12, with higher scores indicating worse function.
After undergoing training with a fellowship-trained uroradiologist (D.J.M.), measurements were performed by two blinded raters (S.P.B., A.R.; urology residents) on sagittal small field-of-view T2-weighted preoperative prostate MRI scans (Supplementary Fig. 2) [7]. Final MUL measurements were made by averaging the measurements recorded by the two raters. For eight men (11.1%) for whom MUL measurements differed by >20% between the two raters, the uroradiologist’s independent measurement was used in the final analysis.
There were no significant differences in age, body mass index (BMI), prostate-specific antigen, RP pathology, nerve-sparing status, or prostate volume by race (Table 1). The median follow-up was 12 mo for both Asian and non-Asian men. The inter-reader agreement k value was 0.92. MUL was significantly shorter for Asian (7.9 mm, 95% confidence interval [CI] 7.5–8.3) than for non-Asian men (10.9 mm, 95% CI 10.2–11.7), with a mean difference of 3.0 mm (95% CI 2.15–3.87; p < 0.01).
Table 1.
Preoperative characteristics and MRI measurements
| Asian | Non-Asian | p valuea | |
|---|---|---|---|
| (n = 36) | (n = 36) | ||
| Clinicopathologic characteristics | |||
| Mean age, yr (95% CI) | 66.8 (64.7–69.0) | 65.6 (62.6–68.6) | 0.61 |
| Mean body mass index, kg/m2 (95% CI) | 25.9 (24.7–27.2) | 26.7 (25.7–27.8) | 0.33 |
| Mean PSA ng/ml (95% CI) | 10.3 (7.6–12.9) | 8.6 (6.3–11.0) | 0.35 |
| Median Gleason grade group at RP (IQR) | 3 (2–4) | 2 (2–3) | 1.0 |
| Nerve-sparing status, n (%) | 1.0 | ||
| Complete | 31 (86) | 31 (86) | |
| Partial | 5 (14) | 5 (14) | |
| MRI measurements | |||
| Mean prostate volume, ml (95% CI) | 50.4 (37.8–63.0) | 41.5 (25.9–46.7) | 0.20 |
| Mean urethral measurements, mm (95% CI) | |||
| Membranous urethral length | 7.9 (7.5–8.3) | 10.9 (10.2–11.7) | <0.01 |
| Infraprostatic urethral length | 13.4 (12.5–14.3) | 16.8 (15.7–17.9) | <0.01 |
| Urethral stump | 5.5 (4.8–6.4) | 5.9 (5.3–6.5) | 0.12 |
CI = confidence interval; IQR = interquartile range; MRI = magnetic resonance imaging; PSA = prostate-specific antigen; RP = radical prostatectomy.
Statistical tests performed: paired t test, Wilcoxon-Mann-Whitney test, χ2 test.
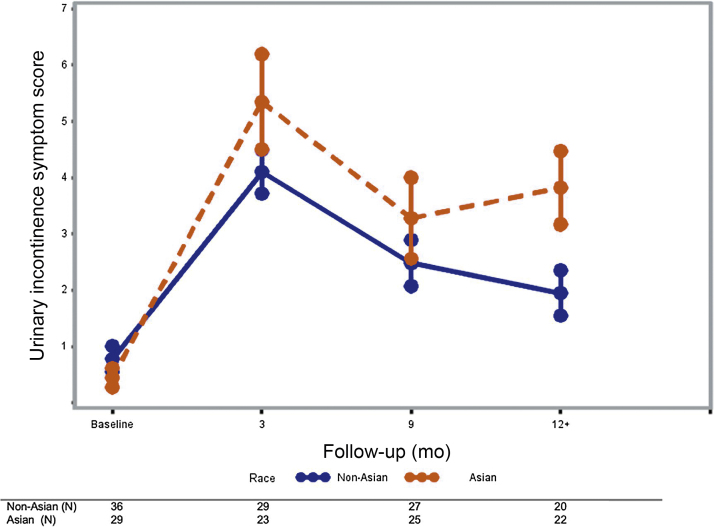
A generalized estimating equation ordinal regression model was constructed with EPIC-CP score as the dependent variable and covariables of race, age, and time following RP (3, 9, and ≥12 mo). Follow-up outcomes at ≥12 mo were pooled because urinary continence does not significantly improve after that time point [8]. There were no differences in EPIC-CP scores between Asian and non-Asian men at baseline, 3, or 9 mo. Asian men had significantly worse EPIC-CP urinary scores at ≥12 mo after RP (3.82, 95% CI 2.47–5.17 vs 1.95, 95% CI 1.11–2.79; mean difference 1.87; 95% CI 0.32–3.42; p = 0.022; Fig. 1). Our model demonstrated that Asian race is predictive of a higher EPIC-CP urinary score over time when compared to non-Asian race (parameter estimate 0.56, 95% CI 0.04–1.08; p = 0.034; Supplementary Table 1). Furthermore, we found that lower MUL (p = 0.03) and Asian race (p = 0.036) were each associated with increased EPIC-CP scores at 12 mo in an ordinal logistic model that included age and BMI (Supplementary Table 2).
Fig. 1.
Urinary function recovery (Expanded Prostate Cancer Index Composite for Clinical Practice score) for Asian versus non-Asian men. The mean and error bar are presented for each time point.
Preoperative MUL is a prognostic risk factor for post-RP continence [3]. Current evidence shows that longer MUL has a significantly positive effect on overall time to continence recovery [4]. However, the role of racial variation and its association with MUL and post-RP continence recovery has not been explored; our study revealed that Asian men have shorter MUL compared to their non-Asian counterparts. We also compared urinary function recovery and found that Asian men have worse urinary function at >1 yr after RP. Our findings highlight the importance of patient selection to avoid urinary incontinence, particularly for Asian men. Moreover, we observed a significant difference in pelvic anatomy by race, a novel finding that may account for racial differences in post-RP urinary function outcomes.
One of the major principles in achieving post-RP urinary continence is preservation of a functional sphincter mechanism. Longer MUL facilitates this by increasing the urethra pressure profile and allowing preservation of a greater amount of urethral smooth muscle and rhabdosphincter [9]. Furthermore, Vis et al [9] showed that MUL-preserving techniques are associated with better continence rates at 3 and 12 mo after RP. Thus, preoperative assessment of MUL could maximize the potential of these surgical reconstructive techniques and help surgeons in planning a reconstructive approach.
To date, research on the role of race in post-RP incontinence has mostly focused on African American (AA) and White men. DeCastro et al [10] demonstrated that AA men were less likely to experience pad-free continence 12 mo after RP (60% vs 76.4%; p < 0.001). More recently, Hu et al [5] found that men of Asian ancestry have significantly worse urinary function within 12 mo of RP (odds ratio 0.76, 95% CI 0.59–0.98; p = 0.036) compared to non-Asian men. The present study demonstrates that Asian race was associated with shorter MUL and that both Asian race and shorter MUL are associated with worse urinary outcomes.
Our study is not without limitations. First, our sample comprises men of largely East-Asian ancestry (eg, Chinese and Korean); therefore, our broad categorization may not reflect differences between Asian ethnic groups. Second, research on preoperative MUL largely comprises single-center studies owing to the intense efforts required to perform two-reviewer ratings with a referee [7], which limits their generalizability. Furthermore, confirmatory studies and comparative racial studies of MUL are needed to elucidate disparities in outcomes [10]. Third, accurate measurement of MUL requires expertise; urologists who would like to incorporate preoperative MUL measurement in their practice would require education or standardized reporting by a skilled uroradiologist. Finally, we recognize that preservation of maximal urethral length, minimal urethral trauma, and individual pelvic-floor parameters is also important for postprostatectomy continence and cannot be objectively quantified.
In summary, we demonstrate that Asian men have significantly shorter MUL and worse post-RP incontinence. Confirmatory studies are needed to validate our findings.
Author contributions: Spyridon P. Basourakos had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Hu.
Acquisition of data: Basourakos, Ramaswamy, Yu, Margolis, Hu.
Analysis and interpretation of data: Basourakos, Ramaswamy, Yu, Margolis, Hu.
Drafting of the manuscript: Basourakos, Ramaswamy, Margolis, Hu.
Critical revision of the manuscript for important intellectual content: Basourakos, Ramaswamy, Hu.
Statistical analysis: Ramaswamy, Yu, Basourakos.
Obtaining funding: Hu.
Administrative, technical, or material support: Hu.
Supervision: Hu.
Other: None.
Financial disclosures: Spyridon P. Basourakos certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: Jim C. Hu receives research support from the Frederick J. and Theresa Dow Wallace Fund of the New York Community Trust and salary support from grants NIH R01 CA241758, PCORI CER-2019C1-15682 and PCORI CER-2019C2-17372. The sponsors did not play a role in the design and conduct of the study, collection and management of the data, and preparation of the manuscript. Weill Cornell Medicine is the recipient of a research agreement with Siemens Healthineers.
Associate Editor: Guillaume Ploussard
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.euros.2021.03.001.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.U.S. Preventive Services Task Force. Is prostate cancer screening right for you? Understanding the potential benefits vs. harms for men 55-69. www.uspreventiveservicestaskforce.org/Home/GetFileByID/3716.
- 2.Martini A., Marqueen K.E., Falagario U.G. Estimated costs associated with radiation therapy for positive surgical margins during radical prostatectomy. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heesakkers J., Farag F., Bauer R.M., Sandhu J., De Ridder D., Stenzl A. Pathophysiology and Contributing Factors in Postprostatectomy Incontinence: A Review. Eur Urol. 2017;71:936–944. doi: 10.1016/j.eururo.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 4.Mungovan S.F., Sandhu J.S., Akin O., Smart N.A., Graham P.L., Patel M.I. Preoperative membranous urethral length measurement and continence recovery following radical prostatectomy: a systematic review and meta-analysis. Eur Urol. 2017;71:368–378. doi: 10.1016/j.eururo.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu J.C., Ehdaie B., Sandhu J. Asian-American race and urinary continence after radical prostatectomy. Eur Urol Open Sci. 2020;22:51–53. doi: 10.1016/j.euros.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang P., Szymanski K.M., Dunn R.L. Expanded Prostate Cancer Index Composite for clinical practice: development and validation of a practical health related quality of life instrument for use in the routine clinical care of patients with prostate cancer. J Urol. 2011;186:865–872. doi: 10.1016/j.juro.2011.04.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.von Bodman C., Matsushita K., Savage C. Recovery of urinary function after radical prostatectomy: predictors of urinary function on preoperative prostate magnetic resonance imaging. J Urol. 2012;187:945–950. doi: 10.1016/j.juro.2011.10.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandhu J.S., Breyer B., Comiter C. Incontinence after prostate treatment: AUA/SUFU guideline. J Urol. 2019;202:369–378. doi: 10.1097/JU.0000000000000314. [DOI] [PubMed] [Google Scholar]
- 9.Vis A.N., van der Poel H.G., Ruiter A.E.C. Posterior, anterior, and periurethral surgical reconstruction of urinary continence mechanisms in robot-assisted radical prostatectomy: a description and video compilation of commonly performed surgical techniques. Eur Urol. 2019;76:814–822. doi: 10.1016/j.eururo.2018.11.035. [DOI] [PubMed] [Google Scholar]
- 10.DeCastro G.J., Jayram G., Razmaria A., Shalhav A., Zagaja G.P. Functional outcomes in African-Americans after robot-assisted radical prostatectomy. J Endourol. 2012;26:1013–1019. doi: 10.1089/end.2011.0507. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.